Abstract
The geko™ device is a single-use, battery-powered, neuromuscular electrostimulation device that aims to reduce the risk of venous thromboembolism (VTE). The National Institute for Health and Care Excellence (NICE) selected the geko™ device for evaluation, and invited the manufacturer, Firstkind Ltd, to submit clinical and economic evidence. King’s Technology Evaluation Centre, an External Assessment Centre (EAC) commissioned by the NICE, independently assessed the evidence submitted. The sponsor submitted evidence related to the geko™ device and, in addition, included studies of other related devices as further clinical evidence to support a link between increased blood flow and VTE prophylaxis. The EAC assessed this evidence, conducted its own systematic review and concluded that there is currently limited direct evidence that geko™ prevents VTE. The sponsor’s cost model is based on the assumption that patients with an underlying VTE risk and subsequently treated with geko™ will experience a reduction in their baseline risk. The EAC assessed this cost model but questioned the validity of some model assumptions. Using the EACs revised cost model, the cost savings for geko™ prophylaxis against a ‘no prophylaxis’ strategy were estimated as £197 per patient. Following a second public consultation, taking into account a change in the original draft recommendations, the NICE medical technologies guidance MTG19 was issued in June 2014. This recommended the adoption of the geko™ for use in people with a high risk of VTE and when other mechanical/pharmacological methods of prophylaxis are impractical or contraindicated in selected patients within the National Health Service in England.
Key Points for Decision Makers
| The geko™ device is a small neuromuscular electrostimulation device that may reduce the risk of venous thromboembolism (VTE). |
| The National Institute for Health and Care Excellence Medical Technologies Evaluation Programme assessed the geko™ device for use in people for whom other methods of prophylaxis are impractical or contraindicated and who have a high risk of VTE. |
| The estimated cost savings for the geko™ device in patients at high risk of VTE compared with no prophylaxis was £197 per patient. |
| In June 2014, the geko™ device was recommended for adoption within the NHS for people who have a high risk of VTE and for whom other mechanical and pharmacological methods of prophylaxis are impractical or contraindicated. |
Introduction
The role of the National Institute for Health and Care Excellence (NICE) is to provide guidance and advice to improve health and social care within the National Health Service (NHS) in England [1]. Part of this role involves selecting and evaluating new or innovative medical technologies for potential adoption within the NHS in England. The NICE Medical Technologies Evaluation Programme (MTEP) undertakes this evaluation. The MTEP requires that for technologies to be eligible for evaluation they must be suitable for NICE guidance, be a new or innovative technology and have a current CE (Conformité Européenne) mark or equivalent regulatory approval, or be expecting one within 12 months [2].
The Medical Technologies Advisory Committee (MTAC) selects new or innovative technologies for evaluation which they consider to have the potential to provide significant benefits to patients and/or the NHS compared with current practice. Technologies must be likely to have the potential either to provide additional benefit to patients at the same or lower cost to the NHS, or to provide equivalent benefit to patients at lower cost to the NHS. All selected technologies proceed through a prescribed evaluation process, which has a timeline of approximately 38 weeks [3]. The MTEP produces a scope outlining the technology, the intended population and expected outcomes. The manufacturer then submits clinical and economic evidence, which meets the NICE scope. An NICE-funded External Assessment Centre (EAC) assesses this evidence independently. The EAC will produce a report based on this evidence and any additional evidence that was not part of the original manufacturer’s submission, which may involve additional review/meta-analyses and/or economic modelling. Input from both public submissions and independent expert advisors, alongside the submitted evidence and the EAC’s report, are all considered by the MTAC at the end of the evaluation process before issuing guidance for the technology.
The geko™ device, manufactured by Firstkind Ltd, is a neuromuscular electrostimulation (NMES) device that is intended to reduce the risk of venous thromboembolism (VTE). In June 2014, the NICE issued a final guidance (MTG19) on this technology [4]. This article presents a summary of the EAC report and the contribution towards the NICE guidance for the geko™ device. It is among a series of NICE medical technology guidance summaries published in Applied Health Economics and Health Policy [5–9].
Decision Problem
Disease Overview
VTE is a collective term for both deep vein thrombosis (DVT) and pulmonary embolism (PE), and is a clinical condition in which a thrombus (blood clot) forms in a vein and travels in the blood [10, 11]. In England, it is estimated that 25,000 people die from hospital-acquired VTE every year [12].
DVT occurs when a thrombus forms in the deep veins, usually in the legs, and is the most common form of VTE. The majority of DVT-related deaths are a result of PE, and the Office for National Statistics for England and Wales reports that DVT (International Classification of Diseases, Tenth Revision [ICD-10] I80.1–I80.3, I80.0 and I82.9) was the underlying cause of death for 3,798 individuals in 2010 [13].
A PE is a potentially fatal cardiovascular event, which occurs when a thrombus dislodges from its original site in the vein, travels in the blood, and subsequently blocks blood flow in the pulmonary artery. It is suspected that many PEs are undiagnosed due to diagnostic difficulties [14]; however, PE remains one of the most common causes of inpatient deaths in the UK, estimated to be between 2 and 10 % of inpatient deaths annually in the UK [12, 14].
The clinical symptoms of VTE vary significantly and in some cases it can be asymptomatic. The clinical presentation of VTE may consist of any of the following: leg swelling/pain, muscle tenderness or cyanosis. More specific PE symptoms include dyspnoea, chest pain, fever, haemoptysis or syncope [15, 16]. A common complication of DVT is post-thrombotic syndrome (PTS), which is estimated to occur in more than one-third of all patients diagnosed with DVT [17]. Symptoms of PTS include recurrent pain/swelling in the legs, skin changes and recurrent leg ulcers [10, 18].
The causes of VTE are not clearly understood, but three clinical features are generally thought to be relevant: venous stasis, hypercoagulability, and endothelial damage/dysfunction. These three components represent Virchow’s triad—a categorised representation of the clinical factors that predispose to thrombosis [19]. Risk factors for VTE are considered to be a combination of both patient-related and setting-related predisposing factors [20]. Patient-related risks include, but are not limited to, age, hormonal therapy, dehydration, active cancer, obesity, one or more significant medical comorbidities, varicose veins, superficial VTE, and known thrombophilias [20, 21]. Recent surgery, hospitalization, recent trauma and immobilization are considered setting-related risk factors for VTE [20, 21]. Furthermore, DVT, or previous DVT, or PE have been shown to increase the risk for future VTE [10].
Risk Assessment and Current Treatment Options
The NICE clinical guideline 92 (CG92) outlines the clinical management of VTE in all patients admitted to hospital in the UK [10]. This guideline recommends that all patients admitted to UK hospitals are assessed for VTE risk within 24 h of admission and in the event of any clinical changes [22, 23]. NICE Pathways outlines a diagnostic tool for estimating the probability of VTE in primary, secondary and tertiary care [24]. This clinical prediction tool uses an adapted two-level DVT/PE Wells score to produce a risk score for DVT or PE [24, 25] (Appendix 1). A patient with a high score is regarded as being at-risk for VTE, and the NICE recommends, where appropriate, the introduction of suitable prophylaxis. Other methods used for diagnosing VTE include tests to detect thrombus, i.e. D-dimer assay, ultrasound or venography, ventilation-perfusion (V/Q) scan, multidetector helical computed tomography (CT) and pulmonary angiography [26, 27].
