Abstract
Understanding the contribution of caregiver feeding practices to adolescent diet and weight is important to refining caregiver roles within the context of adolescent obesity prevention and treatment. This secondary data analysis examined whether feeding practices of female caregivers differentiated persistently non-overweight (n = 29) from persistently obese (n = 47) adolescents. Families who previously participated in a cross-sectional study on correlates of obesity were recruited for this follow-up study. At the time of the follow-up study, anthropometric measures were taken for all female caregivers and adolescents, and caregivers completed the Child Feeding Questionnaire-Adolescent version. Socioeconomic, demographic, female caregiver anthropometric, and psychological (caregiver perceived self-weight and concern for adolescent overweight) variables were examined as predictors of feeding practices found to differentiate the two groups. Female caregivers of persistently obese adolescents reported significantly greater use of restriction and monitoring compared to female caregivers of persistently non-overweight adolescents. Restriction was predicted by female caregiver age and concern for adolescent overweight whereas monitoring was predicted by concern for adolescent overweight only. Caregiver feeding strategies may be an important target for adolescent obesity prevention and intervention efforts particularly among those with heightened concern about their teen’s weight status.
Keywords: Feeding practices, Obesity, Adolescence, Weight control
Introduction
Nearly 35% of adolescents in the United States are currently estimated to be overweight or obese (Ogden, Carroll, Kit, & Flegal, 2014). Despite adolescence being a time of increased autonomy, caregivers continue to influence adolescent lifestyle behaviors and may thus be important concurrent targets for adolescent obesity prevention and intervention programs. This appears especially true for shaping adolescent dietary behaviors given caregiver modeling, provision of healthy food options within the home food environment, and frequent family meals are known correlates of adolescent eating behaviors (e.g., increased fruit and vegetable intake) that may promote a healthy weight (Bauer, Neumark-Sztainer, Hannan, Fulkerson, & Story, 2011; Campbell et al., 2007; Fulkerson, Larson, Horning, & Neumark-Sztainer, 2014; Hanson, Neumark-Sztainer, Eisenberg, Story, & Wall, 2005). These strategies are consistent with what is described by Ogden and colleagues as covert control (Ogden, Reynolds, & Smith, 2006), or strategies parents and caregivers may use to shape adolescent eating behaviors but that are less obvious to teens. It is possible to speculate the unobtrusiveness of these strategies lends to their effectiveness with adolescents, as they do not directly challenge desires for independence.
In contrast, feeding practices like restricting and monitoring intake of highly palatable foods are more obtrusive and direct efforts to control adolescent eating behaviors. Less is known about the use of these more overt controlling feeding practices (Ogden et al., 2006) during adolescence or their potential impact on adolescent weight. A better understanding of these relationships is warranted not only because controlling feeding practices may clash with age-normative assertions for greater independence by adolescents, but also because some controlling feeding practices (e.g., restriction) have been found associated with excess weight gain and obesity promoting behaviors such as eating in the absence of hunger (Birch & Fisher, 2000; Fisher & Birch, 1999a, 1999b) and food hiding (Kenyon, Fulkerson, & Kaur, 2009). Understanding whether and how caregiver foodrelated practices influence adolescent diet and weight may prove critically important to further defining caregiver roles in prevention and treatment of adolescent overweight.
To date, only three studies have examined the relationship between caregiver feeding practices and weight during adolescence (Kaur et al., 2006; Loth, MacLehose, Fulkerson, Crow, & Neumark-Sztainer, 2013b; Sato et al., 2011). Two studies surveyed caregivers of adolescents across the weight spectrum. In the first study, Kaur and colleagues found adolescent body mass index (BMI) was positively associated with caregiver reported use of restriction and inversely associated with pressuring teens to eat (Kaur et al., 2006). No associationswere observed between caregiver monitoring or perceived responsibility for feeding and adolescent weight. Associations between feeding practice use and adolescent weight remained even after controlling for parent ethnicity and BMI and adolescent age and sex. In the second study, Loth and colleagues assessed feeding practice use in one or both parents of adolescent participants (Loth et al., 2013b). Controlling for adolescent race/ethnicity, caregiver BMI, and family household income, caregivers of overweight and obese adolescents were found to report significantly greater use of restriction but significantly less pressuring than caregivers of non-overweight adolescents. Further, while caregiver use of restriction did not differ significantly by adolescent sex, caregivers reported significantly higher use of pressuring for male compared to female adolescents. One study has examined how feeding practice use may impact adolescent weight control efforts. Sato and colleagues found pressuring feeding practices and concern for adolescent overweight accounted for 11% of the variance in BMI changes for overweight and obese adolescents participating in a behavioral weight control intervention (Sato et al., 2011). Adolescents whose caregivers reported higher use of pressuring feeding practices were also significantly less likely to lose >8 pounds than adolescents whose caregivers reported lower use of pressuring feeding practices. Thus, while it appears as though caregiver efforts to control adolescent dietary intake do have some influence on adolescent weight, additional studies are needed to clarify these relationships.
Identifying correlates of feeding practices associated with excess weight gain in adolescence is also important for refining adolescent obesity prevention and intervention efforts.Within the literature for younger children, studies have generally found differences in feeding practice use by caregiver race/ethnicity and socioeconomic status (e.g., Baughcum et al., 2001; Cachelin & Thompson, 2013; Francis, Hofer, & Birch, 2001; Spruijt-Metz, Lindquist, Birch, Fisher, & Goran, 2002). However, findings have been mixed regarding caregiver anthropometric (e.g. McPhie et al., 2011; Powers, Chamberlin, van Schaick, Sherman, & Whitaker, 2006) and other demographic (caregiver and child age; e.g., Gray, Janicke, Wistedt, & Dumont-Driscoll, 2010; Ogden et al., 2006) correlates of feeding practice use. Demographic, socioeconomic, and caregiver anthropometric correlates of feeding have been inconsistently evaluated in the few studies specific to adolescence, with caregiver race/ethnicity and weight status being the only characteristics to be evaluated in more than one study. While the two studies to examine race/ethnicity both reported greater use of restriction and pressuring feeding practices among caregivers from minority compared to White backgrounds (Kaur et al., 2006; Loth, Maclehose, Fulkerson, Crow, & Neumark-Sztainer, 2013a), findings regarding whether caregiver weight status was associated with use of pressuring feeding practices differed (Kaur et al., 2006; Loth et al., 2013a; Sato et al., 2011).
