Abstract
Introduction:
Acne is a prevalent condition in society affecting nearly 80-90% of adolescents often resulting in secondary damage in the form of scarring. Retinoic acid (RA) is said to improve acne scars and reduce postinflammatory hyperpigmentation while glycolic acid (GA) is known for its keratolytic properties and its ability to reduce atrophic acne scars. There are studies exploring the combined effect of retinaldehyde and GA combination with positive results while the efficacy of retinoic acid and GA (RAGA) combination remains unexplored.
Aim:
The aim of this study remains to retrospectively assess the efficacy of RAGA combination on acne scars in patients previously treated for active acne.
Materials and Methods:
A retrospective assessment of 35 patients using topical RAGA combination on acne scars was done. The subjects were 17-34 years old and previously treated for active acne. Case records and photographs of each patient were assessed and the acne scars were graded as per Goodman and Baron's global scarring grading system (GSGS), before the start and after 12 weeks of RAGA treatment. The differences in the scar grades were noted to assess the improvement.
Results:
At the end of 12 weeks, significant improvement in acne scars was noticed in 91.4% of the patients.
Conclusion:
The RAGA combination shows efficacy in treating acne scars in the majority of patients, minimizing the need of procedural treatment for acne scars.
Keywords: Acne scars, glycolic acid, retinoic acid, retinoic acid and glycolic acid
INTRODUCTION
Acne is a prevalent condition in society affecting nearly 80% of adolescents and often results in secondary damage in the form of scarring. Although these lesions can be treated in a number of ways, they are often physically and emotionally troublesome.[1,2]
Retinoic acid (RA) improves acne scars and postinflammatory hyperpigmentation (PIH),[3,4] while glycolic acid (GA) has keratolytic properties and reduces atrophic acne scars. GA is beneficial in treating PIH and melasma.[5,6,7] Though the efficacy of retinaldehyde and GA (RALGA) combination has been well explored in treating acne scars,[8] the efficacy of RA and GA (RAGA) combination has not been recorded. In addition, RA is more readily available than retinaldehyde in India and therefore, we did the following retrospective assessment to study the efficacy of topical RAGA combination in the treatment of acne scars.
MATERIALS AND METHODS
A retrospective assessment was done at Cutis academy of Cutaneous Sciences, Bengaluru to study the efficacy of topical RA 0.025% and GA 12% (RAGA) combination in treating acne scars and PIH (postacne).
The patients previously treated for active acne and reporting with acne scars at our center were prescribed 0.025% RA and 12% GA. They were advised to mix half a fingertip unit of each and apply evenly over full face sparing 1 cm area around eyes, nostrils and mouth.
The duration of application was escalated gradually from half an hour in the evening to few hours to overnight depending on patient's tolerance to the application. A moisturizer was prescribed to ensure least irritation.
The case records and photographs of 35 patients (12 males and 23 females), who were on topical RAGA treatment for acne scars, were assessed. The patients were 17-34 years (mean age = 26.11 years). Photographs taken at the start of acne scar treatment (baseline) and at the end of 12th week were assessed and case records were reviewed for any history of irritation and noncompliance. The patients had not been on any other treatment for acne scars and PIH.
The acne scars were graded according to Goodman and Baron's quantitative global scarring grading system (GSGS)[9] at baseline and after 12 weeks of topical RAGA treatment [Table 1] by an independent observer. The first point on this grading system is “macular erythematous pigmented” scars and the difference in these grades were considered to measure improvement in PIH.
Table 1.
