Abstract
Purpose
To identify radiographic and MR features of hip osteoarthritis (OA) related to reduced hip extension during walking.
Methods
Sixty six subjects, were stratified into those with (n = 36, KL = 2, 3) and without (n = 30, KL = 0, 1) radiographic hip OA. Cartilage and labrum lesions were graded semi-quantitatively on hip MRI. Alpha angle and lateral center edge (LCE) angle were measured. Sagittal kinematics and kinetics were calculated during walking at speed of 1.3 m/sec using 3-D motion capture. All subjects completed Hip disability and Osteoarthritis Outcome Score (HOOS), timed up and go, and 6 minute walk tests. Variables were compared between the two groups using one-way ANOVA (adjusting for age). Correlations of radiographic and MR parameters with peak hip extension were calculated.
Results
The OA group was older, had greater pain, and limitation of function. They also had lower peak hip extension and higher peak hip flexion; and worse acetabular and femoral cartilage lesions. Peak hip extension and flexion correlated with KL grade, cartilage lesions in the inferior and posterior femur.
Conclusions
Reduced hip extension and greater hip flexion during walking are present in high functioning (HOOS > 85%) individuals with mild-moderate hip OA, and is associated with cartilage lesions.
Keywords: Gait, Cartilage, Labrum, HOOS, 6 Minute Walk Test
Introduction
One in four individuals may be at a risk of developing symptomatic hip osteoarthritis (OA) in their lifetime.1; 2 Hip OA leads to significant disability and often leads to surgery.3; 4 Due to the weight-bearing nature of the hip joint, it has been proposed that the pattern and magnitude of loads across the joint during daily activities are related to the pathogenesis of hip degeneration.5-8 Walking is the most common weight-bearing daily activity and earlier studies have demonstrated differences in gait patterns between those with and without hip OA.9-15 Results from these studies show that individuals with hip OA walk with reduced speed, cadence, and joint excursions including reduced hip extension during late stance.12-16 Specifically, a limitation of hip extension during the late stance phase of walking has been proposed as an important marker of the disease process in hip OA.13
Eitzen et al. reported that people with hip OA who have mild-moderate symptoms walk with reduced sagittal plane excursion, less hip extension and lower flexion moment at midstance.12 Similarly, Watelian et al. reported reduced hip extension at push-off in subjects with early hip OA defined as a Kellgren-Lawrence (KL) grade < 3 and a functional Lequesne Index score < 11.17 Other studies have also reported sagittal plane kinematic abnormalities including hip extension motion discontinuity as a key feature of walking gait in individuals with hip OA and its potential use as a biomechanical biomarker of hip OA.13; 14; 16 However, earlier gait studies have only reported radiographic measures of hip OA. Advances in MR imaging now allow a better visualization of hip joint structure and a precise characterization of the OA disease process.18-22 It is not known if specific anatomic findings from MRI are associated with hip OA are related to the limitation of hip extension during walking.
As such the objectives of this study were to investigate if (a) individuals with mild-moderate radiographic hip OA have lower hip extension during walking, in addition to greater pain, greater disability, and worse physical performance when compared to those without radiographic hip OA, and (b) worse radiographic and MR findings are associated with greater limitation of hip extension during walking.
Methods
Subjects
Data from sixty six subjects recruited as a part of a longitudinal cohort study on hip OA were available to be used for this study. The subjects were recruited from the community using flyers and advertisements. The inclusion criteria for subjects with radiographic hip OA in this analyses were age > 35 years, a Kellgren-Lawrence (KL) grade of 2 or 3 at the hip on weight-bearing anterior-posterior radiographs.23 The control subjects were >35 years of age, had a radiographic KL grade of 0 or 1 at both hips, and were without history of diagnosed OA or previous hip injuries. The side with greater KL grade was selected as the “index hip”. Exclusion criteria for all subjects were any contra-indications to MR imaging, KL grade of 4, a joint replacement of any lower extremity joint, previous hip trauma, pain at any other lower extremity joint, radiographic evidence of any knee or ankle joint OA, systemic inflammatory arthritis or any other spine or lower extremity condition that would affect their ability to complete the functional tests. All subjects signed a written informed consent approved by the Institutional Committee on Human Research.
Radiographic imaging
Weight-bearing anterior-posterior radiographs were acquired from all subjects. Initially all radiographs were analyzed using the Kellgren-Lawrence score,23 as part of the inclusion and exclusion criteria. Subsequently all radiographs were graded using the OARSI hip osteoarthritis score,24 which provides a more detailed approach to classify degenerative disease. The OARSI scoring was performed by a second experienced musuloskeletal radiologist (SL). Presence of definite joint space narrowing and osteophytes on the OARSI atlas was used to stratify the subjects into those with and without radiographic hip OA. Additionally, the lateral center-edge (LCE) angle was recorded from the radiographs.25
Motion Analysis
All subjects walked at a fixed speed of 1.35 meters/second while 3-D kinematics (at 250 Hz) using a passive 10-camera system (VICON, Oxford Metrics, UK) and kinetics (at 1000 Hz) using 2 floor embedded force platforms (AMTI, Watertown, MA, USA) were collected. The speed of 1.35 m/sec was selected as the mean of the reported average walking speeds on smooth level surfaces for adult men (1.43 m/sec) and women (1.28 m/sec) by Perry et al.26 A trial was acceptable when there was clean foot-strike on a force platform and the speed was within ± 5% of the first good trial. Five trials were acquired for each subject.