Studies within the literature for younger children have also examined applicability of The Obesity Proneness Model (Costanzo & Woody, 1985) to understanding the relationship between feeding practice use and child weight. This model posits caregivers may change feeding practices based upon perceptions and concerns about their child’s and their own weight and appears to have particular support with respect to use of restricting feeding practices. More specifically, use of restriction has been found to increase in parallel with caregiver concerns for child overweight (Gray et al., 2010; May et al., 2007; Webber, Hill, Cooke, Carnell, & Wardle, 2010), dissatisfaction with their own weight (Gray et al., 2010), and preoccupations and investment in weight more broadly (Cachelin & Thompson, 2013; Francis & Birch, 2005). Surprisingly, these same psychological predictors of caregiver feeding practices have not been evaluated in the adolescent feeding literature. However, one study did find caregiver perceived self-weight was not associated with use of controlling feeding practices (Kaur et al., 2006).
The primary aim of this secondary data analysis was to examine whether caregiver feeding practices differentiated persistently obese from persistently non-overweight adolescents. Based upon the extant literature, we hypothesized that compared to caregivers of non-overweight adolescents, caregivers of persistently obese adolescents would report a) significantly higher use of restrictive feeding practices, b) significantly lower use of pressuring feeding practices, and c) similar levels of monitoring and responsibility for feeding.
Pending outcomes of aim 1, an exploratory aim was to examine socioeconomic, demographic, caregiver anthropometric, and psychological predictors of those feeding practices differentiating the groups for caregivers of persistently obese adolescents. Given the strong predictive value of concern for child overweight on feeding practice use for younger children (Gray et al., 2010;May et al., 2007; Webber et al., 2010), we hypothesized that for caregivers of persistently obese adolescents, concern for adolescent overweightwould account for a significant amount of the variance in feeding practice use above and beyond that accounted for by socioeconomic and demographic characteristics (adolescent age and sex, family ethnicity, and female caregiver age) and caregiver BMI. While we did not assess caregiver dissatisfaction with their own weight or caregiver preoccupations and investment with weight (psychological variables), we did measure caregiver perception of self-weight. Caregiver perception of self-weight was thus included in a separate step because it could be influenced by socioeconomic, demographic, and anthropometric characteristics and because it has the potential to influence caregiver concern for adolescent overweight.
Methods
Participants
Adolescents and their primary caregivers who previously participated in a cross-sectional study with a comparison group that examined youth and family correlates of pediatric obesity were recruited for a follow-up study approximately 4 years later if the youth remained under the age of 19 years old. For the initial study (Zeller et al., 2007; Zeller, Reiter-Purtill, & Ramey, 2008), youth with obesity (BMI = 95th percentile) and their primary caregiver were recruited from a hospital-based pediatric weight management clinic if youth were: a) ages 8 to 16 years old, b) not homeschooled or receiving full-time special education, and c) living within 60 miles of the hospital. A non-overweight comparison youth was recruited from the classroom of each treatment-seeking obese youth who enrolled in the initial study.
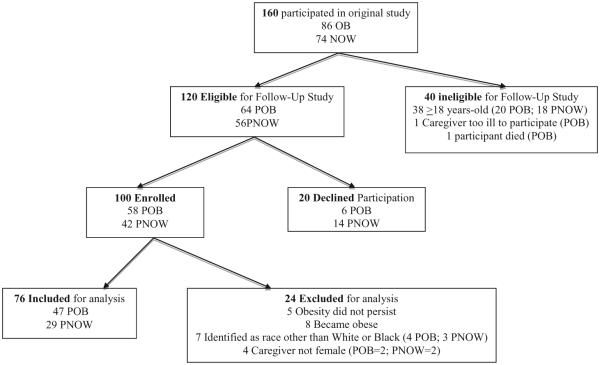
Detailed information regarding recruitment for the present, crosssectional follow-up study by adolescent weight status is presented in Fig. 1. Given the aims of this secondary data analysis, adolescentswere excluded if theirweight status changed since participation in the initial study (n = 13). As the overwhelming majority of caregivers self-identified themselves as either non-Hispanic White or African-American and were female, dyads where caregivers were of other races or male were also excluded (n = 11). Sample characteristics for the final sample of 76 adolescent–female caregiver dyads (47 persistently obese and 29 persistently non-overweight) are presented in Table 1.
Fig. 1.
Recruitment summary. Note: OB, obese; NOW, non-overweight; POB, persistently obese; PNOW, persistently non-overweight.
Table 1.
Sample characteristics.
| Non-overweight (n = 29) |
Persistently obese (n = 47) |
t | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Adolescent | |||||
| Age(years) | 16.16 | 1.22 | 15.97 | 1.29 | −0.65 |
| BMI z-score** | −0.02 | 0.76 | 2.46 | 0.37 | 19.19 |
| Female | 52% | 55% | 0.76a | ||
| Female caregiver | |||||
| Age (years) | 43.66 | 8.46 | 44.84 | 7.34 | 0.62 |
| BMI** | 26.63 | 6.97 | 35.60 | 10.04 | 4.22 |
| White | 59% | 49% | 0.41a | ||
| Family | |||||
| SES*,b | 54.40 | 22.72 | 43.40 | 22.84 | −2.04 |
| Single caregiver home | 75.9% | 53% | 0.48a | ||
SD, standard deviation.
