Abstract
Background
The prevalence of chronic diseases such as type 2 diabetes and chronic low back pain is rising. Patient empowerment is a key strategy in the management of chronic diseases. Patient empowerment can be fostered by Web-based interactive health communication applications (IHCAs) that combine health information with decision support, social support, and/or behavioral change support. Tailoring the content and tone of IHCAs to the needs of individual patients might improve their effectiveness.
Objective
The main objective was to test the effectiveness of a Web-based, tailored, fully automated IHCA for patients with type 2 diabetes or chronic low back pain against a standard website with identical content without tailoring (control condition) on patients’ knowledge and empowerment.
Methods
We performed a blinded randomized trial with a parallel design. In the intervention group, the content was delivered in dialogue form, tailored to relevant patient characteristics. In the control group, the sections of the text were presented in a content tree without any tailoring. Participants were recruited online and offline and were blinded to their group assignments. Measurements were taken at baseline (t0), directly after the first visit (t1), and at 3-month follow-up (t2). The primary hypothesis was that the tailored IHCA would have larger effects on knowledge and patient empowerment (primary outcomes) than the control website. The secondary outcomes were decisional conflict and preparation for decision making. All measurements were conducted by online self-report questionnaires. Intention-to-treat (ITT) and available cases (AC) analyses were performed for all outcomes.
Results
A total of 561 users agreed to participate in the study. Of these, 179 (31.9%) had type 2 diabetes and 382 (68.1%) had chronic low back pain. Usage was significantly higher in the tailored system (mean 51.2 minutes) than in the control system (mean 37.6 minutes; P<.001). Three months after system use, 52.4% of the sample was retained. There was no significant intervention effect in the ITT analysis. In the AC analysis, participants using the tailored system displayed significantly more knowledge at t1 (P=.02) and more emotional well-being (subscale of empowerment) at t2 (P=.009). The estimated mean difference between the groups was 3.9 (95% CI 0.5-7.3) points for knowledge and 25.4 (95% CI 6.3-44.5) points for emotional well-being on a 0-100 points scale.
Conclusions
The primary analysis did not support the study hypothesis. However, content tailoring and interactivity may increase knowledge and reduce health-related negative effects in persons who use IHCAs. There were no main effects of the intervention on other dimensions of patient empowerment or decision-related outcomes. This might be due to our tailored IHCA being, at its core, an educational intervention offering health information in a personalized, empathic fashion that merely additionally provides decision support. Tailoring and interactivity may not make a difference with regard to these outcomes.
Trial Registration
International Clinical Trials Registry: DRKS00003322; http://apps.who.int/trialsearch/Trial2.aspx?TrialID=DRKS00003322 (Archived by WebCite at http://www.webcitation.org/6WPO0lJwE).
Keywords: Type 2 diabetes mellitus, back pain, randomized controlled trial, health communication, Internet
Introduction
Long-term conditions such as type 2 diabetes (T2D) and chronic low back pain (CLBP) are chronic diseases with high and still rising prevalence [1,2], which cause a significant burden on individuals as well as negative social and economic effects [3-8]. Thus, there is a strong need for cost-effective ways to improve the care of these long-term conditions.
To improve care of long-term conditions, patients, practitioners, scientists, and politicians have called for a greater empowerment of patients in the management of their chronic diseases [9]. Patient empowerment can be observed as a motivational construct reflecting the ability to positively influence self-management and health behavior. The main aspects of patient empowerment are knowledge of the disease, its course and treatment options, the ability to be involved in making medical decisions and relate to health care providers [10], and to manage one’s health behavior and treatment regimens [11,12]. Schulz and Nakamoto additionally stressed that these factors must be accompanied by a volitional component to better predict changes in individuals’ behavior [13]. The most popular definition of patient empowerment is probably that of Funnell et al [14] who defined patient empowerment as “the discovery and development of one’s inherent capacity to be responsible for one’s own life. People are empowered when they have sufficient knowledge to make rational decisions, sufficient control, and resources to implement their decisions, and sufficient experience to evaluate the effectiveness of their decisions”. Patient empowerment and health-related knowledge can be considered as predictors of improved self-management and health outcomes [15,16].
In times of rapidly growing Internet adoption, the Web holds the opportunity to deliver health information [17] and self-management support [18] to large numbers of participants at a comparatively low cost and at the preferred time, place, and learning speed of the individuals. Existing systematic reviews and meta-analyses of Internet interventions in somatic diseases aimed at improving lifestyles (smoking, alcohol consumption, diet, physical exercise) show promising effects on either health- or cost-related outcome measures [19]. More specifically, recent reviews and studies on Internet interventions for adults with T2D [20,21] and CLBP [22-24] also found effects on knowledge, self-efficacy, health behavioral changes, and clinical outcomes. Evidence for Internet interventions can also be found with regard to effects on more proximal outcomes such as patient empowerment [22,25,26] or specific antecedents and mediators of patient empowerment [27].
A specific application of Internet interventions combines health information with at least one other type of support, for example, social support, decision support, or behavior change support: interactive health communication applications (IHCAs). These Internet interventions are expected to improve the knowledge, involvement in decision making, motivation, and self-efficacy of users, resulting in enhanced patient empowerment [28]. This improved empowerment can then enable users to initiate changes in health behaviors, which might result in improved clinical outcomes [28,29]. A Cochrane review found that IHCAs could have positive effects on knowledge, self-efficacy, and behavioral and clinical outcomes. However, the authors demanded more evidence regarding the most suitable application and delivery approaches of IHCAs and the effects of IHCAs for different chronic diseases [28].
Still, the effectiveness of those online applications is limited by high attrition rates [30,31], and users often visit a health intervention website only once [32-34]. A major body of evidence suggests that the effect of online interventions increases with the dose (longer stays, repeated website visits, total contact hours) [35,36], and the effectiveness is maximized if patients intensively work with the information offered [37-39] and return for repeated visits [40,41].
Computer tailoring strategies such as the individualization and personalization of information, as well as an interactive presentation, have been found to effectively increase the exposure to [42] and effectiveness of Web-delivered interventions [43,44]. However, these previous studies predominantly focused on tailoring in health behavior change interventions, with great variability in how the tailoring was carried out. In addition to the question of which elements of the intervention work, one remaining challenge of research with regard to Internet interventions is finding out which delivery methods (interactivity, tailoring, individualization) are effective [45]. Therefore, evidence is especially needed with regard to disease-specific tailoring and individualization strategies in IHCAs for T2D and CLBP, focusing on more proximal outcomes such as health-related empowerment and knowledge.
In this randomized controlled trial, we compared a tailored IHCA presenting information on T2D and CLBP, self-management education, and decision support to a website presenting the same information in a content tree without tailoring. The primary hypothesis was that the tailored and individualized delivery format has a greater effect on knowledge and patient empowerment than the control website. The secondary hypothesis was that users, when facing a health decision, experience less decisional conflict and feel better prepared for the consultation after using the tailored rather than the control website. This paper reports on the trial using the two guidelines that were published in 2011 on designing and reporting Internet intervention research [18,46].
Methods
Study Design
We performed a blinded two-armed randomized controlled trial with a parallel design. Measurements were scheduled immediately before the first use of the system (t1), immediately after use (t2), and at 3-months follow-up (t3). Knowledge (primary outcome) and decisional conflict and preparation for decision making (secondary outcomes) were assessed immediately after the first visit. Patient empowerment (primary outcome) was assessed 3 months after the first visit. All measurements were online self-assessment questionnaires. The study design and procedures have been published in two study protocols [47,48]. There were no important changes to the study design, methods, or trial outcomes after trial commencement. Data collection took place between August 2012 and April 2013.
Study Population
The eligibility criteria were age ≥18 years, access to the Internet, sufficient computer/Internet literacy, and a self-reported diagnosis of T2D or CLBP. CLBP was defined as pain in the lower back almost every day for more than 12 weeks [49].
Recruitment
In general, based on the Cochrane review by Murray et al [28], we expected a small effect (Cohen’s d=0.2) of the IHCA. Based on the review by van Vugt et al [20] for diabetes, and based on a similar previous study [23] for patients with back pain, we did expect that the tailored intervention would perform better (d=0.2) than the control on the primary outcome knowledge for both patient groups. Based on the meta-analysis by Samoocha et al [25], we also expected a small effect with regard to the primary outcome empowerment for patients with T2D and CLBP. To detect a small effect with an alpha of .05 and a power of .80 (one-tailed t test), a sample size of 310 (155 per group) was required. Due to the experiences of other Internet trials [40] and the effect of incentives [50], we expected a dropout rate of 20% between registration and immediately after the first visit. Thus, we aimed to include a sample of 414 at baseline. Because we were not aware of differences in the dropout rates between T2D and CLBP patients, we calculated with the same expected dropout rate for both groups.
Recruitment took place using a number of pathways. Two pension funds and six health insurance companies were contacted to request whether they were interested in informing their insurants about the study (eg, via their website, magazine, or newsletter). Three outpatient treatment networks (in which mainly primary care and specialized practices are organized), 15 diabetology practices, 15 practices specialized in CLBP, 87 primary care practices, six rehabilitation centers and hospitals, seven patient associations, and 192 self-help groups were contacted and asked whether they were interested in displaying flyers. Additionally, information on the study and a link to it were disseminated via the mailing list of a population-representative online panel of the University of Münster. Information on the study was also available on the study website. Information and links were placed on the website of the University Medical Centre Hamburg-Eppendorf, as well as on websites that are structurally connected to the work group, one external private diabetes information website, and the website of a doctors’ and therapists’ CLBP network. An article was also published in a regional newspaper (Hamburger Abendblatt).
Study Procedures
In this purely Web-based trial without any face-to-face component, every person meeting the eligibility criteria could register for the study on the study website (open survey on a site created exclusively for the study) by providing a unique email address and choosing a password for login. After providing online informed consent and completing the pre-assessment (T2D: eligibility criteria, demographic data, time since diagnosis, treatment; CLBP: eligibility criteria, demographic data, chronic pain grade [51]), the participants were randomly assigned to the tailored system or the control system with the content tree. The informed consent was the first page entered after login. The participants were told the approximate length of time of the survey, where data were stored and for how long, who the investigators were, and the purpose of the study. Consent was provided via checkbox. Pre-assessments were completed after providing informed consent and before randomization. Only users who had filled in the pre-assessment were allowed to use the intervention (mandatory survey). In the control condition, tailoring variables (T2D: diabetes self-care [52], barriers to insulin treatment (BIT) [53], knowledge; CLBP: coping style [54], knowledge) were assessed immediately after randomization and before the intervention. In the tailored version, coping style (CLBP) was also assessed immediately after randomization and before the intervention, whereas knowledge, diabetes self-care, and barriers to insulin treatment were assessed throughout the intervention. The reason for this is that when tailoring to coping style, the user’s coping type is determined in the beginning. At different places throughout the intervention, messages are tailored to this pre-assessed type. However, when tailoring to knowledge, diabetes self-care, and barriers to insulin treatment, there is no typology. Instead, individual items are assessed at different places throughout the intervention, and at that assessment point, one single message is tailored to the user’s answer to the single item. Immediately after their first visit to the tailored IHCA or the control website, all participants were asked to fill in the post-assessment.