Fourteen millimeter spherical retro-reflective markers were placed on bony landmarks of bilateral lower extremities for identification of joint centers. These were placed on the sacrum, and bilaterally on the iliac crest, anterior superior iliac spine, greater trochanter, medial and lateral femoral condyles, medial and lateral malleoli, and 1st and 5th metatarsal head. Rigid marker clusters placed bilaterally on the lateral surface of the subject's thighs, legs and heel shoe counters were used to track segment motions.
Kinematic and kinetic data were calculated using Visual 3D (C-motion, Georgetown, MD, USA) bilaterally. In the right-hand coordinate system convention used, flexion, abduction and internal rotation were assigned as positive. Variables studied include the peak hip flexion and extension, sagittal excursion, hip extension at toe off, and peak flexion and extension moments. All variables were calculated during the stance phase of walking when the foot was in contact with the floor. The joint moments are reported as external moments and are normalized to the subject's body (BW) and height (Ht) (% BW*Ht). The average of 5 trials was calculated for each subject.
Patient-reported function
The dimensions of Pain and activities of daily living (ADL) from the self-reported Hip disability and Osteoarthritis Outcome Score (HOOS) were used.27 The dimensions are scored from 0 to 4, and then scores are transformed to a percentage score of 0 to 100, with 0 representing extreme hip problems and 100 representing no hip problems. The HOOS has been shown to be a valid, reliable, and responsive measure of overall hip joint function in people with OA.27
Physical Performance
Two tests were used.
Timed-up and Go Test
The TUG requires a subject to rise from a chair, walk 3 m, turn and come back to sit down. Participants were instructed to walk as quickly as they felt safe and comfortable. A stopwatch was be used to measure the time to complete the TUG within the nearest one hundredth of a second. In a recent review TUG has been shown to be one of the 2 tests with best measurement properties among the sit to stand tests for people with hip or knee OA. 28
Six Minute Walk Test (6MWT)
Subjects were instructed to cover as much distance as possible during the 6- minute time frame. The outcome was the distance walked in 6 minutes. The 6MWT has been shown to be related to pain and function in people with hip OA and has high inter-rater reliability in this population. 29; 30
MR imaging
All imaging was performed with a 3-Tesla MR scanner (GE MR750, GE Healthcare, Waukesha, WI, USA) and an 8 -channel cardiac coil (GE Healthcare, Waukesha, WI, USA). Patient positioning aids were used to immobilize and support patients, and ensure a consistent, reproducible, and comfortable hip positioning during scanning. Patients were positioned supine with their feet taped together, their knees supported by cushions to prevent movement. The imaging protocol and parameters are shown in Table 1.
Table 1.
MR sequence parameters.
| Sequence | Parameters |
|---|---|
| Coronal Fast Spin Echo – T2 weighted Fat Suppressed | TR/TE = 2496/60, Echo Train Length = 16, Matrix = 288 × 224, # of slices = 16, Field of View = 20, Slice Thickness = 4, Bandwidth = 50.0, Acquisition Time = 4 min 40 sec |
| Sagittal Fast Spin Echo – T2 weighted Fat Suppressed | TR/TE = 3678/60, Echo Train Length = 16, Matrix = 288 × 224, # of slices = 24, Field of View = 14, Slice Thickness = 4, Bandwidth = 50.0, Acquisition Time = 4 min |
| Axial Fast Spin Echo – T2 weighted Fat Suppressed | TR/TE = 2800/60, Matrix = 288 × 224, # of slices = 18, Field of View = 18, Slice Thickness =3, Bandwidth = 50.0, Acquisition Time = 3 min 50 sec |
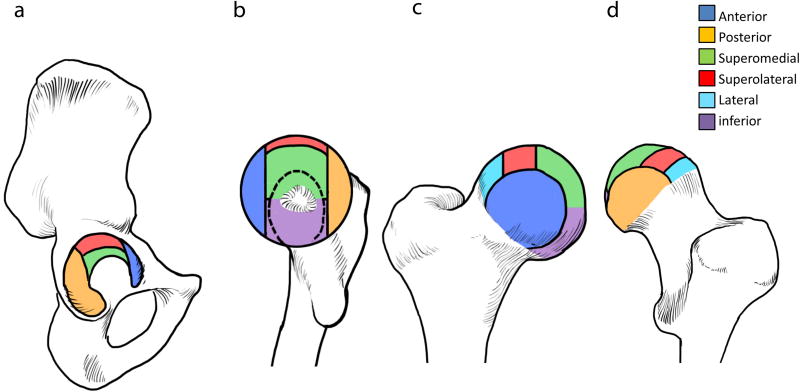
After a calibration session during which 3 radiologists went over 15 hip MRI studies (not included in this cohort) and discussed every classification feature, the studies were read by 2 board-certified musculoskeletal radiologists using a novel hip OA scoring system developed in-house.31 The features scored included cartilage defects, labral tears, bone marrow edema like lesions (BMEL) and subchondral cysts (Figures 1 and 2).22 For cartilage lesions, BMEL and subchondral cysts, the femoral and acetabular segments were divided into six subregions (4 femoral, 2 acetabular) on the coronal studies and 4 subregions (2 femoral, 2 acetabular) on the sagittal studies, for a total of 10 subregions. Cartilage defects were graded as 0 (no defect), 1 (partial thickness) and 2 (full thickness). BMEL were graded as 0 (absent), 1 (< or= 0.5 cm), 2 (0.5-1.5 cm) and 3 (> or = 1.5 cm). Subchondral cysts were graded as 0 (absent), 1 (< or = 0.5 cm) and 2 (> 0.5 cm). The labrum was graded on the sagittal images in the antero superior region, coronal images in the superolateral regions and on the axial images in the anterior and posterior regions. Labral tears were graded as 0 (normal or normal variant), 1 (fraying or signal abnormality), 2 (simple tear), 3 (labor-cartilage sepeartion), 4 (complex tear) and 5 (maceration). Total scores were calculated for cartilage lesions (femoral and acetabular), labral tears, BMELs and subchondral cysts. The third radiologist was consulted in case of a disagreement. Intra and inter-reliability for these measures has been reported previously.22 Additionally, alpha angle32 was measured on the oblique axial MR images. The radiologists were blinded to the gait data but not the radiographic data.