The current standard VTE prophylaxis for patients includes both pharmacological and/or mechanical methods. To determine the most appropriate prophylaxis, several patient-related factors must be considered: the reason for hospitalisation, medical history, expected treatment from the intervention, possible harm of prophylaxis and patient preference. Pharmacological prophylaxis can consist of the following: low-molecular-weight heparin (or unfractionated heparin [UFH] for patients with severe renal impairment or established renal failure), and fondaparinux [23]. If a patient is considered to have a risk of bleeding, and this risk outweighs the risk of VTE, pharmacological prophylaxis will not be offered [23]. Mechanical methods include anti-embolism stockings (thigh- or knee-length), intermittent pneumatic compression (IPC) [thigh- or knee-length] or foot impulse devices (FID) [23]. CG92 recommends that all surgical patients receive both forms of prophylaxis (if pharmacological prophylaxis is not contraindicated) and that all general medical patients are only given mechanical VTE prophylaxis if pharmacological prophylaxis is contraindicated.
If VTE is confirmed via diagnostic tests or suspected based on the Wells score, there are several treatment options possible [28]. Anticoagulation medication (such as heparin or warfarin) may be prescribed to prevent blood clots getting bigger. Compression stockings can be used to prevent and/or reduce leg pain/swelling and also reduce the chance of developing PTS. Patients may also be advised to elevate their leg to help relieve pressure in the veins of the calf. In the event that a patient develops a PE, along with the use of anticoagulation medication, surgery may be required to remove the thrombus directly.
The geko™ Device
The geko™ device is a single-use, non-invasive NMES device that is intended to reduce the risk of VTE, and is manufactured by Firstkind Ltd, a wholly owned subsidiary of Sky Medical Technology Ltd, UK [29]. In October 2010, the device received a CE mark as a Class IIa medical device, to increase blood circulation and for the prevention of venous thrombosis. It is currently available for use in Europe, Australia, New Zealand and Canada. This CE mark was extended in 2013 to include preventing and treating oedema, promoting wound healing and treating venous insufficiency and ischaemia.
The geko™ device is a small (149 mm × 42 mm × 11 mm), lightweight (18 g), self-adhesive, disposable device that is powered by a non-replaceable, lithium battery [30, 31] (see Fig. 1). It is only available in the one size, and does not restrict movement of the knee. It has seven stimulation modes with selectable pulse widths of 70, 100, 140, 200, 280, 400 and 560 µs (± 5 % + 20 µs) [29]. The repetition rate is 1 Hz (± 5 %), with a maximum charge of 20 µC per pulse. The device is intended to be used for up to 24 h (maximum of 30 h) before being replaced. It has a shelf-life of 2 years.
Fig. 1.

The geko™ device [32]
The primary device fitting location positions the head of the device to the side of the knee over the top of the fibula, with the tail wrapping to the rear of the leg below the crease of the knee [33] (see Fig. 2). Alternative fitting locations align the head of the device with the outer tendon, either below the crease of the knee or above the crease of the knee. It is possible to have a device placed on one leg or on both legs simultaneously. The device aims to imitate the effect normally achieved by walking by emitting an electrical impulse which stimulates the common peroneal nerve [31]. This in turn leads to contraction of the calf muscle, aiding the emptying of veins in the lower limb(s) and increasing blood circulation to the heart.
Fig. 2.
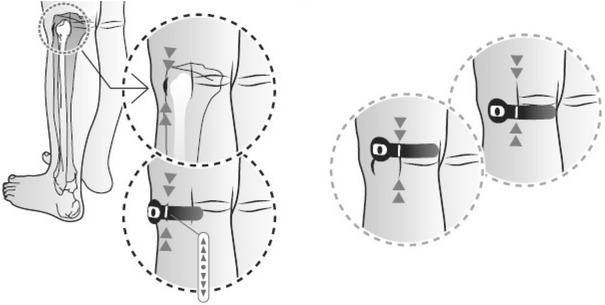
Location of application of the geko™ device [32]. The primary fitting location is for the geko™ device to be positioned over the top of the fibula. Alternative fitting locations are aligned with the outer tendon, below or above the crease of the knee
National Institute for Health and Care Excellence (NICE) Scope
The final scope for the geko™ for VTE prophylaxis was developed by the NICE in consultation with relevant bodies, and published on 21 June 2013 [31]. The scope defined the patient population as: “People at risk of VTE and for whom current mechanical methods of prophylaxis are impractical or contraindicated. The device is most likely to be initiated in a hospital inpatient setting”. The standard prophylaxis for VTE consists of mechanical and/or pharmacological methods (as described in detail earlier), and the scope defined the comparator for this evaluation as ‘no mechanical prophylaxis’. The outcome measures specified for consideration were venous transit time, blood flow/velocity, incidence of PTS, DVT, PE and/or VTE, patient adherence, length of hospital stay and device-related adverse events.
The scope requested that the cost analysis use ‘no mechanical prophylaxis’ as the comparator, and required a sufficient time horizon and sensitivity analysis to be undertaken in order to address any uncertainties in the model parameters. Two specific subgroups were to be considered: (1) those in whom pharmacological prophylaxis is contraindicated; and (2) those in whom pharmacological prophylaxis is indicated and prescribed. Patients with “fragile skin (for example, older patients and children) and those with burns and skin conditions within the application area of the device” and “patients whose common peroneal nerve or device application is inaccessible or where the common peroneal nerve function is impaired” were specified in the scope as requiring special consideration.
External Assessment Centre (EAC) Review
The manufacturer’s submission consisted of two sections: clinical evidence and economic evidence. The clinical section consisted of an overview and systematic review of clinical evidence related to the geko™ device and related devices (NMES, muscular electrostimulation [MEST], IPC and FID). The economic evidence provided by the sponsor consisted of a decision-tree cost model in the absence of direct economic evidence for the geko™ device.
The NICE commissioned King’s Technology Evaluation Centre (KiTEC), an EAC based in the King’s Health Partners Academic Health Science Centre (KHP), to critique the manufacturer’s submission.
Clinical Effectiveness Evidence
The sponsor provided a search strategy that was divided into three sections. The first search strategy related specifically to studies that used the geko™ device. The second and third search strategies related to data on non-pharmacological comparators (NMES and IPC). The sponsor stated that the studies using NMES and IPC devices were included “as evidence on the association between increased blood flow and a reduction in DVT”. The EAC considered that all three search strategies should be regarded as clinical evidence.
The sponsor’s search identified 31 published papers, of which 21 were considered relevant by the sponsor. Of these 21 papers, one related to geko™ (non-randomised controlled trial [non-RCT]), 13 related to NMES (seven RCT, six non-RCT), and seven related to IPC (five RCT, two non-RCT). The sponsor conducted a search for unpublished studies and within their own database, and identified a further six studies. Three of the identified studies were based on a PhD thesis [34]. A search for unpublished studies related to NMES and IPC was not conducted by the sponsor (see Appendix 2 for a list of the included studies).
All geko™ studies reported by the sponsor were descriptive, were within single centres in the UK and were conducted on healthy volunteers aged between 18 and 65 years. The application period of the geko™ device varied by study, and the use of comparators also varied substantially; for example, several studies compared the use of geko™ with IPC, one compared the geko™ device with baseline measures in addition to voluntary dorsiflexions, and one study compared geko™ in subjects with and without a plaster cast and in different positions.
The NMES studies identified by the sponsor also varied in design, from single-centre to multicentre studies, RCT and non-RCT, and blinded and non-blinded. They are a combination of studies conducted among healthy volunteers (six studies) and medical/surgical patients (nine studies). The evidence related to IPC consisted of five RCTs and two observational prospective studies, all of which were conducted among surgical patients.