All participants received an email 3 months after their first visit asking them to fill in the online follow-up questionnaire. Participants were reminded by email twice, at 2 weeks and 4 weeks after the first email. Because non-monetary incentives have been shown to reduce attrition in online trials [50,55], participants who had answered all questionnaires received a €10 Amazon gift voucher. The voucher code was sent to them by email at the end of the study.
Participants were free to use the intervention as often and as long as they wished. Between the post and follow-up assessments, no prompts or reminders were used. No recommendations were provided regarding the duration or frequency of use, but the IHCA was designed to be used in one “go”. Consequently, there were no prompts to use the intervention. No payment was required. Information on the frequency and duration of usage was gathered via server registrations. Usage data, data from the self-assessment questionnaires, and personal data such as name and email address were saved separately. Data were pseudonymized. After data collection, personal data were deleted. If participants withdrew their informed consent to study participation, their data were immediately erased. All data will be erased 5 years after the end of the study.
The study was approved by the Hamburg Medical Chamber ethics committee.
Treatment Allocation
The informed consent outlined that participants would be randomly assigned in consecutive order (50:50) to one of two presentation formats holding the same content. The random allocation (simple randomization) of the participants was automatically performed by the software program, which also provided the website and triggered automatic emails to participants. This centralized, software-driven, computerized, simple randomization procedure to the intervention or control group assured the concealment of allocation, so that randomization could not be subverted by the team of researchers. The two formats were not further elucidated, so participants did not know whether they were in the intervention or control group.
Description of the Intervention and Control Conditions
The tailored IHCA is designed as a stand-alone intervention that complements usual care. The T2D content of both the tailored IHCA and the control website covered basic information on diabetes (pathophysiology, epidemiology, subtypes, symptoms) and its sequelae (neuropathy, nephropathy, retinopathy, heart and vessel problems, sexual dysfunction, and depression), information on health behavior and lifestyle changes, and treatment options (see Table 1). The CLBP content covered essential information on CLBP (physiology of pain, acute vs chronic pain, chronification, epidemiology, psychological aspects, coping and pain management) and related psychological problems (depression, anxiety), diagnostic procedures, and treatment options (pharmacological and non-pharmacological; see Table 1). The look of the website (colors, font, figures, and pictures) was identical in both conditions. After registration, each participant received a password via email with which they could log onto the system as often as they wished.
Table 1.
Overview over the IHCA contents.
| Type 2 diabetes | Chronic low back pain |
| 1. Introduction: What is this website? | 1. Introduction: What is this website? |
| 1.1. Where does the information on this site come from? | 1.1. Where does the information on this site come from? |
| 2. Basics | 2. CLBP Basics |
| 2.1. Different diabetes types | 2.1. Physiological basics: back, spine, and intervertebral discs |
| 2.2. How do I know I have type 2 diabetes? | 2.2. What exactly is pain? |
| 2.3. What causes type 2 diabetes? | 2.3. What is the difference between acute and chronic pain? |
| 2.4. How many people live with type 2 diabetes? | 2.4. Why does the pain stay when the physical injury heals? |
| 2.5. How is type 2 diabetes diagnosed? | 2.5. How many people live with CLBP? |
| 2.6. Diabetes ABCs | 2.6. Managing CLBP in everyday life |
| 2.7. Blood sugar control | 3. How is CLBP diagnosed? |
| 3. How is type 2 diabetes treated? | 3.1. How much diagnostics makes sense and at which point? |
| 3.1. What are the goals of diabetes treatment? | 3.2. Diagnostic options |
| 3.2. What can you do to treat your diabetes? | 4. How is CLBP treated? |
| 3.3. When should you consider taking pills? | 4.1. How much treatment makes sense and at which point? |
| 3.4. Insulin treatment | 4.2. What is the natural, untreated course of CLBP? |
| 3.5. Summary and overview of the treatment options | 5. Are there accompanying conditions or sequelae of CLBP? |
| 4. Acute complications and sequelae | 6. Treatment options |
| 4.1. Which acute complications can occur? | 6.1. How do I recognize good treatment? |
| 4.2. Which sequelae can occur? | 7. Summary |
| 5. Additional information and literature | 8. Additional information and literature |
| 5.1. Associations and self-help | 8.1. Associations and self-help |
| 5.2. Websites | 8.2. Websites |
| 5.3. Journals | 8.3. Journals |
| 5.4. Books | 8.4. Books |
| 6. Glossary | 9. Glossary |
| 7. Legal notice | 10. Legal notice |
| 8. References | 11. References |
Tailored Condition
In the tailored condition, the delivery format was a dialogue-based, tunneled design tailoring the content and tone of the dialogue to relevant patient characteristics. It was developed based on two preliminary studies exploring the quality of existing websites [56] and assessing patient needs [57]. A tunneled design, in which the user is guided through the content, has been found to increase website use and knowledge gained from a website more than a design with more user control [58]. Still, it might annoy the user and evoke resistance [59]. Consequently, we decided to give the user some control over the path they take through the dialogue: at the end of each text passage, the user chose one of at least three reply options. These options always included at least one answer that expressed disagreement or doubt. The user then received a tailored answer that mirrored what the user had said, respected disagreement, conveyed esteem, and empathy and built an individualized bridge to the next content block. It was not possible to skip a whole content block (meaning the subheadings in Table 1), but it was possible to view the content in more or less detail.
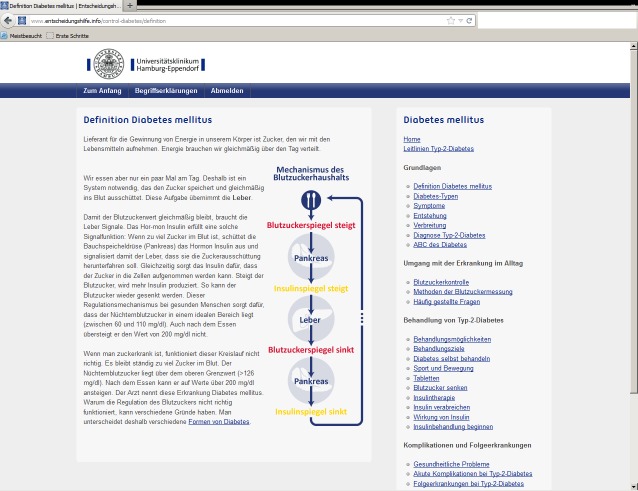
Tailoring was performed using the following characteristics for diabetes patients: current T2D knowledge and preferred level of detail, attitudes toward self-care, and, if insulin treatment was a relevant topic, psychological barriers to it. The questionnaires that assessed patient characteristics were presented during the dialogue. At the beginning of the respective section (eg, diabetic foot), the participant was asked about their knowledge or attitude toward the topic, and the following section was then modified according to their answer. Figure 1 shows such a dialogue window.
Figure 1.
Dialogue window.
Diabetes Section and its Tailoring
Users’ attitudes toward self-care were assessed with items that we adapted from the Summary of Diabetes Self-care Activities Measure (SDSCA) [52] to match the respective content section (see Table 2). Users were asked how important a certain self-care activity or piece of advice is for them. Every item had three reply options: “important or very important”, “a little important”, and “not important”. The goal and techniques were inspired by Motivational Interviewing, a counseling method for addressing ambivalence about change [60].
Table 2.
Example of self-care tailoring: Response to “If you feel thirsty and urinate frequently, it usually means your blood sugar is…”.
| Response options | Reply |
| High (correct answer) | That’s correct! If you want to learn more about what happens in the body and how you know that you have type 2 diabetes, you can go into more detail. Otherwise you can proceed to the next question.
|
| Low (wrong answer) | No, that’s not correct. Actually, it’s the other way around: When you have type 2 diabetes, there is too much sugar in your blood. Unfortunately, you don’t realize it in the beginning. However, there are warning signs. The most important signs are […] |
| I don’t know | That’s ok, [name], that’s what we are here for: to learn, for example, what high blood sugar does to your body. When you have type 2 diabetes, there is too much sugar in your blood. Unfortunately, you don’t realize it in the beginning. However, there are warning signs. The most important signs are […] |
For example, if a user attached great importance to the self-care behavior in question, this behavior was reinforced, positive consequences of the self-care behavior were stressed, and/or ideas were provided on how to keep up motivation. If a user found the self-care behavior in question “a little important”, an understanding of the users’ ambivalence was expressed, and the importance the user attached to the self-care behavior (little as it might be) was stressed and reinforced. Finally, if a user rated the self-care behavior as not important, the autonomy expressed in this answer was respected in order not to elicit resistance. Table 2 shows an example of self-care tailoring.
Psychological barriers to insulin treatment were assessed using the Barriers to Insulin Treatment (BIT) questionnaire [53]. The BIT assesses the following expectations regarding insulin treatment: fear of injection and self-testing; expectations regarding positive insulin-related outcomes; expected hardships from insulin treatment; stigmatization by insulin injections; and fear of hypoglycemia. There are two or three items per subscale. In every item, a certain hope or fear with respect to insulin treatment is expressed (eg, “I am afraid of the pain when injecting insulin”). The user is asked to rate their agreement on a scale from 1 (completely disagree) to 10 (completely agree). A score from 1-10 can be calculated for each subscale. A validating and understanding (if a fear was expressed) or reinforcing (if a hope was expressed) answer was given. If there was a sign of fear (score >1), further information on the topic in question was provided.
Chronic Low Back Pain Section and its Tailoring
For CLBP, the concepts of coping style according to the avoidance endurance model (AEM) [37] and current CLBP knowledge and preferred level of detail were used for tailoring the provided information to the individual preferences of the users. The individual coping style was assessed using a questionnaire, which was presented before starting the dialogue. There are four AEM subtypes: the “depressed endurer”, which is high endurance coping (EC) and high depressiveness (D), the “happy endurer”, which is high EC and low D, the “depressed avoider”, which means low EC and high D, and the “adaptive coper”, which means low EC and low D (see Table 3). During the virtual conversation, the content, tone, and messages were tailored to the coping style of the individual user. The items that assess CLBP knowledge were presented during the dialogue. In the beginning of the respective section (eg, physiological basics), the user was asked about their level of knowledge on this subject. Depending on the response, the subsequent section was accordingly amended.
