Abstract
Background:
The antiphospholipid antibodies (APLA) are directed against phospholipids and their binding proteins and are frequently found in association with connective tissue disorders. Systemic lupus erythematoses (SLE) with APLA may cause a diagnostic dilemma as there are several manifestations like haemolytic anemia, thrombocytopenia, neurologic manifestations, leg ulcerations, serositis proteinuria which overlap in both these conditions. We conducted a study to find out the association of antiphospholipid antibodies with connective tissue diseases and compared the clinical and laboratory parameters between antiphoshpolipid antibody positive and antiphoshpolipid antibody negative group.
Materials and Methods:
This study was carried out in 102 patients diagnosed with connective tissue diseases. APLA testing was done at baseline and for those positive, the test was repeated after 12 weeks.
Results:
14.7 % of patients with connective tissue diseases tissue had positive antiphoshpolipid antibodies. Positive antiphoshpolipid antibody was detected in 73.3% of patients with SLE group, 13.3% of patients with mixed connective tissue disease (MCTD) and 13.3% of patients with systemic sclerosis. APLA positivity was seen in SLE patients with leg ulcers (87.2%), neurologic manifestation (72.7%), hemolytic anemia (62.3%), thrombocytopenia (72.7%), serositis (27.8%) and proteinuria(19.6%).
Conclusions:
Antiphoshpolipid antibodies should be tested in all patients with connective tissue disease.
Keywords: Antiphospholipid antibodies, antiphospholipid syndrome, connective tissue disease
INTRODUCTION
Antiphospholipid antibody (APLA), which occurs secondary to systemic lupus erythematosus (SLE) or other autoimmune diseases is called secondary antiphospholipid antibody syndrome (APS) and is characterized by arterial and venous thrombosis, recurrent miscarriages in pregnancy, and neurologic manifestations along with the presence of APLA.[1] APLA are directed against phospholipids and their binding proteins.[2] These include antibodies to cardiolipin (aCL), b2 glycoprotein and lupus anticoagulant (LA). APLA are more prevalent in patients with SLE (approximately 50%)[3] with LA constituting 15-34% and aCL, 12-30%.[4] SLE with APLA may cause a diagnostic dilemma as there are several manifestations such as hemolytic anemia, thrombocytopenia, neurologic manifestations, leg ulcerations, and serositis proteinuria that overlap in the two conditions.[5] APLA further complicates SLE by subjecting these patients to vaso-occlusive events resulting in higher morbidity rates. There are only a few studies in India showing the association of APLA with connective tissue diseases.[6] Hence, we conducted a study to find out the association of APLA with connective tissue diseases and compared the clinical and laboratory parameters between APLA positive and APLA negative group.
MATERIALS AND METHODS
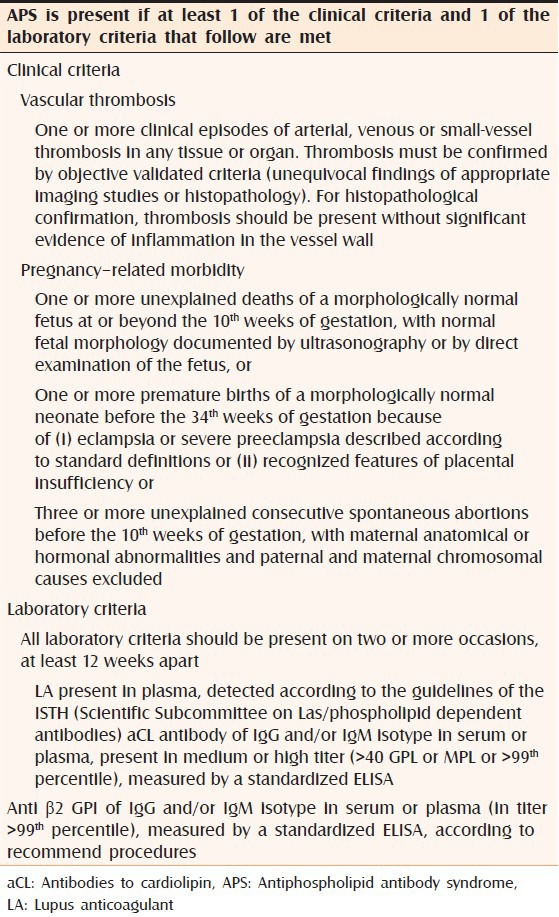
This was a hospital based, descriptive study, which was carried out in 102 patients who were diagnosed with connective tissue diseases such as SLE, mixed connective tissue disease (MCTD), systemic sclerosis and Sjogrens syndrome based on both the clinical criteria and laboratory parameters. After obtaining the Institutional Ethics Committee clearance and written consent from patients, detailed history-taking and examination was performed. All patients were subjected to routine blood tests such as complete hemogram with peripheral smear, renal, liver function tests, urine routine examination, Coomb's test, anti-nuclear antibody and extracted nuclear antigen testing, along with skin biopsy. Chest radiograph, pulmonary function tests, electrocardiogram, echocardiogram, ultrasound and computed tomography brain