Abstract
Sepsis is a frequently fatal condition characterized by an uncontrolled and harmful host reaction to microbial infection. Despite the prevalence and severity of sepsis, we lack a fundamental grasp of its pathophysiology. Here we report that the cytokine interleukin (IL)-3 potentiates inflammation in sepsis. Using a mouse model of abdominal sepsis, we show that innate response activator (IRA) B cells produce IL-3, which induces myelopoiesis of Ly-6Chigh monocytes and neutrophils, and fuels a cytokine storm. IL-3 deficiency protects mice against sepsis. In humans with sepsis, high plasma IL-3 levels associate with high mortality even after adjusting for prognostic indicators. Altogether, this study deepens our understanding of immune activation, identifies IL-3 as an orchestrator of emergency myelopoiesis, and reveals a new therapeutic target for treating sepsis.
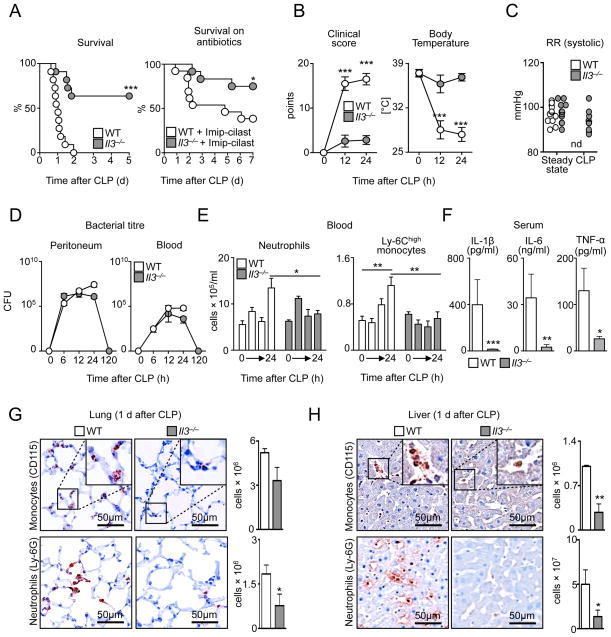
IL-3 contributes to leukocyte production, proliferation, and survival (1–4). Myeloid cells such as monocytes and neutrophils produce IL-1β, IL-6, and tumor necrosis factor (TNF)α, the three inflammatory hallmark cytokines constituting the cytokine storm during septic shock (5–7). Yet despite these links, IL-3’s role in sepsis remains unknown. Il3−/− mice have normal blood monocyte and neutrophil profiles (fig. S1 A–G) (8) and thus do not require IL-3 for myelopoiesis in the steady state. To test whether IL-3 is important in sepsis, we subjected Il3−/− and control wild type (WT) mice to cecal ligation and puncture (CLP), a model of polymicrobial sepsis (9). Compared to WT, Il3−/− mice were protected from sepsis, as seen in lower mortality rates, even after antibiotic treatment (Fig. 1A). Il3−/− mice had better clinical scores, body temperatures (Fig. 1B), and blood pressure (Fig. 1C), and their recovery associated with efficient microbial clearance, indicating that the absence of IL-3 did not compromise bactericidal activity or recognition (Fig. 1D and S2).
Figure 1. IL-3 is detrimental in experimental sepsis.
Comparison of Il3−/− and Balb/c (WT) mice during experimental sepsis using the cecal ligation and puncture (CLP) model. (A) Kaplan-Meier survival curve in mice not receiving antibiotics, days (d) (n = 10/group) and in mice receiving antibiotics (Imipenem) (n = 12–13/group). (B) Clinical score and body temperature (n = 6–10/group). (C) Blood pressure. The blood pressure in WT mice was below detection limit (n = 6–10/group). (D) Bacterial titer of peritoneal cavity and blood (n = 3–10/group). (E) Enumeration of neutrophils and Ly-6Chigh monocytes in 1 ml blood at 0, 6, 12, and 24 h after CLP (n = 3–12/group). (F) Levels of IL-1β, IL-6 and TNF-α in serum 1 day after CLP (n = 8–9/group). (G, H) Immunohistochemical staining and flow cytometric enumeration of monocytes (CD115) and neutrophils (Ly-6G) in entire lung (G) and liver (H) tissue 1 day after CLP (n = 6; *P<0.05, **P<0.01,***P<0.001). Error bars indicate means ± SEM. Significance was assessed by logrank test (A); Mann-Whitney test (B–H). Data are the result of N 2 independent experiments, and are grouped.
