Abstract
Objective
We sought to examine the risk of mortality associated with nonobstructive coronary artery disease (CAD) and to determine the impact of baseline statin and aspirin use on mortality.
Approach and Results
Coronary computed tomographic angiography permits direct visualization of nonobstructive CAD. To date, the prognostic implications of nonobstructive CAD and the potential benefit of directing therapy based on nonobstructive CAD have not been carefully examined. A total of 27 125 consecutive patients who underwent computed tomographic angiography (12 enrolling centers and 6 countries) were prospectively entered into the COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter (CONFIRM) registry. Patients, without history of previous CAD or obstructive CAD, for whom baseline statin and aspirin use was available were analyzed. Each coronary segment was classified as normal or nonobstructive CAD (1%–49% stenosis). Patients were followed up for a median of 27.2 months for all-cause mortality. The study comprised 10 418 patients (5712 normal and 4706 with nonobstructive CAD). In multivariable analyses, patients with nonobstructive CAD had a 6% (95% confidence interval, 1%–12%) higher risk of mortality for each additional segment with nonobstructive plaque (P=0.021). Baseline statin use was associated with a reduced risk of mortality (hazard ratio, 0.44; 95% confidence interval, 0.28–0.68; P=0.0003), a benefit that was present for individuals with nonobstructive CAD (hazard ratio, 0.32; 95% confidence interval, 0.19–0.55; P<0.001) but not for those without plaque (hazard ratio, 0.66; 95% confidence interval, 0.30–1.43; P=0.287). When stratified by National Cholesterol Education Program/Adult Treatment Program III, no mortality benefit was observed in individuals without plaque. Aspirin use was not associated with mortality benefit, irrespective of the status of plaque.
Conclusions
The presence and extent of nonobstructive CAD predicted mortality. Baseline statin therapy was associated with a significant reduction in mortality for individuals with nonobstructive CAD but not for individuals without CAD.
Clinical Trial Registration
URL: http://clinicaltrials.gov/. Unique identifier NCT01443637
Keywords: aspirin, coronary angiography, coronary atherosclerosis, mortality, prognosis, statin
Coronary computed tomographic angiography (CTA) is a noninvasive angiographic modality that allows for direct visualization of obstructive and nonobstructive coronary artery disease (CAD).1–7 Although several previous studies have carefully examined the prognostic implications of obstructive CAD for individuals undergoing coronary CTA, the relationship of nonobstructive CAD to future adverse events remains not completely understood.
Furthermore, the decisions on primary prevention for individuals with nonobstructive CAD remain unclear. Statin and aspirin treatment, for primary prevention, is recommended for patients at high risk of future cardiovascular events based on clinical or laboratory markers, such as those with diabetes mellitus, dyslipidemia, high Framingham or National Cholesterol Education Program/Adult Treatment Program III (NCEP/ATP III) risk scores, or intermediate Framingham Risk Score with elevated high-sensitivity-C-reactive protein.8,9 Several recent analyses have directly challenged the efficacy of statin or aspirin therapy in primary prevention.10–12 Whether the use of coronary CTA to identify nonobstructive CAD offers a feasible method by which at-risk patients can be identified and effectively treated remains unknown.
Therefore, using a large prospective multicenter international registry, we examined the risk of mortality and the impact of baseline statin and aspirin use on mortality risk in individuals without obstructive CAD by coronary CTA.
Materials and Methods
Materials and Methods are available in the online-only Data Supplement.
Results
Study Population
Of the 27 125 CONFIRM registry patients, centers without medication data were excluded (3 centers with 7422 patients). An additional 6074 patients were excluded for incomplete coronary plaque information (836 patients), history of myocardial infarction or revascularization (1491 patients), congenital heart disease (119 patients), missing body mass index (449 patients), missing age (2 patient), and obstructive CAD diagnosed on coronary CTA (3162 patients). Of the remaining 13 629 patients, 3211 (23.6%) patients had missing statin or aspirin information. For those with numeric values of lipoproteins, total cholesterol was 191±43 mg/dL (n=7426), low-density lipoprotein cholesterol was 117.2±36.1 mg/dL (n=6831), and high-density lipo-protein cholesterol was 53.4±16.3 mg/dL (n=7263).
Follow-up (median, 27.2 [interquartile range, 17.7–40.8] months) was available for 99.3% of patients. Although few were lost to follow-up (77 [0.7%] patients), patients lost to follow-up were younger (48.7±11.5 years) and were less likely to be hypertensive (31.2%) or dyslipidemic (40.3%; P<0.01 for all).
A total of 10 418 patients (5712 with normal coronary arteries and 4706 with nonobstructive CAD) met the enrolment criteria and were analyzed (Table 1). There were observed differences between statin and nonstatin users for age (60.5 versus 55.6 years; P<0.001), and prevalence of hypertension (54.7% versus 42.3%; P<0.001), diabetes mellitus (18.5% versus 8.4%; P<0.001), dyslipidemia (85.0% versus 39.1%, P<0.001), but not smoking (24.7% versus 25.5%; P=0.38). Important also clinical differences existed between aspirin users and nonaspirin users for measures of age (59.6 versus 55.8 years; P<0.001), hypertension (54.5% versus 51.6%; P<0.001), diabetes mellitus (15.5% versus 9.5%; P<0.001), dyslipidemia (62.3% versus 49.5%; P<0.001), but not smoking (25.0% versus 25.4%; P=0.67).
Table 1.