Figure 1.
Illustration of hip joint subregion subdivisions with color coding. (A) Acetabulum joint surface subregions seen from lateral aspect. (B) Femur joint surface subregions seen from medial aspect. Foveal attachment is noted in the medial center of femoral head. Dotted crescent line represents outline of acetabular fossa. (C) Femur joint surface subregions seen from anterior aspect. (D) Femur joint surface subregions seen from posterior aspect.
Figure 2.
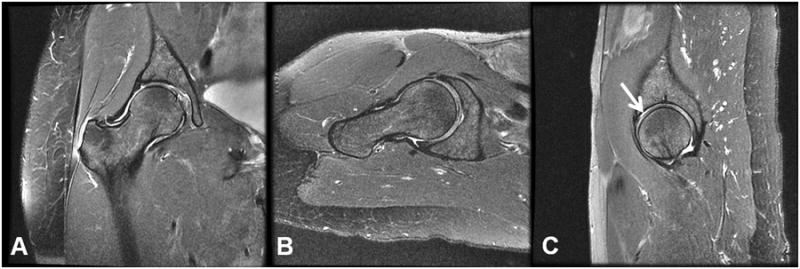
Examples of clinical images acquired on the right hip of a 52 year old female subject with KL=2 and the presence of acetabular and cartilage lesions. The images represent (a) the coronal FSE (b) the axial FSE, and (c) sagittal FSE acquisitions. An arrow on the sagittal FSE points to the location of an acetabular cartilage lesion.
Statistical Analyses
Although the subjects were recruited based on radiographic KL grading, for the statistical analyses the subjects were stratified into those with (n = 36) and without (n = 30) radiographic OA using the OARSI guidelines of definite joint space narrowing and definite presence of osteophytes. Primary analyses were to compare the group differences in HOOS, physical performance, and gait variables using ANOVA (adjusting for age). The radiologic variables were compared using independent samples t-tests (for alpha angle, CE angle), and Mann-Whitney U tests (for cartilage, labrum, BML, and subchondral cyst scores). Gender distribution was compared between the groups using a chi-square test. Correlations of gait variabels with KL, LCE, alpha angle, total labral scores, and regional cartilage lesion scores were calculated. Secondary analyses were to compare joint moments during walking between the two groups using ANOVA (adjusting for age). Significance was set at an alpha of 0.05.
Results
Subject characteristics, pain and function
There were thirty subjects without radiographic OA and thirty six subjects had radiographic hip OA as defined using OARSI guidelines (Table 2). The OA group had 15 subjects with KL =1, 11 with KL =2, and 10 with KL =3. The subjects with hip OA were older (P = 0.015) but with similar BMI (P = 0.132). The distribution of males and females was not different between the groups (χ2 = 2.68, P = 0.102). Subjects with hip OA had greater pain (P = 0.022), and greater limitation in the ADL (P = 0.048) (Table 2). The differences in the time taken to complete the TUG and the distance covered in the 6MWT were not significant between the groups (P > 0.05).
Table 2.
Mean and 95% confidence intervals for age, BMI, HOOS, TUG, and 6MWT parameters, and the gender distribution for subjects with and without radiographic hip osteoarthritis.
| Control (n = 30) | Osteoarthritis (n = 36) | P | ||
|---|---|---|---|---|
| Age (years) | 48.2 (44.0. 52.5) | 54.5 (51.5, 57.5) | 0.015† | |
| BMI (kg/m2) | 23.3 (22.1, 24.6) | 24.5 (23.5, 25.5) | 0.132† | |
| Gender (Male:Female) | 14:16 | 24:12 | 0.102* | |
| HOOS | Pain | 95.9 (93.2, 98.7) | 87.9 (81.9, 93.8) | 0.022† |
| Activities of Daily Living | 97.8 (95.8, 99.9) | 91.8 (86.9, 96.9) | 0.048† | |
| Timed Up and Go Test (sec) | 6.4 (5.9, 6.8) | 6.3 (6.0, 6.6) | 0.482† | |
| 6 Minute Walk Test (m) | 610.5 (564.8, 656.3) | 628.0 (598.0, 657.9) | 0.147# | |
P value from the Chi-Square test
- adjusted for age
adjusted for age and height
Gait Mechanics
Results are shown in Table 3. The hip OA subjects walked with approximately 4.5° higher peak hip flexion (P = 0.006) and 3° lower peak hip extension (P = 0.048). They also had approximately 3.5° lower hip extension at toe off (P = 0.032) compared to the control group. The difference in sagittal excursion (P = 0.287) was not significant. The differences in peak sagittal plane moments were not significant but there was a trend for greater external peak hip flexion moment in people with knee OA (P = 0.057).
