Abstract
Background and Objectives:
For reduced port surgery in pediatric patients, the initial umbilical incision plays an important role in both functional ability and cosmetic impact. Larger umbilical incisions enable better manipulation of forceps, extraction of larger surgical specimens, and easier exteriorization of the intestine for anastomosis. We have pursued an incision of the small pediatric umbilicus that allows for enlargement of the orifice of the abdominal opening with preservation of the natural umbilical profile. This article aims to present a new umbilical incision technique and describe the outcomes.
Methods:
We devised a new umbilical incision technique for reduced port surgery in pediatric patients. Our incision is made in an inverted Y shape (Benz incision), allowing for access port device insertion. The Benz incision technique was applied between November 2010 and May 2014 and was retrospectively studied.
Results:
Seventy-five patients underwent Benz incisions. The median age of all patients was 6 years 6 months (range, 26 days to 18 years), and the median body weight was 21.7 kg (range, 3.1–54.3 kg). Benz incisions were applied for various procedures, including reduced port surgery with hepaticojejunostomy for congenital biliary dilatation, portojejunostomy for biliary atresia, Meckel diverticulectomy, tumor resection, varicocelectomy, cholecystectomy, splenectomy, ileus surgery, ileocecal resection, and total colectomy. All patients were successfully treated, without a significant increase in operating time or severe complications. The cosmetic profile of the umbilicus was maintained after surgery.
Conclusion:
The Benz incision is a feasible, effective, and scarless approach for reduced port surgery in pediatric patients whose umbilical rings are too small for the conventional approach.
Keywords: Reduced port surgery, Transumbilical laparoscopic surgery, Pediatric surgery
INTRODUCTION
Because of continuous efforts to minimize scarring and make procedures less invasive, reduced port surgery (RPS) procedures, such as laparoendoscopic single-site surgery, have been developed and have gained popularity in not only general but also pediatric surgery over the past few years.1 For RPS, the initial umbilical incision plays an important role in both functional ability and cosmetic impact. Larger incisions enable better manipulation of forceps, extraction of larger surgical specimens, and easier exteriorization of the intestine for anastomosis. However, minimally invasive surgery seeks to maintain cosmesis by preserving the umbilical profile because the umbilicus is an important abdominal landmark and plays an important cosmetic role for most patients.2,3 Unfortunately, given the size of the pediatric umbilical ring, a conventional longitudinal incision at the umbilicus does not provide enough space for triangulation of several instruments, specimen removal, or exteriorization of the intestine for anastomosis. Extension of the longitudinal incision past the umbilical ring causes visible scarring, resulting in reduced cosmesis.
Several techniques for the initial umbilical incision have been described that all facilitate removal of surgical specimens (up to a certain size) and improve cosmetic outcomes.4–6 For the pediatric population, these special incisions (eg, circumumbilical incision) can leave a visible scar around the umbilicus, disrupting its configuration, especially if the incision is large when compared with the size of the umbilicus. To overcome these problems, we developed a new umbilical incision, made in an inverted Y shape (Benz incision). The Benz incision is a simple and effective technique for enlarging the orifice of the abdominal opening, and it allows for umbilical remodeling without complications. The aim of this article is to present our innovative umbilical incision technique, which is associated with successful outcomes, minimal esthetic effects, and optimum patient compliance.
METHODS
From November 2010 to May 2014, 75 children underwent Benz incisions, at the umbilicus, at Saitama Children's Medical Center and Nagoya University Hospital. The Benz incision was used for RPS and laparoscopic surgical procedures that required specimen removal or exteriorization of the intestine for anastomosis. A retrospective study was then conducted on these patients, and the technical aspects and surgical outcomes were evaluated. The ethics committees at our hospitals approved this retrospective survey.