Patient Characteristics
| All Patients n=10418 |
No Plaque n=5712 |
Nonobstructive CAD n=4706 |
P Value* | |
|---|---|---|---|---|
| Age, y | 57.2±11.8 | 53.7±11.8 | 61.6±10.3 | <0.001 |
| Men | 5490 (52.7%) | 2630 (46.0%) | 2860 (60.8%) | <0.001 |
| Body mass index, kg/m2 | 26.7±5.1 | 26.4±5.1 | 27.0±5.1 | <0.001 |
| Cardiac risk factors | ||||
| Smoker/ex-smoker | 2626 (25.2%) | 1248 (21.8%) | 1378 (29.3%) | <0.001 |
| Hypertension | 4837 (46.4%) | 2444 (42.8%) | 2393 (50.8%) | <0.001 |
| Dyslipidemia† | 5662 (54.3%) | 2888 (50.6%) | 2774 (58.9%) | <0.001 |
| Diabetes mellitus | 1226 (11.8%) | 525 (9.2%) | 701 (14.9%) | <0.001 |
| Family history of CAD | 2885 (27.7%) | 1501 (26.3%) | 1384 (29.4%) | <0.001 |
| Indications for study | ||||
| Chest pain | 6012 (57.7%) | 3566 (62.4%) | 2446 (52.0%) | <0.001 |
| Typical angina | 1094 (10.5%) | 625 (10.9%) | 469 (10.0%) | 0.109 |
| Dyspnea | 784 (7.5%) | 358 (6.3%) | 426 (9.1%) | <0.001 |
| Chest pain+dyspnea | 1127 (10.8%) | 586 (10.3%) | 541 (11.5%) | 0.043 |
| NCEP/ATP III risk | ||||
| Low risk | 3240 (31.1%) | 2155 (37.7%) | 1085 (23.1%) | <0.001 |
| Intermediate risk | 5699 (54.7%) | 2899 (50.8%) | 2800 (59.5%) | <0.001 |
| High risk | 1479 (14.2%) | 658 (11.5%) | 821 (17.4%) | <0.001 |
| Medications | ||||
| Aspirin | 3932 (37.7%) | 1758 (30.8%) | 2174 (46.2%) | <0.001 |
| Statin | 3465 (33.3%) | 1432 (25.1%) | 2033 (43.2%) | <0.001 |
Values are given as mean±SD or n (%). CAD indicates coronary artery disease; and NCEP/ATP III, National Cholesterol Education Program/Adult Treatment Program III.
Comparison of patients with no plaque and with nonobstructive CAD.
Self-reported dyslipidemia.
Compared with patients with normal coronary arteries, those with nonobstructive CAD were older, more often men, had more cardiac risk factors, and had higher NCEP/ATP III risk scores (P<0.001 for all). Patients with nonobstructive CAD by coronary CTA were more likely to be taking statins (43.2% versus 25.1%; P<0.001) and aspirin (46.2% versus 30.8%; P<0.001) at the time of coronary CTA when compared with patients without CAD by coronary CTA.
At follow-up, there were a total of 120 deaths. Seventy-nine deaths occurred in 4706 patients with nonobstructive coronary plaque (1.68%) and 41 deaths occurred in the 5712 individuals with normal coronary arteries (0.72%). Of the 3465 patients treated with statins, there were a total of 29 (0.76%) deaths, whereas of the 6953 patients without statin therapy, there were 91 (1.31%) deaths. The relationship of statin use and plaque as a function of mortality exhibited differences. Deaths occurred in 9 (0.6%) statin-using patients compared with 32 (0.8%) non–statin-using patients (P=0.64) with normal coronary arteries, whereas occurring in 20 (1.0%) statin-using patients and 59 (2.2%) non–statin-using patients (P=0.001) with nonobstructive CAD.
Univariable Analysis of Clinical Variables and Medications for All-Cause Mortality
In univariable analysis of the entire study cohort, age, cardiac risk factors, and NCEP/ATP III risk were associated with all-cause mortality (Table 2). Baseline statin therapy was associated with lower mortality in the entire study cohort (hazard ratio [HR], 0.65 [0.43–0.99]; P=0.046) and those with nonobstructive CAD (HR, 0.45 [0.27–0.75]; P=0.002), but not in patients with normal coronary arteries (HR, 0.84 [0.40–1.76]; P=0.646). Aspirin use at baseline was not associated with differences in survival in the overall study group (HR, 0.89 [0.61–1.3]; P=0.537) or in those with and without nonobstructive CAD (HR, 0.72 [0.46–1.14]; P=0.161) and (HR, 0.84 [0.40–1.76]; P=0.646, respectively).
Table 2.