Table 3.
Mean and 95% confidence intervals for sagittal hip joint kinematics (in degrees) and external moments (in %BW*Ht) during the stance phase of walking in subjects with and without radiographic hip osteoarthritis.
| Control (n = 30) | Osteoarthritis (n = 36) | P* | |
|---|---|---|---|
| Sagittal Excursion | 40.7 (39.2, 42.2) | 42.0 (40.1, 43.8) | 0.287 |
| Peak Flexion | 22.0 (19.2, 24.6) | 26.5 (24.3, 28.6) | 0.006 |
| Peak Extension | -18.7 (-21.4, -16.0) | -15.5 (-17.9, -13.1) | 0.048 |
| Extension at Toe-off | -9.2 (-11.8, -6.6) | -5.7 (-7.9, -3.4) | 0.032 |
| Peak Flexion Moment | 4.2 (3.6, 4.8) | 5.1 (4.7, 5.6) | 0.057 |
| Peak Extension Moment | -3.5 (-3.0, -4.0) | -3.7 (-3.2, -4.3) | 0.475 |
adjusted for age
Radiologic findings
Results are shown in Table 4 and 5. People with hip OA had greater severity of acetabular (P = 0.013) and femoral (P = 0.006) cartilage lesions but the differences were not significant for labral tears (P = 0.109), BMLs (P = 0.747), and subchondral cysts (P = 0.160). The differences between the groups were not significant for the MR alpha angle (P = 0.689), and the radiographic LCE angle (P = 0.934).
Table 4.
Distribution of cartilage and labral lesions in each subregion for both groups.
| Control (n = 30) | OA (n = 36) | ||||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Coronal | Superolateral Acetabulum | 6 | 20.0 | 18 | 50.0 |
| Superomedial Acetabulum | 4 | 13.3 | 12 | 33.3 | |
| Lateral Femur | 8 | 26.7 | 20 | 55.6 | |
| Superolateral Femur | 5 | 16.7 | 18 | 50.0 | |
| Superomedial Femur | 7 | 23.3 | 13 | 36.1 | |
| Inferior Femur | 4 | 13.3 | 15 | 41.7 | |
| Sagittal | Anterior Acetabulum | 6 | 20.0 | 15 | 41.7 |
| Posterior Acetabulum | 1 | 3.3 | 6 | 16.7 | |
| Anterior Femur | 6 | 20.0 | 18 | 50.0 | |
| Posterior Femur | 3 | 10.0 | 10 | 27.8 | |
| Labrum | Anterior Superior | 23 | 76.7 | 29 | 80.6 |
| Superior Lateral | 13 | 43.3 | 24 | 66.7 | |
| Anterior Lateral | 17 | 56.7 | 22 | 61.1 | |
| Posterior Lateral | 1 | 3.3 | 6 | 16.7 | |
Table 5.
Hip anatomic grading of cartilage lesions, labrum tears, BMLs, and subchondral cysts in subjects with and without radiographic hip osteoarthritis. Alpha Angle, and LCE anglealso shown for the two groups.
| Control (n = 30) | Osteoarthritis (n = 36) | P* | |
|---|---|---|---|
| Total Acetabular Cartilage Lesion Score | 0.6 (1.1) | 1.7 (1.9) | 0.013 |
| Total Femoral Cartilage Lesion Score | 1.4 (2.0) | 3.1 (2.9) | 0.006 |
| Total Labral Tear Score | 6.2 (3.2) | 8.1 (4.8) | 0.109 |
| Total Bone Marrow Lesion Score | 0.4 (1.2) | 0.8 (2.2) | 0.747 |
| Total Subchondral Cyst Score | 0.2 (0.6) | 1.5 (0.3) | 0.160 |
| Alpha Angle (°) | 56.3 (15.8) | 59.6 (12.5) | 0.689 |
| Lateral Center-edge Angle (°) | 30.9 (6.2) | 31.3 (7.1) | 0.934 |
Correlations
Results are shown in Table 6. Higher KL grade was associated with greater peak hip flexion, lower peak hip extension, and lower hip extension at toe-off (P < 0.05). Greater cartilage lesions score in the inferior and posterior femur was associated with greater peak hip flexion, lower peak hip extension, and lower hip extension at toe-off (P < 0.05). Additionally, greater cartilage lesions score in the posterior acetabulum was associated with lower sagittal excursion. There were no other significant correlations for any of the comparisons.
Table 6.