Table 3.
Example of tailoring to coping style (CLBP).
| Coping type | Adaptive coper | Happy endurer | Depressed endurer | Depressed avoider |
| Description of coping style | You go about your pain in a matter-of-fact manner. You know that on one hand, there is no serious disease behind it but that on the other hand, it can signal to you physical strain. You are good at taking short breaks at the right time to keep up your daily routine – maybe temporarily a little slower than usual. | You tend to keep going in your daily routine even if the pain is strong. This is, on one hand, a personal strength. However, at the same time, you run the risk of actually straining your muscles, ligaments, joints, and intervertebral discs. | You are a multi-tasker. Saying “No” to someone or not getting things done is hard on you. To meet requirements and get things done, you push yourself to your limits and beyond. Often, you don’t listen to your body before it is overstrained. | You are unsettled by your pain. You are worried that there might be a serious disease behind it, and / or you avoid activities that might increase the pain. |
| Take home message | Keep on like that! Make exercise part of your routine if you haven´t yet. Choose something fun and back-friendly. If you strengthen your muscles and stick to your relaxing breaks, the pain should soon vanish. | Even if it’s hard, try to pay more attention to your pain and take breaks early enough. Keep working, do things that are pleasant and fun, and keep moving – but remember to pause when you might need to! | Reconsider what you are asking from yourself: do you really have to demand so much? Maybe there are times when it is possible to leave something undone, to do it o.k. instead of perfectly, or to ask for assistance. These things are closely related to your pain. | Pain is unpleasant but not dangerous. Don’t let it suffocate you. Expand your limits step by step, and make pleasant activities a part of your everyday life. |
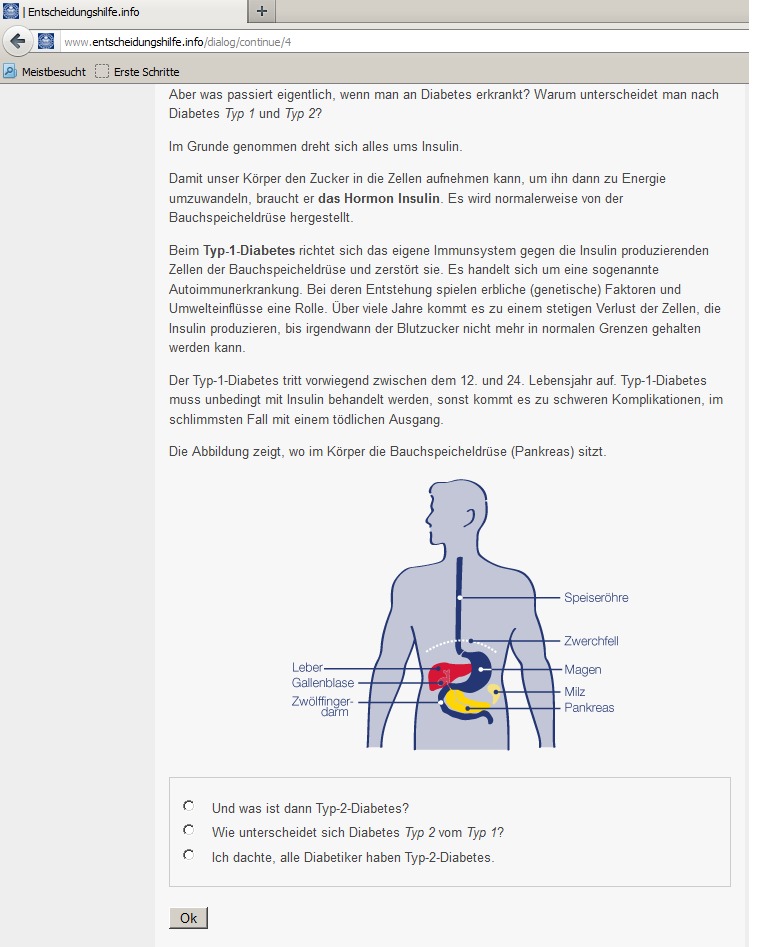
Control Condition
On the control website, the content was not tailored and was not presented in a dialogue format. In contrast to the tailored, interactive version, the control website was not tunneled, and there was no guidance through the content. On the right side of each page, a content tree displayed a menu of all content sections that the participant could click on to get to the content of interest (see Figure 2). On both the intervention and control websites, the institutional affiliation of the University Medical Center Hamburg-Eppendorf was displayed at the top of each webpage.
Figure 2.
Control window.
Potential Risks for Participants
Research focusing on the negative effects of Internet interventions is scarce. One recent study on the side effects of Internet interventions for social anxiety disorder found that 14% of participants experienced negative effects, of which the most frequent was the emergence of new symptoms [61]. Concerning long-term conditions like T2D or CLBP, possible negative effects on cognitive or emotional variables such as self-efficacy or anxiety should be considered, because of high demands concerning self-management tasks or fear-inducing information. However, several recent reviews did not find any contraindications or negative side effects of IHCAs [21,28].
Intervention Development and Trial Design
The development process was user-oriented, evidence-based, and peer-reviewed. Two preliminary studies were conducted informing intervention development. To find out which topics are relevant to patients with T2D or CLBP, we performed a needs assessment with two steps. First, we conducted semistructured interviews with 12 physicians (T2D: 7 internists, 2 of whom were specialized in diabetology; CLBP: 5 physicians specialized in orthopedics) and 19 patients (10 with T2D, 9 with CLBP). In the second step, a self-assessment questionnaire was developed based on the main results of the interviews, and it was administered to a new and larger patient sample (T2D: N=178, CLBP: N=117). The needs assessment for T2D is described in more detail elsewhere [57]. We then conducted a cross-sectional study on the information and support available online, evaluating the formal quality, usability, and presence and quality of decision support of websites for CLBP or T2D. The results on T2D have been published elsewhere [56]. To ensure that the information is evidence-based, selected treatment guidelines were used as primary sources. Based on review articles [62,63] and up-to-dateness, the British [64] and the American [65] T2D guidelines were chosen. For CLBP, certain guidelines [49,66,67] and Cochrane reviews [68-73] were chosen. The theoretical foundations and the development of the T2D IHCA are described in more detail elsewhere [74]. Programming and graphic design were performed by the Gaia AG, a subcontractor specializing in Web-based health interventions. The intervention was not changed during the trial.
Outcomes Assessment
The primary outcomes were knowledge (assessed immediately after the first visit) and patient empowerment (assessed at 3-months follow-up).
T2D knowledge was assessed immediately after the first visit with 16 items, and CLBP knowledge was assessed with 29 items. The items were developed to map the content covered in the sections of the tailored IHCA and could be answered with true/false/I don’t know.
For the context of long-term conditions, patient empowerment was defined as a feeling of confidence and the ability to manage the challenges resulting from the chronic disease [10]. An empowered patient can better understand and participate in care processes, use resources, and measures to reduce negative emotions, and enhance strategies to cope with chronic disease. Consequently, patient empowerment includes intrapersonal and behavioral dimensions [75]. However, at the time this study started, we could not identify a generic, adequately validated questionnaire of empowerment for general use in long-term conditions as reported by a systematic review [76]. Patient empowerment was therefore measured with the Health Education Impact Questionnaire (heiQ) [77,78]. The heiQ includes 42 items and eight dimensions: Positive and Active Engagement in Life, Health Directed Behavior, Skill and Technique Acquisition, Constructive Attitudes and Approaches, Self-Monitoring and Insight, Health Service Navigation, Social Integration and Support, and Emotional Well-being. Schuler et al [79] translated the questionnaire into German and evaluated its psychometric properties (Raykov’s Composite Reliability Coefficient, factorial and concurrent validity). They were able to replicate the structure of the eight scales and found the questionnaire to be a reliable and valid measure. We removed Social Integration and Support from our testing battery because we did not expect an effect of our IHCA on that dimension. Although these 7 heiQ scales may not comprehensively measure the multidimensional construct of empowerment given, the selected scales do cover the intrapersonal and behavioral dimensions that are part of health-related empowerment. Patient empowerment was assessed only at 3-months follow-up because we expected changes on the heiQ to take more time.
The secondary outcomes were decisional conflict and preparation for decision making, assessed immediately after the first visit. Decisional conflict was assessed with the Decisional Conflict Scale (DCS) by O’Connor [80,81]. This questionnaire measures personal perceptions of uncertainty in choosing options, modifiable factors contributing to uncertainty such as feeling uninformed, unclear about personal values, and unsupported in decision making, and effective decision making such as feeling that the choice is informed, values-based, and likely to be implemented and expressing satisfaction with the choice. Reliability is good, with a Cronbach alpha between .78 and .92 [80]. The discriminant validity is acceptable. Preparation for decision making was measured with the Preparation for Decision Making Scale (PDMS).
Preparation for decision making was measured with the Preparation for Decision Making Scale (PDMS) [82,83]. This 11-item scale assesses a patient’s or participant’s perception of how useful a decision aid or decision support intervention was in preparing them to communicate with their practitioner in making a health decision. The reliability is very good, ranging from alpha=.92 to alpha=.94. Both questionnaires were offered only to those participants who had indicated that they were facing a health decision concerning their T2D or CLBP.
To avoid missing data, all questionnaires included validation checks that alerted participants when their answers were implausible or when items were skipped. Usage data were assessed via log files. Before going online, the usability and technical functionality of the electronic questionnaire was tested by members of the research team. All outcomes were self-assessed through online questionnaires. The questionnaires were not validated for online use.
Statistical Analysis
Baseline Data
Data on sample characteristics were analyzed using t tests (for metric data) and chi-square tests (for categorical data) to test for differences between treatment groups. A dropout analysis was performed to test for possible attrition bias. The effects of the intervention (tailored vs control condition), disease (T2D vs CLBP), gender, age, education, family status, and employment status on attrition were evaluated using t tests (for metric data) and chi-square tests (for categorical data).
Intention-to-Treat Analysis
To evaluate the effectiveness of the tailored IHCA, multiple linear regression analyses were performed using the intervention, the disease, and their interaction term as dummy-coded predictors. Intention-to-treat (ITT) and available cases (AC) analyses were performed for all outcomes. The ITT approach pooled 10 analyses, estimating missing values by a multiple regression approach using all outcomes, demographic data, and diseases but not intervention information for multiple data imputation (MI). In the primary ITT analysis, a corrected level of significance was used for testing the eight primary outcomes (Bonferroni adjustment); thus, the results with a type I error rate of P<.001 were considered statistically significant. For secondary outcomes, P<.05 was used.