Hazards of All-Cause Mortality in Relation to Clinical Characteristics (Univariable Analysis)
| Overall | No Plaque | Nonobstructive CAD | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | P Value | Hazard Ratio | 95% CI | P Value | Hazard Ratio | 95% CI | P Value | |
| Age, y | 1.09 | 1.07–1.11 | <0.001 | 1.06 | 1.03–1.09 | 0.0002 | 1.10 | 1.07–1.13 | <0.0001 |
| Men | 0.78 | 0.54–1.11 | 0.164 | 0.82 | 0.44–1.53 | 0.540 | 0.61 | 0.39–0.95 | 0.027 |
| BMI, kg/m2 | 0.98 | 0.94–1.02 | 0.379 | 1.00 | 0.93–1.07 | 0.908 | 0.96 | 0.91–1.02 | 0.165 |
| Diabetes mellitus | 2.03 | 1.32–3.14 | 0.001 | 2.63 | 1.26–5.51 | 0.010 | 1.55 | 0.91–2.65 | 0.110 |
| Dyslipidemia | 0.48 | 0.33–0.70 | <0.001 | 0.51 | 0.27–0.96 | 0.036 | 0.43 | 0.27–0.67 | 0.0003 |
| Hypertension | 2.72 | 1.84–4.02 | <0.001 | 2.52 | 1.32–4.80 | 0.005 | 2.59 | 1.58–4.23 | 0.0002 |
| Family history of CAD | 1.60 | 1.10–2.34 | 0.014 | 0.58 | 0.24–1.38 | 0.215 | 2.21 | 1.42–3.44 | 0.0005 |
| Smoker/ex-smoker | 1.70 | 1.17–2.49 | 0.006 | 1.16 | 0.55–2.42 | 0.703 | 1.76 | 1.12–2.76 | 0.014 |
| Indications for study | |||||||||
| Chest pain | 0.68 | 0.47–0.97 | 0.032 | 0.87 | 0.47–1.62 | 0.658 | 0.68 | 0.44–1.07 | 0.092 |
| Typical angina | 1.06 | 0.60–1.89 | 0.842 | 1.74 | 0.77–3.92 | 0.184 | 0.76 | 0.33–1.75 | 0.519 |
| Dyspnea | 3.78 | 2.43–5.88 | <0.001 | 2.45 | 0.96–6.25 | 0.061 | 3.94 | 2.37–6.54 | <0.0001 |
| NCEP/ATP III risk score | 2.13 | 1.62–2.80 | <0.001 | 2.32 | 1.47–3.68 | 0.0003 | 1.80 | 1.27–2.55 | 0.001 |
| Low risk | 0.37 | 0.23–0.61 | <0.001 | 0.45 | 0.22–0.95 | 0.036 | 0.40 | 0.20–0.80 | 0.010 |
| Intermediate risk | 1.07 | 0.75–1.53 | 0.721 | 0.84 | 0.46–1.55 | 0.581 | 1.08 | 0.69–1.70 | 0.727 |
| High risk | 2.61 | 1.76–3.88 | <0.001 | 3.76 | 1.95–7.25 | <0.0001 | 1.90 | 1.16–3.10 | 0.011 |
| Medications | |||||||||
| Aspirin | 0.89 | 0.61–1.30 | 0.537 | 0.86 | 0.43–1.72 | 0.669 | 0.72 | 0.46–1.14 | 0.161 |
| Statin | 0.65 | 0.43–0.99 | 0.046 | 0.84 | 0.40–1.76 | 0.646 | 0.45 | 0.27–0.75 | 0.002 |
BMI indicates body mass index; CAD, coronary artery disease; CI, confidence interval; and NCEP/ATP, National Cholesterol Education Program/Adult Treatment Panel.
Nonobstructive CAD and All-Cause Mortality
When compared with individuals with normal coronary arteries, patients with nonobstructive CAD in Coronary computed tomographic angiography (CCTA) experienced higher mortality and there was incremental risk both with the number of coronary vessels and the number of coronary segments involved (Table 3; Figure 1). The relationship between the summed total number of segments with nonobstructive CAD and mortality risk was assessed. All segment scores >0 were associated with increased mortality risk, and there was no lower threshold for the absence of mortality risk.
Table 3.
Univariable and Multivariable Hazard Ratios for All-Cause Mortality by Per-Segment, Per-Vessel and Location-Based Coronary Computed Tomographic Angiography-Identified Nonobstructive CAD (Compared With Patients without Coronary Plaque)
| Unadjusted HR | P Value | H NCEP/ATP III Adjusted R | P Value | NCEP/ATP III and Statin Adjusted HR | P Value | |
|---|---|---|---|---|---|---|
| Nonobstructive CAD | 2.47 (1.69–3.60) | <0.001 | 2.17 (1.49–3.18) | <0.0001 | 2.30 (1.56–3.39) | <0.0001 |
| Segment-based analysis | ||||||
| Per additional segment | 1.13 (1.08–1.18) | <0.0001 | 1.12 (1.07–1.17) | <0.0001 | 1.12 (1.07–1.17) | <0.0001 |
| 1–4 segments | 4.02 (2.26–7.18) | <0.0001 | 3.75 (2.10–6.69) | <0.0001 | 3.92 (2.19–6.99) | <0.0001 |
| ≥5 segments | 7.30 (3.97–13.4) | <0.0001 | 6.55 (3.56–12.1) | <0.0001 | 6.82 (3.69–12.6) | <0.0001 |
| Vessel-based analysis | ||||||
| 1 vessel vs no coronary plaque | 1.43 (0.79–2.58) | 0.2407 | 1.25 (0.69–2.26) | 0.462 | 1.33 (0.73–2.41) | 0.3538 |
| 2 vessels vs no coronary plaque | 2.98 (1.77–5.00) | <0.0001 | 2.64 (1.57–4.45) | 0.0003 | 2.84 (1.68–4.81) | 0.0001 |
| 3 vessels vs no coronary plaque | 2.99 (1.94–4.60) | <0.001 | 2.62 (1.70–4.05) | <0.0001 | 2.76 (1.78–4.29) | <0.0001 |
CAD indicates coronary artery disease; HR, hazard ratio; and NCEP/ATP III, National Cholesterol Education Program/Adult Treatment Program III
Figure 1.
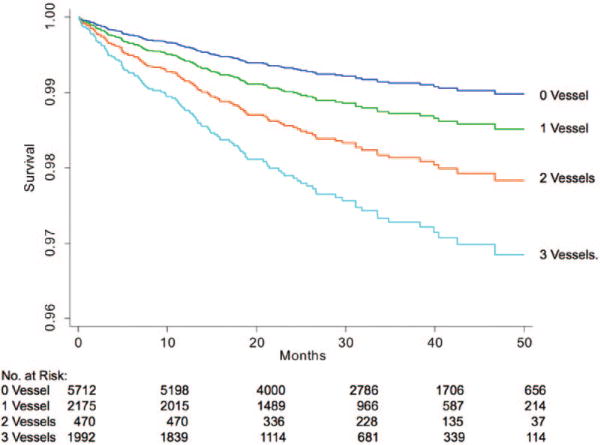
Kaplan–Meier Survival curves as a function of number of major coronary arteries with nonobstructive coronary artery disease (CAD; 0 [blue line], 1 [green line], 2 [red line], and 3 [light blue line] vessels with coronary atherosclerosis).