Correlations of KL, labral lesion, cartilage lesion, alpha angle, and LCE angle with gait parameters.
| Spearman'r Rho and P value |
KL | Labral Tears |
Superolateral Acetabulum |
Superomedial Acetabulum |
Lateral Femur |
Superolateral Femur |
Superomedial Femur |
Inferior Femur |
Anterior Acetabulum |
Posterior Acetabulum |
Anterior Femur |
Posterior Femur |
Alpha Angle* |
LCE Angle* |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sagittal Excursion | -0.09 | -0.14 | -0.15 | -0.11 | 0.03 | -0.10 | -0.01 | -0.09 | -0.22 | -0.41 | -0.17 | -0.04 | 0.03 | -0.06 |
| .465 | .256 | .239 | .371 | .822 | .406 | .935 | .459 | .078 | .001 | .182 | .744 | .836 | .661 | |
| Peak Flexion | 0.28 | 0.14 | 0.05 | -0.06 | 0.16 | 0.07 | 0.00 | 0.26 | 0.03 | -0.10 | 0.13 | 0.26 | 0.07 | -0.19 |
| .026 | .258 | .719 | .661 | .201 | .587 | .993 | .037 | .826 | .416 | .317 | .034 | .565 | .136 | |
| Peak Extension | 0.27 | 0.18 | 0.10 | 0.01 | 0.11 | 0.11 | -0.02 | 0.27 | 0.11 | 0.15 | 0.20 | 0.24 | 0.05 | -0.15 |
| .027 | .151 | .427 | .943 | .373 | .396 | .898 | .028 | .385 | .218 | .103 | .049 | .667 | .240 | |
| Extension at Toe-Off | 0.29 | 0.20 | 0.13 | 0.04 | 0.15 | 0.12 | 0.01 | 0.30 | 0.10 | 0.15 | 0.21 | 0.26 | 0.03 | -0.14 |
| .017 | .111 | .282 | .768 | .235 | .325 | .968 | .013 | .406 | .231 | .094 | .038 | .843 | .271 | |
| Peak Flexion Moment | -0.08 | 0.03 | 0.11 | 0.04 | 0.06 | 0.07 | -0.03 | 0.07 | 0.09 | 0.14 | 0.11 | 0.00 | 0.10 | -0.04 |
| .538 | .782 | .386 | .756 | .647 | .592 | .788 | .598 | .449 | .267 | .383 | .987 | .432 | .767 | |
| Peak Extension Moment | -0.08 | -0.18 | -0.10 | 0.01 | -0.13 | -0.16 | 0.07 | -0.12 | -0.09 | -0.19 | -0.10 | -0.03 | -0.08 | 0.05 |
| .532 | .151 | .415 | .950 | .288 | .211 | .555 | .330 | .481 | .133 | .428 | .809 | .533 | .670 |
Pearson's correlation
Discussion
The results show that people with mild-moderate radiographic hip OA had greater hip flexion and lower hip extension during walking compared to controls. The subjects with hip OA had greater self-reported pain and activity limitation compared to controls but average HOOS scores were > 85% for both groups. KL grade and lesions in the posterior and inferior femur region had weak associations with greater peak hip flexion and lower peak hip extension during walking. These results demonstrate weak but significant associations of imaging findings with movement patterns in people with early hip OA, and the importance of objective quantification of walking patterns in the early stage of hip OA disease. Furthermore, these results also highlight the clinical importance of MRI for describing the degeneration of the hip joint.
We observed greater hip flexion and lower extension in the subjects with hip OA compared to those without radiographic hip OA. Earlier studies have demonstrated reduced hip extension as a key biomechanical finding during walking in populations with hip OA.14; 15; 17 Our data are consistent with a recent study on 48 subjects with mild-moderate symptomatic hip OA (defined as a Harris Hip Score between 60-95) and 22 controls, which also reported 9.6° lower hip extension during the 2nd half stance.12 Recently it has been suggested the a reversal in the extension motion in people with hip OA is associated with structural and symptomatic severity of hip OA, and could potentially be used an indicators of OA disease status.13 Although motion reversal and limitation of peak hip extension are not equivalent, both are potentially related to the inability to extend the hip due to OA related changes.14 These recent findings suggest that reduced peak hip extension in subjects with mild-moderate radiographic hip OA is a common finding and may play a role in the pathomechanics of the disease.
We did not observe significant differences in the external peak hip extension moment during the late-stance but the OA group tended to have greater external flexion moment in early stance (P = 0.057). Eitzen et al. did not compare the peak external hip flexion moment in early stance between the 2 groups in their study.12 However, looking at their data, it appears that the OA group did indeed have higher flexion moment in early stance. It is not possible to determine if this difference was statistically significant. Eitzen et al. reported lower hip moment external extension moment during mid-stance and late-stance in individuals with mild-moderate symptomatic hip OA. 12 They did not control the walking speed and reported significantly lower walking speed for subjects with hip OA which can lead to lower joint moments. We required our subjects to walk at a fixed speed of 1.35 m/sec. Although the differences in joint moments in their study were significant even after adjusting for the walking speed, it may be possible that the difference in the walking task in the two studies may be related to these findings. The self-selected walking speed for our controls was 1.46±0.23 m/sec, and for the OA group it was 1.56±0.25 m/sec. The difference in the self-selected speed between the 2 groups was not significant. Also, the self-selected speed for both groups was faster than the 1.35 m/sec fixed speed used in this study. If the self-selected walking speed of our OA group, and not the control group, were slower than the fixed speed used in our study, it could have been possible that higher moments in the OA group due to the demands of the faster walking speed may have masked real differences in sagittal plane moments between the groups. The OA subjects in the Eitzen et al. study were also older (59 ± 9.5 years) than those included in our study (55±9 years). Lastly, Eitzen et al. used data from subjects recruited for a randomized controlled trial. These subjects were recruited from hospitals and clinics. On the other hand we recruited our subjects from the community. It may be possible that our cohort of mild-moderate hip OA subjects recruited from the community was relatively high functioning. This is supported by HOOS scores being > 85% on an average in our OA cohort. Further support for the observation that our cohort was high functioning comes from the lack of significant differences between the OA and control groups for the TUG and 6MWT tests. We also excluded individuals with severe radiographic hip OA (KL =4) as well as individuals who were had any lower extremity conditions that would prevent them from completing the functional testing. Hence, it is possible that the muscle weakness seen with advanced hip OA may not have been present in these individuals. Since we did not collect muscle strength measures from our cohort so we are unable to confirm these speculations. Furthermore, since our cohort was relatively high functioning, the results demonstrate that the kinematic gait deviations appear to be sensitive to early hip OA. Future longitudinal studies would be needed to evaluate if these kinematic differences are related to longitudinal changes in structural and symptomatic progression of the disease.