Goodman and Baron's quantitative global acne scarring grading system
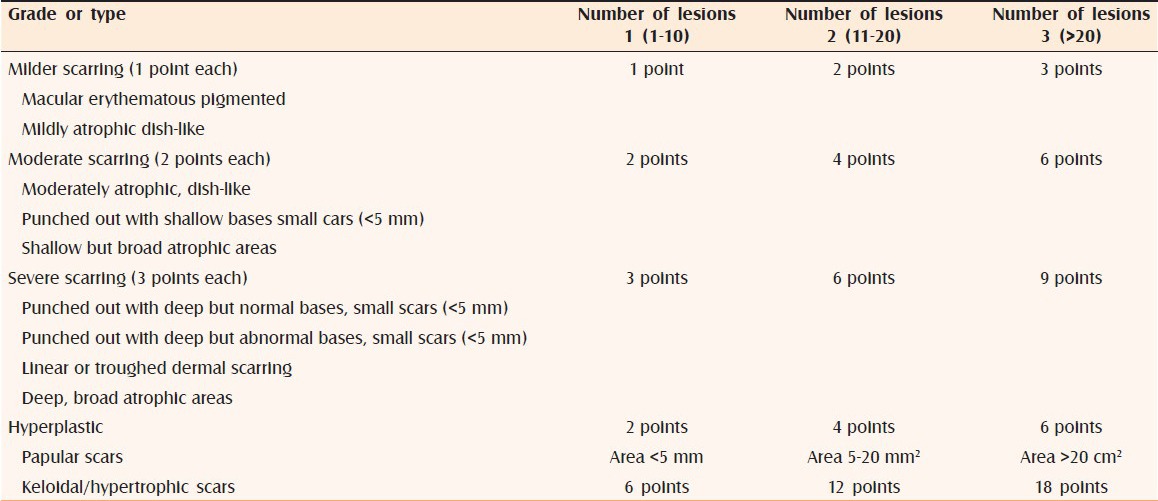
The differences in the acne scar grades before and after the treatment were noted. The improvement status was categorized into a 5-point scale depending on the reduction in the GSGS scores as depicted in Table 2. When difference between the GSGS scores of a patient before the treatment and after RAGA treatment is 0, the improvement status would be categorized as no improvement (when scar grades remained the same). Similarly when difference is 1-5 points then the improvement is categorized as mild, moderate improvement when scar grades reduced between 6 and 10 points, good improvement when scar grades decreased by 11-15 points and very good improvement when scar grades reduced by more than 15 points [Table 2].
Table 2.
Improvement status
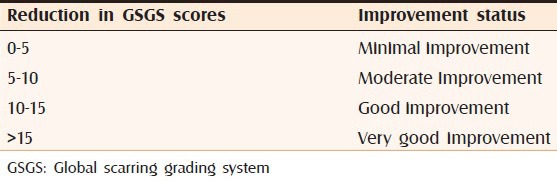
While considering only macular erythematous pigmented lesions, the improvement was categorized according to Table 3 as no improvement (no change in 3 points score), mild improvement (1 point reduction), moderate improvement (2 point reduction in score), and good improvement (3 point reduction in score).
Table 3.
Improvement status of postinflammatory hyperpigmentation
RESULTS
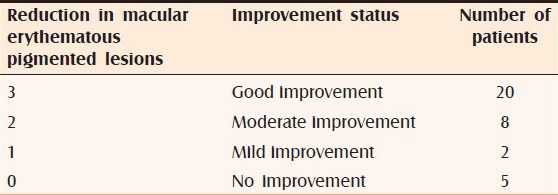
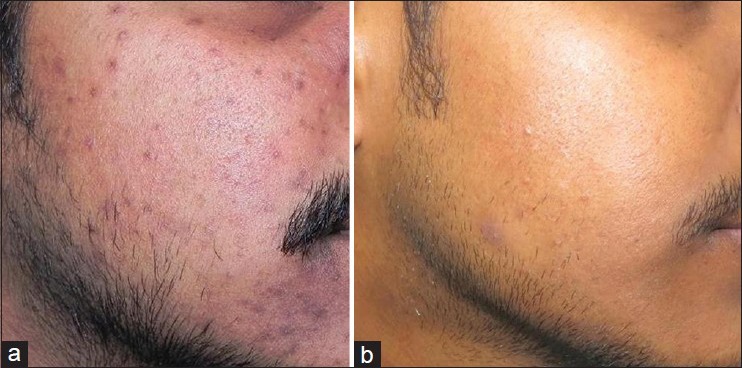
Of the 35 patients, three showed no improvement in scar grades at the end of 12 weeks, while 16 patients demonstrated a mild improvement in their scars that is, the acne scar grades reduced to up to 5 points [Figure 1a and b]. Thirteen patients had moderate improvement in their acne scars [Figure 2a and b], two had good improvement [Figure 3a and b] and one patient demonstrated 21 points reduction in the appearance of his acne scars and had very good improvement [Figure 4a and b]. The overall improvement in acne scars is shown graphically in Figures 5 and 6.