Based on two-tailed independent t tests,
p < 0.05,
p < 0.01.
Chi-square value, nonsignificant.
SES, socioeconomic status; based on Duncan TSE12. Higher score indicates greater occupational attainment.
Procedure
Informed consent and assent were obtained from all caregivers and adolescents who expressed interest in participating in the follow-up study. Measures were administered by trained research staff at participants’ homes or in a clinical research space at the host institution. An Institutional Review Board approved the larger study from which the secondary data presented in this manuscript were obtained.
Measures
Only data collected during the follow-up study are presented in this paper. The Child Feeding Questionnairewas administered during the follow-up study only.
Demographic information
Female primary caregivers completed a self-report measure that assessed caregiver and adolescent age, sex, and race, aswell as family composition (one or two caregivers), highest education level obtained, and occupation for all caregivers in the home. Family socioeconomic status (SES) was determined using the Revised Duncan score (Nakao & Treas, 1989; Stevens & Featherman, 1981), which is an occupation-based measure of SES (Mueller & Parcel, 1981). If adolescents were from a two-caregiver home, then the highest Duncan score within the caregiver set was included for analysis.
Anthropometric measures
Height and weight for adolescents and female caregivers were measured by trained personnel using standard procedures (Cameron, 1986). Measures were obtained with participants wearing street clothing and without shoes using a calibrated custom portable stadiometer (Creative Health Products, Plymouth, MI) and a portable SECA digital scale (SECA, Hamburg, Germany). Measurements were taken in triplicate and the means were used to calculate Body Mass Index (BMI: kg/m2). BMI z-score values were calculated for adolescent participants using age- (to the nearest month) and sexspecific median, standard deviation, and power of the Box–Cox transformation (LMS method) based on national norms from the Centers for Disease Control (Kuczmarski et al., 2000).
Child Feeding Questionnaire-Adolescent Version
The Child Feeding Questionnaire-Adolescent Version (CFQ-A; Kaur et al., 2006) is a 27-item questionnaire assessing caregiverreport of controlling feeding practices, perception of weight, and concern about adolescent weight. Similar to the 31-item Child Feeding Questionnaire (Birch et al., 2001) fromwhich it was derived, the CFQ-A asks caregivers to use a 5-point Likert scale to rate how much they agree with statements (“disagree” to “agree”) or use specific practices (“never” to “always”) for items corresponding to the four controlling feeding practice scales: Restriction (six items, e.g., “I have to watch out that my teen does not eat too much of his/her favorite foods), Monitoring (four items, e.g., “How much do you keep track of the snack food (potato chips, cheese puffs, etc.) that your teen eats?”), Pressure to Eat (four items, e.g., “My teen should always eat all of the food on his/her plate”), and Responsibility for Feeding (three items, e.g., “How often are you responsible for deciding what your teen’s portion sizes are?”). Different response choices (“unconcerned” to “very concerned” and “very underweight” to “very overweight”) are used for items corresponding to the three scales describing the caregiver’s perception of their adolescent’s obesity proneness: Concern for Adolescent Overweight (three items, e.g., “How concerned are you about your teen maintaining a desirable weight?”), Perceived Parent Self- Weight (four items; “your adolescence”), and Perceived Adolescent Weight (three items; “your teen from 3rd to 5th grade was. . .”). Internal consistency alpha values for the CFQ-A subscales in the current sample were similar to those reported in the literature (Kaur et al., 2006; Kenyon et al., 2009; Loth et al., 2013a): Restriction (α = 0.92), Monitoring (α = 0.95), Pressuring to Eat (α = 0.62), Responsibility for Feeding (α = 0.68), Perceived Parent Self-Weight (α = 0.80), Perceived AdolescentWeight (α = 0.85), and Concern for Adolescent Overweight (α = 0.88).
Preliminary analyses and statistical analysis plan
Persistently obese and non-overweight adolescents differed significantly on the variables of family SES and maternal BMI (see Table 1), so these variableswere entered as covariates in all betweengroups analyses. A multivariate analysis of covariance (MANCOVA) was used to examine between-groups differences on the CFQ-A. If the MANCOVA was significant, then univariate ANCOVAs were applied to examine between groups differences for each CFQ-A scale separately. Step-wise, hierarchical linear regression analyses were applied to examine predictors of those feeding practices differentiating the two groups in the persistently obese sample only. Within these regression models, caregiver and adolescent socioeconomic and demographic variables (adolescent and caregiver age, adolescent sex, family SES and race/ethnicity) and female caregiver BMI were entered in step one, perceived caregiver self-weightwas entered in step two, and female caregiver concern about adolescent weight statuswas entered into step three. All analyseswere conducted using SPSS version 22.0 (SPSS Inc., Chicago, IL).
Results
Results of the MANCOVA were significant [(F1, 46) = 27.02, p < 0.001]. Summary statistics for univariate ANCOVAs for all scales of the CFQ-A are presented in Table 2.
Table 2.
Between-groups comparisons of child feeding questionnaire-adolescent scales.
| Non-overweight (n = 29) |
Persistently obese (n = 47) |
F | |||
|---|---|---|---|---|---|
| Meana | SE | Meana | SE | ||
| Feeding practices | |||||
| Restriction** | 2.03 | 0.23 | 3.78 | 0.17 | 34.09 |
| Pressure to Eat | 1.96 | 0.17 | 1.60 | 0.13 | 2.78 |
| Monitoring* | 2.61 | 0.23 | 3.32 | 0.17 | 5.67 |
| Perceived Responsibility for Feeding | 3.11 | 0.16 | 3.03 | 0.12 | 0.15 |
| Perceived weight | |||||
| Perceived Adolescent Weight** | 2.78 | 0.10 | 4.06 | 0.07 | 101.64 |
| Perceived Parent Self-Weight | 3.42 | 0.11 | 3.33 | 0.09 | 0.31 |
| Concern for Adolescent Weight** | 1.85 | 0.20 | 4.28 | 0.15 | 8789 |
Based on analyses of variance with covariates including female caregiver BMI and family SES.
p < 0.05,
p < 0.001.