Critique of Clinical Effectiveness Evidence
The EAC considered that the sponsor had submitted all of the available evidence related to the geko™ device, including internal post-market surveillance and an interim report. Seven studies related directly to the use of the geko™ device. Of these, all were descriptive studies; there was a combination of published and unpublished manuscripts, and all studies recruited only healthy volunteers. Three of these studies were considered by the EAC as providing a suitable comparator, as defined in the final scope (no mechanical prophylaxis) [35]. These studies provided clinical evidence that the geko™ device increased blood flow in healthy volunteers.
Four of the geko™ studies identified by the sponsor were rejected using the EAC search criteria. The study by Tucker et al. [38] was rejected as the comparator measures were not controlled adequately and voluntary muscle action (dorsiflexions), neither of which are listed comparators in the scope. In the study by Warwick et al. [64], the EAC considered that the lack of a control appropriate to the scope, as well as the use of cardiac outcomes in the study by Jawad [39], meant that these studies fell outside the prescribed scope. The study by Williams et al. [40] did not provide sufficient detail of how baseline measurements were obtained, and therefore the EAC could not determine whether this baseline measurement was suitable as a comparator, as defined in the scope.
The application period of the geko™ device varied substantially between studies, ranging from 15 min to 4 h. Current management of VTE risk according to the NICE CG92 recommends the use of prophylaxis continually “until the risk of VTE recedes with recovery and mobilization, generally 5 to 7 days”. Therefore, the EAC questioned the appropriateness of the geko™-related studies submitted by the sponsor, given that none assessed the device over a time period similar to that used in the relevant clinical setting.
Seven outcomes are listed in the scope; however, only one of these outcomes (venous transit time, blood flow and blood velocity) is considered in the geko™ studies included by the sponsor as clinical evidence. The EAC concluded that there are two reasons for this. First, there is currently limited clinical evidence regarding the geko™ device, therefore the sponsor included NMES/MEST and IPC studies to support a link between increased blood flow and VTE prophylaxis. Second, the sponsor failed to include certain outcome terms in the systematic review. To address this, the EAC conducted a revised systematic review with additional search terms related to outcomes, as defined in the scope. The sponsor excluded studies that used a pharmacological intervention, which the EAC considered inappropriate given that patients receiving pharmacological prophylaxis are listed as a subgroup in the scope. Therefore, the EAC included this subgroup in its systematic review and also reinstated the two exclusions listed in the sponsor’s search strategy. Whilst the EAC identified additional relevant NMES/MEST and IPC studies (n = 5 additional studies [41–45]), they did not add to or alter the EAC’s opinion that there is currently little direct clinical evidence that geko™ prevents VTE, and that such evidence as there is depends on an unproven assumption that blood-flow measurements predict VTE risk.
All geko™ studies included only healthy volunteers, and may therefore not be generalizable to a typical patient population. These studies used exclusion criteria and/or performed prior screening of their subjects to exclude any subjects presenting with a known risk factor for VTE. The EAC judged that the population defined in the scope would include subjects with conditions that may impair the effectiveness of geko™ (e.g. oedema, chemical or physical muscle paralysis, venous insufficiency and adipose tissue insulating the stimulation area). These factors were effectively ruled out by the exclusion criteria used in the sponsor-submitted evidence. Therefore, the EAC considered the population used in the evidence to differ from the population defined in the scope in ways that might have a bearing on effectiveness. Outcome measurements varied substantially between the geko™ studies, therefore no meta-analysis or synthesis could be conducted by the sponsor or the EAC.
The sponsor also provided several studies using NMES and IPC devices, several of which included a suitable comparator, as defined in the scope. Only two NMES studies directly investigated the incidence of DVT alongside measures of blood flow—Nicolaides et al. [46] and Velmahos et al. [47]—as well as four of the NMES studies [45, 48–50], which used an older style of NMES device that could only be used while patients were under general anaesthesia. Of the IPC studies, most compared IPC or FID with a pharmacological intervention. The EAC did not consider these to be relevant to the scope, and therefore subsequently excluded these studies.
Overall, none of the geko™, NMES and IPC studies included by the sponsor analysed any potential statistical association between changes in blood flow and/or velocity in relation to incidence of DVT or PE/VTE. No reported studies assessed the outcomes of PTS or length of hospital stay, as listed in the scope. There are important differences in both the method of application and the type of electrical stimulation used by the various geko™, MEST and NMES devices used in the studies.
Economic Evidence
The manufacturer submitted details of the search strategy designed to retrieve relevant health economic studies from published and unpublished literature. The conclusion was that no economic evidence was available for geko™ or other NMES/MEST devices. Therefore, the manufacturer submitted a decision-tree cost model from the NHS and personal social services perspective using prices from 2012. The decision-tree structure is an amended version of that used in the NICE VTE guidelines [10]. The cost model assessed the impact of geko™ in the patient population for whom current mechanical methods of prophylaxis are impractical or contraindicated. The comparator, as per the scope, was no mechanical prophylaxis, and the subgroup analysis related to the use of pharmaceutical prophylaxis (i.e. combined prophylaxis) and to stroke patients.
The model, as well as all subsequent estimated cost impacts relating to geko™, was built on the assumption that patients who have an underlying risk of DVT, and who are subsequently administered the geko™ device, will experience a reduction in their baseline risk of DVT. The model then assumed that a proportion of those patients who experienced DVT would progress to PE, while the remainder would have either asymptomatic or symptomatic DVT.
Subsequently, a proportion of patients were also assumed to experience PTS, a permanent comorbidity that can generate costs over the patient’s lifetime. Furthermore, it was also assumed that the PE patients have a risk of death. The time horizon for the decision tree was 1 year, within which time most of the costs associated with prophylaxis, DVT and PE treatment were assumed to occur. The model included the lifetime (15 years) cost of PTS.
Most of the clinical parameters (Appendix 3) used in the model were based on the NICE VTE guideline [10] and other published literature [49]. The important data sources for costs included the annual Personal Social Services Research Unit (PSSRU) unit cost compendium [51], NHS reference costs [52] and other literature [53].
The manufacturer estimated the cost per patient within the decision model for geko™ to be £359, and that of the comparator (no prophylaxis) to be £565, resulting in a cost saving for geko™ of £206 per patient. Univariate and probabilistic sensitivity analysis also showed that geko™ is cost-saving compared with no prophylaxis. In the subgroup analysis, compared with pharmacological prophylaxis alone, geko™ in combination with pharmacological prophylaxis was not estimated to be a cost-saving option, with an incremental cost of £69.
Critique of Economic Evidence
The EAC reviewed the search strategy and considered it appropriate. The EAC additionally searched the NHS Economic Evaluation Database (EED), which was not included by the manufacturer. The EAC found no further useful publications, substantiating the conclusions reached by the sponsor that no economic evidence is available for geko™ or other NMES/MEST devices.
The EAC considered that most of the base-case clinical parameters and cost estimates used were appropriate and, wherever there was uncertainty, appropriate sensitivity analysis was used. The cost model was credible since it was an amended version of a model that has been used to develop existing NICE guidelines. The major difference between the NICE VTE model and the sponsor’s model is that the NICE considered DVT and PE as separate arms in the model, whereas the sponsor modelled PE to commonly occur as a result of DVT, which the EAC believed was a reasonable amendment to make. The EAC did not find any areas for improvement and considered the model structure, with its assumptions, pathways and health states, to be sound.