Figure 1.

(a) Acne scars with global scarring grading system score of 6 before starting of retinoic acid and glycolic acid treatment (b) Acne scars after 12 weeks of retinoic acid and glycolic acid treatment showing mild improvement with a global scarring grading system score of 3
Figure 2.

(a) Acne scars with global scarring grading system score of 15 before starting of retinoic acid and glycolic acid treatment (b) Acne scars after 12 weeks of retinoic acid and glycolic acid treatment showing moderate improvement with a global scarring grading system score of 9
Figure 3.

(a) Acne scars with global scarring grading system score of 28 before starting of retinoic acid and glycolic acid treatment (b) Acne scars after 12 weeks of retinoic acid and glycolic acid treatment showing good improvement with a global scarring grading system score of 17
Figure 4.
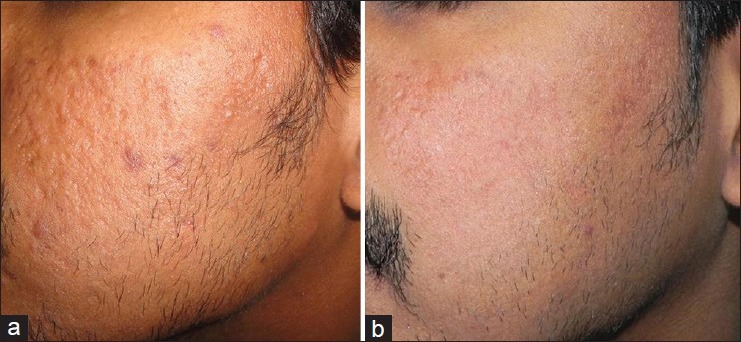
(a) Acne scars with global scarring grading system score of 37 before starting RAGA treatment (b) Acne scars showing very good improvement with global scarring grading system score of 16
Figure 5.
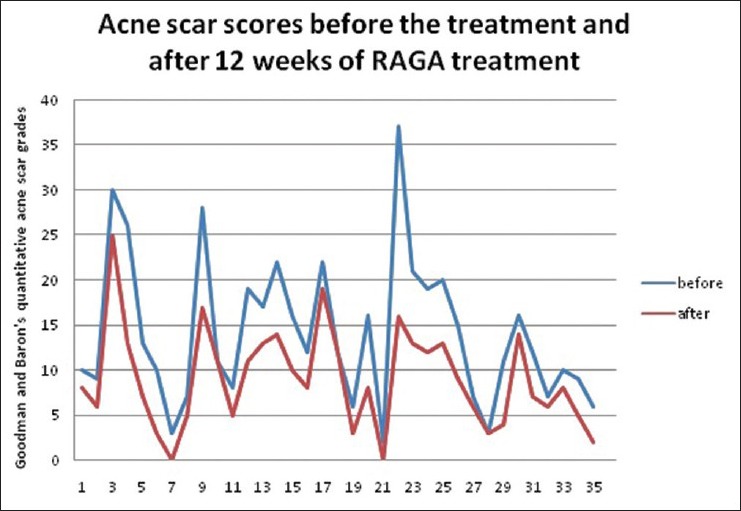
Line graph depicting the acne scar grades before starting retinoic acid and glycolic acid (RAGA) treatment (blue) and after 12 weeks of RAGA treatment (red)
Figure 6.