Statin and Aspirin Primary Prevention and All-Cause Mortality
Statin use at the time of CCTA was associated with lower mortality (0.76% versus 1.31%) and a lower annual death rate (0.33% versus 0.59%; P=0.032). In patients with nonobstructive CAD, the annual death rate was significantly lower in those (0.47% and 1.04%; P=0.002). Conversely, aspirin therapy was not (1.04% versus 1.22%; P=0.473) associated with an improvement in all-cause mortality. In multivariable risk-adjusted models, statin use was associated with a significant survival benefit (HR, 0.52; 95% confidence interval, 0.34–0.79; P=0.002); however, an interaction analysis between statin use and nonobstructive CAD showed the survival benefit of statin use without an obvious difference between those with plaque and those with normal coronary arteries (P=0.233). Further subgroup analysis showed that the effect of statin use was only observed for patients with nonobstructive CAD (HR, 0.39 [0.23–0.65]; P<0.001) and was not observed in patients with normal coronary arteries (HR, 0.64 [0.30–1.37]; P=0.252; Table 4). The lower HR for patients with nonobstructive CAD suggests that a larger study will be needed to identify an interaction (Figures 2 and 3).
Table 4.
Cox Models for All-Cause Mortality in Patients With Nonobstructive CAD
| Models | Hazard Ratio* (95% CI) | P Value |
|---|---|---|
| All patients (n=10 418) | ||
| Statin therapy | 0.52 (0.34–0.79) | 0.002 |
| ASA therapy | 0.77 (0.53–1.12) | 0.173 |
| Nonobstructive CAD (n=4706) | ||
| Statin therapy | 0.39 (0.23–0.65) | <0.001 |
| ASA therapy | 0.66 (0.42–1.04) | 0.070 |
| No coronary plaque (n=5712) | ||
| Statin therapy | 0.64 (0.30–1.37) | 0.252 |
| ASA therapy | 0.73 (0.37–1.47) | 0.384 |
CAD indicates coronary artery disease; and CI, confidence interval.
Adjusted for National Cholesterol Education Program/Adult Treatment Program III risk.
Figure 2.
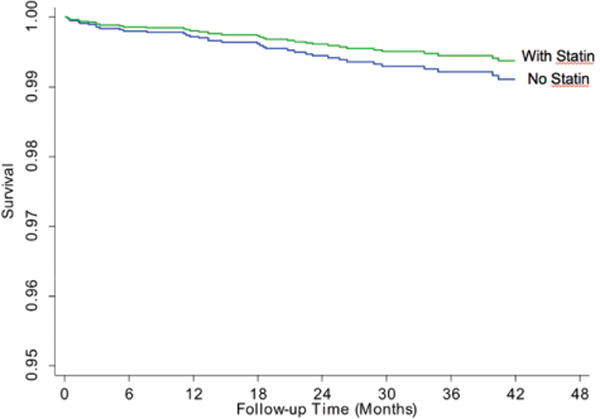
Kaplan–Meier survival curves as a function of statin use in patients without coronary plaque.
Figure 3.
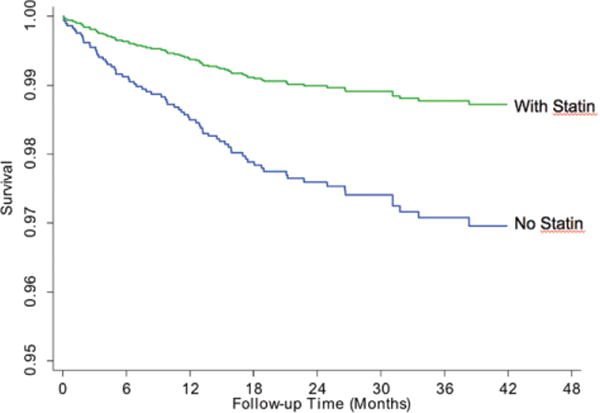
Kaplan–Meier survival curves as a function of statin use in patients with coronary plaque.
When stratified by NCEP/ATP III risk, the beneficial effect of statins was observed in patients with nonobstructive CAD and in a subanalysis of these patients, a significant reduction in mortality was observed in those patients with coronary atherosclerosis and at intermediate NCEP/ATP III risk. A trend was observed in patients at high NCEP/ATP III risk (P=0.060; Table 5). Further subgroup analyses in the univariable models and also multivariable models adjusting for NCEP/ATP III risk, both showed that mortality reduction was also observed across many subgroups taking statins at baseline (Figure 4). Particularly, there was a significant interaction between hypertension and statins (P=0.013) with statins therapy being more effective in hypertensive patients versus normotensive patients (HR, 0.35 [0.20–0.60] versus 1.13 [0.56–2.30]) There was also weak interaction between diabetes mellitus and statin use (P=0.051) such that patients with diabetes mellitus seemed to have a greater benefit from statin therapy. Initial analysis of suggested a trend toward benefit of statin therapy in patients without dyslipidemia. Acknowledging that diabetics could be categorized as without dyslipidemia, a post hoc analysis was performed excluding diabetics. The HR for patients with dyslipidemia was 0.70 (0.28–1.77) and without dyslipidemia was 1.09 (0.55–2.15).
Table 5.