The EAC did not agree with the sponsor’s choice of the relative risk of 0.39 for DVT with the geko™ device, as used in the base-case analysis. This estimated relative risk was based on the incidence of DVT following use of NMES, as reported in the literature [49]. The manufacturer justified the use of this relative risk value with reference to the fact that it falls within the range (0.31–0.58) identified for IPC devices in the NICE VTE guidelines [10]. The EAC believed that this was a weak assumption to make in the absence of clinical evidence that directly links the use of geko™ with a reduction in the risk of DVT. The manufacturer had used clinical evidence to infer that if geko™ improves venous flow by the same amount as IPC, it can be assumed to have the same efficacy as IPC in preventing VTE. The EAC considered this assumption to be unsubstantiated since, while IPC devices have been shown clinically to reduce the incidence of VTE, this prophylactic effect may relate to any combination of the three components of Virchow’s Triad, not just increased venous blood flow [54]. Two of the nominated experts expressed the opinion that venous volume and venous distension factors may play important roles. It is not known which of these effects, or combination of effects, has the greatest impact on VTE prophylaxis [54, 55].
Furthermore, the relative risk pertaining to NMES/MEST devices may not apply to the geko™ device since the devices produce very different types of muscle contractions. Responses from NICE experts on this point were mixed, although most of them indicated that it was not appropriate to use the NMES/MEST evidence, especially from old studies in which the electrical stimuli used were strong, painful and need to be used under general anaesthesia.
For the costing, the manufacturer estimated the administration time for geko™ by a nurse to be around 1.5 min per day. The cost per administration of £1.02 in the manufacturer’s model was based on an hourly cost of £41 for a ward nurse [51]. However, the EAC considered that since this was a patient contact task, an hourly cost of £100 [51] should have been used, and this would give a cost per administration of £2.50. The EAC used this cost to re-estimate the cost savings of geko™ in the base-case analysis. Based on this change, the total cost per patient for geko™ prophylaxis was £368 (instead of £359), against £565 for the ‘no prophylaxis’ strategy. This changed the cost savings of geko™ from £206 to £197 per patient.
Conclusions of the EAC
The sponsor submitted all clinical evidence related to the geko™ device. The sponsor’s evidence relied on the assumption that efficacy in VTE prophylaxis can be assessed for geko™ by comparing its effect on venous blood-flow volume with that of IPC devices. The EAC considered the outcome of venous blood flow to be a surrogate for prevention of VTE, and noted the conclusions of a review on the use of surrogate comparisons [56]. This study demonstrated that, when compared with equivalent trials that have used true clinical endpoints, surrogates give over-optimistic results as they are more likely to report larger treatment effects. Therefore, the EAC was concerned that this inference may not be sound.
The literature shows that VTE is considered to have three major risk factors for VTE, known as Virchow’s Triad. While the EAC agrees that venous stasis is a risk factor, it does not believe that the literature shows it to be essential for venous thrombosis [55]. Therefore, the efficacy of VTE prevention is not proven on the basis of venous stasis prevention alone. The EAC’s consultation with the nominated experts agreed with this. Therefore, the EAC considers that it is not sufficient to suggest that the geko™ device reduces VTE risk through increasing blood flow alone. To be confident in VTE risk reduction, evidence is needed to demonstrate that geko™ can maintain blood flow at a level that decreases the risk of blood clotting, taking into account all aspects of Virchow’s Triad.
The sponsor compared the effect of geko™ on venous blood flow to that of IPC devices. The inference being made is that if geko™ improves venous flow by the same amount as IPC, it can be assumed that geko™ is as efficacious as IPC in preventing VTE. The sponsor’s evidence centres on the assumption that IPC devices work by increasing venous blood flow, therefore reducing VTE incidence. However, the EAC questioned the validity of this given the conflicting evidence for the relationship between IPC use and VTE prophylaxis. Whilst some studies documented in this report found a reduction in the incidence of VTE with the use of IPC, it was not clear whether this was due to increased venous blood flow or other prophylactic effects. Furthermore, one of the sponsor’s own identified studies found reduced venous blood flow with IPC use; Jawad [36] documents an average percentage change to baseline for venous flow of −4 %.
Although the cost-model structure, along with its assumptions, pathways and health states, is appropriate, the basic assumption that geko™ will reduce the relative risk of DVT is uncertain since there is no direct clinical evidence to support this. The EAC believes that there is now an opportunity to generate new clinical evidence on the impact of geko™ on DVT/VTE incidence to populate an updated economic model.
Overall, it was the EAC’s opinion that there was insufficient clinical evidence to determine the ability of the geko™ device to reduce the risk of VTE. The three main weaknesses in the evidence provided are that that none of the studies were performed using patients rather than healthy volunteers, none were conducted using geko™ for an appropriate time period (days instead of hours), and none used DVT or VTE incidence as the endpoint. Therefore, the EAC recommended that in order to demonstrate the efficacy of the geko™ device, it would be ideal to conduct a carefully designed RCT in patients, with a suitable comparator or inferiority assessment defined by the specific measured outcome.
NICE Guidance
In accordance with the NICE’s MTEP process, draft recommendations for the adoption of the geko™ device were produced based on deliberation by the MTAC, input from expert advisors, and the EAC report. Consultation was conducted among interested parties, and all comments were collated and submitted to the MTAC after a period of time, for further discussion.
Draft Recommendations
In October 2013, the MTAC met and reviewed the sponsor’s submission and EAC report together. Input from expert advisers was also included. Based on this meeting, the MTAC concluded “that the geko™ device showed promise as a means of VTE prophylaxis”; however, it noted the lack of current clinical evidence. Therefore, the MTAC provisionally recommended further research to support a case for routine adoption in the NHS [57].
Consultation Response
Between 13 November and 11 December 2013, public consultation was invited on the published provisional recommendations. During this period, detailed comments (n = 56) were received, including new evidence provided by the sponsor. The new evidence consisted of interim results of two studies using the geko™ device in patient populations [58, 59]. The EAC reviewed this new information to determine whether it added significantly to the evidence provided in the original submission from the sponsor and the additional evidence identified by the EAC. The EAC considered that this new evidence (although interim) was promising as both studies had been conducted in a patient population with an activated geko™ device. The sponsor also provided additional post-market surveillance data [60], mainly related to patient wear time of the geko™ device in a post-surgical population. However, there were significant limitations in both the study methodology (in general and in terms of the scope) and the level of information provided for all three new pieces of evidence, which casts doubt on the reliability and interpretation of these interim study results in their present form. Therefore, the EAC considered that the conclusions that were presented in the original EAC report remained valid and appropriate.
The detailed consultation comments challenged several aspects of the draft guidance. Notably, several expert advisers who had commented earlier in the evaluation subsequently submitted comments which re-contextualised their original advice. Comments sought to clarify areas of uncertainty around the size of the target unmet need population (n = 14 comments), the use of surrogate outcomes (such as venous blood flow) in the assessment of VTE prophylaxis (n = 9 comments), and the magnitude of the effect of the geko™ device on VTE with respect to other mechanical devices (n = 13 comments). The MTEP team, in collaboration with the EAC, prepared draft responses to all comments and presented them to the MTAC for consideration at its January 2014 meeting.
During this meeting, the consultation comments were discussed at length with expert advisers and EAC representatives. The subject of the target population and its size was discussed, as well as the magnitude of the physiological effect of the geko™ device in relation to other mechanical devices and the mechanism of action versus the action of exercise. This led the MTAC to change its original provisional research recommendation to one of positive guidance for the adoption of the geko™ device in a limited specific population of patients where the geko™ device may reduce the high risk of VTE in patients who cannot use other forms of prophylaxis.