along with Doppler study of the lower limbs was done in selected patients in whom it was indicated. APLA test was performed at baseline, and for patients who tested positive, it was repeated 12 weeks later according to international consensus statement on an update of the classification criteria for definite APS [Table 1]. The tests for APLA included anticardiolipin antibody and LA. An automated coagulation analyzer based on coagulation tests was used to detect LA and the test was considered positive if the results showed >1.2 s (normal value: <1.2 s). Testing for aCL was done by ELISA method and was considered positive if the results showed >12 u/ml (normal value: upto 12 u/ml)
Table 1.
Revised classification criteria for APS
RESULTS
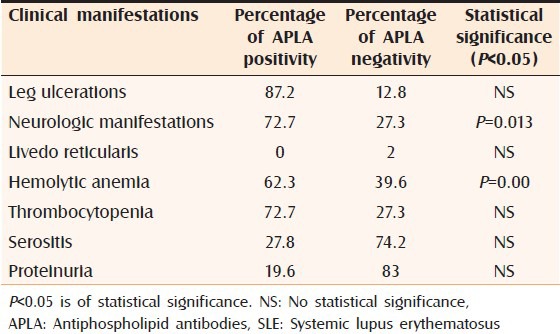
A total of 102 patients were included in the study and 53.9% (55/102) were diagnosed SLE, 18.6% (19/102) were MCTD, 15.7% (16/102) were systemic sclerosis and 11.8% (12/102) were Sjogrens syndrome. 14.7% of patients with connective tissue diseases had positive APLA. 73.3% of APLA positivity was found in the SLE group followed by 13.3% in MCTD and systemic sclerosis each [Table 2]. Percentage of APLA positivity and APLA negativity in patients with leg ulcers, livedo reticularis, neurologic manifestation, hemolytic anemia, thrombocytopenia, serositis and proteinuria, which are overlapping manifestations between APLA and connective tissue disorders, has been tabulated with statistical values [Table 3]. All patients with the above clinical manifestations and positive APLA belonged to the SLE group.
Table 2.
Percentage of positive APLA (aCL and LA) in connective tissue disorders
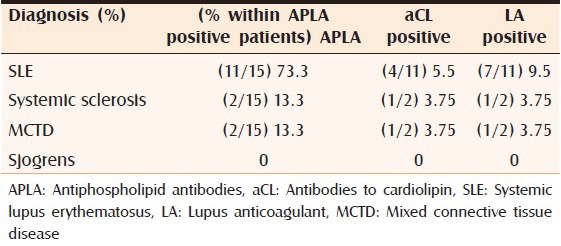
Table 3.
Percentage of APLA positivity and APLA negativity in SLE patients with the following manifestations
DISCUSSION
Antiphospholipid antibodies are directed against cell membrane phospholipids and play an important role in maintaining the vessel wall integrity. There are several manifestations such as hemolytic anemia, thrombocytopenia, neurologic manifestations, leg ulcerations, serositis and proteinuria, which are overlapping clinical manifestations in APLA and connective tissue disorders especially SLE, causing a diagnostic dilemma. In a study by Unikiene and Misiuniene, the incidence of APLA positivity was found to be 30.2% in the SLE group and 29% in the systemic sclerosis group.[7] In our study, 73.3% of patients with positive APLA belonged to the SLE group and 11.8% to the systemic sclerosis group. About 87.2% of SLE patients with leg ulcerations had positive APLA in this study. Although, livedo reticularis is the commonest cutaneous manifestation in SLE with APS as shown in studies published by Krause et al. in 2005 and Cervera et al. in 2002,[8,9] only 2/102 patients in this study showed livedo reticularis and none had positive APLA. Similar to the study by Sanna et al., 50.9% of APLA positive SLE had at least one neurological manifestation and headache was the most common manifestation followed by seizures.[10] In this study, 72.7% of APLA positive SLE patients showed neurologic manifestations such as headache and seizures. Delezé et al. in his study showed that among SLE patients who presented with hemolytic anemia and thrombocytopenia, there was a statistically significant association between thrombocytopenia and APLA positivity.[11] Similarly in our study, 62.3% of SLE patients with hemolytic anemia and 72.7% with thrombocytopenia were APLA positive and statistically significant association was found between hemolytic anemia and SLE. Although, serositis and proteinuria can overlap between APLA and SLE, in our study no statistically significant association was found between these manifestations and APLA positivity.