Multivariable Hazard Ratios for All-Cause Mortality of Individuals Treated at Baseline With Statins as Stratified by NCEP/ATP III Risk
| HR | 95% CI | P Value | |
|---|---|---|---|
| Overall study group | |||
| NCEP/ATP III risk | |||
| Low risk | 2.52 | 0.98–6.51 | 0.056 |
| Intermediate risk | 0.39 | 0.21–0.72 | 0.003 |
| High risk | 0.40 | 0.19–0.84 | 0.015 |
| Normal | |||
| NCEP/ATP III risk | |||
| Low risk | 2.55 | 0.64–10.22 | 0.637 |
| Intermediate risk | 0.69 | 0.23–2.07 | 0.503 |
| High risk | 0.25 | 0.06–1.11 | 0.068 |
| Nonobstructive | |||
| NCEP/ATP III risk | |||
| Low risk | 2.07 | 0.55–7.72 | 0.281 |
| Intermediate risk | 0.24 | 0.11–0.52 | <0.001 |
| High risk | 0.45 | 0.19–1.06 | 0.068 |
CI indicates confidence interval; HR, hazard ratio; and NCEP/ATP III, National Cholesterol Education Program/Adult Treatment Program III.
Figure 4.
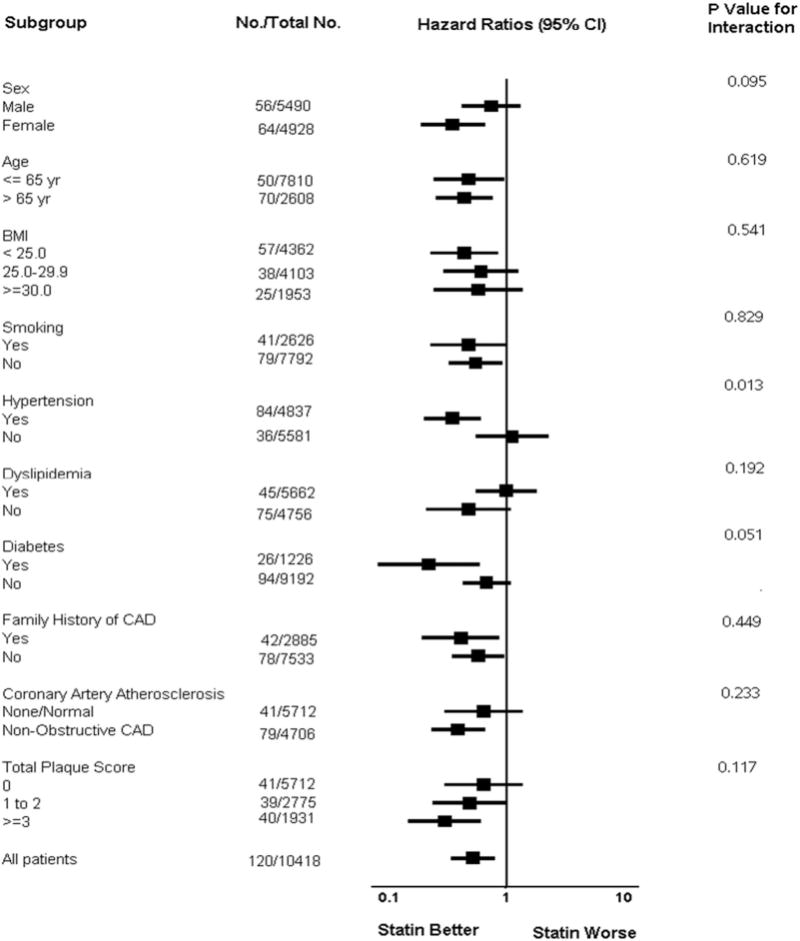
Forest plot of subgroup analyses, adjusted for National Cholesterol Education Program/Adult Treatment Program III Risk. BMI indicates body mass index; CAD, coronary artery disease; and CI, confidence interval.
Discussion
The present study represents the first large prospective multicenter international study to estimate the risk of mortality for patients with nonobstructive CAD, and further determine the therapeutic implications of statin and aspirin use in patients with nonobstructive CAD, stratified by NCEP/ATP III risk. In this intermediate-term follow-up, we identified a relationship between increasing burden of nonobstructive CAD and higher mortality rates and observed a reduction in mortality risk associated with baseline statin therapy but not aspirin, a finding that may be because of a statistical underpowering because of the number of observed events (n=120). This finding was accentuated for individuals with coronary CTA-identified nonobstructive CAD and intermediate NCEP/ATP III risk. Although underpowered, a trend was observed in those patients with high NCEP/ATP III risk and nonobstructive CAD. Importantly, we observed no significant mortality benefit of statins at baseline in those with normal coronary arteries by coronary CTA.
These findings in patients with nonobstructive CAD, extend those of previous studies that have focused primarily on the presence, extent, and severity of obstructive CAD,2,13,14 but confirm those recently observed with invasive coronary angiography.15 Because of the size of our cohort, we were able to examine the hazards of nonobstructive CAD as stratified by NCEP/ATP III risk, and observed a low mortality risk, over the follow-up period, of patients with nonobstructive CAD already considered low risk by clinical risk assessment. As well, during this follow-up period, we identified no mortality benefit associated with statin use in patients who were considered higher clinical risk but without evidence of coronary CTA-identified plaque.
Although it remains possible that some of the nonobstructive lesions (1%–49% diameter stenosis) could result in lesion-specific ischemia, it is likely that these were few in number,16 and more likely to be undetectable using traditional methods of CAD evaluation, such as exercise treadmill testing, stress echocardiography, and myocardial perfusion imaging. Previous investigations have shown that minor coronary stenoses are associated the majority of acute myocardial infarctions and sudden cardiac deaths. Thus, our analysis highlights a potential advantage of atherosclerosis imaging with coronary CTA and its potential to direct patient therapy.