Sensitivity Analysis (Available Cases)
The AC analysis included all of the available participants providing valid data on t1 and/or t2. In both analyses, estimated marginal means with standard errors for both the tailored and control conditions were calculated with analysis of variance (ANOVA). Additionally, these parameters were also retained for subgroups stratified by condition. In all AC analyses, results with a type I error rate of P<.05 were considered statistically significant. All analyses were performed using SPSS 18.0.
Results
Participant Flow
A total of 561 users agreed to participate in the study. Of these, 179 (31.9%) had T2D, and 382 (68.1%) had CLBP. Analyzable data (availability of at least basic demographic information such as age and gender) at t0 were available from 551 users. For data analysis at t1, data for 360 participants was available (availability of data for at least one of the outcomes of t1). Three months after system use, the questionnaires of 295 participants contained data on at least one of the three outcomes at t2 and could thus be used for analyses (Figure 3). There were no significant differences with regard to gender, age, family status, educational level, or working status between those participants who provided all questionnaires and those who dropped out of the study after providing at least demographic data. Participants with T2D who were treated with oral anti-diabetics provided data at t1significantly more often than those who were treated with dietary changes or insulin. Those participants who provided data at t1 spent significantly more time using the system, and participants in the tailored condition spent significantly more time in the IHCA than participants in the control condition spent in the control website (see Table 4).
Figure 3.
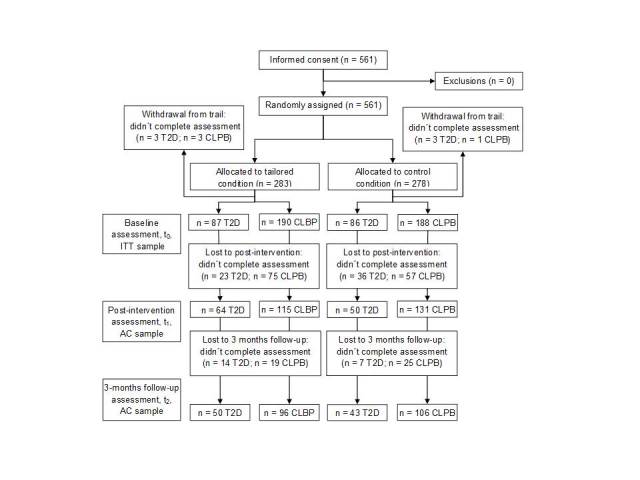
Flow of participants after randomization (ITT=intention-to-treat, AC=available cases).
Table 4.
Sample characteristicsa.
|
|
Tailored condition t0
(n=277) |
Control condition t0
(n=274) |
Baseline differences (tailored vs control condition), P value |
Total t1
(n=360) |
Dropout analysis (t1available vs t1not available), P value |
|
| Female, n (%) | 162 (58.5) | 162 (59.1) | .474 | 216 (60.0) | .467 | |
| Age in years, mean (SD) | 52.2 (13.1) | 52.7 (13.0) | .668 | 51.8 (13.1) | .116 | |
| Family status, n (%) | ||||||
|
|
Single | 67 (24.2) | 77 (28.1) | .742 | 100 (27.8) | .341 |
|
|
Married | 162 (58.5) | 150 (54.7) |
|
194 (53.9) |
|
|
|
Divorced | 39 (14.1) | 37 (13.5) |
|
52 (14.4) |
|
|
|
Widowed | 9 (3.2) | 10 (3.6) |
|
14 (3.9) |
|
| Educational level, highb, n (%) | 148 (53.4) | 140 (51.1) | .322 | 198 (55.0) | .089 | |
| Working status, employed, n (%) | 145 (55.6) | 160 (58.4) | .282 | 207 (57.5) | .786 | |
| Years since diagnosisc, mean (SD) | 11.1 (7.6) | 10.5 (8.0) | .649 | 10.7 (8.2) | .858 | |
| Current diabetes treatment a | ||||||
|
|
Dietary change | 40 (44.4) | 46 (51.7) | .371 | 57 (50.0) | .535 |
|
|
Insulin | 35 (38.9) | 25 (28.1) | .154 | 43 (37.7) | .139 |
|
|
Oral anti-diabetics | 59 (65.6) | 55 (61.8) | .643 | 80 (70.2) | .023 |
| Disability scored, mean (SD) | 41.4 (22.5) | 42.7 (22.8) | .573 | 42.2 (20.9) | .855 | |
| System usage in minutes, mean (SD) | 51.16 (39.7) | 37.6 (35.0) | <.001 | 49.7 (35.1) | <.001 | |
at0 = demographic data available (ITT population); t1= at least one outcome after intervention reported.
bmore than 10 years of education.
cfor patients with diabetes.
dfor patients with back pain.
There was also selective dropout between t0 and t1among participants with CLBP. At t1, participants with CLBP were significantly (P=.015) younger in the tailored condition (mean 48.0; SD 12.9) than in the control condition (mean 52.0; SD 12.7). Additionally, there are significantly (P=.021) more participants with higher education in the tailored condition (62.6%) than in the control condition (48.9%). Among the participants with T2D, there was no selective dropout between t0 and t1. At t2, there were no significant differences in either of the two diseases (T2D or CLBP).
Baseline Data
The mean age was 52.2 years (SD 13.1) in the tailored condition and 52.7 years (SD 13.0) in the control condition. Of the participants using the IHCA, 58.5% (162/277) were female (control condition: 59.1%, 162/274). There were no statistically significant differences in further demographic variables such as marital status, educational level, and working status. Sample characteristics are shown in Table 4.
Intention-to-Treat Analysis
The following results were obtained using the ITT approach including all randomized participants. The results of the sensitivity analysis using the available cases approach are reported in a separate section. Table 5 shows all of the results in detail.
Table 5.
Results of ITT and AC analyses.
|
|
N | Tailored condition | Control condition | Intervention main effect P |
Disease main effect P |
Intervention x disease P |
||||||
| T2D,M (SE) | CLBP,M (SE) | Total, M (SE) | T2D, M (SE) | CLBP, M (SE) | Total, M (SE) | |||||||
| Intention-to-treat analysis | ||||||||||||
|
|
Primary outcomes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Knowledge | 551 | 81.3 (1.9) | 74.4 (1.2) | 77.9 (1.2) | 82.9 (2.3) | 69.8 (1.4) | 76.3 (1.3) | .53 | <.001 | .04 |
|
|
|
Positive and active engagement in life | 551 | 71.9 (2.5) | 69.7 (1.8) | 70.8 (1.4) | 71.4 (2.3) | 70.9 (1.8) | 71.2 (1.4) | .88 | .86 | .43 |
|
|
|
Health directed behavior | 551 | 63.5 (3.9) | 68.7 (2.4) | 66.1 (2.4) | 63.7 (3.3) | 68.3 (2.4) | 66.0 (2.0) | .97 | .28 | .92 |
|
|
|
Emotional well-being | 551 | 68.8 (3.9) | 63.2 (2.8) | 66.0 (2.6 ) | 62.6 (3.7) | 60.2 (2.8) | 61.4 (2.3) | .28 | .60 | .66 |
|
|
|
Constructive attitudes and approaches | 551 | 78.3 (2.9) | 75.4 (2.1) | 76.8 (1.9) | 75.8 (2.5) | 75.6 (1.9) | 75.7 (1.6) | .498 | .95 | .59 |
|
|
|
Skill and technique acquisition | 551 | 77.6 (2.6) | 65.1 (1.7) | 71. 4 (1.5) | 75.8 (2.9) | 67.6 (1.7) | 71.7 (1.8) | .62 | .01 | .36 |
|
|
|
Self-monitoring and insight | 551 | 80.1 (2.1) | 70.8 (1.4) | 75.4 (1.4) | 79.5 (2.2) | 73.4 (1.3) | 76.5 (1.2) | .85 | .04 | .52 |
|
|
|
Health service navigation | 551 | 77.9 (3.1) | 70.0 (2.1) | 73.9 (2.0) | 74.0 (2.9) | 69.7 (1.8) | 71.8 (1.6) | .32 | .24 | .44 |
|
|
Secondary outcomes | |||||||||||
|
|
|
Decisional conflict | 551 | 79.7 (2.3) | 61.3 (1.6) | 70.5 (1.5) | 75.5 (2.3) | 60.3 (1.7) | 67.9 (1.4) | .15 | <.001 | .33 |
|
|
|
Preparation for decision making | 551 | 60.5 (3.4) | 53.8 (2.5) | 56.7 (2.1) | 57.6 (3.7) | 51.2 (2.3) | 54.4 (2.2) | .57 | .14 | .85 |
| Available cases analysis | ||||||||||||
|
|
Primary outcome | |||||||||||
|
|
|
Knowledge | 330 | 81.1 (1.9) | 77.1 (1.4) | 79.1 (1.2) | 81.8 (2.1) | 68.7 (1.3) | 75.2 (1.2) | .02 | <.001 | .008 |
|
|
|
Positive and active engagement in life | 295 | 71.8 (2.6) | 69.9 (1.8) | 70.9 (1.6) | 71.3 (2.8) | 71.3 (1.8) | 71.3 (1.6) | .86 | .68 | .68 |
|
|
|
Health directed behavior | 295 | 63.0 (3.4) | 69.4 (2.5) | 66.2 (2.1) | 64.9 (3.7) | 68.7 (2.4) | 66.8 (2.2) | .84 | .10 | .68 |
|
|
|
Emotional well-being | 295 | 70.8 (3.7) | 66.1 (2.6) | 68.5 (2.3) | 60.7 (3.9) | 59.3 (2.5) | 60.0 (2.3) | .009 | .35 | .60 |
|
|
|
Constructive attitudes and approaches | 295 | 78.8 (2.8) | 76.1 (2.0) | 77.5 (1.7) | 3.2 (0.09) | 74.5 (3.0) | 75.2 (1.9) | .30 | .68 | .51 |
|
|
|
Skill and technique acquisition | 295 | 78.3 (2.4) | 64.3 (1.7) | 71.3 (1.5) | 75.0 (2.6) | 68.8 (1.6) | 71.9 (1.5) | .78 | <.001 | .06 |
|
|
|
Self-monitoring and insight | 295 | 80.3 (1.9) | 70.0 (1.3) | 75.2 (1.2) | 79.3 (2.0) | 74.7 (1.3) | 77.0 (1.2) | .27 | <.001 | .09 |
|
|
|
Health service navigation | 295 | 79.1 (2.7) | 71.2 (1.9) | 75.2 (1.6) | 73.4 (2.9) | 69.8 (1.8) | 71.6 (1.7) | .13 | .02 | .37 |
|
|
Secondary outcomes | |||||||||||
|
|
|
Decisional conflict | 324 | 79.9 (2.4) | 61.9 (1.8) | 70.9 (1.5) | 74.8 (2.7) | 60.4 (1.7) | 67.6 (1.6) | .13 | <.001 | .47 |
|
|
|
Preparation for decision making | 324 | 61.0 (3.3) | 52.1 (2.4) | 56.4 (2.0) | 55.7 (3.6) | 51.2 (2.2) | 53.5 (2.1) | .29 | .02 | .47 |
Knowledge Immediately After the First Visit (t1)
With regard to knowledge of T2D or CLBP users in the tailored condition had a mean score of 77.9 (SE 1.2) compared with 76.3 (SE 1.3) in the control condition. There were no significant differences between groups (P=.53). There was, however, a significant difference between users with T2D and CLBP (P<.001), indicating higher knowledge scores in the T2D group. In addition, we observed a significant interaction effect between intervention and disease (P=.04), more strongly favoring the tailored condition over the control condition in CLBP (estimated mean difference of 4.6 [95% CI 1.0-8.2] points on a 0-100 points scale) than in T2D participants (estimated mean difference of -1.6 points [95% CI -7.4 to 4.2] on a 0-100 points scale).