Benz Incision Technique
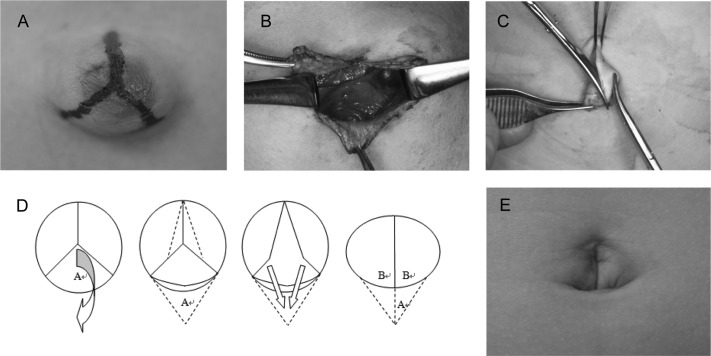
With the patient under general anesthesia, we marked 3 points in the umbilical region, which corresponded to the vertices of an equilateral triangle. After pulling out the center of the umbilicus, we then drew 3 lines (13 mm each) in an inverted Y shape (Figure 1A). Incisions were made along each line, creating 3 triangular skin flaps. The incisions were extended beneath the skin, by dissecting the subcutaneous tissue from the underlying fascia using an electrocautery, and the linea alba and peritoneum were incised longitudinally. The fascial opening was then enlarged in the shape of a circle, with a circumference of approximately 78 mm (Figure 1B). Access port devices such as E-Z Access with a Lap Protector (Hakko Medical, Nagano, Japan), GelPoint (Applied Medical, Rancho Santa Margarita, California), SILS Port (Covidien, Mansfield, Massachusetts), and Alexis wound retractor (Applied Medical) were then inserted through the umbilical incision. At the end of the operation, the fascia and peritoneum were closed with 4 or 5 No. 3–0 absorbable sutures. If necessary, the periumbilical subcutaneous fat tissue was trimmed to maintain the concavity of the umbilicus. The sides of each adjoining flap were also trimmed, as shown in Figure 1C. The tips of the 3 skin flaps were anchored to the caudal end of the fascia with a No. 5–0 absorbable suture to retain the umbilicus' concave curvature toward the caudal aspect. The sides of each adjoining flap were then closed with buried, No. 6–0 absorbable dermal sutures (Figure 1D). With a cotton ball placed in the umbilicus, dressing was applied. Air was aspirated from the space around the cotton ball to compress the skin flaps to the surrounding tissue, as well as preserve the natural concavity of the umbilicus.
Figure 1.
Benz incision technique. A, An inverted Y–shaped incision is marked, with three 13-mm incisions in the shape of the Mercedes-Benz logo. B, The linea alba and peritoneum are incised longitudinally. The fascial opening is enlarged to a circle shape with a radius of 13 mm. C, The sides of each adjoining flap are trimmed. D, The tips of the 3 skin flaps are anchored to the caudal end of the fascia to retain the umbilicus' concave curvature toward the caudal aspect, and the sides of each adjoining flap are then closed. E, The umbilical scar becomes essentially invisible 3 months after surgery.
RESULTS
Of the 75 patients who received Benz incisions in this study, 45 were male patients and 30 were female patients. The median age of the patients was 6 years 6 months (range, 26 days to 18 years), and the median body weight was 21.7 kg (range, 3.1–54.3 kg). The Benz incision was used for RPS and laparoscopic surgical procedures requiring removal of surgical specimens or exteriorization of the intestine for anastomosis. By use of the access port device, which was inserted into the Benz incision, a combination of exteriorization of the intestine and RPS or a combination of specimen removal and RPS was performed. The operative procedures in which the Benz incision at the umbilicus was applied are listed in Table 1.
Table 1.
Operative Procedures by Benz Incision at Umbilicus
| Operative Procedures | No. of Patients | RPSa | Exteriorization | Removal |
|---|---|---|---|---|
| Laparoscopic hepaticojejunostomy for CBDa | 16 | + | + | − |
| Laparoscopic tumor resection | 11 | + | − | + |
| Laparoscopic-assisted SIa Meckel diverticulectomy | 8 | + | + | + |
| Laparoscopic portojejunostomy for biliary atresia | 7 | + | + | − |
| Laparoscopic-assisted SI pull-through for HDa | 6 | + | − | − |
| Laparoscopic SI varicocelectomy | 6 | + | − | − |
| Laparoscopic SI cholecystectomy | 4 | + | − | + |
| Laparoscopic-assisted SI ileocecal resection | 3 | + | + | + |
| Laparoscopic SI splenectomy | 3 | + | − | + |
| Laparoscopic SI ileus surgery | 3 | + | + | − |
| Laparoscopic-assisted total colectomy | 2 | + | + | − |
| Laparoscopic-assisted Partington-Rochelle procedure | 2 | + | + | − |
| Laparoscopic-assisted repair of left paraduodenal hernia | 1 | + | − | − |
| Laparoscopic SI gastropexy | 1 | + | − | − |
| Laparoscopic-assisted gastrectomy | 1 | + | − | + |
| Laparoscopic-assisted removal of gastric trichobezoar | 1 | + | + | + |
CBD = congenital biliary dilatation, RPS = reduced port surgery, SI = single incision, HD = Hirschsprung's disease.