In this regard, the present study findings also sought to examine the benefit of medical therapy for reduction of mortality in individuals with nonobstructive CAD. Although statin therapy is routinely advocated and prescribed for patients with documented cardiovascular disease,17–28 the evidence underlying the efficacy in primary prevention is less robust.10,11,29–32 The Cochrane meta-analysis and a meta-analysis by Kostis et al demonstrated a reduction in total mortality with statin use, whereas a meta-analysis by Ray et al11 showed a strong trend toward benefit but the confidence interval overlapped 1.0.10,32,33 The results of our study further lend support for statin use in primary prevention, specifically in those with subclinical atherosclerosis.
Similarly, the benefit of aspirin therapy for primary prevention has also been questioned.12 At present, statin and aspirin treatment recommendations for primary prevention exist only for patients at high risk of future cardiovascular events. To date, these high-risk classifications have been restricted to definitions based on clinical or laboratory markers, and include diabetes mellitus, dyslipidemia, high Framingham or NCEP/ATP III risk scores, or intermediate Framingham Risk Score with elevated high-sensitivity C-reactive protein.8,9 At present, no uniform recommendation exists for primary prevention therapies based on imaging findings, and results of the present study challenge these recommendations, and suggest that the individual with intermediate or high NCEP/ATP III risk and nonobstructive CAD may derive significant benefit from statin therapy.
Attractive to clinicians and healthcare payers is the potential shift of primary prevention treatment from a population-based treat all patients paradigm to one of individualized tailoring of therapies to those who actually have disease and are actually at risk for incident adverse events. Our study results identified higher risk for patients who had both elevated clinical risk scores and nonobstructive CAD, with no increased risk in individuals who had either one or the other alone. Although it is currently unknown whether statin therapy in patients with subclinical atherosclerosis improves outcomes, the current study results suggest that statin therapy in patients with nonobstructive plaque may be of mortality benefit. Given several recent analyses that have failed to show efficacy of statin or aspirin therapy for primary prevention,10–12 proof that coronary CTA identifies patients who benefit from prevention strategies will require extensive corroboration in longer term follow-up studies and with additional nonfatal and fatal cardiovascular end points. In a collaborative meta-analysis of 6 primary prevention trials (95 000 patients), no apparent mortality benefit was observed with aspirin therapy.12 As such, current guidelines do not recommend aspirin to prevent ischemic vascular events in patients without evidence of manifest vascular disease.29 In daily coronary CTA practice, the identification of patients with nonobstructive CAD is common. Whether the presence of nonobstructive CAD by coronary CTA constitutes manifest vascular disease has remained a clinical challenge, and many clinicians have adopted a protocol of reflexive statin or aspirin use for these patients. However, the use of aspirin was not significantly associated with mortality reduction in our patient cohort, even if coronary atherosclerotic plaque was present. Given the wide confidence intervals associated with aspirin use, caution should be taken when interpreting these results. The HR ratios (0.64 and 0.75) associated with aspirin use may be clinically important but were not statistically significant in our study, which may be a function of power. Additional study is needed before definitive conclusions on aspirin therapy can be made.
Limitations
This study is not without limitations. We included information on statin use at baseline; however, 23% of patients did not have medication information, which could result in a bias in our population. As well, we do not have data on the initial statin dose, subsequent initiation, discontinuation, dose modification, or compliance changes that may have occurred after coronary CTA. Although longitudinal differences in statin use may significantly affect study outcomes, we think that patients already being treated with statins would have been less likely to discontinue therapy after documentation of nonobstructive CAD.30–32 Indeed, the initiation of statins after coronary CTA in individuals with nonobstructive CAD would serve to reduce the apparent difference in outcomes between the statin and no-statin groups and would have resulted in the underestimation rather than overestimation of the true benefit of statin therapy. Conversely patients with normal arteries may have discontinued statin therapy, thereby underestimating the benefit of statins in this subpopulation. Although a recommendation cannot be made on discontinuing statin therapy in those without coronary atherosclerosis on CCTA, Blaha et al33 have previously demonstrated that the absence of coronary calcification in the asymptomatic population portended an excellent prognosis with a 10-year mortality rate of ≈1%. Similarly, there is also a lack of data on pretherapy lipid profiles and subsequent changes in lipid profile, which could also affect our conclusions. Additional large-scale studies examining the impact of statin therapy on outcomes in individuals with nonobstructive CAD by CCTA now seem warranted. Finally, it is possible that the higher use of statins may be explained by factors beyond the scope of this study, such as better access to healthcare or healthier lifestyles.
We used all-cause mortality as the primary end point for our study, given its unparalleled clinical importance and freedom from ascertainment bias. However, as specific causes of death for each patient were not uniformly available at all sites, the true proportion of deaths that may have been attributable to cardiovascular events in the study population is unknown. Also germane to this limitation is that the NCEP/ATP III risk algorithms are aimed at prediction of future cardiovascular events and not all-cause mortality. Consequently, the present study may result in the underestimation of the prognostic power of clinical variables and overestimate those of coronary CTA and statin therapy. Although the capture of other major adverse cardiovascular events (eg, stroke) is desirable, one distinct advantage of using all-cause mortality as a primary outcome measure is its ability to capture adverse deaths that may have been related to medication use (eg, hemorrhagic stroke, liver failure, and rhabdomyolysis).
This study is comprised a cohort of individuals who were clinically referred for coronary CTA for suspected CAD, with the majority being symptomatic. Although our cohort’s symptoms are unlikely to be related to nonobstructive plaque, the generalized application of our study findings to asymptomatic individuals remains uncertain.