To characterize the host response more completely, we performed time-course tissue, cellular, and molecular experiments. At 1 day after CLP, WT mice developed neutrophilia and inflammatory Ly-6Chigh monocytosis (Fig. 1E), whereas in Il3−/− mice monocyte and neutrophil numbers remained relatively unchanged. The increased cell numbers in WT mice associated with higher serum levels of IL-1β, IL-6, and TNFα (Fig. 1F). Phagocytic leukocytes were major sources of IL-1β, IL-6, and TNFα, as phagocyte depletion with clodronate liposomes and anti-Ly-6G prior to CLP abolished the cytokine storm (fig. S3A). However, IL-3-mediated cytokine induction was indirect: both WT and Il3−/− neutrophils and monocytes contained similar intracellular reservoirs of the 3 cytokines (fig. S3B). Analyzing other leukocytes showed IL-3-dependent differences in T and B cell numbers after CLP (fig. S4A), but no differences in basophils, mast cells (10–12) (fig. S4 B, C), or histamine (fig. S4D), which suggests that IL-3 had little to no effect on basophil and mast cell production and function during the initial inflammation-dominant phase. Consequently, WT but not Il3−/− mice accumulated monocytes and neutrophils in the lung (Fig. 1G) and liver (Fig. 1H); developed lung pathology (fig. S5A) with increased protein in bronchoalveolar lavage (fig. S5B); and evolved abnormal liver morphology (fig. S5C) with increased markers of cytolysis in serum (fig. S5D). These data show that IL-3 contributed to septic shock, the most severe form of sepsis (13, 14).
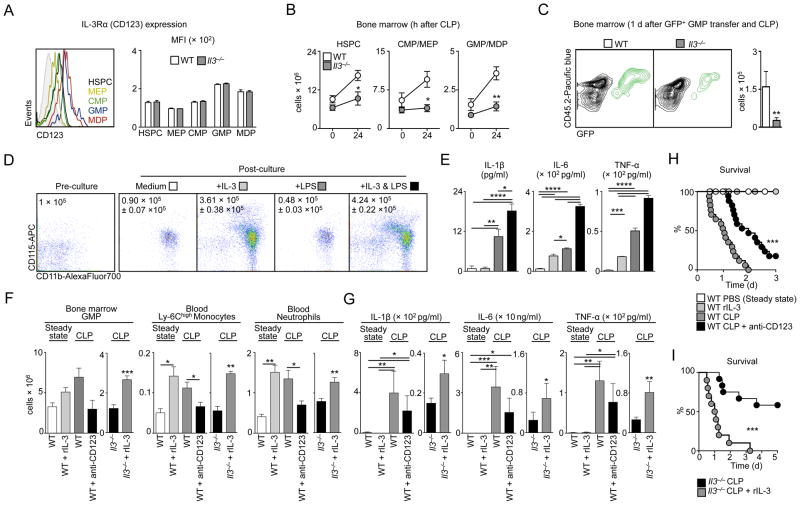
IL-3 promotes hematopoiesis by acting on its receptor, a heterodimer that consists of the IL-3-specific α chain (CD123) and the common β chain (CD131) (4). In the steady state, Lin− c-kit+ hematopoietic stem and progenitor cells (HSPC), including megakaryocyte and erythrocyte progenitors (MEP), common myeloid progenitors (CMP), granulocyte and macrophage progenitors (GMP), and macrophage and dendritic progenitors (MDP), expressed CD123 at the same level in both WT and Il3−/− mice (Fig. 2A and S6). 1 day after CLP, the number of medullary HSPC, CMP, MEP, and GMP/MDP increased over steady state in wild type but not Il3−/− mice (Fig. 2B). GMP are committed to differentiate into monocytes and neutrophils (15). We therefore pursued fate mapping experiments involving adoptively transferring green fluorescent protein positive (GFP+) GMP into WT or Il3−/− mice. In response to CLP, the bone marrow of WT mice contained a larger population of GFP+ cells than the bone marrow of Il3−/− mice, indicating IL-3-dependent progenitor expansion (Fig. 2C). To bolster this observation, we placed Lin− bone marrow cells (containing predominantly HSPC) in vitro in medium either alone or supplemented with IL-3, LPS, or both. We found that IL-3, but not LPS, increased cell expansion and generated myeloid cells well above numbers initially placed into culture (Fig. 2D). Though IL-3 alone modestly affected IL-1β, IL-6, and TNFα production, combined IL-3 and LPS exacerbated the response (Fig. 2E). The data suggest that IL-3 is responsible for the cytokine storm, albeit indirectly, by generating a large pool of cells that, upon recognizing bacterial components, produce cytokines in larger quantities.