In all cases the Benz incision was effective at enlarging a fascial opening to a circumference of approximately 78 mm, which provides sufficient space for performing operations in the standard fashion. The Benz incision allowed for easy manipulation of the surgical instruments without conflict, as well as removal of surgical specimens. Roux-en-Y anastomosis and retrocolic fixation were performed in an extracorporeal manner without stress, and the anastomosed intestine was then internalized through the Benz incision without difficulty. In all cases blood loss was minimal, and the operative time was not significantly increased. There were no intraoperative complications related to the Benz incision. A postoperative stitch abscess developed in 1 patient, but this healed without treatment. In another patient, ischemic flaps of the umbilicus developed after a 10-hour operation, although these also healed without special treatment. Necrosis of the tips of the triangles has never been observed. The operative wounds were satisfactory and were almost invisible 3 months after surgery in all cases (Figure 1E). No complications have been observed during long-term follow-up.
DISCUSSION
RPS was developed over the past decade and has gained popularity, especially in general surgery. More recently, it has been gradually accepted for use in pediatric populations, despite the limited working space. Unfortunately, the size of the pediatric umbilical ring is so small that a longitudinal incision at the umbilicus does not allow several instruments to be triangulated and does not provide enough space for removal of specimens or exteriorization of the intestine for anastomosis. Special umbilical incisions such as the circumumbilical incision and omega-shaped incision have been proposed as simple techniques to provide acceptable cosmetic results in patients undergoing laparoscopic procedures that require specimen extraction.5–7 However, over three quarters of the circumference of the umbilicus is prone to umbilical ischemia and deformity of the natural umbilical profile. Wounds outside the umbilical ring, such as those occurring with the circumumbilical or omega-shaped incision, typically result in scar formation, although scarring inside the umbilicus is generally invisible. Moreover, it is difficult to make these incisions extended if a larger fascial opening is required to extract large specimens. In general surgery, Hachisuka et al8 described an umbilical zigzag skin incision that can enlarge the fascial opening to a diameter of 6 cm while maintaining cosmesis. Unfortunately, this type of incision cannot create a wide enough opening for surgery in a small umbilicus and fascia while still preserving cosmesis. Therefore it was necessary to develop an incision technique specific for pediatric patients with small umbilici that creates the larger umbilical opening and profile required for the highly advanced, and evolving, field of laparoscopic surgery.
In the pediatric field, umbilicoplasty is a common surgical procedure for the repair of an umbilical hernia. Various techniques such as making several skin flaps and anchoring the tip of the caudal skin flap to the caudal end of the fascia to create a natural-appearing umbilicus have been reported.9–11 Therefore we developed an umbilical incision technique in accordance with the procedure for umbilicoplasty for use in laparoscopic surgery in pediatric patients whose umbilical rings are smaller than those of adults. Our new technique creates 3 skin flaps and preserves the natural shape of the umbilicus. We chose incisions of 13 mm in length and created them in an inverted Y shape, similar to the Mercedes-Benz logo (3-pointed star). The Benz incision can enlarge the fascial opening to approximately 78 mm in circumference, whereas a conventional longitudinal umbilical incision of 26 mm can only create an opening with a circumference of 52 mm (Figure 2). In our experience thus far, skin flaps of 13 mm in length are appropriate for smooth manipulation during RPS and can fit in the umbilical ring of an infant. Our Benz incision not only provides a larger opening but also retains the natural appearance of the umbilicus. By use of the Benz incision, transumbilical laparoscopic surgery has been performed for multiple procedures, as shown in Table 1, and all procedures were successfully completed without severe complications. Although there was no control group, blood loss was minimal and the operative duration was not significantly increased compared with standard approaches. For a wide range of applications, creation of an ileal J-pouch and mincing of an enlarged spleen during splenectomy were easily performed with RPS. Therefore use of the Benz incision at the umbilicus has successfully reduced the number of incisions for ports in pediatric patients, without increasing complications.
Figure 2.
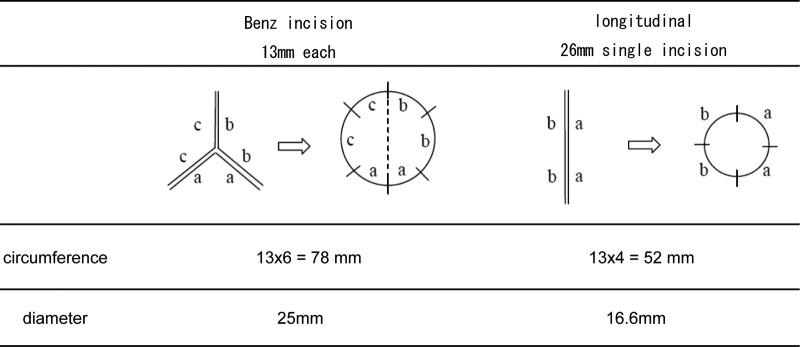
The Benz incision can enlarge the fascial opening to approximately 78 mm in circumference, whereas a conventional longitudinal 26-mm single incision in the pediatric umbilical ring can only produce a circumference of 52 mm.