CONCLUSION
Antiphospholipid antibodies and SLE have several overlapping manifestations and APLA can further complicate SLE resulting in higher morbidity rates. Hence detection of APLA is important for early diagnosis and to prevent life-threatening complications in patients with connective tissue disorders especially SLE.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Harris EN, Baguley E, Asherson RA, Asherson Hughes GR. Clinical and serological features of antiphospholipid syndrome. J Rheumatol. 1987;26:19. [Google Scholar]
- 2.Oosting JD, Derksen RH, Bobbink IW, Hackeng TM, Bouma BN, de Groot PG. Antiphospholipid antibodies directed against a combination of phospholipids with prothrombin, protein C, or protein S: An explanation for their pathogenic mechanism? Blood. 1993;81:2618–25. [PubMed] [Google Scholar]
- 3.Mackworth-Young CG, Loizou S, Walport MJ. Primary antiphospholipid syndrome: Features of patients with raised anticardiolipin antibodies and no other disorder. Ann Rheum Dis. 1989;48:362–7. doi: 10.1136/ard.48.5.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cervera R, Khamashta MA, Font J, Sebastiani GD, Gil A, Lavilla P, et al. Systemic lupus erythematosus: Clinical and immunologic patterns of disease expression in a cohort of 1,000 patients. The European working party on systemic lupus erythematosus. Medicine (Baltimore) 1993;72:113–24. [PubMed] [Google Scholar]
- 5.Furmanczyk A, Komuda-Leszek E, Gadomska W, Windyga J, Durlik M. Catastrophic antiphospholipid syndrome. Pol Arch Med Wewn. 2009;119:427–30. [PubMed] [Google Scholar]
- 6.Gupta R, Thabah MM, Gupta S, Shankar S, Kumar A. Clinical significance of antiphospholipid antibodies in Indian scleroderma patients. Rheumatol Int. 2009;30:277–9. doi: 10.1007/s00296-009-1107-0. [DOI] [PubMed] [Google Scholar]
- 7.Unikiene D, Misiuniene N. Antiphospholipid syndrome in patients with systemic connective tissue diseases. Medicina (Kaunas) 2003;39:454–9. [PubMed] [Google Scholar]
- 8.Krause I, Blank M, Fraser A, Lorber M, Stojanovich L, Rovensky J, et al. The association of thrombocytopenia with systemic manifestations in the antiphospholipid syndrome. Immunobiology. 2005;210:749–54. doi: 10.1016/j.imbio.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Cervera R, Piette JC, Font J, Khamashta MA, Shoenfeld Y, Camps MT, et al. Antiphospholipid syndrome: Clinical and immunologic manifestations and patterns of disease expression in a cohort of 1,000 patients. Arthritis Rheum. 2002;46:1019–27. doi: 10.1002/art.10187. [DOI] [PubMed] [Google Scholar]
- 10.Sanna G, Bertolaccini ML, Cuadrado MJ, Laing H, Khamashta MA, Mathieu A, et al. Neuropsychiatric manifestations in systemic lupus erythematosus: Prevalence and association with antiphospholipid antibodies. J Rheumatol. 2003;30:985–92. [PubMed] [Google Scholar]
- 11.Delezé M, Oria CV, Alarcón-Segovia D. Occurrence of both hemolytic anemia and thrombocytopenic purpura (Evans’ syndrome) in systemic lupus erythematosus. Relationship to antiphospholipid antibodies. J Rheumatol. 1988;15:611–5. [PubMed] [Google Scholar]