Due to this change, a second period of public consultation was invited between 19 February and 19 March 2014. During this period, a further seven comments were received and one additional study abstract was supplied by the sponsor as clinical evidence. Again, the EAC reviewed all new information. The comments did not materially impact on the guidance recommendations and the EAC considered that the abstract did not add significantly to the current evidence base, although the study subjects were patients using the geko™ device [61].
Final Guidance
An MTAC meeting was held on 10 April 2014 to produce final guidance for the geko™ device for reducing the risk of VTE. The MTAC considered the comments arising from the second consultation and decided not to change the recommendations. The final medical technology guidance (MTG19) [10] document for the geko™ device for reducing the risk of VTE was published by the NICE in June 2014.
The final MTAC guidance for the geko™ device included the following recommendations [57]:
The case for adopting the geko™ device is supported for use in people who have a high risk of VTE and for whom other mechanical and pharmacological methods of prophylaxis are impractical or contraindicated. Although clinical evidence is limited, the case is supported because of the plausibility that the geko™ device may reduce the high risk of VTE in patients who cannot use other forms of prophylaxis, and the low risk of the device causing harm.
In patients at high risk of VTE who would otherwise receive no prophylaxis, using the geko™ device is estimated to be cost-saving. The amount saved depends on the level of reduction in relative risk of DVT associated with geko™ treatment compared with no treatment. There is no direct evidence on the size of this reduction, but when values obtained with other mechanical methods of prophylaxis were used in cost modeling, the estimated cost-saving for the geko™ device in patients at high risk of VTE compared with no prophylaxis was £197 per patient.
Challenges
The EAC encountered several challenges when reviewing the clinical evidence for the geko™ device. One of the main challenges was the absence of direct clinical evidence for the efficacy of the geko™ device. The EAC noted that the use of blood flow as a surrogate measure of VTE prevention can lead to over-optimistic results, resulting in larger treatment effects, and does not account for any effects on other aspects of Virchow’s Triad. Furthermore, all of the studies originally submitted as clinical evidence were conducted among healthy volunteers, measured few of the outcomes specified in the scope, and assessed the geko™ device in such a way as to make comparability between studies impractical (i.e. it was not possible to perform meta-analysis). A further challenge was the inclusion of clinical evidence using NMES/MEST and IPC studies as these studies were not considered by the EAC to provide substantial evidence related to the geko™ device.
A further challenge faced by this and many other medical technology evaluations was balancing expert advice against the quality of existing clinical evidence. Accepted clinical wisdom, which is taken at face value by expert advisers, may, in reality, lack high-quality and robust evidence. This was the case with the geko™ device and the use of surrogate outcomes, such as venous blood flow for VTE prophylaxis. A fully powered trial as suggested by several experts would require considerable numbers; the EAC provided a provisional design for an RCT to compare geko™ with a control in patients for whom no other treatment was possible. The RCT proposed was a two-arm, randomised controlled superiority trial of geko™ versus control in patients in whom no other known effective treatment was indicated. Using DVT as the primary outcome, this trial would require 560 patients in total (n = 280 per arm) using a two-sided design, 5 % significance level and 80 % power.
Conclusions
The assessment of medical technology is demanding due to limitations in both the quality and quantity of the evidence-base available. However, the EAC recognises that it is important to provide medical options for patients who are not able to use any other form of device or medication to reduce DVT risk, and in this context the geko™ device may provide a solution.
Acknowledgments
Janet Peacock was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. The authors thank Linda Bonner and Arya Roopen from King’s College Hospital NHS Foundation Trust for their advice on the clinical evidence and for their contribution to the original EAC report for the NICE.
Disclosures
KiTEC is funded by the NICE to act as an EAC for the MTEP. This summary of the medical technologies guidance was produced following publication of the final guidance report. The summary has been reviewed by the NICE but has not been externally peer reviewed by Applied Health Economics and Health Policy. Two of the authors (Cornelius Lewis and Stephen Keevil) are employees of the NHS; the NHS has a financial interest in the guidance issued by the NICE as a result of this work. Paul Dimmock is an employee of the NICE and he had no role in the preparation of the EAC report.
Author contributions
The clinical effectiveness section of this paper was written by Jennifer Summers, James Clinch and Janet Peacock. The economic section and other sections were written by Muralikrishnan Radhakrishnan, Andy Healy and Tiago Rua. Viktoria McMillan, Elizabeth Morris, Mercy Ofuya, Yanzhong Wang, Cornelius Lewis, Stephen Keevil and Paul Dimmock contributed to the preparation of the review. Cornelius Lewis and Stephen Keevil are guarantors for the overall content.
Appendix 1: Two-level deep vein thrombosis and pulmonary embolism Wells score [24]a
| DVT—clinical feature | Points | PE—clinical feature | Points |
|---|---|---|---|
| Active cancer (treatment ongoing, within 6 months, or palliative) | 1 | Clinical signs and symptoms of DVT (minimum of leg swelling and pain with palpation of the deep veins) | 3 |
| Paralysis, paresis or recent plaster immobilisation of the lower extremities | 1 | An alternative diagnosis is less likely than PE | 3 |
| Recently bedridden for 3 days or more, or major surgery within 12 weeks requiring general or regional anaesthesia | 1 | Heart rate >100 beats per minute | 1.5 |
| Localised tenderness along the distribution of the deep venous system | 1 | Immobilisation for more than 3 days, or surgery in the previous 4 weeks | 1.5 |
| Entire leg swollen | 1 | Previous DVT/PE | 1.5 |
| Calf swelling 3 cm larger than asymptomatic side | 1 | Haemoptysis | 1 |
| Pitting oedema confined to the symptomatic leg | 1 | Malignancy (on treatment, treated in the last 6 months, or palliative) | 1 |
| Collateral superficial veins (non-varicose) | 1 | ||
| Previously documented DVT | 1 | ||
| An alternative diagnosis is at least as likely as DVT | −2 | ||
| Clinical probability simplified score | Clinical probability simplified score | ||
| DVT likely | ≥2 | PE likely | >4 |
| DVT unlikely | ≤1 | PE unlikely | ≤4 |
Appendix 2: Overview of sponsor-included clinical evidence
| Reference | Technology/intervention | Comparator |
|---|---|---|
| Tucker et al. [38] | geko™ | Contralateral leg |
| Jawad (cardiac) [39] | geko™ | No mechanical device at baseline measure |
| Jawad (coagulation) [35] | geko™ | No mechanical device |
| Williams et al. [40] | geko™ | Baseline measure and IPC |
| Jawad et al. (vs. IPC) [36] | geko™ | Baseline measure and IPC |
| Warwick et al. [63] | geko™ | Plaster cast |
| Williams et al. (unpublished) [37] | geko™ | Baseline measure and IPC |
| Corley et al. [64] | NMES | No mechanical device |
| Czyrny et al. [65] | NMES | IPC |
| Faghri et al. [66] | NMES | IPC |
| Lindstrom et al. [45] | NMES | Pharmacological prophylaxis or no mechanical device |