Not surprisingly, we observed that the subjects with radiographic hip OA had greater prevalence and severity of femoral and acetabular cartilage lesions. However, we did not observe a difference in the scores for labral tears, BMLs, and subchondral cysts. Earlier work has shown that cartilage lesions are related to symptomatic and structural hip OA disease but labral tears may not be as clinically significant.21; 22 This is supported by observations of 70-86% prevalence of labral tears in asymptomatic populations. 33,34 MRI is known to offer limited sensitivity towards detecting labral lesions at the hip with arthroscopic evaluation being the gold standard. 35 However, recently optimized non-contrast hip MRI has shown favorable results. 36 The ability to visualize the labrum in our study was enhanced by the use an optimized non-contrast hip MRI protocol, using a small field of view on a 3.0-Tesla scanner. Nonetheless, even with the use of these advanced techniques, we did not observe differences between groups.
We observed that lower peak hip extension (and greater peak flexion, lower hip extension at toe-off) had weak but significant associations with higher KL grade and worse cartilage lesion scores in the inferior and posterior femur. Although the association of gait parameters was similar with both radiographic and MR parameters, MR imaging allowed further identification of regional differences in hip degenerative process.18; 20-22 Due to the correlations being weak, we performed further investigations comparing peak hip extension in people with and without lesions in the inferior femur, with and without lesions in posterior femur, and with different KL grades. Results showed that the subjects with lesions in the inferior femur (n = 18) walked with approximately 4° less peak hip extension (P = 0.015) compared to those without lesions in the inferior femur (n = 48) (results not shown). The peak hip extension was not significantly different across KL grades (P = 0.190), and close to significant for posterior femur lesions (P = 0.063). Based on instrumented knee and finite element studies, the contact stress at the hip during the walking is greater anteriorly and superiorly than posteriorly.37; 38 However, it may be possible that the observed sagittal plane deviations could be related to a change in contact stress pattern so as to overload and/or underload the posterior and inferior femoral cartilage subregions. Due to the cross-sectional nature of the study, it is unclear if the cartilage lesions precede the kinematic findings or vice versa. However, these data further highlight the association between movement patterns and joint structure in people with hip OA and support the necessity for future investigations to explore this phenomenon longitudinally.
We also utilized a different radiographic definition of OA for this study than that used for the inclusion criteria in the parent study. This resulted in 15 subjects with KL=1 being classified as having OA under the OARSI classification. Hence we performed additional sensitivity analyses for key outcomes in this study comparing subjects without radiographic hip OA (n =30) and those with radiographic hip OA based on OARSI atlas and with KL >1 (n = 21). So the 15 subjects with KL = 1 were excluded. Results showed that subjects with OA had greater external peak hip flexion moment in early stance (P = 0.042), greater peak hip flexion angle (P=0.002), lower peak hip extension angle (P = 0.007), and lower hip extension angle at toe-off (P = 0.008). These sensitivity analyses demonstrate that the key findings from this study are not affected by the inclusion of subjects with KL =1 in the OA group.
The study has limitations which need to be considered while interpreting the findings. Due to the cross-sectional nature causality cannot be determined from these data. Future studies would be needed to evaluate the long-term effects of limitations in hip extension on hip degeneration. Furthermore, our cohort consisted of subjects with early radiographic hip OA and who were high-functioning including those with and without hip OA related symptoms. Hence, the results may not be generalized to all subjects with hip OA. Also, the observed associations between imaging (radiograph, MRI) parameters and gait parameters were weak. Hence, caution should be observed while interpreting these findings, and studies in larger samples are needed to confirm these findings. Finally, although we adjusted for age in our statistically analyses, age related loss of hip extension may have affected our findings since the OA group was significantly older. Additionally, we did not observe an association between age and peak hip extension in our cohort (r = -0.047, P= .707).
In conclusion, we observed lower hip extension in people with mild-moderate radiographic hip OA compared to controls. Subjects with hip OA had worse cartilage lesions in femoral and acetabular surfaces but the difference in labral tear scores were not significant. Finally, KL grade, and lesions in the inferior and posterior femur region had weak but significant associations with greater peak hip flexion and lower peak hip extension during walking.