Adjusted means.
Perception of adolescent obesity proneness
Caregivers of persistently obese adolescents perceived teens to be significantly heavier andwere significantly more concerned about their adolescent’s weight compared to caregivers of adolescents who were persistently non-overweight (both scales p < 0.001). Despite their significantly higher BMI, female caregivers of persistently obese adolescents did not perceive themselves to be any different from caregivers of persistently non-obese adolescents with respect to weight status (p = 0.58).
Feeding practices differentiating persistently obese and non-overweight adolescents
As hypothesized, female caregivers of persistently obese adolescents self-reported significantly higher use of restriction (p < 0.001) but did not differ significantly on responsibility for feeding (p = 0.70) compared to caregivers of persistently non-overweight adolescents. In contrast to our hypothesis, caregivers of persistently obese adolescents reported significantly higher use of monitoring (p < 0.05) and did not differ significantly in their use of pressuring feeding practices (p = 0.10) from caregivers of persistently non-overweight adolescents.
Predictors of restriction and monitoring in caregivers of persistently obese adolescents
Based upon the above findings, hierarchical linear regression analyses were conducted to examine whether caregiver concern for adolescent weight accounted for unique variance in caregiver use of restriction or monitoring above and beyond caregiver and adolescent socioeconomic an demographic characteristics, caregiver BMI, and caregiver perception of own weight status. These analyses were completed for caregivers of persistently obese adolescents only (Table 3).
Table 3.
Regression analysis summary of predictors of restriction and monitoring in caregivers of persistently obese adolescents (n = 47).
| B | SE B | β | 95% Confidence interval (B) | |
|---|---|---|---|---|
| Restriction | ||||
| Step One | ||||
| Female caregiver age | 0.06 | 0.02 | 0.40** | 0.02,0.11 |
| Female caregiver BMI | −0.03 | 0.02 | −0.26 | −0.07, 0.01 |
| Female caregiver Racea | 0.42 | 0.39 | 0.18 | −0.36, 1.20 |
| Adolescent age | −0.21 | 0.12 | −0.22 | −0.49, 0.07 |
| Adolescent sexa | −0.23 | 0.32 | −0.10 | −0.88, 0.42 |
| Family SES | 0.00 | 0.01 | 0.06 | −0.02, 0.02 |
| Step Two | ||||
| Female caregiver perceived self-weight | 0.34 | 0.30 | 0.21 | −0.26, 0.94 |
| Step Three | ||||
| Concern for youth weight | 0.93 | 0.13 | 0.71*** | 0.66, 1.19 |
| Monitoring | ||||
| Step One | ||||
| Female caregiver age | 0.04 | 0.02 | 0.29 | −0.00, 0.08 |
| Female caregiver BMI | −0.03 | 0.02 | −0.29 | −0.07, 0.01 |
| Female caregiver racea | 0.05 | 0.36 | −0.02 | −0.78, 0.69 |
| Adolescent age | −0.22 | 0.13 | −0.27 | −0.48, 0.05 |
| Adolescent sexa | −0.25 | 0.30 | −0.20 | −0.86, 0.36 |
| Family SES | −0.01 | 0.01 | −0.20 | −0.03, 0.01 |
| Step Two | ||||
| Female caregiver perceived self-weight | 0.50 | 0.28 | 0.35 | −0.06, 1.05 |
| Step Three | ||||
| Concern for youth weight | 0.68 | 0.15 | 0.60*** | 0.37, 0.98 |
R2 = 0.31 for Restriction Step 1 (p < .05); ΔR2 = 0.02 for Restriction Step 2 (p < .05); ΔR2 = 0.64 for Restriction Step 3 (p < .001).
R2 = 0.17 for Monitoring Step 1 (p > .05); ΔR2 = 0.06 for Monitoring Step 2 (p > .05); ΔR2 = 0.39 for Monitoring Step 3 (p < .001).
p < .01,
p < .001.
Sex (female = 1, male = 0) and race (Black = 1, White = 0) are categorical variables.
Restriction
Step one revealed that caregiver age was a significant predictor of caregiver restrictive feeding practice use (R2 = 0.29, F6,46 = 2.74, p < 0.05) such that older caregivers reported higher use of restrictive feeding practices. While Step two overall was found to be significant (R2Δ = 0.02, F7,46 = 2.55, p < 0.05), caregiver perceived self-weight was not found to be a significant predictor of caregiver use of restriction (p = 0.26). Caregiver concern for adolescent overweight accounted for an additional 39% of the variance in caregiver use of restrictive feeding practices (R2Δ = 0.39, F8,46 = 11.42, p < 0.001). More specifically, caregivers utilized more restrictive feeding practices as their concern about adolescent weight status increased.
Monitoring
Step one revealed caregiver and adolescent socioeconomic and demographic variables did not predict caregiver use of monitoring (R2 = 0.17, F6,46 = 1.35, p = 0.26). Step two indicated that caregiver perception of own weight status was also not a significant predictor of caregiver monitoring (R2Δ = 0.07, F7,46 = 1.76, p = 0.06). Step three revealed concern for adolescent weight was a significant predictor and accounted for 27% of the variance in monitoring after controlling for caregiver and adolescent socioeconomic and demographic characteristics, caregiver BMI, and caregiver perception of self-weight (R2Δ = 0.27, F8,46 = 4.94, p < 0.001). More specifically, caregivers increased their monitoring of adolescent intake of highly palatable foods and sugar-sweetened beverages as their concern for adolescent overweight increased.