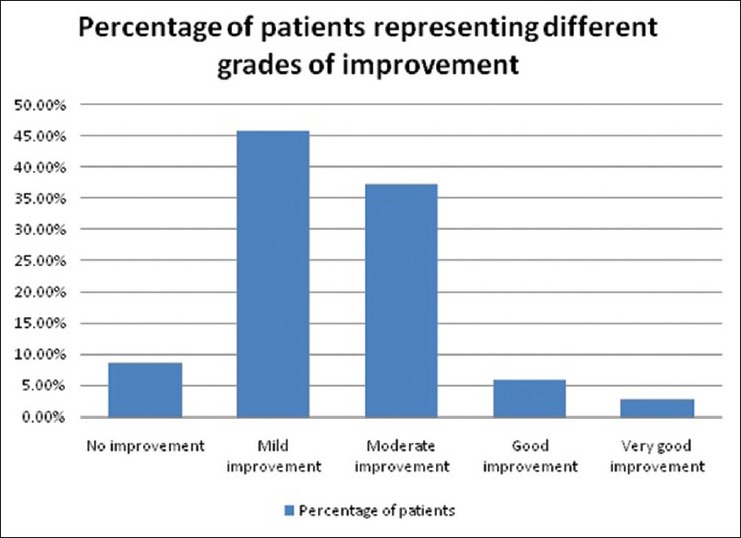
Bar graph representing the number of patients with different improvement grades on taking retinoic acid and glycolic acid treatment on acne scars
Among macular pigmentary lesions, 20 patients showed a 3-point reduction in macular lesions [Figure 7a and 7b], while eight of them had a reduction of 2 points and 2 patients showed a reduction of 1 point. Overall 85.71% of the patients had an improvement in the appearance of their pigmented macules. The improvement is depicted in Figure 8 and Table 3. None of the patients complained of erythema or burning.
Figure 7.
(a) Picture showing postinflammatory hyperpigmentation as a sequelae to acne before starting retinoic acid and glycolic acid treatment (b) Photograph showing 3 points improvement in postinflammatory hyperpigmentation
Figure 8.
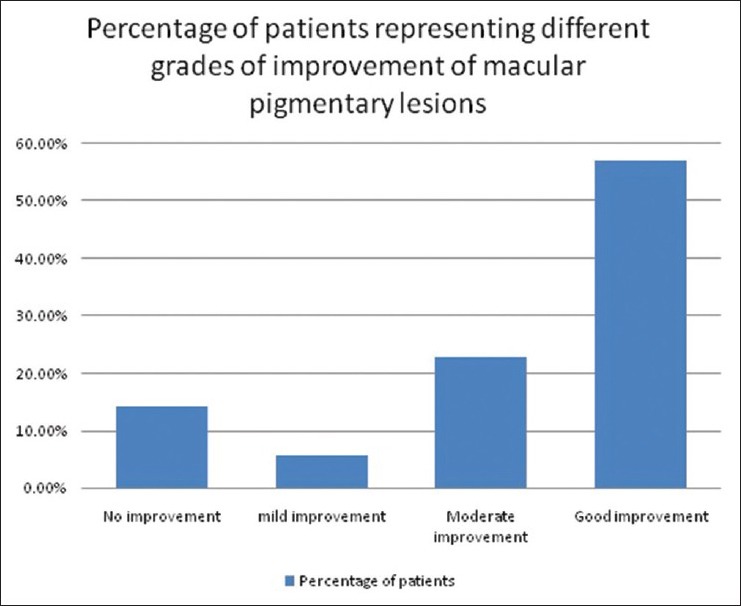
Graphical representation of the percentage of patients with different grades of improvement of macular pigmentary lesions
DISCUSSION
On an average 80-90% of people with acne scars have atrophic scars associated with a loss of collagen compared to a minority who show hypertrophic scars and keloids.[2] Scars originate at the site of tissue injury (during healing of active acne) and the wound healing process progresses through three stages: (1) inflammation; (2) granulation and tissue formation; and (3) matrix remodeling.