Acknowledgments
The authors thank Melissa Guan for patient recruitment, K. Subburaj for software support, and Peter K. Lee for the artful illustrations in Figure 1. Funding was from NIH-NIAMS P50 AR060752.
Contributor Information
Cory Wyatt, Email: cory.wyatt@ucsf.edu, 1700 4th St, Suite 203, Byers Hall, Mission Bay, University of California, San Francisco, CA 94158.
Ko Chiba, Email: kohchiba@estate.ocn.ne.jp, Department of Orthopedic Surgery, Nagasaki University School of Medicine.
Sonia lee, Email: Sonia.lee@ucsf.edu, 185 Berry St, Suite 350, UCSF China Basin, San Francisco, CA, 94107.
Lorenzo Nardo, Email: Lorenzo.nardo@ucsf.edu, 185 Berry St, Suite 350, UCSF China Basin, San Francisco, CA, 94107.
Thomas M. Link, Email: Thomas.link@ucsf.edu, 185 Berry St, Suite 350, UCSF China Basin, San Francisco, CA, 94107.
Sharmila Majumdar, Email: Sharmila.majumdar@ucsf.edu, 1700 4th Street, Suite 203, Byers Hall, UCSF Mission Bay, San Francisco, CA 94158.
Richard B. Souza, Email: Richard.souza@ucsf.edu, 185 Berry St, Suite 350, UCSF China Basin, San Francisco, CA, 94107.
References
- 1.Murphy LB, Helmick CG, Schwartz TA, et al. One in four people may develop symptomatic hip osteoarthritis in his or her lifetime. Osteoarthritis Cartilage. 2010;18:1372–1379. doi: 10.1016/j.joca.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nho SJ, Kymes SM, Callaghan JJ, et al. The burden of hip osteoarthritis in the United States: epidemiologic and economic considerations. J Am Acad Orthop Surg. 2013;21(Suppl 1):S1–6. doi: 10.5435/JAAOS-21-07-S1. [DOI] [PubMed] [Google Scholar]
- 3.Salaffi F, Carotti M, Stancati A, et al. Health-related quality of life in older adults with symptomatic hip and knee osteoarthritis: a comparison with matched healthy controls. Aging Clin Exp Res. 2005;17:255–263. doi: 10.1007/BF03324607. [DOI] [PubMed] [Google Scholar]
- 4.Katz JN, Losina E, Barrett J, et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2001;83-A:1622–1629. doi: 10.2106/00004623-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Polkowski GG, Clohisy JC. Hip biomechanics. Sports Med Arthrosc. 2010;18:56–62. doi: 10.1097/JSA.0b013e3181dc5774. [DOI] [PubMed] [Google Scholar]
- 6.Ganz R, Leunig M, Leunig-Ganz K, et al. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar D, Dillon A, Nardo L, et al. Differences in the Association of Hip Cartilage Lesions and Cam-Type Femoroacetabular Impingement With Movement Patterns: A Preliminary Study. PM & R : the journal of injury, function, and rehabilitation. 2014 doi: 10.1016/j.pmrj.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Block JA, Shakoor N. Lower limb osteoarthritis: biomechanical alterations and implications for therapy. Current opinion in rheumatology. 2010;22:544–550. doi: 10.1097/BOR.0b013e32833bd81f. [DOI] [PubMed] [Google Scholar]
- 9.Beaulieu ML, Lamontagne M, Beaule PE. Lower limb biomechanics during gait do not return to normal following total hip arthroplasty. Gait Posture. 2010;32:269–273. doi: 10.1016/j.gaitpost.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 10.Foucher KC, Hurwitz DE, Wimmer MA. Preoperative gait adaptations persist one year after surgery in clinically well-functioning total hip replacement patients. J Biomech. 2007;40:3432–3437. doi: 10.1016/j.jbiomech.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 11.Lenaerts G, Mulier M, Spaepen A, et al. Aberrant pelvis and hip kinematics impair hip loading before and after total hip replacement. Gait Posture. 2009;30:296–302. doi: 10.1016/j.gaitpost.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 12.Eitzen I, Fernandes L, Nordsletten L, et al. Sagittal plane gait characteristics in hip osteoarthritis patients with mild to moderate symptoms compared to healthy controls: a cross-sectional study. BMC Musculoskelet Disord. 2012;13:258. doi: 10.1186/1471-2474-13-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foucher KC, Schlink BR, Shakoor N, et al. Sagittal plane hip motion reversals during walking are associated with disease severity and poorer function in subjects with hip osteoarthritis. J Biomech. 2012;45:1360–1365. doi: 10.1016/j.jbiomech.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 14.Hurwitz DE, Hulet CH, Andriacchi TP, et al. Gait compensations in patients with osteoarthritis of the hip and their relationship to pain and passive hip motion. J Orthop Res. 1997;15:629–635. doi: 10.1002/jor.1100150421. [DOI] [PubMed] [Google Scholar]
- 15.Kubota M, Shimada S, Kobayashi S, et al. Quantitative gait analysis of patients with bilateral hip osteoarthritis excluding the influence of walking speed. J Orthop Sci. 2007;12:451–457. doi: 10.1007/s00776-007-1160-z. [DOI] [PubMed] [Google Scholar]