Discussion
Understanding whether and how caregiver feeding practices influence adolescent weight is important to defining caregiver roles in adolescent weight management efforts. Despite a significant literature on feeding and weight in early childhood, few studies have explored this relationship during adolescence. Our study addresses this gap and is the first to examine this relationship among caregivers of adolescents whose weight status (obese or non-overweight) was known to persist for at least 4 years. Caregivers of persistently obese adolescents reported significantly greater restriction and monitoring of their teen’s intake of highly palatable foods compared to caregivers of persistently non-overweight adolescents. Use of controlling feeding practices at this later time was predicted most strongly by concern for adolescent overweight, with caregivers of persistently obese adolescents reporting greater use of controlling feeding practices as concern about their teen’s weight increased. Irrespective of adolescent weight, caregivers reported sharing feeding responsibilities (e.g., preparing food and determining portion sizes) with teens and rarely pressuring them to eat. Our findings thus suggest that caregivers of persistently obese adolescents allow teens more independence in controlling how much food they consumed but take a more overtly controlling approach to regulation of their high-calorie foods and beverage intake.
As hypothesized, and consistent with the adolescent feeding literature (Kaur et al., 2006; Loth et al., 2013b), caregivers of persistently obese adolescents reported significantly greater use of restrictive feeding practices compared to caregivers of non-overweight adolescents. Interestingly, mean values for caregiver use of restriction in our sample of treatment-seeking persistently obese adolescents did not differ significantly from those reported by caregivers of non-treatment seeking adolescents with obesity (data not shown; Kenyon et al., 2009). Restriction of adolescent intake of highly palatable foods may seem an intuitive feeding strategy to a caregiver of a teen with obesity, especiallywhen excessweight persists despite seeking treatment. However, use of this feeding practice has unintended negative consequences like increasing preferences for restricted foods and their consumption when accessible, even in the absence of self-reported hunger (Birch, Fisher, & Davison, 2003; Fisher & Birch, 1999a, 1999b). Further, in the adolescent literature, restriction has been found associated with food hiding in overweight and obese adolescents (Kenyon et al., 2009) and extreme weight control behaviors in adolescents across the weight spectrum (Loth, MacLehose, Fulkerson, Crow, & Neumark-Sztainer, 2014).
Given reductions in caregiver use of restrictive feeding practices have been found associated with obesity reduction in schoolaged children (Epstein, Paluch, Beecher, & Roemmich, 2008; Holland et al., 2014), a more adaptive strategy may be to aid teens on how to consume energy-dense, highly palatable foods in moderation. For example, rather than serving energy-dense foods at home, intake of these choices could be reserved for social events and time spent with peers where it may be harder for adolescents with obesity to pass on these choices if they are being consumed by others. Caregivers could work with teens to determine healthier choices and strategies for portion control (e.g., share with a friend) a priori. Further, given that nearly 40% of adolescents have a smartphone (Madden, Lenhart, Duggan, Cortesi, & Gasser, 2013), caregivers could encourage teens to use nutrition applications or read nutrition information on food establishment websites if pre-planning is not possible.
In contrast to our hypothesis, caregivers of persistently obese adolescents reported greater monitoring of their teen’s diet relative to caregivers of persistently non-overweight adolescents. This finding was surprising for two reasons. First, it differs from Kaur et al. (2006) who found no association between monitoring and weight in their adolescent sample where nearly half of participating caregivers had an overweight or obese teen. Second, one might expect caregiver monitoring to decrease over time in the absence of teen weight loss. Among caregivers of persistently obese adolescents in our sample, use of monitoring was found to be significantly, positively associated with use of restriction (r = 0.78, p < .001). It is thus possible to speculate that as concern increases, so too does caregiver use of controlling feeding practices more broadly. Increased use of these more overtly controlling feeding practices may result in negative caregiverdyad interactions around consumption of highly palatable foods, which could be especially counter-productive for teens that are struggling in their efforts to control weight. A balance must be achieved between supporting teens’ independent efforts and ensuring caregivers have information on teens’ progress in making behavior changes that support achieving a healthy weight. Goal setting and self monitoring, key components of social cognitive theory of selfregulation (Bandura, 1991), may be effective approaches given positive associations found between use of this behavior change strategy and weight control for adolescents (Saelens & McGrath, 2003) and adults (Baker & Kirschenbaum, 1993; Boutelle & Kirschenbaum, 1998). Caregiver involvement could be limited to reviewing monitoring records with teens and problem-solving as needed at a pre-set time each week. This approach would encourage teen independence, minimize what might be perceived by teens as nagging by their caregivers, and promote supportive discussions about regulation of dietary intake.
Our hypotheses regarding caregiver use of pressuring feeding practices and responsibility for feeding were partially supported. While contrasting the adolescent (Kaur et al., 2006; Loth et al., 2013b) and pediatric literature more broadly (Francis et al., 2001; Keller, Pietrobelli, Johnson, & Faith, 2006; Matheson, Robinson, Varady, & Killen, 2006; Powers et al., 2006; Spruijt-Metz et al., 2002), our finding that caregivers of persistently obese adolescents reported similarly low levels of pressuring teens to eat as caregivers of non-overweight teens is positive as this feeding practice has been found associated with poorer weight outcomes for adolescents participating in a weight control intervention (Sato et al., 2011), unhealthy and extreme dieting behaviors in adolescent males of varying weight statuses (Loth et al., 2014), and higher caloric intake in observational studies with younger children (Campbell, Crawford, & Ball, 2006; Klesges, Mallott, Boschee, & Weber, 1986). However, provision of the same degree of feeding responsibility by caregivers to persistently obese teens as non-overweight teens may not be a strategy that promotes weight loss. For example, if teens are unaware of portion sizes and the caloric content of their food and beverage choices, then ensuring they have the necessary foundation of skills to make healthy choices is an important step in promoting their autonomy in making healthy dietary decisions. While caregiver modeling appears important to shaping healthy dietary behaviors for adolescents, family-based intervention regarding portion sizes and healthy food preparation techniques may be necessary for obese teens to fully experience the benefits of this strategy given the high propensity (including within the present study) for obese children to also have at least one parent who is also obese. Given caregivers are still largely responsible for grocery shopping and subsequently determining which foods and beverages will be available in the home, stimulus control is another covert control strategy caregivers can employ to support teens in making healthy dietary choices (Hanson et al., 2005).
