Abstract
Background
Inflammatory bowel disease (IBD) is a chronic condition of the bowel that affects over 1 million people in the United States. The recurring nature of disease makes IBD patients ideal candidates for patient-engaged care that is centered on enhanced self-management and improved doctor-patient communication. In IBD, optimal approaches to management vary for patients with different phenotypes and extent of disease and past surgical history. Hence, a single quality metric cannot define a heterogeneous disease such as IBD, unlike hypertension and diabetes. A more comprehensive assessment may be provided by complementing traditional quality metrics with measures of the patient’s quality of life (QOL) through an application like HealthPROMISE.
Objective
The objective of this pragmatic randomized controlled trial is to determine the impact of the HealthPROMISE app in improving outcomes (quality of care [QOC], QOL, patient adherence, disease control, and resource utilization) as compared to a patient education app. Our hypothesis is that a patient-centric self-monitoring and collaborative decision support platform will lead to sustainable improvement in overall QOL for IBD patients.
Methods
Participants will be recruited during face-to-face visits and randomized to either an interventional (ie, HealthPROMISE) or control (ie, education app). Patients in the HealthPROMISE arm will be able to update their information and receive disease summary, quality metrics, and a graph showing the trend of QOL (SIBDQ) scores and resource utilization over time. Providers will use the data for collaborative decision making and quality improvement interventions at the point of care. Patients in the control arm will enter data at baseline, during office visits, and at the end of the study but will not receive any decision support (trend of QOL, alert, or dashboard views).
Results
Enrollment in the trial will be starting in first quarter of 2015. It is intended that up to 300 patients with IBD will be recruited into the study (with 1:1 allocation ratio). The primary endpoint is number of quality indicators met in HealthPROMISE versus control arm. Secondary endpoints include decrease in number of emergency visits due to IBD, decrease in number of hospitalization due to IBD, change in generic QOL score from baseline, proportion of patients in each group who meet all eligible outpatient quality metrics, and proportion of patients in disease control in each group. In addition, we plan to conduct protocol analysis of intervention patients with adequate HealthPROMISE utilization (more than 6 log-ins with data entry from week 0 through week 52) achieving above mentioned primary and secondary endpoints.
Conclusions
HealthPROMISE is a unique cloud-based patient-reported outcome (PRO) and decision support tool that empowers both patients and providers. Patients track their QOL and symptoms, and providers can use the visual data in real time (integrated with electronic health records [EHRs]) to provide better care to their entire patient population. Using pragmatic trial design, we hope to show that IBD patients who participate in their own care and share in decision making have appreciably improved outcomes when compared to patients who do not.
Trial Registration
ClinicalTrials.gov NCT02322307; https://clinicaltrials.gov/ct2/show/NCT02322307 (Archived by WebCite at http://www.webcitation.org/6W8PoYThr).
Keywords: medical informatics, patient reported outcome, mHealth, engagement
Introduction
Background
Inflammatory bowel disease (IBD) is a chronic condition of the bowel that affects over 1 million people in the United States [1]. Although the incidence of IBD is rising, the precise cause of the disease remains unknown. Medical treatment for IBD has improved significantly in recent years; however, current efforts are largely ameliorative rather than curative. As a result, IBD patients have to cope with a lifelong condition in which there are commonly remissions and relapses. This makes IBD patients the ideal candidates to target for improved self-management when it comes to care.
While diseases such as hypertension and diabetes render themselves well to quality improvement efforts because of standardized indicators such as blood pressure and hemoglobin A1C respectively, a single quality-of-care (QOC) metric cannot define a heterogeneous disease such as IBD, where optimal approaches to manage patients differ between different phenotypes. Furthermore, IBD profoundly affects patients not only physically but also in social, professional, and emotional activities [1,2]. Overall well-being of IBD patients cannot be achieved if these dimensions are not improved [3-6]. Unfortunately, most of the currently proposed quality improvement initiatives in IBD are process measures and do not include quality of life (QOL) or clinically meaningful outcomes such as clinical remission or hospitalizations that matter most to patients and their state of health [7].
Chronic diseases affect almost 1 out of every 2 Americans and produce a significant burden on US health care [8,9]. Meaningful health system quality improvement warrants patient-provider interaction focused on QOC and QOL in chronic diseases like IBD [10,11]. For health care teams, the question remains: how do we better engage patients without placing increased time constraints on health care staff? Based on pilot work, we believe that patients are as eager as physicians, if not more, to improve their QOL and care, and involving them as partners to improve care can bring remarkable efficiency to current quality improvement efforts [3].