Patient Empowerment at 3-Month Follow-Up (t2)
The heiQ does not provide a total score for patient empowerment. Table 5 shows the results for the seven included dimensions. There was no significant intervention main effect or interaction. However, there was a significant disease main effect on the dimensions Skill and Technique Acquisition (P=.01) and Self-Monitoring and Insight (P=.04), both indicating higher scores for users with T2D.
Decisional Conflict Immediately After the First Visit (t1)
There was a highly significant disease main effect. After the first use of the system, decisional conflict was lower in the CLBP group than in the T2D group (P<.001). There was no significant intervention main effect and no significant interaction.
Preparation for Decision Making Immediately After the First Visit (t1)
There was no significant main effect or interaction.
Sensitivity Analysis (Available Cases)
In addition to the ITT approach, we performed all calculations following the AC approach, including only participants who filled in all of the questionnaires. The aim of this procedure was to determine the extent to which missing data impacted the results reported above (sensitivity analysis).
Knowledge Immediately After the First Visit (t1)
The AC analysis showed a significant intervention main effect for knowledge (P=.02) indicating higher scores for the tailored condition (mean 79.1, SE 1.2) than for the control condition (mean 75.2, SE 1.2). The estimated mean difference between groups was 3.9 (95% CI 0.5-7.3) points on a 0-100 points scale. There was a significant disease x intervention interaction (P=.008) for knowledge, indicating the superiority of the tailored condition over the control condition in CLBP (estimated mean difference of 8.4 [95% CI 4.7-12.1] points on a 0-100 points scale) but not in T2D participants (estimated mean difference of -0.7 [95% CI -6.5 to 5.1] points on a 0-100 points scale). Additionally, there was a significant disease main effect for knowledge favoring the T2D group.
Patient Empowerment at 3-Month Follow-Up (t2)
We found a significant intervention main effect for Emotional Well-being (meaning less health-related negative effects such as anxiety, anger, and depression [78]) (P=.009) favoring the tailored condition (mean 68.5, SE 2.3) over the control condition (mean 60.0, SE 2.3). The estimated mean difference between groups was 25.4 (95% CI 6.3-44.5) points on a 0-100 points scale. Finally, there were significant disease main effects for Skill and Technique Acquisition (P<.001), Self-Monitoring and Insight (P<.001), and Health Service Navigation (P=.02) favoring the T2D group.
Decisional Conflict Immediately After the First Visit (t1)
We found a significant disease main effect (P<.001) showing more decisional conflict in the T2D group.
Preparation for Decision Making Immediately After the First Visit (t1)
There was a significant disease main effect (P=.02) indicating higher scores for the T2D compared with the CLBP group.
Discussion
Principal Findings
In a randomized controlled trial, we compared a Web-based, tailored, dialogue-based information system containing information on T2D or CLBP (tailored condition) with a website providing identical information without dialogue structure, tailoring, or interactive elements (control condition). The primary outcomes of the trial were knowledge and patient empowerment. Secondary outcomes were decisional conflict and preparation for decision making.
We expected that the tailored IHCA would be more attractive than the control website, be used more, and would thus lead to more knowledge and more empowerment. Indeed, participants spent significantly more time with the tailored website than the control website. Still, this did not lead to more knowledge or empowerment in the primary ITT analysis. In the AC analysis, the participants in the tailored condition displayed more knowledge at t1 and more Emotional Well-being at t2. This indicates that the tailored IHCA was more effective on these two dimensions than the control website. This was not the case for all users included; this was only the case for those who remained in the study and thus spent more time using the system. Contrary to the hypothesis, the tailored IHCA did not result in higher scores on the other six heiQ scales. It is possible that the effect was limited to the emotional level and could not be transferred to the cognitive or behavior level. This is in line with the results of Pal et al, who found that positive effects on cognitive outcomes could not be converted into behavioral changes [21]. There was a significant intervention x disease interaction favoring the tailored condition over the control condition more strongly in CLBP than in T2D participants. This superiority might indicate that tailoring in the CLBP IHCA may be more effective than tailoring in the T2D IHCA.
Other recent studies aimed directly at behavioral changes found effects on behavioral outcomes [24], and a meta-analysis on Internet-based cognitive behavioral therapy for patients with chronic somatic diseases found effects on psychological and physical outcomes [84]. A Web-based intervention aimed at psychosocial well-being in older adults with diabetes found improvements in depression, quality of life, social support, and self-efficacy [85], and a Web-based depression treatment for people with diabetes was found to reduce diabetes-specific emotional distress but had no beneficial effect on glycemic control [86]. Taken together, these results suggest that interventions aimed specifically at certain outcomes reliably have effects on these outcomes but have fewer effects on related or more distal outcomes. Consequently, our IHCA, as an educational intervention providing health information and adding behavioral change and decision support, has more consistent effects on knowledge (in persons who actually use it) than on cognitive or behavioral outcomes.
There were no significant effects regarding decisional conflict or preparation for decision making. A recent Cochrane review found that decision aids have, among other outcomes, an impact on knowledge and decisional conflict [87]. Again, the fact that we did find an impact on knowledge in the AC analysis but not on decisional conflict or preparation for decision making might be due to our IHCA being more of an educational intervention, providing the information necessary for shared decision making, than a classical decision tool.
Users with T2D yielded significantly better results regarding knowledge, preparation for decision making (only AC), and three (ITT: two) dimensions of the heiQ than participants with CLBP. One possible explanation might be that education and empowerment are traditionally cornerstones of diabetes management [88], which is not as explicitly true for the treatment of CLBP. Still, this result should be interpreted cautiously, because the instruments used to measure knowledge were different in both groups.
Strengths and Limitations
The work presented is the first trial on a German language IHCA on T2D or CLBP. The intervention was designed carefully based on two preliminary studies. There are some limitations to the work. One limitation concerns the representativeness of the sample. Only people with Internet access could be included in the study. Of the German general population, 73% are online [89], but of the population over 50, only 47% use the Internet. Because the prevalence of both T2D [90] and CLBP increases with age [91,92], there might be a selection bias in our sample. The diagnosis was self-assessed. In addition, this presents a limitation regarding the implementation and reach of online support for these diseases. Still, attrition was comparatively low for an online trial [23]. At t2, 52.4% of the sample was retained. The comparatively low attrition rate in the tailored and control conditions might be due to the incentive given for complete datasets. Because none of the outcome criteria were assessed at t0, we cannot know whether the differences between conditions at t1 were caused by the intervention or had been there from the beginning.
We did not include quantitative or qualitative feedback on user acceptance. We also did not assess potential confounders (eg, which other interventions the participants used while enrolled in the study). These variables might have added to our understanding of the IHCA effects. Going beyond the scope of our study, investigating the effectiveness of the tested intervention, further research should focus on the mechanisms of change and the role of context variables through analyzing potential mediators and moderators [93]. Although the participants were blinded to the group assignment, it might be possible that participants identified the intervention group due to the unusual dialogue-based delivery format used in the intervention group. However, the design and content of both groups were nearly identical.
Another limitation arises from the measures used. First, there are concerns regarding data quality and response rates in online questionnaires [94,95]. Psychometric properties have been found to be equivalent to or even better than data obtained from paper pencil questionnaires [96,97]. There are also advantages of online assessment: data quality can additionally be improved by validation checks that alert participants if their answers are implausible or if items are skipped [96]. Furthermore, online assessment seems to be less prone to social desirability [98]. Second, only some of the measures used in this trial are standardized (DCS, PDMS, BIT), whereas others are adapted (attitudes toward self-care) for our purposes. The measure to assess the primary outcome of T2D/CLBP knowledge was developed for the purpose of this study and has not been validated. Different versions of this outcome measure with different numbers of items for T2D and CLBP are used. None of the measures have been adapted for online use, which limits their comparability to results obtained from paper pencil tests [99].
Finally, the intervention had multiple components. We cannot know which component resulted in which effect. Future research should determine which components are effective and which are not.
Conclusions
The tailored IHCA enhanced knowledge and empowerment in persons who actually used it but failed to have effects in the total study population and on more distal outcomes. It might be concluded that tailoring and interactivity do not have effects with regard to these outcomes. Intervention components more specifically targeting cognitive and behavioral outcomes might enhance the effects. Pathways of change connecting intervention components and effects should be explored.
With regard to implementation, the IHCA could function outside of the study without major changes. Still, it would require some resources for updates and maintenance. Involving sponsors from the beginning might facilitate implementation. If our IHCA had made it to this stage, there would have been steps taken to extend its reach and effectiveness. In addition to being more specific, adaptability to tablets and mobile phones might have been an asset [21]. Another feature could be blended care to more explicitly integrate personal contacts, telephone, and online support [100]. The opportunity to share information and experiences with peers might be an especially attractive and important feature. The Pew Internet and American Life Project [101] found that people living with a chronic disease are more actively using the opportunities of Web 2.0: they generate and share content on their disease, use social media, blog, and chat more than people with no chronic conditions. Stepping into a multimedia dialogue with the users and letting expert-generated content and user-generated content spur each other might be the next step toward patient-centeredness in online support.
Acknowledgments
This study was funded by the German Federal Ministry of Education and Research (grant number: 01GX0710).
Abbreviations
- ADA
American Diabetes Association
- AEM
avoidance endurance model
- ANCOVA
analysis of covariance
- DCS
Decisional Conflict Scale
- heiQ
Health Education Impact Questionnaire
- IHCA
Interactive Health Communication Application
- PDMS
Preparation for Decision Making Scale
Multimedia Appendix 1
CONSORT-EHEALTH checklist V1.6.2 [46].