Finally, our findings extend the literature on younger pediatric age-groups demonstrating caregiver concern for child overweight as a strong predictor of controlling feeding practice use even during adolescence. Validation of caregiver concern is likely a crucial first step for health care providers and, when supplemented with findings regarding the contraindications of controlling feeding practice from the literature, could be used as a platform for teaching feeding practices that may better help caregivers to support adolescents in their weight control efforts. Caregiver age (older) was the only predictor of feeding practice use beyond concern for adolescent weight, and was limited to our model for restriction. This finding was surprising as it contrasts other studies in the adolescent literature where race/ethnicity, income, adolescent age and sex, and caregiver sex and weight status have been found associated with caregiver use of restrictive feeding practices (Kaur et al., 2006; Loth et al., 2013a, 2013b; Sato et al., 2011). We also did not find that caregiver perception of self-weight predicted use of restriction or monitoring feeding practices.
Our study builds upon an emergent literature examining the relationship between caregiver feeding practices and adolescentweight and has several strengths. The larger study from which these data originated provided a unique opportunity to examine feeding practices in treatment-seeking youth whose weight status (obese or non-overweight) was known to persist over several years. The diversity of our sample with respect to sex and race also allowed us to better examine the influence of these demographic variables on caregiver feeding practice use. Finally, our study further validates use of the CFQ-A, which is important for examining the role of feeding practices on weight across child development.
Despite these strengths, our study was not without limitations and consequent directions for future research. Caregivers of persistently obese adolescents in our sample had previously participated in a weight management program for their teens, so it is possible that caregivers reported more frequent monitoring and restricting of unhealthy foods because they believed this was in line with prior treatment recommendations. Findings should also be considered preliminary given our relatively small sample size. Replication with a larger sample will prove informative. Given the cross-sectional design of the present study, future investigations including longitudinal and randomized controlled designs are needed to address causality of the relationship between caregiver feeding practice use and adolescent weight. Due to the limited number of male caregivers, our study examined feeding practices of female caregivers only. Future research should examine feeding practice use for all caregivers within the adolescents’ home environment, given studies have found differences by parent sex (Loth et al., 2013b). We also did not examine adolescent perception of caregiver feeding practice use. However, findings that adolescent perception of maternal use of restrictive feeding practices were associated with adolescent reported inability to self-regulate eating (Nickelson, Bryant, McDermott, Buhi, & Debate, 2012) suggest that understanding caregiver feeding practices from teens’ perspective is an important area for future research. Finally, the inclusion of an assessment of the adolescent’s dietary intake and the home food environment would provide a more definitive measure of adolescent eating behaviors from which to examine links to caregiver feeding practices.
Conclusions
Our study provides preliminary evidence that caregiver feeding practices may be an important target within the context of adolescent weight control efforts, particularly among those who express great concern about their adolescent’s weight status. Caregivers of persistently obese adolescents in our sample reported significantly greater restriction and monitoring of their teen’s intake of high-calorie, high-fat foods. Use of these overtly controlling feeding practices increased in parallel with caregiver concerns about adolescent overweight. Tightening control of highly palatable foods may make sense to a caregiver who is concerned about their teen’s weight, especially in our sample where adolescent obesity persisted despite seeking treatment for weight loss. However, the literature suggests controlling feeding practices, restriction in particular, may result in development of eating behaviors that promote instead of reduce weight gain. Increased caregiver use of overtly controlling feeding practices also contrasts with normative adolescent desires for independence and could hamper shaping the adaptive eating behaviors that are necessary to promote positive weight management that will be maintained in early adulthood when teens truly are “on their own.” Additional work is needed to better delineate the relationship between caregiver feeding practices, eating, and weight during adolescent to refine the role of caregivers in adolescent weight control efforts.
Footnotes
Acknowledgments: This research was funded by the National Institutes of Health through a post-doctoral training grant from the National Institutes of Health (T32 DK063929) supporting the first and second authors as well as career development awards (K23-DK087826 K23-DK60031) awarded to the third and final authors respectively. We extend our thanks to the families who participated in this study. We would also like to thank the research assistants and summer students who were instrumental in recruiting participants and collecting data including Christina Ramey, LindsayWilson, Carrie Piazza-Waggoner, Julie Koumoutsos, Sarah Valentine, Stephanie Ridel, Kate Grampp, Ambica Tumkur, Rachel Jordan, Matt Flanigan, and Neha Godiwala.
Conflict of interest: The authors wish to report that they have no financial disclosures or competing interests.