Objectives
HealthPROMISE [12] is a unique cloud-based PRO (patient-reported outcome) and decision support platform developed at Sinai AppLab, Icahn School of Medicine at Mount Sinai [13] Patients track their QOL and symptoms, and providers can use the visual data in real time (integrated with electronic health records [EHRs]) to provide better care to their entire patient population (Figures 1 and 2). HealthPROMISE addresses unique challenges to improving quality and outcomes for patients with a chronic disease like IBD.
Figure 1.

Quality of life measure.
Figure 2.
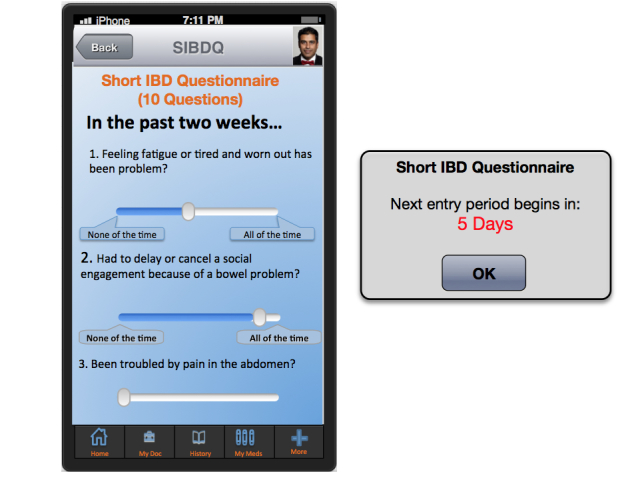
Short Inflammatory Bowel Disease Questionnaire.
Adopting a Broader Definition of Quality
A more comprehensive assessment may be provided by complementing the QOL with quality of care metrics (Figure 3). QOL has been defined as “a global measure of patient’s perceptions, illness experience, and functional status that incorporates social, cultural, psychological, and disease-related factors” [14]. QOL metrics can be used to inform outcomes in clinical encounters, monitor population health, and as end points in clinical trials [14]. National Institutes of Health (NIH) Patient Reported Outcomes Measurement Information System [15] and more recently Project Health Design [16] have provided valuable insights into generic measurements for QOL. To address this challenge, we have previously defined a set of comprehensive quality indicators for IBD patients through analyzing different focus groups to study what factors patients assess and value when defining “quality” in terms of living with IBD and the treatment of IBD. Additionally, through semi-structured interviews and Delphi panel sessions with 15 providers, provider input on QOC was recorded.
Figure 3.

Quality of care.
Decreasing the Burden of Measuring Quality
Quality improvement efforts so far have shown that measuring even limited QOC metrics carries a prohibitively high administrative and cost burden. The estimated costs from the Institute for Healthcare Improvement quality improvement initiative for either congestive heart failure or diabetes ranged from $81,000 to $148,000 per organization [17]. Chen and Bates have shown that total reported costs for inpatient quality improvement for a hospital ranged from $2 million to $21 million, with the majority of costs attributed to collecting and reporting quality metrics for national organizations [18]. This burden of measuring quality is likely to increase exponentially when multiple QOC metrics are included in quality measurement. To address this challenge, patient- and physician-provided indicators were incorporated into a mobile health strategy platform, HealthPROMISE, that allows patients to record and self-report their QOL and treatment with regards to their IBD.
Improving the Effectiveness of Quality Improvement Initiatives
Currently, there is no well-accepted national model for quality improvement. Most of the quality improvement projects to date involve some kind of data abstraction from the clinical encounters that is fed into a registry to allow benchmarking, risk adjustment, and quality reporting. This cycle takes anywhere from a few weeks to a few months and happens long after the patient has left the health care facility. Patients are not involved in measuring or improving quality. Thus, an important patient-physician “productive interaction” opportunity to improve outcomes at the point of care is missed [19]. In HealthPROMISE, patients track symptoms and QOL before office visits and in waiting rooms, thus allowing meaningful discussion about QOC to take place during office visits (Figures 1 and 2).