| Rosenberg et al. [50] | NMES | Pharmacological prophylaxis or no mechanical device |
| Velmahos et al. [47] | NMES | No mechanical device |
| Broderick et al. [67] | NMES | No mechanical device in contralateral leg |
| Broderick et al. [68] | NMES | Contralateral leg |
| Browse and Negus [49] | NMES | No mechanical device in contralateral leg |
| Griffin et al. [69] | NMES | No mechanical device at baseline measure |
| Izumi et al. [70] | NMES | IPC, electrical muscle stimulation, and patient’s movements in a variety of positions |
| Kaplan et al. [71] | NMES | No mechanical device in contralateral leg |
| Nicolaides et al. [46] | NMES | No mechanical device |
| Nicolaides et al. [72] | IPC and NMES | Pharmacological prophylaxis |
| Pitto and Young [77] | IPC | Pharmacological prophylaxis |
| Santori et al. [73] | FID | Pharmacological prophylaxis |
| Sobieraj-Teague et al. [74] | IPC | Standard VTE prophylaxis care |
| Warwick et al. [75] | FID | Pharmacological prophylaxis |
| Kurtoglu et al. [76] | IPC | No mechanical device |
| Pitto and Young [77] | IPC | Stockings and no mechanical device |
FID foot impulse device, IPC intermittent pneumatic compression, NMES neuromuscular electrical stimulation, VTE venous thromboembolism
Appendix 3: Model assumptions for clinical parameters
| Assumption | Justification |
|---|---|
| Underlying risk of DVT is 29.1 % with no prophylaxis. Note: underlying risk of all other medical patients (23.8 %) was tested in a sensitivity analysis | Based on the average risk of DVT for all surgical-related patients as per the NICE VTE clinical guidelines [10]. Risk of DVT for general medical patients as per the NICE VTE clinical guidelines [10] |
| The proportion of DVT progressing to a PE is assumed to be 10.5 % | The NICE VTE clinical guidelines report the incidence of symptomatic PE at 3.1 % [10]. Assuming that PEs occur as a result of a DVT and the underlying risk of a DVT is 29.1 %, the proportion of DVTs that must progress to a PE can be approximated to 10.5 % |
| There is a 6 % chance of death resulting from a PE. No other mortality is considered | PE fatality rate based on general surgery patients from the NICE VTE clinical guidelines [10]. This is considered conservative as the fatality rate reported is as high as 44.7 % for the general medical cohort |
| RR of a DVT for the geko™ device is 0.39 | Risk for NMES reported by Browse and Negus [49]. This RR is within the ranges reported for IPC in the NICE VTE clinical guidelines (0.31 for TKR up to 0.58 for hip-fracture surgery) and more conservative than that reported for NMES by Nicolaides et al. [78] |
| PTS occurs in 25 % of patients with symptomatic DVT, 15 % of patients with asymptomatic DVT, and 25 % of patients with a PE | Based on assumptions made within the NICE VTE clinical guidelines [10] |
DVT deep vein thrombosis, IPC intermittent pneumatic compression, NICE National Institute for Health and Care Excellence, NMES neuromuscular electrical stimulation, PE pulmonary embolism, PTS post-thrombotic syndrome, VTE venous thromboembolism
Appendix 4: Abbreviations
- CE
Conformité Européenne
- CG92
NICE clinical guidance 92
- CT
Computed tomography
- DVT
Deep vein thrombosis
- EAC
External assessment centre
- FID
Foot impulse device
- ICD
International classification of disease
- IPC
Intermittent pneumatic compression
- KiTEC
King’s Technology Evaluation Centre
- MEST
Muscular electrical stimulation
- MTAC
Medical Technologies Advisory Committee
- MTEP
Medical Technologies Evaluation Programme
- MTG19
NICE Medical Technology Guidance 19
- NHS
National Health Service
- NHS EED
National Health Service Economic Evaluation Database
- NICE
National Institute for Health and Care Excellence
- NIHR
National Institute for Health Research
- NMES
Neuromuscular Electrical Stimulation
- PE
Pulmonary embolism
- PSSRU
Personal Social Services Research Unit
- PTS
Post-Thrombotic Syndrome
- RCT
Randomised Controlled Trial
- UFH
Unfractionated heparin
- UK
United Kingdom
- VTE
Venous thromboembolism
References
- 1.National Institute for Health and Care Excellence. 2014. Available from: http://www.nice.org.uk/about. Accessed June 2014.
- 2.National Institute for Health and Care Excellence. NICE medical technologies evaluation programme (MTEP). 2014. Available from: http://www.nice.org.uk/About/What-we-do/Our-Programmes/NICE-guidance/NICE-medical-technologies-evaluation-programme. Accessed June 2014.
- 3.National Institute for Health and Care Excellence. Medical technologies evaluation programme: process guide. 2011. Available from: http://www.nice.org.uk/Media/Default/About/what-we-do/NICE-guidance/NICE-medical-technologies/Medical-technologies-evaluation-programme-methods-guide.pdf. Accessed July 2014. [PubMed]
- 4.National Institute for Health and Care Excellence. Medical technologies evaluation programme. NICE medical technologies guidance [MTG19]. The geko device for reducing the risk of venous thromboembolism. 2014. Available from: https://www.nice.org.uk/guidance/MTG19/chapter/1-recommendations. Accessed June 2014.
- 5.Radhakrishnan M, et al. E-vita open plus for treating complex aneurysms and dissections of the thoracic aorta: a NICE medical technology guidance. Appl Health Econ Health Policy. 2014;12(5):485–95. [DOI] [PMC free article] [PubMed]
- 6.Willits I, et al. WatchBP Home A for opportunistically detecting atrial fibrillation during diagnosis and monitoring of hypertension: a NICE medical technology guidance. Appl Health Econ Health Policy. 2014;12(3):255–265. doi: 10.1007/s40258-014-0096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Withers K, Carolan-Rees G, Dale M. Pipeline™ embolization device for the treatment of complex intracranial aneurysms: a NICE medical technology guidance. Appl Health Econ Health Policy. 2013;11(1):5–13. doi: 10.1007/s40258-012-0005-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.White J, Carolan-Rees G. PleurX peritoneal catheter drainage system for vacuum-assisted drainage of treatment-resistant, recurrent malignant ascites: a NICE medical technology guidance. Appl Health Econ Health Policy. 2012;10(5):299–308. doi: 10.1007/BF03261864. [DOI] [PubMed] [Google Scholar]
- 9.Campbell B, Campbell M. NICE medical technologies guidance: a novel and rigorous methodology to address a new health technology assessment challenge. Appl Health Econ Health Policy. 2012;10(5):295–297. doi: 10.1007/BF03261863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Institute for Health and Care Excellence. NICE guidelines [CG92]. Venous thromboembolism: reducing the risk: reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to hospital. 2010. Available from: http://www.nice.org.uk/Guidance/CG92. Accessed July 2014.
- 11.National Health Service. Blood clots. 2013. Available from: http://www.nhs.uk/Conditions/Thrombosis/Pages/Introduction.aspx. Accessed July 2014.
- 12.House of Commons Health Committee. HC99: the prevention of venous thromboembolism in hospitalised patients. London: The Stationery Office Limited; 2005.
- 13.Office for National Statistics. Deaths in England and Wales due to deep vein thrombosis and pulmonary embolism, 2006–10. 2012. http://www.ons.gov.uk/ons/.
- 14.Kopcke D, et al. Mortality from pulmonary embolism is decreasing in hospital patients. J Soc Med. 2011;104(8):327–331. doi: 10.1258/jrsm.2011.100395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Torbicki A, et al. Guidelines on the dianosis and management of acute pulmonary embolism. Eur Heart J. 2008;29(18):2276–2315. doi: 10.1093/eurheartj/ehn310. [DOI] [PubMed] [Google Scholar]
- 16.Royal College of Nursing. Understanding VTE. 2014. Available from: http://www.rcn.org.uk/development/practice/cpd_online_learning/nice_care_preventing_venousthromboembolism/understanding_vte. Accessed July 2014.