During inflammation, vasoconstriction for homeostasis results in blanching. After the blood flow has been stopped, vasodilatation and resultant erythema replace vasoconstriction. Melanogenesis may also be stimulated. This step plays an important role in the development of postacne erythema and hyperpigmentation.
During granulation and tissue formation stage the damaged tissues are repaired and new capillaries are formed. New production of collagen by fibroblasts begins approximately 3-5 days after the wound is created.
The matrix remodeling stage is associated with production of enzymes, by fibroblasts and keratinocytes, that determine the architecture of the extracellular matrix metalloproteinases (MMPs) and tissue inhibitors of MMPs. This results in an imbalance in the ratio of MMPs to tissue inhibitors of MMPs leading to the development of atrophic or hypertrophic scars. Inadequate response results in diminished deposition of collagen and formation of an atrophic scar while, if the healing response is exuberant, a raised nodule of fibrotic tissue forms hypertrophic scars.[2,10]
Topical retinoids such as tretinoin have been shown to decrease the synthesis of MMPs and increase dermal procollagen and collagen synthesis and hence may provide some benefits in preventing scar development and potentially reduce the extent of scar formation that is in progress.[10,11] Schmidt et al. in their study showed that tretinoin-iontophoresis significantly decreased the depth of atrophic scars in 94% of the study subjects.[3]
Topical retinoids improve several features of photoaging that include dispigmentation and wrinkling (fine and coarse). The clinical improvement is accompanied by the reversal of epidermal atrophy and dysplasia along with increased collagen synthesis.[10] This is supported by the study conducted by Schwartz et al. which stated that retinoic acid stimulates collagen synthesis in vivo.[11]
Glycolic acid is a naturally occurring alpha-hydroxy acid and has been well-established in dermatological practice for its cosmetic benefits when used on skin. The mechanism of its effect might be due to epidermal remodeling and accelerated desquamation, which would result in quick pigment dispersion on pigmentary lesions. It also directly reduces melanin formation in melanocytes by tyrosinase inhibition.[12,13]
Erbağci and Akçali in their study titled “biweekly serial GA peels versus long term daily use of topical low-strength GA in the treatment of atrophic acne scars” showed that long term daily use of GA is effective on scars and may be recommended for patients who cannot tolerate the peeling procedure.[14]
Studies conducted by Dreno et al. showed that RALGA combination can efficiently treat acne scars and PIH.[8] However, the combination of RAGA had not yet been studied. Both RA and GA play an active role in scar remodeling, their combination can work synergistically in enhancing and hastening improvement in acne scars.
In our study, we noticed that 91.4% showed improvement in their acne scars and of these 85.71% of patients showed a definite reduction in PIH. All the patients were previously treated for active acne and perhaps the scar formation was still in the early stages. The improvement in the acne scars might be attributed to the increased MMPs and collagen synthesis brought about by retinoic acid and epidermal remodeling and pigment dispersion brought about by GA in the RAGA combination. None of the patients complained of erythema.
Limitations
This retrospective assessment was conducted in a small sample size of patients and there was no interaction with the patients during this assessment. A prospective study of the same with a larger study group is intended in the future.
CONCLUSION
This study shows that the RAGA combination can be considered as a topical treatment for early acne scars including PIH, thereby minimizing the need of procedural treatment for acne scars. However, more studies are required to optimize the ideal concentration of each ingredient, viability of combined formulations in a single tube, frequency of application, and duration of treatment.
Footnotes
Source of Support: NFunded by the CUTIS Academy of Cutaneous Sciences, Bengaluru, Karnataka, India
Conflict of Interest: None declared.