References
- Baker RC, Kirschenbaum DS. Self-monitoring may be necessary for successful weight control. Behavior Therapy. 1993;24(3):377–394. [Google Scholar]
- Bandura A. Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes. 1991;50:248–271. [Google Scholar]
- Bauer KW, Neumark-Sztainer D, Hannan PJ, Fulkerson JA, Story M. Relationships between the family environment and school-based obesity prevention efforts. Can school programs help adolescents who are most in need? Health Education Research. 2011;26(4):675–688. doi: 10.1093/her/cyr027. doi:10.1093/her/cyr027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baughcum AE, Powers SW, Johnson SB, Chamberlin LA, Deeks CM, Jain A, et al. Maternal feeding practices and beliefs and their relationships to overweight in early childhood. Journal of Developmental and Behavioral Pediatrics. 2001;22(6):391–408. doi: 10.1097/00004703-200112000-00007. [DOI] [PubMed] [Google Scholar]
- Birch LL, Fisher JO. Mothers’ child-feeding practices influence daughters’ eating and weight. The American Journal of Clinical Nutrition. 2000;71(5):1054–1061. doi: 10.1093/ajcn/71.5.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL, Fisher JO, Davison KK. Learning to overeat. Maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. The American Journal of Clinical Nutrition. 2003;78(2):215–220. doi: 10.1093/ajcn/78.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire. A measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36(3):201–210. doi: 10.1006/appe.2001.0398. doi:10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- Boutelle KN, Kirschenbaum DS. Further support for consistent self-monitoring as a vital component of successful weight control. Obesity Research. 1998;6(3):219–224. doi: 10.1002/j.1550-8528.1998.tb00340.x. [DOI] [PubMed] [Google Scholar]
- Cachelin FM, Thompson D. Predictors of maternal child-feeding practices in an ethnically diverse sample and the relationship to child obesity. Obesity. 2013;21(8):1676–1683. doi: 10.1002/oby.20385. doi:10.1002/oby.20385. [DOI] [PubMed] [Google Scholar]
- Cameron N. The methods of auxological anthropometry. In: Falkner F, Tanner JM, editors. Human growth. 2nd Vol. 3. Plenum Press; New York, NY: 1986. pp. 3–43. [Google Scholar]
- Campbell KJ, Crawford DA, Ball K. Family food environment and dietary behaviors likely to promote fatness in 5-6 year-old children. International Journal of Obesity (2005) 2006;30(8):1272–1280. doi: 10.1038/sj.ijo.0803266. doi:10.1038/sj.ijo.0803266. [DOI] [PubMed] [Google Scholar]
- Campbell KJ, Crawford DA, Salmon J, Carver A, Garnett SP, Baur LA. Associations between the home food environment and obesity-promoting eating behaviors in adolescence. Obesity. 2007;15(3):719–730. doi: 10.1038/oby.2007.553. doi:10.1038/oby.2007.553. [DOI] [PubMed] [Google Scholar]
- Costanzo PR, Woody EZ. Domain specific parenting styles and their impact on the child’s development of particular deviance. The example of obesity proneness. Journal of Social and Clinical Psychology. 1985;3:425–445. [Google Scholar]
- Epstein LH, Paluch RA, Beecher MD, Roemmich JN. Increasing healthy eating vs. reducing high energy-dense foods to treat pediatric obesity. Obesity. 2008;16(2):318–326. doi: 10.1038/oby.2007.61. doi:10.1038/oby.2007.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Restricting access to foods and children’s eating. Appetite. 1999a;32(3):405–419. doi: 10.1006/appe.1999.0231. doi:10.1006/appe.1999.0231. [DOI] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Restricting access to palatable foods affects children’s behavioral response, food selection, and intake. The American Journal of Clinical Nutrition. 1999b;69(6):1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- Francis LA, Birch LL. Maternal weight status modulates the effects of restriction on daughters’ eating and weight. International Journal of Obesity. 2005;29(8):942–949. doi: 10.1038/sj.ijo.0802935. doi:10.1038/sj.ijo.0802935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis LA, Hofer SM, Birch LL. Predictors of maternal child-feeding style. Maternal and child characteristics. Appetite. 2001;37(3):231–243. doi: 10.1006/appe.2001.0427. doi:10.1006/appe.2001.0427. [DOI] [PubMed] [Google Scholar]
- Fulkerson JA, Larson N, Horning M, Neumark-Sztainer D. A review of associations between family or shared meal frequency and dietary and weight status outcomes across the lifespan. Journal of Nutrition Education and Behavior. 2014;46(1):2–19. doi: 10.1016/j.jneb.2013.07.012. doi:10.1016/j.jneb.2013.07.012. [DOI] [PubMed] [Google Scholar]
- Gray WN, Janicke DM, Wistedt KM, Dumont-Driscoll MC. Factors associated with parental use of restrictive feeding practices to control their children’s food intake. Appetite. 2010;55(2):332–337. doi: 10.1016/j.appet.2010.07.005. doi:10.1016/j.appet.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Hanson NI, Neumark-Sztainer D, Eisenberg ME, Story M, Wall M. Associations between parental report of the home food environment and adolescent intakes of fruits, vegetables and dairy foods. Public Health Nutrition. 2005;8(1):77–85. doi: 10.1079/phn2005661. [DOI] [PubMed] [Google Scholar]
- Holland JC, Kolko RP, Stein RI, Welch RR, Perri MG, Schechtman KB, et al. Modifications in parent feeding practices and child diet during family-based behavioral treatment improve child zBMI. Obesity. 2014;22(5):E119–E126. doi: 10.1002/oby.20708. doi:10.1002/oby.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur H, Li C, Nazir N, Choi WS, Resnicow K, Birch LL, et al. Confirmatory factor analysis of the child-feeding questionnaire among parents of adolescents. Appetite. 2006;47(1):36–45. doi: 10.1016/j.appet.2006.01.020. doi:10.1016/j.appet.2006.01.020. [DOI] [PubMed] [Google Scholar]
- Keller KL, Pietrobelli A, Johnson SL, Faith MS. Maternal restriction of children’s eating and encouragements to eat as the ‘non-shared environment’. A pilot study using the child feeding questionnaire. International Journal of Obesity (2005) 2006;30(11):1670–1675. doi: 10.1038/sj.ijo.0803318. doi:10.1038/sj.ijo.0803318. [DOI] [PubMed] [Google Scholar]