The aim of this research protocol is to evaluate the patient-centric Web- and mobile-based application, HealthPROMISE, where IBD patients longitudinally measure their QOC and QOL metrics and physicians use this information for collaborative decision making and improving patient outcomes. Our hypothesis is that a patient-centric self-monitoring and collaborative decision support platform will lead to sustainable improvement in overall QOL for IBD patients.
Methods
Study Design
This is a phase III, single-center, pragmatic randomized controlled trial (RCT) to evaluate if a patient-centric self-monitoring and collaborative decision support platform will lead to sustainable improvement in overall QOL for IBD patients. It is intended that 300 patients with IBD will be recruited into the study (allocation ratio 1:1; Figure 4). After meeting all the inclusion criteria with no exclusions, patient is asked to complete a tablet-based screening questionnaire at the end of which patient is randomized at the point of care to intervention or control arm. Patients in the control arm will receive an IBD education app PIN whereas the intervention arm will receive HealthPROMISE app PIN (Figure 3). Intervention patients enter their data once every 2 weeks and this data is then made visible to providers using a Web-based dashboard integrated with the EHR (Figures 4 and 5). Intervention and control apps will be provided free of charge to patients, and patients will be given $25 after completing initial and end of study questionnaires.
Figure 4.
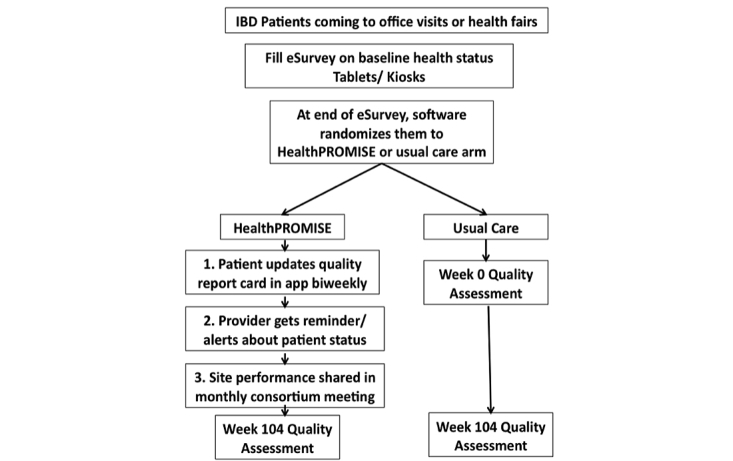
Point of care recruitment and randomization.
Figure 5.

Shows initial mock-up of app.
Study Population
Patients will be recruited at outpatient and inpatient facilities in an academic center through informational paper and electronic flyers. Once enrolled, patients will receive a walkthrough of the app, which includes access to a training video. The provider dashboard will also have access to the training video. Eligible patients will be 18 years or older, have a mobile phone or access to the Internet at home, and be able to complete a Web-based questionnaire in English. Exclusion criteria include the inability to communicate with the investigators and comply with the study requirements, presence of short bowel syndrome or stoma, and presence of a condition or disease that, in the opinion of the investigators, may make it difficult for the patient to use the HealthPROMISE app, including, but not limited to, advanced dementia.
Study Instruments
Overview
A combination of different questionnaires (eg, SIBDQ), symptom updates, and quality indicators relevant for evaluating patient status will be the data collected during this study through the HealthPROMISE app (Figure 6).
Figure 6.
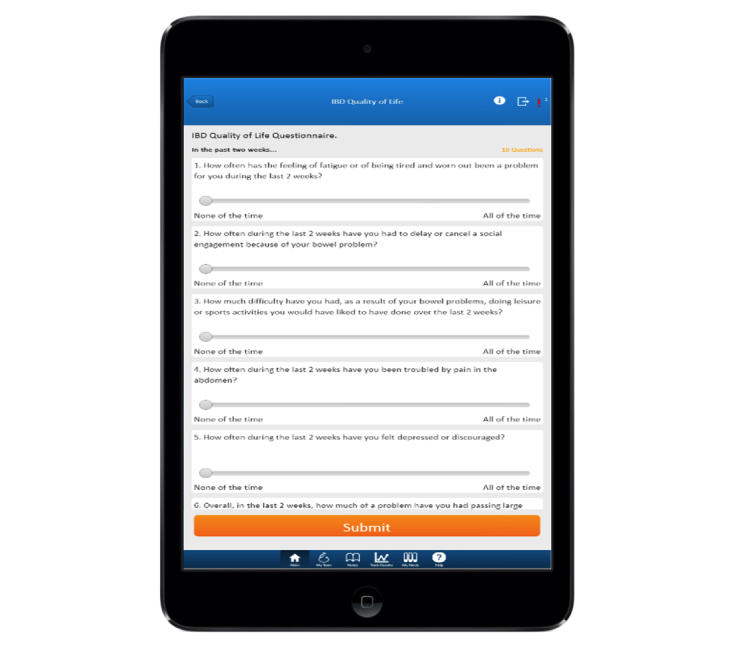
Shows completed app.