In our study a stitch abscess developed in patient, and ischemia developed in the skin flaps in another patient after a 10-hour operation. However, these complications were resolved without treatment within 3 months of surgery, and therefore it appears that the Benz incision at the umbilicus does not increase wound infections. Furthermore, no visible postoperative scar is left because the incision is entirely within the umbilical region. If a larger fascial opening is required to extract large specimens, the incision can easily be extended from each incision line to the flaps. In addition to laparoscopic surgery, we successfully applied our technique to Ramstedt pyloromyotomy, and we believe that our new umbilical incision is applicable to various types of surgical procedures.
CONCLUSION
The Benz umbilical incision can provide a wide enough fascial opening to maintain the triangulation of instruments, removal of specimens, and exteriorization of the intestine for anastomosis. Therefore we conclude that the Benz incision at the umbilicus appears to be a feasible, effective, and scarless approach for RPS in pediatric patients with small umbilical rings.
Contributor Information
Hizuru Amano, Department of Pediatric Surgery, Saitama Children's Medical Center, Saitama, Japan..
Hiroo Uchida, Department of Pediatric Surgery, Nagoya University Graduate School of Medicine, Nagoya, Japan..
Hiroshi Kawashima, Department of Pediatric Surgery, Saitama Children's Medical Center, Saitama, Japan..
Kyoichi Deie, Department of Pediatric Surgery, Saitama Children's Medical Center, Saitama, Japan..
Naruhiko Murase, Department of Pediatric Surgery, Nagoya University Graduate School of Medicine, Nagoya, Japan..
Satoshi Makita, Department of Pediatric Surgery, Nagoya University Graduate School of Medicine, Nagoya, Japan..
Kazuki Yokota, Department of Pediatric Surgery, Nagoya University Graduate School of Medicine, Nagoya, Japan..
Yujiro Tanaka, Department of Pediatric Surgery, Saitama Children's Medical Center, Saitama, Japan..
References:
- 1. Dutta S. Early experience with single incision laparoscopic surgery: eliminating the scar from abdominal operations. J Pediatr Surg. 2009;44:1741–1745. [DOI] [PubMed] [Google Scholar]
- 2. Iranmanesh P, Morel P, Inan I, Hagen M. Choosing the cosmetically superior laparoscopic access to the abdomen: the importance of the umbilicus. Surg Endosc. 2011;25:2578–2585. [DOI] [PubMed] [Google Scholar]
- 3. Cristaudi A, Matthey-Gie ML, Demartines N, Christoforidis D. Prospective assessment of trocar-specific morbidity in laparoscopy. World J Surg. 2014;38:3089–3096. [DOI] [PubMed] [Google Scholar]
- 4. Hong SH, Seo SI, Kim JC, Hwang TK. Rapid communication: cosmetic circumumbilical incision for extraction of specimen after laparoscopic radical prostatectomy. J Endourol. 2006;20:519–521. [DOI] [PubMed] [Google Scholar]
- 5. Casciola L, Codacci-Pisanelli M, Ceccarelli G, Bartoli A, Di Zitti L, Patriti A. A modified umbilical incision for specimen extraction after laparoscopic abdominal surgery. Surg Endosc. 2008;22:784–786. [DOI] [PubMed] [Google Scholar]
- 6. Huang CK, Tsai JC, Lo CH, et al. Preliminary surgical results of single-incision transumbilical laparoscopic bariatric surgery. Obes Surg. 2011;21:391–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blackburn SC, Adams SD, Mahomed AA. A semicircular incision in the superior umbilical fold for SILS preserves the umbilical profile. Minim Invasive Surg. 2012;2012:412623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hachisuka T, Kinoshita T, Yamakawa T, et al. Transumbilical laparoscopic surgery using GelPort through an umbilical zigzag skin incision. Asian J Endosc Surg. 2012;5:50–52. [DOI] [PubMed] [Google Scholar]
- 9. Takasu H, Watanabe Y. Umbilicoplasty with 3 triangular skin flaps and excised diamond-shaped skin flap. J Pediatr Surg. 2010;45:2041–2044. [DOI] [PubMed] [Google Scholar]
- 10. Tamir G, Kurzbart E. Umbilical reconstruction after repair of large umbilical hernia: the “lazy-M” and omega flaps. J Pediatr Surg. 2004;39:226–228. [DOI] [PubMed] [Google Scholar]
- 11. Southwell-Keely JP, Berry MG. Umbilical reconstruction: a review of techniques. J Plast Reconstr Aesthet Surg. 2011;64:803–808. [DOI] [PubMed] [Google Scholar]