- Kenyon DB, Fulkerson JA, Kaur H. Food hiding and weight control behaviors among ethnically diverse, overweight adolescents. Associations with parental food restriction, food monitoring, and dissatisfaction with adolescent body shape. Appetite. 2009;52(2):266–272. doi: 10.1016/j.appet.2008.10.004. doi:10.1016/j.appet.2008.10.004. [DOI] [PubMed] [Google Scholar]
- Klesges RC, Mallott JM, Boschee PF, Weber JM. The effects of parental influences on children’s food intake, physical activity, and relative weight. International Journal of Eating Disorders. 1986;5:859–864. [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC growth charts. United States. Advance Data. 2000;314:1–27. [PubMed] [Google Scholar]
- Loth KA, Maclehose RF, Fulkerson JA, Crow S, Neumark-Sztainer D. Eat this, not that! Parental demographic correlates of food-related parenting practices. Appetite. 2013a;60(1):140–147. doi: 10.1016/j.appet.2012.09.019. doi:10.1016/j.appet.2012.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loth KA, MacLehose RF, Fulkerson JA, Crow S, Neumark-Sztainer D. Food-related parenting practices and adolescent weight status. A population-based study. Pediatrics. 2013b;131(5):e1443–e1450. doi: 10.1542/peds.2012-3073. doi:10.1542/peds.2012-3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loth KA, MacLehose RF, Fulkerson JA, Crow S, Neumark-Sztainer D. Are food restriction and pressure-to-eat parenting practices associated with adolescent disordered eating behaviors? International Journal of Eating Disorders. 2014;47(3):310–314. doi: 10.1002/eat.22189. doi:10.1002/eat.22189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden M, Lenhart A, Duggan M, Cortesi S, Gasser U. Teens and Technology 2013. 2013 http://www.pewinternet.org/2013/03/13/teens-and -technology-2013/
- Matheson DM, Robinson TN, Varady A, Killen JD. Do Mexican-American mothers’ food-related parenting practices influence their children’s weight and dietary intake? Journal of the American Dietetic Association. 2006;106(11):1861–1865. doi: 10.1016/j.jada.2006.08.004. doi:10.1016/j.jada.2006.08.004. [DOI] [PubMed] [Google Scholar]
- May AL, Donohue M, Scanlon KS, Sherry B, Dalenius K, Faulkner P, et al. Child-feeding strategies are associated with maternal concern about children becoming overweight, but not children’s weight status. Journal of the American Dietetic Association. 2007;107(7):1167–1175. doi: 10.1016/j.jada.2007.04.009. doi:10.1016/j.jada.2007.04.009. [DOI] [PubMed] [Google Scholar]
- McPhie S, Skouteris H, McCabe M, Ricciardelli LA, Milgrom J, Baur LA, et al. Maternal correlates of preschool child eating behaviours and body mass index. A cross-sectional study. International Journal of Pediatric Obesity. 2011;6(5–6):476–480. doi: 10.3109/17477166.2011.598937. doi:10.3109/17477166.2011.598937. [DOI] [PubMed] [Google Scholar]
- Mueller CW, Parcel TL. Measures of socioeconomic status. Alternatives and recommendations. Child Development. 1981;52:13–20. [Google Scholar]
- Nakao K, Treas J. The 1989 socioeconomic index of occupations. Construction from the 1989 occupational prestige scores. University of Chicago, National Opinion Research Center; Chicago, IL: 1989. [Google Scholar]
- Nickelson J, Bryant CA, McDermott RJ, Buhi ER, Debate RD. A modified obesity proneness model predicts adolescent weight concerns and inability to self-regulate eating. Journal of School Health. 2012;82(12):560–571. doi: 10.1111/j.1746-1561.2012.00737.x. doi:10.1111/j.1746-1561.2012.00737.x. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. Journal of the American Medical Association. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. doi:10.1001/jama. 2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden J, Reynolds R, Smith A. Expanding the concept of parental control. A role for overt and covert control in children’s snacking behaviour? Appetite. 2006;47(1):100–106. doi: 10.1016/j.appet.2006.03.330. doi:10.1016/j.appet.2006.03.330. [DOI] [PubMed] [Google Scholar]
- Powers SW, Chamberlin LA, van Schaick KB, Sherman SN, Whitaker RC. Maternal feeding strategies, child eating behaviors, and child BMI in low-income African-American preschoolers. Obesity. 2006;14(11):2026–2033. doi: 10.1038/oby.2006.237. doi:10.1038/oby.2006.237. [DOI] [PubMed] [Google Scholar]
- Saelens BE, McGrath AM. Self-monitoring adherence and adolescent weight control efficacy. Children’s Health Care. 2003;32(2):137–152. [Google Scholar]
- Sato AF, Jelalian E, Hart CN, Lloyd-Richardson EE, Mehlenbeck RS, Neill M, et al. Associations between parent behavior and adolescent weight control. Journal of Pediatric Psychology. 2011;36(4):451–460. doi: 10.1093/jpepsy/jsq105. doi:10.1093/jpepsy/jsq105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruijt-Metz D, Lindquist CH, Birch LL, Fisher JO, Goran MI. Relation between mothers’ child-feeding practices and children’s adiposity. The American Journal of Clinical Nutrition. 2002;75(3):581–586. doi: 10.1093/ajcn/75.3.581. [DOI] [PubMed] [Google Scholar]
- Stevens G, Featherman DL. A revised socioeconomic index of occupational status. Social Science Research. 1981;10:364–395. [Google Scholar]
- Webber L, Hill C, Cooke L, Carnell S, Wardle J. Associations between child weight and maternal feeding styles are mediated by maternal perceptions and concerns. European Journal of Clinical Nutrition. 2010;64(3):259–265. doi: 10.1038/ejcn.2009.146. doi:10.1038/ejcn.2009.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller MH, Reiter-Purtill J, Modi AC, Gutzwiller J, Vannatta K, Davies WH. Controlled study of critical parent and family factors in the obesigenic environment. Obesity. 2007;15(1):126–136. doi: 10.1038/oby.2007.517. doi:10.1038/oby.2007.517. [DOI] [PubMed] [Google Scholar]
- Zeller MH, Reiter-Purtill J, Ramey C. Negative peer perceptions of obese children in the classroom environment. Obesity. 2008;16(4):755–762. doi: 10.1038/oby.2008.4. doi:10.1038/oby.2008.4. [DOI] [PMC free article] [PubMed] [Google Scholar]