Disease Specific Quality of Life Questionnaire
The Short Inflammatory Bowel Disease Questionnaire (SIBDQ) [20] is a validated and reliable tool to measure health-related QOL in adult patients with IBD. The questionnaire consists of 10 questions scored in four domains: bowel symptoms, emotional health, systemic systems, and social function. The SIBDQ is a respected QOL questionnaire used extensively in academic research and clinical trials. Study patients in the control arm and interventional arm will complete an SIBDQ as part of a survey to objectively measure QOL at baseline and at exit (52 weeks or 104 weeks). Additionally, patients in the intervention arm will be asked to complete the SIBDQ every 2 weeks; this will be used to classify patients as having “good control,” “fair control,” or “poor control.”
General Quality of Life Questionnaire
EQ-5D is a standardized instrument for measuring generic QOL [21]. Applicable to a wide range of health conditions and treatments, it provides a simple descriptive profile and a single index value for health status. EQ-5D is primarily designed for self-completion by respondents. It is cognitively simple and takes only a few minutes to complete. It is generally recognized that a change of 0.5 points (on a scale of 1-7) is the minimal clinically important difference (MCID), consistent with moderate effect size. Patients in the intervention arm will be asked to complete the EQ-5D every 2 weeks.
Other Instruments
eHEALS is an 8-item measure of eHealth literacy developed to measure consumers’ combined knowledge, comfort, and perceived skills at finding, evaluating, and applying electronic health information to health problems [22]. This instrument has been psychometrically validated and its score positively correlated with intention to use personal health records. Patient Activation Measure (PAM-13) will be used to measure patient activation and engagement with health [23]. eHEALS and PAM-13 will be completed by patients in both arms during entry and exit surveys only.
Quality indicators are included from a list of indicators published by national societies and finalized through a Delphi panel of IBD providers [24,25]. These will be updated every three months by either providers or patients, along with hospitalization and emergency department visit information (Figure 7).
Figure 7.

Provider workflow on app dashboard.
Utilization will be assessed through log-in, page views, health information updates, and response to alerts and reminders.
Results
Outcome Measures
All outcome data (Textbox 1) will be collected online. Additionally, we will conduct subgroup analysis of patients with poor disease control at week 0 (SIBDQ≤30) and in those with high patient-reported anxiety, depression, or stress achieving primary and secondary endpoints. We will assess change in inflammatory markers, endoscopic scores, and additional quality metrics in each group and determine predictors of HealthPROMISE and control app utilization and its impact on other primary and secondary end-points. Consistent with the pragmatic nature of the trial, study progress will be assessed throughout and effort will be optimized to better engage providers and patients (Table 1).
Primary and secondary endpoints.
Primary endpoint
Number of quality indicators met in HealthPROMISE versus control arm
Secondary endpoints
Decrease in number of emergency visits due to IBD
Decrease in number of hospitalization due to IBD
Change in generic QOL score (EQ-5D) from baseline
Proportion of patients in each group who meet all eligible outpatient quality metrics
Proportion of patients in disease control in each group
Emergency visits in each group
Hospitalizations in each group
General QOL scores in each group
Per protocol analysis of intervention patients with adequate HealthPROMISE use (more than 6 log-ins with data entry from week 0 through week 52) achieving above mentioned primary and secondary endpoints
Table 1.