- 17.Kahn S. How I treat postthrombotic syndrome. Blood. 2009;114(21):4624–31. [DOI] [PubMed]
- 18.Vazquez S, Kahn S. Postthrombotic Syndrome. Circulation. 2010;121:a217–a219. doi: 10.1161/CIRCULATIONAHA.109.925651. [DOI] [PubMed] [Google Scholar]
- 19.Makin A, Silverman SH, Lip GYH. Peripheral vascualr disease and Virchow’s triad for thrombogenesis. QJM. 2002;95(4):199–210. doi: 10.1093/qjmed/95.4.199. [DOI] [PubMed] [Google Scholar]
- 20.Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107:I-9–16. [DOI] [PubMed]
- 21.National Institute for Health and Care Excellence. Pulmonary embolism. 2013. Available from: http://cks.nice.org.uk/pulmonary-embolism-!backgroundsub:4. Accessed June 2014.
- 22.Department of Health. Risk assessment for venous thromboembolism (VTE). 2010. Available from: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digitalasset/dh_113355.pdf. Accessed June 2014.
- 23.National Institute for Health and Care Excellence. NICE pathways: venous thromboembolism overview. 2014. Available from: http://pathways.nice.org.uk/pathways/venous-thromboembolism. Accessed June 2014.
- 24.National Institute for Health and Care Excellence. NICE pathways: diagnosing venous thromboembolism in primary, secondary and tertiary care. 2014. Available from: http://pathways.nice.org.uk/pathways/venous-thromboembolism/diagnosing-venous-thromboembolism-in-primary-secondary-and-tertiary-care-content=view-node%3Anodes-patient-with-signs-or-symptoms-of-pulmonary-embolism-pe-such-as-chest-pain-shortness-of-breath-or-haemoptysis. Accessed June 2014.
- 25.Wells PS, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003;349:1227–1235. doi: 10.1056/NEJMoa023153. [DOI] [PubMed] [Google Scholar]
- 26.National Health Service. Deep vein thrombosis: diagnosis. 2014. Available from: http://www.nhs.uk/Conditions/Deep-vein-thrombosis/Pages/Diagnosis.aspx. Accessed June 2014.
- 27.Qaseem A, et al. Current diagnosis of venous thromboembolism in primary care: a clinical roactise guideline from the American Academy of family physicians and the American College of Physicians. Ann Fam Med. 2007;5(1):57–62. doi: 10.1370/afm.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Health Service. Deep vein thrombosis: treatment. 2014. Available from: http://www.nhs.uk/Conditions/Deep-vein-thrombosis/Pages/Treatment.aspx. Accessed July 2014.
- 29.FirstKind Ltd. Neuromuscular electrostimulation geko™ T-1: specifications. 2013. Available from: http://www.gekodevices.com/enuk/technology/specifications/neuromuscular-electrostimulation-geko™-t-1/. Accessed June 2014.
- 30.FirstKind Ltd. DVT prevention geko device designed to increase venous circulation for VT prophylaxis: what it does and how it works. 2013. Available from: http://www.gekodevices.com/en-uk/technology/what-it-does-and-how-it-works.aspx. Accessed June 2014.
- 31.National Institute for Health and Care Excellence. Medical technology guidance MT196—scope. The geko device for venous thromboembolism prophylaxis. 2013. Available from: http://www.nice.org.uk/guidance/mtg19/resources/the-geko-device-for-venous-thromboembolism-prophylaxis-scope2. Accessed June 2014.
- 32.FirstKind Ltd. Sponsor submission of evidence: the geko™ device for venous thromboembolism (VTE) prophylaxis. In: National Institute for Health and Care Excellence, editor. Medical Technologies Evaluation Programme (MTEP). London; 2013.
- 33.FirstKind Ltd. geko ciruclation support: insturctions for use. 2013. Available from: http://www.gekodevices.com/media/34381/fk-geko_ifu_1a-r4_a4-v1.pdf. Accessed June 2014.
- 34.Jawad H. The effect of a novel electrical stimulation method for improving lower limb blood flow in healthy volunteers. London: Queen Mary, University of London; 2012.
- 35.Jawad H. Coagulation, in the effect of a novel electrical stimulation method for improving lower limb blood flow in healthy volunteers. London: Queen Mary, University of London; 2012.
- 36.Jawad H. Geko vs IPC, in the effect of a novel electrical stimulation method for improving lower limb blood flow in healthy volunteers. London: Queen Mary, University of London; 2012.
- 37.Williams KJ, et al. Haemodynamic changes with the use of neuromuscular electrical stimulation compared to intermittent pneumatic compression. (Manuscript in preparation). [DOI] [PubMed]
- 38.Tucker A, et al. Augmentation of venous, arterial and microvascular blood supply in the leg by isometric neuromuscular stimulation via the peroneal nerve. Int J Angiol. 2010;19(1):e31–e37. doi: 10.1055/s-0031-1278361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jawad H. Cardiac, in the effect of a novel electrical stimulation method for improving lower limb blood flow in healthy volunteers. London: Queen Mary, University of London; 2012.
- 40.Williams KJ, et al. Intermittent pneumatic compression and neuromuscular electrical stimulation of the leg: venous haemodynamic effects. In: 14th Annual Meeting of the European Venous Forum in collaboration with the Balkan Venous Forum and the Serbia College of Phlebology. 2013.
- 41.Broderick BJ, et al. Hemodynamic performance of NMES in the early post operative period following orthopaedic surgery. In: Annual International Conference of the IEEE Engineering in Medicine and Biology Society-EMBC; 2011. p. 7630–7633. [DOI] [PubMed]
- 42.Broderick BJ, et al. A pilot evaluation of a neuromuscular electrical stimulation (NMES) based methodology for the prevention of venous stasis during bed rest. Med Eng Phys. 2010;32(4):349–355. doi: 10.1016/j.medengphy.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 43.Broderick BJ, et al. Venous emptying from the foot: Influences of weight bearing, toe curls, electrical stimulation, passive compression, and posture. J Appl Physiol. 2010;109(4):1045–1052. doi: 10.1152/japplphysiol.00231.2010. [DOI] [PubMed] [Google Scholar]
- 44.Katz RT, et al. Functional electric stimulation to enhance systemic fibrinolytic activity in spinal cord injury patients. Arch Phys Med Rehabil. 1987;68(7):423–426. [PubMed] [Google Scholar]
- 45.Lindstrom B, et al. Prediction and prophylaxis of postoperative thromboembolism: a comparison between peroperative calf muscle stimulation with groups of impulses and dextran 40. Br J Surg. 1982;69(11):633–637. doi: 10.1002/bjs.1800691102. [DOI] [PubMed] [Google Scholar]
- 46.Nicolaides AN, et al. Optimal electrical stimulus for prevention of deep vein thrombosis. Br Med J. 1972;3(5829):756–758. doi: 10.1136/bmj.3.5829.756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Velmahos GC, et al. Electrostimulation for the prevention of deep venous thrombosis in patients with major trauma: a prospective randomized study. Surgery. 2005;137(5):493–498. doi: 10.1016/j.surg.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 48.Moloney GE, Morrell MT, Fell RH. The effect of electrical stimulation of the legs on postoperative thrombosis. Br J Surg. 1972;59(1):65–68. doi: 10.1002/bjs.1800590118. [DOI] [PubMed] [Google Scholar]
- 49.Browse NL, Negus D. Prevention of postoperative leg vein thrombosis by electrical muscle stimulation: an evaluation with 125I-labelled fibrinogen. BMJ. 1970;3(5723):615–618. doi: 10.1136/bmj.3.5723.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rosenberg IL, Evans M, Pollock AV. Prophylaxis of postoperative leg vein thrombosis by low dose subcutaneous heparin or peroperative calf muscle stimulation: a controlled clinical trial. Br Med J. 1975;1(5959):649–651. doi: 10.1136/bmj.1.5959.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Curtis L. Unit costs of health and social care. 2012. Available from: http://www.pssru.ac.uk/project-pages/unit-costs/2012/. Accessed June 2014.