Footnotes
Authors' Contributions: NW participated in the conception and design of the study, interpreted the findings, and drafted the manuscript. JD participated in the conception and design of the study, interpreted the findings, and revised the manuscript. AW analyzed the data, interpreted the findings, and participated in drafting and revising the manuscript. LK participated in the conception and design of the study, analyzed the data, interpreted the findings, and participated in revising the manuscript. MH was awarded the grant, participated in the conception and design of the study and the interpretation of the findings, and revised the manuscript.
All authors read and approved the final manuscript.
Conflicts of Interest: NW, JD, and MH were among the developers of the intervention.
References
- 1.Hoy Damian, Bain Christopher, Williams Gail, March Lyn, Brooks Peter, Blyth Fiona, Woolf Anthony, Vos Theo, Buchbinder Rachelle. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012 Jun;64(6):2028–37. doi: 10.1002/art.34347. http://dx.doi.org/10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 2.Danaei Goodarz, Finucane Mariel M, Lu Yuan, Singh Gitanjali M, Cowan Melanie J, Paciorek Christopher J, Lin John K, Farzadfar Farshad, Khang Young-Ho, Stevens Gretchen A, Rao Mayuree, Ali Mohammed K, Riley Leanne M, Robinson Carolyn A, Ezzati Majid, Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet. 2011 Jul 2;378(9785):31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 3.Wild Sarah, Roglic Gojka, Green Anders, Sicree Richard, King Hilary. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004 May;27(5):1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 4.Becker Annette, Held Heiko, Redaelli Marcus, Strauch Konstantin, Chenot Jean F, Leonhardt Corinna, Keller Stefan, Baum Erika, Pfingsten Michael, Hildebrandt Jan, Basler Heinz-Dieter, Kochen Michael M, Donner-Banzhoff Norbert. Low back pain in primary care: costs of care and prediction of future health care utilization. Spine (Phila Pa 1976) 2010 Aug 15;35(18):1714–20. doi: 10.1097/brs.0b013e3181cd656f. [DOI] [PubMed] [Google Scholar]
- 5.Freburger Janet K, Holmes George M, Agans Robert P, Jackman Anne M, Darter Jane D, Wallace Andrea S, Castel Liana D, Kalsbeek William D, Carey Timothy S. The rising prevalence of chronic low back pain. Arch Intern Med. 2009 Feb 9;169(3):251–8. doi: 10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knauer Stefanie R, Freburger Janet K, Carey Timothy S. Chronic low back pain among older adults: a population-based perspective. J Aging Health. 2010 Dec;22(8):1213–34. doi: 10.1177/0898264310374111. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) Prevalence and most common causes of disability among adults--United States, 2005. MMWR Morb Mortal Wkly Rep. 2009 May 1;58(16):421–6. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5816a2.htm. [PubMed] [Google Scholar]
- 8.Agency for Healthcare Research and Quality (AHRQ): Medical Expenditure Panel Survey Total expenses and percent distribution for selected conditions by type of service. 2014. http://meps.ahrq.gov/data_stats/tables_compendia_hh_interactive.jsp?_SERVICE=MEPSSocket0&_PROGRAM=MEPSPGM.TC.SAS&File=HC2Y2011&Table=HC2Y2011_CNDXP_C&_Debug=
- 9.Segal L. The importance of patient empowerment in health system reform. Health Policy. 1998 Apr;44(1):31–44. doi: 10.1016/s0168-8510(98)00007-4. [DOI] [PubMed] [Google Scholar]
- 10.Wang J M, Walter S, Mantovani A. Re-evaluation of the chemotactic activity of tumour necrosis factor for monocytes. Immunology. 1990 Nov;71(3):364–7. [PMC free article] [PubMed] [Google Scholar]
- 11.Aujoulat Isabelle, d'Hoore William, Deccache Alain. Patient empowerment in theory and practice: polysemy or cacophony? Patient Educ Couns. 2007 Apr;66(1):13–20. doi: 10.1016/j.pec.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 12.Anderson Robert M, Funnell Martha M. Patient empowerment: myths and misconceptions. Patient Educ Couns. 2010 Jun;79(3):277–82. doi: 10.1016/j.pec.2009.07.025. http://europepmc.org/abstract/MED/19682830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schulz Peter J, Nakamoto Kent. Health literacy and patient empowerment in health communication: the importance of separating conjoined twins. Patient Educ Couns. 2013 Jan;90(1):4–11. doi: 10.1016/j.pec.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 14.Funnell M M, Anderson R M, Arnold M S, Barr P A, Donnelly M, Johnson P D, Taylor-Moon D, White N H. Empowerment: an idea whose time has come in diabetes education. Diabetes Educ. 1991;17(1):37–41. doi: 10.1177/014572179101700108. [DOI] [PubMed] [Google Scholar]
- 15.Bodenheimer Thomas, Lorig Kate, Holman Halsted, Grumbach Kevin. Patient self-management of chronic disease in primary care. JAMA. 2002 Nov 20;288(19):2469–75. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 16.Camerini Luca, Schulz Peter J, Nakamoto Kent. Differential effects of health knowledge and health empowerment over patients' self-management and health outcomes: a cross-sectional evaluation. Patient Educ Couns. 2012 Nov;89(2):337–44. doi: 10.1016/j.pec.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 17.Lustria Mia Liza A, Cortese Juliann, Noar Seth M, Glueckauf Robert L. Computer-tailored health interventions delivered over the Web: review and analysis of key components. Patient Educ Couns. 2009 Feb;74(2):156–73. doi: 10.1016/j.pec.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 18.Proudfoot Judith, Klein Britt, Barak Azy, Carlbring Per, Cuijpers Pim, Lange Alfred, Ritterband Lee, Andersson Gerhard. Establishing guidelines for executing and reporting Internet intervention research. Cogn Behav Ther. 2011;40(2):82–97. doi: 10.1080/16506073.2011.573807. [DOI] [PubMed] [Google Scholar]
- 19.Elbert Niels J, van Os-Medendorp Harmieke, van Renselaar Wilco, Ekeland Anne G, Hakkaart-van Roijen Leona, Raat Hein, Nijsten Tamar E C. Pasmans Suzanne G M A Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: a systematic review of systematic reviews and meta-analyses. J Med Internet Res. 2014;16(4):e110. doi: 10.2196/jmir.2790. http://www.jmir.org/2014/4/e110/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Vugt Michael, de Wit Maartje, Cleijne Wilmy H J, Snoek Frank J. Use of behavioral change techniques in web-based self-management programs for type 2 diabetes patients: systematic review. J Med Internet Res. 2013;15(12):e279. doi: 10.2196/jmir.2800. http://www.jmir.org/2013/12/e279/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pal Kingshuk, Eastwood Sophie V, Michie Susan, Farmer Andrew J, Barnard Maria L, Peacock Richard, Wood Bindie, Inniss Joni D, Murray Elizabeth. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2013;3:CD008776. doi: 10.1002/14651858.CD008776.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Riva Silvia, Camerini Anne-Linda, Allam Ahmed, Schulz Peter J. Interactive sections of an Internet-based intervention increase empowerment of chronic back pain patients: randomized controlled trial. J Med Internet Res. 2014;16(8):e180. doi: 10.2196/jmir.3474. http://www.jmir.org/2014/8/e180/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simon Daniela, Kriston Levente, von Wolff Alessa, Buchholz Angela, Vietor Christine, Hecke Torsten, Loh Andreas, Zenker Matthias, Weiss Mario, Härter Martin. Effectiveness of a web-based, individually tailored decision aid for depression or acute low back pain: a randomized controlled trial. Patient Educ Couns. 2012 Jun;87(3):360–8. doi: 10.1016/j.pec.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 24.Schulz Daniela N, Kremers Stef PJ, Vandelanotte Corneel, van Adrichem Mathieu J G, Schneider Francine, Candel Math J J M, de Vries Hein. Effects of a web-based tailored multiple-lifestyle intervention for adults: a two-year randomized controlled trial comparing sequential and simultaneous delivery modes. J Med Internet Res. 2014;16(1):e26. doi: 10.2196/jmir.3094. http://www.jmir.org/2014/1/e26/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Samoocha David, Bruinvels David J, Elbers Nieke A, Anema Johannes R, van der Beek Allard J. Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis. J Med Internet Res. 2010;12(2):e23. doi: 10.2196/jmir.1286. http://www.jmir.org/2010/2/e23/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuijpers Wilma, Groen Wim G, Aaronson Neil K, van Harten Wim H. A systematic review of web-based interventions for patient empowerment and physical activity in chronic diseases: relevance for cancer survivors. J Med Internet Res. 2013;15(2):e37. doi: 10.2196/jmir.2281. http://www.jmir.org/2013/2/e37/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ciere Yvette, Cartwright Martin, Newman Stanton P. A systematic review of the mediating role of knowledge, self-efficacy and self-care behaviour in telehealth patients with heart failure. J Telemed Telecare. 2012 Oct;18(7):384–91. doi: 10.1258/jtt.2012.111009. [DOI] [PubMed] [Google Scholar]
- 28.Murray E, Burns J, See Tai S, Lai R, Nazareth I. Interactive Health Communication Applications for people with chronic disease. Cochrane Database Syst Rev. 2005;(4):CD004274. doi: 10.1002/14651858.CD004274.pub4. [DOI] [PubMed] [Google Scholar]
- 29.Camerini Luca, Schulz Peter Johannes. Effects of functional interactivity on patients' knowledge, empowerment, and health outcomes: an experimental model-driven evaluation of a web-based intervention. J Med Internet Res. 2012;14(4):e105. doi: 10.2196/jmir.1953. http://www.jmir.org/2012/4/e105/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murray Elizabeth, White Ian R, Varagunam Mira, Godfrey Christine, Khadjesari Zarnie, McCambridge Jim. Attrition revisited: adherence and retention in a web-based alcohol trial. J Med Internet Res. 2013;15(8):e162. doi: 10.2196/jmir.2336. http://www.jmir.org/2013/8/e162/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Habibović Mirela, Cuijpers Pim, Alings Marco, van der Voort Pepijn, Theuns Dominic, Bouwels Leon, Herrman Jean-Paul, Valk Suzanne, Pedersen Susanne. Attrition and adherence in a WEB-Based Distress Management Program for Implantable Cardioverter defibrillator Patients (WEBCARE): randomized controlled trial. J Med Internet Res. 2014;16(2):e52. doi: 10.2196/jmir.2809. http://www.jmir.org/2014/2/e52/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brouwer Wendy, Oenema Anke, Raat Hein, Crutzen Rik, de Nooijer Jascha, de Vries Nanne K, Brug Johannes. Characteristics of visitors and revisitors to an Internet-delivered computer-tailored lifestyle intervention implemented for use by the general public. Health Educ Res. 2010 Aug;25(4):585–95. doi: 10.1093/her/cyp063. http://her.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=19897515. [DOI] [PubMed] [Google Scholar]