Evaluation metrics for HealthPROMISE progress
| Metric | Target Group | Goal / Timeline | |
| Process | |||
| Number of providers trained | Investigators | 10 in 2 months | |
|
|
Number of patients enrolled | Participants | 300 in 6 months |
|
|
Recruitment and training of key personnel | Coordinator | 1 in 3 months |
|
|
Patient utilization of HealthPROMISE | Participants | Ongoing |
|
|
Provider utilization of HealthPROMISE | Providers | Ongoing |
|
|
Response to alert within 2 business days | Providers | >90% |
| Outcome | |||
|
|
Improvement in quality of care metrics | Provider, Center | Quarterly reports |
|
|
Improvement in quality of life | Provider, Center | Quarterly reports |
|
|
Readmission rate in two arms | Provider, Center | Quarterly reports |
Statistical Analysis Plan
Overview
We will use SAS 9.2 (SAS Institute, Inc) to calculate frequencies and percentages for categorical factors and means with standard deviations and/or percentiles for continuous factors. Pearson’s chi-square tests will be used for primary outcome (number of quality indicators met in HealthPROMISE vs control arm) and secondary outcomes. We will calculate percentage score for each patient at baseline and at week 104 ([number of quality metrics met/quality metrics eligible]*100). Change in the percentage score from baseline to week 104 will be aggregated for each arm to calculate percentage-point improvement in quality metric, similar to the strategy by Cebul et al [26].
Analysis of covariance (ANCOVA) will be performed to assess differences in the area under the curve of QOL scores while adjusting for baseline QOL score. To assess the association between patient and practice characteristics and achievement of eligible quality metrics, we will use multivariable analyses. Since the data will be hierarchically structured, with patients clustered within physicians and metrics clustered within patients, we will construct multilevel, generalized, linear mixed models with random effects to determine predictors of quality care, similar to the strategy used by Kanwal et al [27]. Independent variables will include demographic characteristics (age, gender), education and income level, race and ethnicity, computer usage, eHealth literacy scores, clinical characteristics (comorbidities, phenotype, disease severity), and provider characteristics (gender, age, site of practice, years of practice, presence of nurse practitioner).
Interim Analysis
Interim analysis will be performed once 150 patients are followed up for week 52. If primary outcome is met by that time, all patients will be offered HealthPROMISE app and followed for the additional 52 weeks.
Sample Size Justification
Study endpoints will be primarily assessed using intention-to-treat (ITT) analysis; however, per-protocol analysis will also be performed. The study is to be powered such that there is a>80% probability of demonstrating a difference with a P value (P = .05) using a two-tailed t test.
We assume that 128 out of 150 subjects (85%) in the intervention arm will meet all quality indicators (primary outcome) and expect that this percentage will be at least 15% lower in the control arm. A sample size of 95 patients will be needed in each arm to achieve at least 80% power to detect the difference with a 5% one-sided significance level.
Accounting for an estimated 30% attrition rate, we will require a total of 250 IBD patients to be enrolled in the study. Since some patients may agree to enroll but not download the app or use the PIN, we will recruit a total of 300 patients in the study.
For secondary outcomes related to QOL, the control arm is not a placebo arm and physicians are free to initiate any therapy based on patients' symptoms. Hence, we will assess the difference in proportion of patients achieving MCID in the HealthPROMISE arm versus control arm in the study. Using the distribution-based approach, an effect size of 0.5 SD is the closest estimate for determining MCID for SIBDQ and EQ-5D. Assuming that 20% more patients in HealthPROMISE arm will achieve MCID than in the control arm, the sample size of 250 patients will have 88% power to detect the difference with a 5% one-sided significance level and an estimated 30% attrition rate.
Discussion
Principal Findings
This pragmatic trial will help us study if a patient-centric self-monitoring and collaborative disease management app and dashboard can lead to improvement in care provided to IBD patients. Our hypothesis is that IBD patients using the HealthPROMISE platform will have significant improvement in QOC metrics, QOL, and resource utilization by the end of the 2-year study period when compared to IBD patients in the control arm (using a health education app alone).
Future Direction and Sustainability
HealthPROMISE can be a sustainable platform in the long run because it is patient-centric, device and disease agnostic, and not dependent on proprietary EHRs. As most of the data is entered by patients, the cost of running, supporting, and sustaining HealthPROMISE is very low compared to traditional disease registries. HealthPROMISE has a rapid form generator capability to allow it to be customized for other chronic diseases. Additionally, the decision support that generates alerts and dashboard reports is within the stand-alone HealthPROMISE app and not dependent on proprietary EHRs. We aim to integrate HealthPROMISE with personal health records, partner with national societies, and support through consortia so it can become a new standard of quality care for IBD and other chronic diseases.