- 52.Department of Health. NHS reference costs: financial year 2011–2012. 2012. Available from: https://www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012. Accessed June 2014.
- 53.Caprini JA, et al. Economic burden of long-term complications of deep vein thrombosis after total hip replacement surgery in the United States. Value Health. 2003;6(1):59–74. doi: 10.1046/j.1524-4733.2003.00204.x. [DOI] [PubMed] [Google Scholar]
- 54.Dai G, Gertler JP, Kamm RD. The effects of external compression on venous blood flow and tissue deformation in the lower leg. J Biomech Eng. 1999;121:557–564. doi: 10.1115/1.2800853. [DOI] [PubMed] [Google Scholar]
- 55.Morris RJ, Woodcock JP. Evidenced-based compression: prevention of stasis and deep vein thrombosis. Ann Surg. 2004;239(2):62–71. [DOI] [PMC free article] [PubMed]
- 56.Ciani O, et al. Comparison of treatment effect sizes associated with surrogate and final patient relevant outcomes in randomised controlled trials: meta-epidemiological study. BMJ. 2013;346:f457. doi: 10.1136/bmj.f457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.National Institute for Health and Care Excellence. MT196 draft guidance: the geko device for venous thromboembolism prophylaxis: consultation document. 2013. Available from: http://admin.nice.org.uk/guidance/MT/196/Consultation/DraftGuidance. Accessed June 2014.
- 58.Unknown. Study 8.1.1: the geko™ device vs Intermittent Pneumatic Compression (IPC) of the foot following elective Total Hip Replacement (THR). Medical Technologies Evaluation Programme: MT196. The geko device for reducing the risk of venous thromboembolism: consultation comments table for MTCD2 2014. Available from: http://admin.nice.org.uk/nicemedia/live/14166/66628/66628.pdf. Accessed July 2014.
- 59.Unknown. Study 8.1.2: the geko™ device vs TEDS following elective THR. Medical Technologies Evaluation Programme: MT196. The geko device for reducing the risk of venous thromboembolism: Consultation Comments table for MTCD2 2014. Available from: http://admin.nice.org.uk/nicemedia/live/14166/66628/66628.pdf. Accessed July 2014.
- 60.FirstKind Ltd. Geko post market surveillance (PMS). Medical Technologies Evaluation Programme: MT196. The geko device for reducing the risk of venous thromboembolism: consultation comments table for MTCD2 2014. Available from: http://admin.nice.org.uk/nicemedia/live/14166/66628/66628.pdf. Accessed July 2014.
- 61.Barnes R, et al. Haemodynamic efficacy of the GEKO™ electrical euromuscular stimulation device in claudicants. In: Society of Academic and Research Surgery. Cambridge: UK; 2014. [Google Scholar]
- 62.Wells PS, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83(3):416–420. [PubMed] [Google Scholar]
- 63.Warwick D, et al. Neuromuscular electrostimulation via the common peroneal nerve promotes lower limb blood flow in a below knee cast: a potential for thromboprophylaxis. Bone Joint Res. 2013;2(9):179–85. [DOI] [PMC free article] [PubMed]
- 64.Corley GJ, et al. Hemodynamic effects of habituation to a week-long program of neuromuscular electrical stimulation. Med Eng Phys. 2012;34(4):459–465. doi: 10.1016/j.medengphy.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 65.Czyrny JJ, et al. Electrical foot stimulation: a potential new method of deep venous thrombosis prophylaxis. Vascular. 2010;18(1):20–27. doi: 10.2310/6670.2010.00001. [DOI] [PubMed] [Google Scholar]
- 66.Faghri PD, et al. Electrical stimulation-induced contraction to reduce blood stasis during arthroplasty. IEEE Trans Rehabil Eng. 1997;5(1):62–69. doi: 10.1109/86.559350. [DOI] [PubMed] [Google Scholar]
- 67.Broderick B, et al. Haemodynamic performance of neuromuscular electrical stimulation (NMES) during recovery from total hip arthroplasty. J Orthop Surg Res. 2013;8:3. [DOI] [PMC free article] [PubMed]
- 68.Broderick BJ, et al. Patient tolerance of neuromuscular electrical stimulation (NMES) in the presence of orthopaedic implants. Med Eng Phys. 2011;33(1):56–61. doi: 10.1016/j.medengphy.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 69.Griffin M, et al. The efficacy of a new stimulation technology to increase venous flow and prevent venous stasis. Eur J Vasc Endovasc Surg. 2010;40(6):766–771. doi: 10.1016/j.ejvs.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 70.Izumi M, et al. Prevention of venous stasis in the lower limb by transcutaneous electrical nerve stimulation. Eur J Vasc Endovasc Surg. 2010;39(5):642–645. doi: 10.1016/j.ejvs.2009.11.035. [DOI] [PubMed] [Google Scholar]
- 71.Kaplan RE, et al. Electrical foot stimulation and implications for the prevention of venous thromboembolic disease. Thromb Haemost. 2002;88(2):200–204. [PubMed] [Google Scholar]
- 72.Nicolaides AN, Miles C, Hoare M. Intermittent sequential pneumatic compression of the legs and thromboembolism-deterrent stockings in the prevention of postoperative deep venous thrombosis. Surgery. 1983;94(1):21–25. [PubMed] [Google Scholar]
- 73.Santori FS, et al. Prophylaxis against deep-vein thrombosis in total hip replacement. Comparison of heparin and foot impulse pump. J Bone Joint Surg Br. 1994;76(4):579–83. [PubMed]
- 74.Sobieraj-Teague M, et al. Randomized controlled trial of a new portable calf compression device (Venowave) for prevention of venous thrombosis in high-risk neurosurgical patients. J Thromb Haemost. 2012;10(2):229–235. doi: 10.1111/j.1538-7836.2011.04598.x. [DOI] [PubMed] [Google Scholar]
- 75.Warwick D, et al. A randomised comparison of a foot pump and low-molecular-weight heparin in the prevention of deep-vein thrombosis after total knee replacement. J Bone Joint Surg Br. 2002;84(3):344–350. doi: 10.1302/0301-620X.84B3.12372. [DOI] [PubMed] [Google Scholar]
- 76.Kurtoglu M, et al. Intermittent pneumatic compression in the prevention of venous thromboembolism in high-risk trauma and surgical ICU patients. Ulusal Travma Acil Cerrahi Derg. 2005;11(1):38–42. [PubMed]
- 77.Pitto RP, Young S. Foot pumps without graduated compression stockings for prevention of deep-vein thrombosis in total joint replacement: efficacy, safety and patient compliance. A comparative, prospective clinical trial [published erratum appears in Int Orthop. 2008;32(3):337] Int Orthop. 2008;32(3):331–336. doi: 10.1007/s00264-007-0326-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nicolaides AN, et al. Venous stasis and deep-vein thrombosis. Br J Surg. 1972;59(9):713–717. doi: 10.1002/bjs.1800590908. [DOI] [PubMed] [Google Scholar]