- 33.Neve Melinda J, Collins Clare E, Morgan Philip J. Dropout, nonusage attrition, and pretreatment predictors of nonusage attrition in a commercial Web-based weight loss program. J Med Internet Res. 2010;12(4):e69. doi: 10.2196/jmir.1640. http://www.jmir.org/2010/4/e69/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glasgow Russell E, Christiansen Steven M, Kurz Deanna, King Diane K, Woolley Tim, Faber Andrew J, Estabrooks Paul A, Strycker Lisa, Toobert Deborah, Dickman Jennifer. Engagement in a diabetes self-management website: usage patterns and generalizability of program use. J Med Internet Res. 2011;13(1):e9. doi: 10.2196/jmir.1391. http://www.jmir.org/2011/1/e9/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verheijden Marieke W, Jans Marielle P, Hildebrandt Vincent H, Hopman-Rock Marijke. Rates and determinants of repeated participation in a web-based behavior change program for healthy body weight and healthy lifestyle. J Med Internet Res. 2007;9(1):e1. doi: 10.2196/jmir.9.1.e1. http://www.jmir.org/2007/1/e1/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fan L, Sidani S. Effectiveness of Diabetes Self-management Education Intervention Elements: A Meta-analysis. Canadian Journal of Diabetes. 2009 Jan;33(1):18–26. doi: 10.1016/S1499-2671(09)31005-9. [DOI] [Google Scholar]
- 37.Eysenbach Gunther. The law of attrition. J Med Internet Res. 2005;7(1):e11. doi: 10.2196/jmir.7.1.e11. http://www.jmir.org/2005/1/e11/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Danaher Brian G, Boles Shawn M, Akers Laura, Gordon Judith S, Severson Herbert H. Defining participant exposure measures in Web-based health behavior change programs. J Med Internet Res. 2006;8(3):e15. doi: 10.2196/jmir.8.3.e15. http://www.jmir.org/2006/3/e15/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Donkin Liesje, Christensen Helen, Naismith Sharon L, Neal Bruce, Hickie Ian B, Glozier Nick. A systematic review of the impact of adherence on the effectiveness of e-therapies. J Med Internet Res. 2011;13(3):e52. doi: 10.2196/jmir.1772. http://www.jmir.org/2011/3/e52/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Christensen Helen, Griffiths Kathleen M, Farrer Louise. Adherence in internet interventions for anxiety and depression. J Med Internet Res. 2009;11(2):e13. doi: 10.2196/jmir.1194. http://www.jmir.org/2009/2/e13/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Norman Gregory J, Zabinski Marion F, Adams Marc A, Rosenberg Dori E, Yaroch Amy L, Atienza Audie A. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med. 2007 Oct;33(4):336–345. doi: 10.1016/j.amepre.2007.05.007. http://europepmc.org/abstract/MED/17888860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kelders Saskia M, Kok Robin N, Ossebaard Hans C, Van Gemert-Pijnen Julia E W C. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J Med Internet Res. 2012;14(6):e152. doi: 10.2196/jmir.2104. http://www.jmir.org/2012/6/e152/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lustria Mia Liza A, Noar Seth M, Cortese Juliann, Van Stee Stephanie K, Glueckauf Robert L, Lee Junga. A meta-analysis of web-delivered tailored health behavior change interventions. J Health Commun. 2013;18(9):1039–69. doi: 10.1080/10810730.2013.768727. [DOI] [PubMed] [Google Scholar]
- 44.Krebs Paul, Prochaska James O, Rossi Joseph S. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med. 2010;51(3-4):214–21. doi: 10.1016/j.ypmed.2010.06.004. http://europepmc.org/abstract/MED/20558196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bennett Gary G, Glasgow Russell E. The delivery of public health interventions via the Internet: actualizing their potential. Annu Rev Public Health. 2009;30:273–92. doi: 10.1146/annurev.publhealth.031308.100235. [DOI] [PubMed] [Google Scholar]
- 46.Eysenbach Gunther, CONSORT-EHEALTH Group CONSORT-EHEALTH: improving and standardizing evaluation reports of Web-based and mobile health interventions. J Med Internet Res. 2011;13(4):e126. doi: 10.2196/jmir.1923. http://www.jmir.org/2011/4/e126/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dirmaier Jörg, Härter Martin, Weymann Nina. A tailored, dialogue-based health communication application for patients with chronic low back pain: study protocol of a randomised controlled trial. BMC Med Inform Decis Mak. 2013;13:66. doi: 10.1186/1472-6947-13-66. http://www.biomedcentral.com/1472-6947/13/66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Weymann Nina, Härter Martin, Dirmaier Jörg. A tailored, interactive health communication application for patients with type 2 diabetes: study protocol of a randomised controlled trial. BMC Med Inform Decis Mak. 2013;13:24. doi: 10.1186/1472-6947-13-24. http://www.biomedcentral.com/1472-6947/13/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Becker A, Chenot J-F, Niebling W, Kochen M M, Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin [Guidelines for back pain] Z Orthop Ihre Grenzgeb. 2004;142(6):716–9. doi: 10.1055/s-2004-832488. [DOI] [PubMed] [Google Scholar]
- 50.Khadjesari Zarnie, Murray Elizabeth, Kalaitzaki Eleftheria, White Ian R, McCambridge Jim, Thompson Simon G, Wallace Paul, Godfrey Christine. Impact and costs of incentives to reduce attrition in online trials: two randomized controlled trials. J Med Internet Res. 2011;13(1):e26. doi: 10.2196/jmir.1523. http://www.jmir.org/2011/1/e26/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klasen Bernhard W, Hallner Dirk, Schaub Claudia, Willburger Roland, Hasenbring Monika. Validation and reliability of the German version of the Chronic Pain Grade questionnaire in primary care back pain patients. Psychosoc Med. 2004;1:Doc07. http://europepmc.org/abstract/MED/19742049. [PMC free article] [PubMed] [Google Scholar]
- 52.Toobert D J, Hampson S E, Glasgow R E. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000 Jul;23(7):943–50. doi: 10.2337/diacare.23.7.943. http://care.diabetesjournals.org/cgi/pmidlookup?view=long&pmid=10895844. [DOI] [PubMed] [Google Scholar]
- 53.Petrak Frank, Stridde Elmar, Leverkus Friedhelm, Crispin Alexander A, Forst Thomas, Pfützner Andreas. Development and validation of a new measure to evaluate psychological resistance to insulin treatment. Diabetes Care. 2007 Sep;30(9):2199–204. doi: 10.2337/dc06-2042. [DOI] [PubMed] [Google Scholar]
- 54.Hasenbring M. Hallner D: Telemedizinisches Patienten-Diagnose-System (TPDS) : Selbsterklärende PC-Lösung zur Analyse von Risikofaktoren der Chronifizierung von Rückenschmerzen. Dtsch Arztebl. 1999;6:49–50. [Google Scholar]
- 55.Edwards Philip James, Roberts Ian, Clarke Mike J, Diguiseppi Carolyn, Wentz Reinhard, Kwan Irene, Cooper Rachel, Felix Lambert M, Pratap Sarah. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 2009;(3):MR000008. doi: 10.1002/14651858.MR000008.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Weymann Nina, Härter Martin, Dirmaier Jörg. Quality of online information on type 2 diabetes: a cross-sectional study. Health Promot Int. 2014 Mar 30;:epub ahead of print. doi: 10.1093/heapro/dau019. [DOI] [PubMed] [Google Scholar]
- 57.Weymann Nina, Härter Martin, Dirmaier Jörg. Information and decision support needs in patients with type 2 diabetes. Health Informatics J. 2014 Jun 10;:-. doi: 10.1177/1460458214534090. [DOI] [PubMed] [Google Scholar]
- 58.Crutzen Rik, Cyr Dianne, de Vries Nanne K. The role of user control in adherence to and knowledge gained from a website: randomized comparison between a tunneled version and a freedom-of-choice version. J Med Internet Res. 2012;14(2):e45. doi: 10.2196/jmir.1922. http://www.jmir.org/2012/2/e45/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Danaher Brian G, McKay H Garth, Seeley John R. The information architecture of behavior change websites. J Med Internet Res. 2005;7(2):e12. doi: 10.2196/jmir.7.2.e12. http://www.jmir.org/2005/2/e12/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Miller William R, Rollnick Stephen. Motivational Interviewing, Third Edition: Helping People Change (Applications of Motivational Interviewing) New York: The Guilford Press; 2012. [Google Scholar]
- 61.Boettcher J, Rozental A, Andersson G, Carlbring P. Side effects in Internet-based interventions for Social Anxiety Disorder. Internet Interventions. 2014 Mar;1(1):3–11. doi: 10.1016/j.invent.2014.02.002. [DOI] [Google Scholar]
- 62.Burgers Jako S, Bailey Julia V, Klazinga Niek S, Van Der Bij Akke K, Grol Richard, Feder Gene. Inside guidelines: comparative analysis of recommendations and evidence in diabetes guidelines from 13 countries. Diabetes Care. 2002 Nov;25(11):1933–9. doi: 10.2337/diacare.25.11.1933. [DOI] [PubMed] [Google Scholar]
- 63.Stone M A, Wilkinson J C, Charpentier G, Clochard N, Grassi G, Lindblad U, Müller U A, Nolan J, Rutten G E, Khunti K. Evaluation and comparison of guidelines for the management of people with type 2 diabetes from eight European countries. Diabetes Res Clin Pract. 2010 Feb;87(2):252–60. doi: 10.1016/j.diabres.2009.10.020. [DOI] [PubMed] [Google Scholar]
- 64.National Institute for Health and Clinical Excellence (NICE): National Guideline C The management of type 2 diabetes. [2014-06-20]. Type 2 diabetes http://www.guideline.gov/content.aspx?id=15202.
- 65.American Diabetes Association Standards of medical care in diabetes--2010. Diabetes Care. 2010 Jan;33 Suppl 1:S11–61. doi: 10.2337/dc10-S011. http://europepmc.org/abstract/MED/20042772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Airaksinen O, Brox J I, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion A F, Reis S, Staal J B, Ursin H, Zanoli G, COST B13 Working Group on Guidelines for Chronic Low Back Pain Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006 Mar;15 Suppl 2:S192–300. doi: 10.1007/s00586-006-1072-1. http://europepmc.org/abstract/MED/16550448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bundesärztekammer (BÄK), Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF): Nationale Versorgungsleitlinie Kreuzschmerz – Kurzfassung Version. 2010. [2014-06-20]. http://www.versorgungsleitlinien.de/themen/kreuzschmerz/pdf/nvl-kreuzschmerz-lang-4.pdf.