Conclusions
In this intermediate-term follow-up of individuals undergoing CCTA, the presence and extent of nonobstructive CAD are associated with increased mortality. Baseline statin therapy seems to be associated with a significant reduction in mortality for individuals with nonobstructive CAD. Future studies applying targeted therapies to patients with nonobstructive CAD should be considered. Whether statin therapy benefits those with normal coronary arteries remains uncertain and requires further investigation.
Supplementary Material
Significance.
This study was to examine a large-scale population of patients with nonobstructive coronary artery disease—as diagnosed by coronary computed tomographic angiography—and to examine the prognosis of these findings in relation to treatment with statins and aspirin. This study found that statins, but not aspirin, was highly efficacious at reducing the rates of death for patients with nonobstructive plaque.
Acknowledgments
Sources of Funding: Research reported in this publication was supported by the Heart Lung and Blood Institute of the National Institutes of Health under award numbers 1R01HL115150 and R011HL118019. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This research was also supported by Leading Foreign Research Institute Recruitment Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (MSIP; 2012027176). This study was also funded, in part, by a generous gift from the Dalio Institute of Cardiovascular Imaging and the Michael Wolk Foundation.
Nonstandard Abbreviations and Acronyms
- CAD
coronary artery disease
- CTA
computed tomographic angiography
- HR
hazard ratio
- NCEP/ATP III
National Cholesterol Education Program/Adult Treatment Program III
Footnotes
This manuscript was sent to Robert A. Hegele, Consulting Editor, for review by expert referees, editorial decision, and final disposition.
The online-only Data Supplement is available with this article at http://atvb.ahajournals.org/lookup/suppl/doi:10.1161/ATVBAHA.114.304351/-/DC1.
Arterioscler Thromb Vasc Biol is available at http://atvb.ahajournals.org
Disclosures
Dr Min serves as a consultant to HeartFlow. The other authors report no conflicts.
References
- 1.Chow BJ, Abraham A, Wells GA, Chen L, Ruddy TD, Yam Y, Govas N, Galbraith PD, Dennie C, Beanlands RS. Diagnostic accuracy and impact of computed tomographic coronary angiography on utilization of invasive coronary angiography. Circ Cardiovasc Imaging. 2009;2:16–23. doi: 10.1161/CIRCIMAGING.108.792572. [DOI] [PubMed] [Google Scholar]
- 2.Chow BJ, Wells GA, Chen L, Yam Y, Galiwango P, Abraham A, Sheth T, Dennie C, Beanlands RS, Ruddy TD. Prognostic value of 64-slice cardiac computed tomography severity of coronary artery disease, coronary atherosclerosis, and left ventricular ejection fraction. J Am Coll Cardiol. 2010;55:1017–1028. doi: 10.1016/j.jacc.2009.10.039. [DOI] [PubMed] [Google Scholar]
- 3.Chow BJ, Freeman MR, Bowen JM, et al. Ontario multidetector computed tomographic coronary angiography study: field evaluation of diagnostic accuracy. Arch Intern Med. 2011;171:1021–1029. doi: 10.1001/archinternmed.2011.74. [DOI] [PubMed] [Google Scholar]
- 4.Leber AW, Knez A, von Ziegler F, Becker A, Nikolaou K, Paul S, Wintersperger B, Reiser M, Becker CR, Steinbeck G, Boekstegers P. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol. 2005;46:147–154. doi: 10.1016/j.jacc.2005.03.071. [DOI] [PubMed] [Google Scholar]
- 5.Kass M, Glover CA, Labinaz M, So DY, Chen L, Yam Y, Chow BJ. Lesion characteristics and coronary stent selection with computed tomographic coronary angiography: a pilot investigation comparing CTA, QCA and IVUS. J Invasive Cardiol. 2010;22:328–334. [PubMed] [Google Scholar]
- 6.van Velzen JE, Schuijf JD, de Graaf FR, Boersma E, Pundziute G, Spanó F, Boogers MJ, Schalij MJ, Kroft LJ, de Roos A, Jukema JW, van der Wall EE, Bax JJ. Diagnostic performance of non-invasive multidetector computed tomography coronary angiography to detect coronary artery disease using different endpoints: detection of significant stenosis vs. detection of atherosclerosis. Eur Heart J. 2011;32:637–645. doi: 10.1093/eurheartj/ehq395. [DOI] [PubMed] [Google Scholar]
- 7.Pohle K, Achenbach S, Macneill B, Ropers D, Ferencik M, Moselewski F, Hoffmann U, Brady TJ, Jang IK, Daniel WG. Characterization of non-calcified coronary atherosclerotic plaque by multi-detector row CT: comparison to IVUS. Atherosclerosis. 2007;190:174–180. doi: 10.1016/j.atherosclerosis.2006.01.013. doi:10.1016/j. atherosclerosis.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 8.National Cholesterol Education Program Expert Pane on Detection… Final Report. Washington, DC: National Institutes of Health; 2009. [Google Scholar]
- 9.Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult – 2009 recommendations. Can J Cardiol. 2009;25:567–579. doi: 10.1016/s0828-282x(09)70715-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taylor F, Ward K, Moore TH, Burke M, Davey Smith G, Ward K, Ebrahim S. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2011:CD004816. doi: 10.1002/14651858.CD004816.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ray KK, Seshasai SR, Erqou S, Sever P, Jukema JW, Ford I, Sattar N. Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch Intern Med. 2010;170:1024–1031. doi: 10.1001/archinternmed.2010.182. [DOI] [PubMed] [Google Scholar]