- 16.Ewen AM, Stewart S, St Clair Gibson A, et al. Post-operative gait analysis in total hip replacement patients-a review of current literature and meta-analysis. Gait Posture. 2012;36:1–6. doi: 10.1016/j.gaitpost.2011.12.024. [DOI] [PubMed] [Google Scholar]
- 17.Watelain E, Dujardin F, Babier F, et al. Pelvic and lower limb compensatory actions of subjects in an early stage of hip osteoarthritis. Arch Phys Med Rehabil. 2001;82:1705–1711. doi: 10.1053/apmr.2001.26812. [DOI] [PubMed] [Google Scholar]
- 18.Gold SL, Burge AJ, Potter HG. MRI of hip cartilage: joint morphology, structure, and composition. Clin Orthop Relat Res. 2012;470:3321–3331. doi: 10.1007/s11999-012-2403-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guermazi A, Roemer FW, Haugen IK, et al. MRI-based semiquantitative scoring of joint pathology in osteoarthritis. Nat Rev Rheumatol. 2012 doi: 10.1038/nrrheum.2012.223. [DOI] [PubMed] [Google Scholar]
- 20.Mamisch TC, Zilkens C, Siebenrock KA, et al. MRI of hip osteoarthritis and implications for surgery. Magn Reson Imaging Clin N Am. 2009;18:111–120. doi: 10.1016/j.mric.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 21.Roemer FW, Hunter DJ, Winterstein A, et al. Hip Osteoarthritis MRI Scoring System (HOAMS): reliability and associations with radiographic and clinical findings. Osteoarthritis Cartilage. 2011;19:946–962. doi: 10.1016/j.joca.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 22.Kumar D, Wyatt CR, Lee S, et al. Association of cartilage defects, and other MRI findings with pain and function in individuals with mild-moderate radiographic hip osteoarthritis and controls. Osteoarthritis Cartilage. 2013;21:1685–1692. doi: 10.1016/j.joca.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2007;15(Suppl A):A1–56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 25.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 26.Perry J, Burnfield JM. Gait Analysis: Normal and Pathological Function. SEcond. Thorofare, New Jersey: SLACK Incorporated; 2010. [Google Scholar]
- 27.Nilsdotter AK, Lohmander LS, Klassbo M, et al. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10. doi: 10.1186/1471-2474-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dobson F, Hinman RS, Hall M, et al. Measurement properties of performance-based measures to assess physical function in hip and knee osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2012;20:1548–1562. doi: 10.1016/j.joca.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 29.Rydevik K, Fernandes L, Nordsletten L, et al. Functioning and disability in patients with hip osteoarthritis with mild to moderate pain. J Orthop Sports Phys Ther. 2010;40:616–624. doi: 10.2519/jospt.2010.3346. [DOI] [PubMed] [Google Scholar]
- 30.Stratford PW, Kennedy DM, Woodhouse LJ. Performance measures provide assessments of pain and function in people with advanced osteoarthritis of the hip or knee. Phys Ther. 2006;86:1489–1496. doi: 10.2522/ptj.20060002. [DOI] [PubMed] [Google Scholar]
- 31.Lee S, Nardo L, Kumar D, et al. Scoring hip osteoarthritis with MRI (SHOMRI): A whole joint osteoarthritis evaluation system. Journal of magnetic resonance imaging : JMRI. 2014 doi: 10.1002/jmri.24722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Notzli HP, Wyss TF, Stoecklin CH, et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620x.84b4.12014. [DOI] [PubMed] [Google Scholar]
- 33.Schmitz MR, Campbell SE, Fajardo RS, et al. Identification of acetabular labral pathological changes in asymptomatic volunteers using optimized, noncontrast 1.5-T magnetic resonance imaging. Am J Sports Med. 2012;40:1337–1341. doi: 10.1177/0363546512439991. [DOI] [PubMed] [Google Scholar]
- 34.Register B, Pennock AT, Ho CP, et al. Prevalence of abnormal hip findings in asymptomatic participants: a prospective, blinded study. Am J Sports Med. 2012;40:2720–2724. doi: 10.1177/0363546512462124. [DOI] [PubMed] [Google Scholar]
- 35.Smith TO, Hilton G, Toms AP, et al. The diagnostic accuracy of acetabular labral tears using magnetic resonance imaging and magnetic resonance arthrography: a meta-analysis. Eur Radiol. 2011;21:863–874. doi: 10.1007/s00330-010-1956-7. [DOI] [PubMed] [Google Scholar]
- 36.Mintz DN, Hooper T, Connell D, et al. Magnetic resonance imaging of the hip: detection of labral and chondral abnormalities using noncontrast imaging. Arthroscopy. 2005;21:385–393. doi: 10.1016/j.arthro.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 37.Bergmann G, Deuretzbacher G, Heller M, et al. Hip contact forces and gait patterns from routine activities. J Biomech. 2001;34:859–871. doi: 10.1016/s0021-9290(01)00040-9. [DOI] [PubMed] [Google Scholar]
- 38.Harris MD, Anderson AE, Henak CR, et al. Finite element prediction of cartilage contact stresses in normal human hips. J Orthop Res. 2012;30:1133–1139. doi: 10.1002/jor.22040. [DOI] [PMC free article] [PubMed] [Google Scholar]