Conclusion
HealthPROMISE is a unique cloud-based PRO and decision support tool that empowers both patients and providers. Patients track their QOL and symptoms, and providers can use the visual data in real time (integrated with EHRs) to provide better care to their entire patient population. Using pragmatic trial design, we hope to show that IBD patients who participate in their own care and share in decision making have appreciably improved outcomes when compared to patients who do not [28,29].
Acknowledgments
The study is supported by the Crohn's & Colitis Foundation of America (grant #253624) and the National Institutes of Health (5 K23 DK97451-02) with Ashish Atreja as the principal investigator.
Abbreviations
- IBD
inflammatory bowel disease
- QOL
quality of life
- QOC
quality of care
- PRO
patient-reported outcome
- EHR
electronic health records
- NIH
National Institutes of Health
- RCT
randomized controlled trial
- SIBDQ
Short Inflammatory Bowel Disease Questionnaire
- MCID
minimal clinically important difference
- PAM
patient activation measure
Multimedia Appendix 1
Initial critique of the proposal before it got funded in second attempt.
Multimedia Appendix 2
Informed consent form.
Multimedia Appendix 3
CONSORT-EHEALTH checklist V1.6.2 [30].
Footnotes
Conflicts of Interest: The app was developed in-house at Sinai AppLab.
References
- 1.Cohen RD. The quality of life in patients with Crohn's disease. Aliment Pharmacol Ther. 2002 Sep;16(9):1603–1609. doi: 10.1046/j.1365-2036.2002.01323.x. http://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0269-2813&date=2002&volume=16&issue=9&spage=1603. [DOI] [PubMed] [Google Scholar]
- 2.Irvine EJ. Quality of life issues in patients with inflammatory bowel disease. Am J Gastroenterol. 1997 Dec;92(12 Suppl):18S–24S. [PubMed] [Google Scholar]
- 3.Atreja A, Bahuva R, Achkar JP, Brzezinski A, Shen B, Kandiel A, Lashner B. Can patients reliably report quality indicators and disease phenotype? Proceedings of the 11th Advances in Inflammatory Bowel Diseases, Crohn’s & Colitis Foundation’s Clinical and Research Conference; 2011 Dec 1-3; Hollywood Florida. Advances in Inflammatory Bowel Diseases, Crohn's & Colitis Foundation's Clinical and Research Conference; 2011; Hollywood, FL. 2011. Dec, [Google Scholar]
- 4.De Feo J, Barnard W. Juran Institute's Six Sigma Breakthrough and Beyond: Quality Performance Breakthrough Methods. New York: McGraw-Hill; 2004. [Google Scholar]
- 5.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. N Engl J Med. 2003 Jun 26;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare & Medicaid Services (CMS)‚ HHS. Medicare program; payment policies under the physician fee schedule, five-year review of work relative value units, clinical laboratory fee schedule: signature on requisition, and other revisions to part B for CY 2012. Final rule with comment period. Fed Regist. 2011 Nov 28;76(228):73026–73474. http://www.gpo.gov/fdsys/pkg/FR-2011-11-28/pdf/2011-28597.pdf. [PubMed] [Google Scholar]
- 7.Kappelman MD, Dorn SD, Peterson E, Runge T, Allen JI. Quality of care for gastrointestinal conditions: a primer for gastroenterologists. Am J Gastroenterol. 2011 Jul;106(7):1182–1187. doi: 10.1038/ajg.2011.118. [DOI] [PubMed] [Google Scholar]
- 8.Wu SY, Green A. Projection of chronic illness prevalence and cost inflation. Santa Monica, CA: RAND Health. 2000 [Google Scholar]
- 9.DeVol R, Bedroussian A, Charuworn A, Chatterjee A, Kim IK, Kim S, Klowden K. Santa Monica, CA; Milken Institute. 2007. [2015-01-24]. An unhealthy America: the economic burden of chronic disease—charting a new course to save lives and increase productivity and economic growth http://www.milkeninstitute.org/publications/view/321.