- 12.Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, Meade T, Patrono C, Roncaglioni MC, Zanchetti A. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373:1849–1860. doi: 10.1016/S0140-6736(09)60503-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ostrom MP, Gopal A, Ahmadi N, Nasir K, Yang E, Kakadiaris I, Flores F, Mao SS, Budoff MJ. Mortality incidence and the severity of coronary atherosclerosis assessed by computed tomography angiography. J Am Coll Cardiol. 2008;52:1335–1343. doi: 10.1016/j.jacc.2008.07.027. [DOI] [PubMed] [Google Scholar]
- 14.Jespersen L, Hvelplund A, Abildstrøm SZ, Pedersen F, Galatius S, Madsen JK, Jørgensen E, Kelbæk H, Prescott E. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012;33:734–744. doi: 10.1093/eurheartj/ehr331. [DOI] [PubMed] [Google Scholar]
- 15.Gould KL, Lipscomb K, Hamilton GW. Physiologic basis for assessing critical coronary stenosis. Instantaneous flow response and regional distribution during coronary hyperemia as measures of coronary flow reserve. Am J Cardiol. 1974;33:87–94. doi: 10.1016/0002-9149(74)90743-7. [DOI] [PubMed] [Google Scholar]
- 16.Randomized trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 17.Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA, Langendorfer A, Stein EA, Kruyer W, Gotto AM., Jr Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279:1615–1622. doi: 10.1001/jama.279.20.1615. [DOI] [PubMed] [Google Scholar]
- 18.Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, McKillop JH, Packard CJ. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:1301–1307. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 19.Shepherd J, Blauw GJ, Murphy MB, et al. PROSPER study group PROspective Study of Pravastatin in the Elderly at Risk. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–1630. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- 20.Knopp RH, d’Emden M, Smilde JG, Pocock SJ. Efficacy and safety of atorvastatin in the prevention of cardiovascular end points in subjects with type 2 diabetes: the Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in non-insulin-dependent diabetes mellitus (ASPEN) Diabetes Care. 2006;29:1478–1485. doi: 10.2337/dc05-2415. [DOI] [PubMed] [Google Scholar]
- 21.Asselbergs FW, Diercks GF, Hillege HL, van Boven AJ, Janssen WM, Voors AA, de Zeeuw D, de Jong PE, van Veldhuisen DJ, van Gilst WH, Prevention of Renal and Vascular Endstage Disease Intervention Trial (PREVEND IT) Investigators Effects of fosinopril and pravastatin on cardiovascular events in subjects with microalbuminuria. Circulation. 2004;110:2809–2816. doi: 10.1161/01.CIR.0000146378.65439.7A. [DOI] [PubMed] [Google Scholar]
- 22.Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. [Google Scholar]
- 23.Minder CM, Blaha MJ, Horne A, Michos ED, Kaul S, Blumenthal RS. Evidence-based use of statins for primary prevention of cardiovascular disease. Am J Med. 2012;125:440–446. doi: 10.1016/j.amjmed.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 24.Kostis WJ, Cheng JQ, Dobrzynski JM, Cabrera J, Kostis JB. Meta-analysis of statin effects in women versus men. J Am Coll Cardiol. 2012;59:572–582. doi: 10.1016/j.jacc.2011.09.067. [DOI] [PubMed] [Google Scholar]
- 25.Bell AD, Roussin A, Cartier R, et al. The use of antiplatelet therapy in the outpatient setting: Canadian Cardiovascular Society Guidelines Executive Summary. Can J Cardiol. 2011;27:208–221. doi: 10.1016/j.cjca.2010.12.033. doi:10.1016/j. cjca.2010.12.033. [DOI] [PubMed] [Google Scholar]
- 26.Kalia NK, Miller LG, Nasir K, Blumenthal RS, Agrawal N, Budoff MJ. Visualizing coronary calcium is associated with improvements in adherence to statin therapy. Atherosclerosis. 2006;185:394–399. doi: 10.1016/j.atherosclerosis.2005.06.018. doi:10.1016/j. atherosclerosis.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 27.Orakzai RH, Nasir K, Orakzai SH, Kalia N, Gopal A, Musunuru K, Blumenthal RS, Budoff MJ. Effect of patient visualization of coronary calcium by electron beam computed tomography on changes in beneficial lifestyle behaviors. Am J Cardiol. 2008;101:999–1002. doi: 10.1016/j.amjcard.2007.11.059. doi:10.1016/j. amjcard.2007.11.059. [DOI] [PubMed] [Google Scholar]
- 28.Wong ND, Detrano RC, Diamond G, Rezayat C, Mahmoudi R, Chong EC, Tang W, Puentes G, Kang X, Abrahamson D. Does coronary artery screening by electron beam computed tomography motivate potentially beneficial lifestyle behaviors? Am J Cardiol. 1996;78:1220–1223. doi: 10.1016/s0002-9149(96)00599-1. [DOI] [PubMed] [Google Scholar]
- 29.Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. The Long-Term Intervention with Pravastatin in Ischemic Disease (LIPID) Study Group. N Engl J Med. 1998;339:1349–1357. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 30.Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, Jr, Kastelein JJ, Koenig W, Libby P, Lorenzatti AJ, MacFadyen JG, Nordestgaard BG, Shepherd J, Willerson JT, Glynn RJ, JUPITER Study Group Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 31.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT-LLT) JAMA. 2002;288:2998–3007. doi: 10.1001/jama.288.23.2998. [DOI] [PubMed] [Google Scholar]
- 32.Sever PS, Dahlöf B, Poulter NR, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O’Brien E, Ostergren J, ASCOT investigators Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003;361:1149–1158. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- 33.Blaha M, Budoff MJ, Shaw LJ, Khosa F, Rumberger JA, Berman D, Callister T, Raggi P, Blumenthal RS, Nasir K. Absence of coronary artery calcification and all-cause mortality. JACC Cardiovasc Imaging. 2009;2:692–700. doi: 10.1016/j.jcmg.2009.03.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