REFERENCES
- 1.Rivera AE. Acne scarring: A review and current treatment modalities. J Am Acad Dermatol. 2008;59:659–76. doi: 10.1016/j.jaad.2008.05.029. [DOI] [PubMed] [Google Scholar]
- 2.Fabbrocini G, Annunziata MC, D’Arco V, De Vita V, Lodi G, Mauriello MC, et al. Acne scars: Pathogenesis, classification and treatment. Dermatol Res Pract 2010. 2010 doi: 10.1155/2010/893080. 893080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmidt JB, Donath P, Hannes J, Perl S, Neumayer R, Reiner A. Tretinoin-iontophoresis in atrophic acne scars. Int J Dermatol. 1999;38:149–53. doi: 10.1046/j.1365-4362.1999.00586.x. [DOI] [PubMed] [Google Scholar]
- 4.Rossi AB, Leyden JJ, Pappert AS, Ramaswamy A, Nkengne A, Ramaswamy R, et al. A pilot methodology study for the photographic assessment of post-inflammatory hyperpigmentation in patients treated with tretinoin. J Eur Acad Dermatol Venereol. 2011;25:398–402. doi: 10.1111/j.1468-3083.2010.03798.x. [DOI] [PubMed] [Google Scholar]
- 5.Van Scott EJ, Yu RJ. Alpha hydroxy acids: Procedures for use in clinical practice. Cutis. 1989;43:222–8. [PubMed] [Google Scholar]
- 6.Van Scott EJ, Yu RJ. Hyperkeratinization, corneocyte cohesion, and alpha hydroxy acids. J Am Acad Dermatol. 1984;11:867–79. doi: 10.1016/s0190-9622(84)80466-1. [DOI] [PubMed] [Google Scholar]
- 7.Goodman GJ, Baron JA. Postacne scarring: A qualitative global scarring grading system. Dermatol Surg. 2006;32:1458–66. doi: 10.1111/j.1524-4725.2006.32354.x. [DOI] [PubMed] [Google Scholar]
- 8.Dreno B, Katsambas A, Pelfini C, Plantier D, Jancovici E, Ribet V, et al. Combined 0.1% retinaldehyde/6% glycolic acid cream in prophylaxis and treatment of acne scarring. Dermatology. 2007;214:260–7. doi: 10.1159/000099593. [DOI] [PubMed] [Google Scholar]
- 9.Goodman GJ, Baron JA. Postacne scarring: A quantitative global scarring grading system. J Cosmet Dermatol. 2006;5:48–52. doi: 10.1111/j.1473-2165.2006.00222.x. [DOI] [PubMed] [Google Scholar]
- 10.Harmer JC, Sami N. Topical retinoids. In: Wolverton SE, editor. Comprehensive Dermatologic Drug Therapy. 2nd ed. Philadelphia, USA: Saunders Elsevier; 2007. pp. 625–41. [Google Scholar]
- 11.Schwartz E, Cruickshank FA, Mezick JA, Kligman LH. Topical all-trans retinoic acid stimulates collagen synthesis in vivo. J Invest Dermatol. 1991;96:975–8. doi: 10.1111/1523-1747.ep12476385. [DOI] [PubMed] [Google Scholar]
- 12.Lewis AB, Radoszycki H. Alpha hydroxy acids. In: Wolverton SE, editor. Comprehensive Dermatologic Drug Therapy. 2nd ed. Philadelphia, USA: Saunders Elsevier; 2007. pp. 731–43. [Google Scholar]
- 13.Sharad J. Glycolic acid peel therapy: A current review. Clin Cosmet Investig Dermatol. 2013;6:281–8. doi: 10.2147/CCID.S34029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erbağci Z, Akçali C. Biweekly serial glycolic acid peels vs. long-term daily use of topical low-strength glycolic acid in the treatment of atrophic acne scars. Int J Dermatol. 2000;39:789–94. doi: 10.1046/j.1365-4362.2000.00076.x. [DOI] [PubMed] [Google Scholar]