- 10.Kappelman MD, Palmer L, Boyle BM, Rubin DT. Quality of care in inflammatory bowel disease: a review and discussion. Inflamm Bowel Dis. 2010 Jan;16(1):125–133. doi: 10.1002/ibd.21028. [DOI] [PubMed] [Google Scholar]
- 11.Reddy SI, Friedman S, Telford JJ, Strate L, Ookubo R, Banks PA. Are patients with inflammatory bowel disease receiving optimal care? Am J Gastroenterol. 2005 Jun;100(6):1357–61. doi: 10.1111/j.1572-0241.2005.40849.x. [DOI] [PubMed] [Google Scholar]
- 12.HealthPROMISE. [2015-01-23]. http://www.healthpromise.org/
- 13.Sinai AppLab. [2015-01-24]. http://sinaiapplab.org/
- 14.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993 Apr 15;118(8):622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- 15.Patient Reported Outcomes Measurement Information System. [2015-01-29]. http://www.nihpromis.org/?AspxAutoDetectCookieSupport=1.
- 16.Project HealthDesign. [2015-01-29]. http://www.projecthealthdesign.org/
- 17.Cretin S, Shortell SM, Keeler EB. An evaluation of collaborative interventions to improve chronic illness care. Framework and study design. Eval Rev. 2004 Feb;28(1):28–51. doi: 10.1177/0193841X03256298. [DOI] [PubMed] [Google Scholar]
- 18.Chen LM, Rein MS, Bates DW. Costs of quality improvement: a survey of four acute care hospitals. Jt Comm J Qual Patient Saf. 2009 Nov;35(11):544–550. doi: 10.1016/s1553-7250(09)35074-6. [DOI] [PubMed] [Google Scholar]
- 19.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4. http://www.acponline.org/journals/ecp/augsep98/cdm.htm. [PubMed] [Google Scholar]
- 20.Irvine EJ, Zhou Q, Thompson AK. The Short Inflammatory Bowel Disease Questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn's Relapse Prevention Trial. Am J Gastroenterol. 1996 Aug;91(8):1571–1578. [PubMed] [Google Scholar]
- 21.Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001 Jul;33(5):337–43. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- 22.Norman CD, Skinner HA. eHEALS: The eHealth Literacy Scale. J Med Internet Res. 2006;8(4):e27. doi: 10.2196/jmir.8.4.e27. http://www.jmir.org/2006/4/e27/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005 Dec;40(6 Pt 1):1918–1930. doi: 10.1111/j.1475-6773.2005.00438.x. http://europepmc.org/abstract/MED/16336556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Allen. JI. Dassopoulos T. American Gastroenterology Association. [2014-12-17]. Adult inflammatory bowel disease physician performance measures set http://www.gastro.org/practice/quality-initiatives/IBD_Measures.pdf.
- 25.The physician quality reporting system. [2014-12-17]. American Gastroenterology Association http://www.gastro.org/practice/quality-initiatives/cms-physician-qualitative-report-initiative.
- 26.Cebul RD, Love TE, Jain AK, Hebert CJ. Electronic health records and quality of diabetes care. N Engl J Med. 2011 Sep 1;365(9):825–833. doi: 10.1056/NEJMsa1102519. [DOI] [PubMed] [Google Scholar]
- 27.Kanwal F, Schnitzler MS, Bacon BR, Hoang T, Buchanan PM, Asch SM. Quality of care in patients with chronic hepatitis C virus infection: a cohort study. Ann Intern Med. 2010 Aug 17;153(4):231–239. doi: 10.7326/0003-4819-153-4-201008170-00005. [DOI] [PubMed] [Google Scholar]
- 28.Riippa I, Linna M, Rönkkö I. The effect of a patient portal with electronic messaging on patient activation among chronically ill patients: controlled before-and-after study. J Med Internet Res. 2014;16(11):e257. doi: 10.2196/jmir.3462. http://www.jmir.org/2014/11/e257/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kuijpers W, Groen WG, Aaronson NK, van Harten WH. A systematic review of web-based interventions for patient empowerment and physical activity in chronic diseases: relevance for cancer survivors. J Med Internet Res. 2013;15(2):e37. doi: 10.2196/jmir.2281. http://www.jmir.org/2013/2/e37/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eysenbach G, CONSORT-EHEALTH Group CONSORT-EHEALTH: improving and standardizing evaluation reports of Web-based and mobile health interventions. J Med Internet Res. 2011;13(4):e126. doi: 10.2196/jmir.1923. http://www.jmir.org/2011/4/e126/ [DOI] [PMC free article] [PubMed] [Google Scholar]