- 68.Deshpande A, Furlan A, Mailis-Gagnon A, Atlas S, Turk D. Opioids for chronic low-back pain. Cochrane Database Syst Rev. 2007;(3):CD004959. doi: 10.1002/14651858.CD004959.pub3. [DOI] [PubMed] [Google Scholar]
- 69.Furlan Andrea D, Imamura Marta, Dryden Trish, Irvin Emma. Massage for low-back pain. Cochrane Database Syst Rev. 2008;(4):CD001929. doi: 10.1002/14651858.CD001929.pub2. [DOI] [PubMed] [Google Scholar]
- 70.Hayden J A, van Tulder M W, Malmivaara A, Koes B W. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev. 2005;(3):CD000335. doi: 10.1002/14651858.CD000335.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Heymans M W, van Tulder M W, Esmail R, Bombardier C, Koes B W. Back schools for non-specific low-back pain. Cochrane Database Syst Rev. 2004;(4):CD000261. doi: 10.1002/14651858.CD000261.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Staal J Bart, de Bie Rob, de Vet Henrica CW, Hildebrandt Jan, Nelemans Patty. Injection therapy for subacute and chronic low-back pain. Cochrane Database Syst Rev. 2008;(3):CD001824. doi: 10.1002/14651858.CD001824.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Urquhart D M, Hoving J L, Assendelft W W J, Roland M, van Tulder M W. Antidepressants for non-specific low back pain. Cochrane Database Syst Rev. 2008;(1):CD001703. doi: 10.1002/14651858.CD001703.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Weymann Nina, Härter Martin, Petrak Frank, Dirmaier Jörg. Health information, behavior change, and decision support for patients with type 2 diabetes: development of a tailored, preference-sensitive health communication application. Patient Prefer Adherence. 2013;7:1091–9. doi: 10.2147/PPA.S46924. http://dx.doi.org/10.2147/PPA.S46924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Maunsell Elizabeth, Lauzier Sophie, Brunet Jennifer, Pelletier Sylvie, Osborne Richard H, Campbell H Sharon. Health-related empowerment in cancer: validity of scales from the Health Education Impact Questionnaire. Cancer. 2014 Oct 15;120(20):3228–36. doi: 10.1002/cncr.28847. [DOI] [PubMed] [Google Scholar]
- 76.Herbert Rosemary J, Gagnon Anita J, Rennick Janet E, O'Loughlin Jennifer L. A systematic review of questionnaires measuring health-related empowerment. Res Theory Nurs Pract. 2009;23(2):107–32. doi: 10.1891/1541-6577.23.2.107. [DOI] [PubMed] [Google Scholar]
- 77.Nolte Sandra, Elsworth Gerald R, Sinclair Andrew J, Osborne Richard H. The extent and breadth of benefits from participating in chronic disease self-management courses: a national patient-reported outcomes survey. Patient Educ Couns. 2007 Mar;65(3):351–60. doi: 10.1016/j.pec.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 78.Osborne Richard H, Elsworth Gerald R, Whitfield Kathryn. The Health Education Impact Questionnaire (heiQ): an outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Educ Couns. 2007 May;66(2):192–201. doi: 10.1016/j.pec.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 79.Schuler Michael, Musekamp Gunda, Faller Hermann, Ehlebracht-König Inge, Gutenbrunner Christoph, Kirchhof Roland, Bengel Jürgen, Nolte Sandra, Osborne Richard H, Schwarze Monika. Assessment of proximal outcomes of self-management programs: translation and psychometric evaluation of a German version of the Health Education Impact Questionnaire (heiQ™) Qual Life Res. 2013 Aug;22(6):1391–403. doi: 10.1007/s11136-012-0268-6. [DOI] [PubMed] [Google Scholar]
- 80.O'Connor A M. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 81.Buchholz A, Hölzel L, Kriston L, Simon D. Härter M: Die Decisional Conflict Scale in deutscher Sprache (DCS-D) - Dimensionale Struktur in einer Stichprobe von Hausarztpatienten. Klinische Diagnostik und Evaluation. 2011;4:15–30. [Google Scholar]
- 82.Graham I, O'Connor A. Preparation for Decision Making Scale - User manual. 1996. [2014-06-20]. l http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_PrepDM.pdf.
- 83.Buchholz A, Simon D. Härter M: Die Preparation for Decision-Making Scale (PDMS-G). Faktorielle und konkurrente Validität in einer Onlinestichprobe von Personen mit Kreuzschmerz und Depression. Klinische Diagnostik und Evaluation. 2011;4:31–45. [Google Scholar]
- 84.van Beugen Sylvia, Ferwerda Maaike, Hoeve Dane, Rovers Maroeska M, Spillekom-van Koulil Saskia, van Middendorp Henriët, Evers Andrea Wm. Internet-based cognitive behavioral therapy for patients with chronic somatic conditions: a meta-analytic review. J Med Internet Res. 2014;16(3):e88. doi: 10.2196/jmir.2777. http://www.jmir.org/2014/3/e88/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bond Gail E, Burr Robert L, Wolf Fredric M, Feldt Karen. The effects of a web-based intervention on psychosocial well-being among adults aged 60 and older with diabetes: a randomized trial. Diabetes Educ. 2010;36(3):446–56. doi: 10.1177/0145721710366758. [DOI] [PubMed] [Google Scholar]
- 86.van Bastelaar Kim M P, Pouwer François, Cuijpers Pim, Riper Heleen, Snoek Frank J. Web-based depression treatment for type 1 and type 2 diabetic patients: a randomized, controlled trial. Diabetes Care. 2011 Feb;34(2):320–5. doi: 10.2337/dc10-1248. http://europepmc.org/abstract/MED/21216855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Stacey Dawn, Légaré France, Col Nananda F, Bennett Carol L, Barry Michael J, Eden Karen B, Holmes-Rovner Margaret, Llewellyn-Thomas Hilary, Lyddiatt Anne, Thomson Richard, Trevena Lyndal, Wu Julie H C Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2014;1:CD001431. doi: 10.1002/14651858.CD001431.pub4. [DOI] [PubMed] [Google Scholar]
- 88.Krans H, Porta M, Keen H. Diabetes Care and Research in Europe: the St. Vincent Declaration Action Programme. Copenhagen: World Health Organization. Regional Office for Europe. (EUR/ICP/CLR 055/3); 1992. [2014-06-20]. http://www.codex.vr.se/texts/SVD.pdf. [Google Scholar]
- 89.van Eimeren B, Frees B. Ergebnisse der ARD/ZDF-Onlinestudie 2011: Drei von vier Deutschen im Netz -- ein Ende des digitalen Grabens in Sicht? media perspektiven. 2011;7:334–349. [Google Scholar]
- 90.Centers for Disease Control and Prevention, US Department of Health and Human Services . Centers for Disease Control and Prevention (CDC): Diabetes Report Card 2012. Atlanta, GA: 2012. [2014-06-20]. http://www.cdc.gov/diabetes/pubs/pdf/diabetesreportcard.pdf. [Google Scholar]
- 91.Göbel H. [Epidemiology and costs of chronic pain syndromes exemplified by specific and unspecific low back pain] Schmerz. 2001 Apr;15(2):92–8. doi: 10.1007/s004820170031. [DOI] [PubMed] [Google Scholar]
- 92.Rückenschmerzen Kapitel 1.2.5.1. 2006. Gesundheitsberichterstattung des Bundes (GBE): Gesundheit in Deutschland http://www.gbe-bund.de/gbe10/abrechnung.prc_abr_test_logon?p_uid=gastg&p_aid=&p_knoten=FID&p_sprache=D&p_suchstring=10410::Dorsopathien.
- 93.Craig Peter, Dieppe Paul, Macintyre Sally, Michie Susan, Nazareth Irwin, Petticrew Mark, Medical Research Council Guidance Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. doi: 10.1136/bmj.a1655. http://europepmc.org/abstract/MED/18824488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wyatt J C. When to use web-based surveys. J Am Med Inform Assoc. 2000;7(4):426–9. doi: 10.1136/jamia.2000.0070426. http://jamia.oxfordjournals.org/lookup/pmidlookup?view=long&pmid=10887170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Best SJ, Krueger B, Hubbard C, Smith A. An Assessment of the Generalizability of Internet Surveys. Social Science Computer Review. 2001 May 01;19(2):131–145. doi: 10.1177/089443930101900201. [DOI] [Google Scholar]
- 96.van Gelder Marleen M H J, Bretveld Reini W, Roeleveld Nel. Web-based questionnaires: the future in epidemiology? Am J Epidemiol. 2010 Dec 1;172(11):1292–8. doi: 10.1093/aje/kwq291. http://aje.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=20880962. [DOI] [PubMed] [Google Scholar]
- 97.Pouwer F, Snoek F J, van der Ploeg H M, Heine R J, Brand A N. A comparison of the standard and the computerized versions of the Well-being Questionnaire (WBQ) and the Diabetes Treatment Satisfaction Questionnaire (DTSQ) Qual Life Res. 1998 Jan;7(1):33–8. doi: 10.1023/a:1008832821181. [DOI] [PubMed] [Google Scholar]
- 98.Booth-Kewley S, Larson GE, Miyoshi DK. Social desirability effects on computerized and paper-and-pencil questionnaires. Computers in Human Behavior. 2007 Jan;23(1):463–477. doi: 10.1016/j.chb.2004.10.020. [DOI] [Google Scholar]
- 99.Buchanan Tom. Internet-based questionnaire assessment: appropriate use in clinical contexts. Cogn Behav Ther. 2003;32(3):100–9. doi: 10.1080/16506070310000957. [DOI] [PubMed] [Google Scholar]
- 100.Brouwer Wendy, Kroeze Willemieke, Crutzen Rik, de Nooijer Jascha, de Vries Nanne K, Brug Johannes, Oenema Anke. Which intervention characteristics are related to more exposure to internet-delivered healthy lifestyle promotion interventions? A systematic review. J Med Internet Res. 2011;13(1):e2. doi: 10.2196/jmir.1639. http://www.jmir.org/2011/1/e2/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fox S, Purcell K. California Health Care Foundation: Chronic Disease and the Internet. 2010. [2014-06-20]. http://www.pewinternet.org/2010/03/24/chronic-disease-and-the-internet/