Figure 2. IL-3 induces emergency hematopoiesis and potentiates the cytokine storm in sepsis.
(A) Surface expression of IL-3Rα (CD123) on HSPC, MEP, CMP, GMP, and MDP in bone marrow of WT and Il3−/− mice (n = 3/group). A representative plot of n = 3 is shown. (B) Enumeration of HSPC, CMP/MEP and GMP/MDP in bone marrow in steady state and 1 day after CLP in WT and Il3−/− mice (n = 3/group). (C) Analysis and enumeration of GFP+ cells retrieved from the bone marrow 1 d after CLP from WT and Il3−/− mice that received 2 × 105 GFP+ GMP i.v. prior to CLP (n = 3/group). (D) Bone marrow cells were sorted for Lin− cells (i.e., enriched for HSPC). Representative CD11b vs. CD115 flow cytometry plots showing cell phenotype just before placement into culture and 4 d after in vitro culture in the indicated conditions. The numbers inside the plots denote cells plated and retrieved (n=4/group). (E) Supernatant levels of IL-1β, IL-6, and TNFα in the 4 post-culture groups shown in D. Values are the result of technical triplicates from N = 2 experiments. (F) Enumeration of indicated cell types in: (i) WT mice at steady state; (ii) WT mice receiving recombinant (r) IL-3 alone; (iii) WT mice subjected to CLP; (iv) WT mice subjected to CLP and receiving anti-CD123 antibody; (v) Il3−/− mice subjected to CLP; and (vi) Il3−/− mice subjected to CLP and receiving recombinant rIL-3 (n = 4–10). (G) Serum levels of IL-1β, IL-6 and TNFα in the 6 groups shown in F (n = 4–10). (H) Kaplan-Meier survival curves showing the four WT mouse groups (n = 6–17/group). (I) Kaplan-Meier survival curves showing the two Il3−/− mouse groups (n = 10/group). (*P<0.05, **P<0.01, ***P<0.001). Error bars indicate means ± SEM. Significance was assessed by Mann-Whitney test (B, C, F, G); 1-way ANOVA with Tukey’s multiple comparison test (E); Kruskal-Wallis test with Dunn’s multiple comparison test (F, G); and logrank (H, I). Data are the result of N = 2 independent experiments acquired in triplicates (in vitro) and N ≥ 2 independent experiments (in vivo), and are grouped.
To determine if IL-3 can trigger severe sepsis in vivo, whether it can do so alone or in combination with infection, and whether it relies on its specific receptor, we injected: (i) recombinant (r)IL-3 to otherwise healthy WT mice; (ii) anti-CD123 to WT mice subjected to CLP; and (iii) rIL-3 to Il3−/− mice subjected to CLP. rIL-3 augmented GMP in the bone marrow and leukocyte numbers in the blood of healthy WT mice to levels akin to those in WT mice subjected to CLP (Fig. 2F). Despite this increase, rIL-3 per se did not induce a cytokine storm in the absence of infection (Fig. 2G), thus confirming our in vitro observations. Conversely, anti-CD123 attenuated cell number in WT CLP mice (Fig. 2F) and tended to decrease serum cytokines (although the differences were not statistically significant) (Fig. 2G) without depleting HSPC (fig. S7). Il3−/− mice receiving rIL-3 in the context of CLP augmented medullary GMP, circulating neutrophil, and Ly-6Chigh monocyte numbers (Fig. 2F). These increases corresponded to higher cytokine levels in serum (Fig. 2G). Ultimately, WT mice treated with anti-CD123 had a modest but significant improvement in survival (Fig. 2H), whereas Il3−/− mice receiving rIL-3 succumbed to infection and died as often as WT mice (Fig. 2I). These data confirm the effects of IL-3 on cell production and survival and identify the IL-3-CD123 axis as a potential new therapeutic target for sepsis.
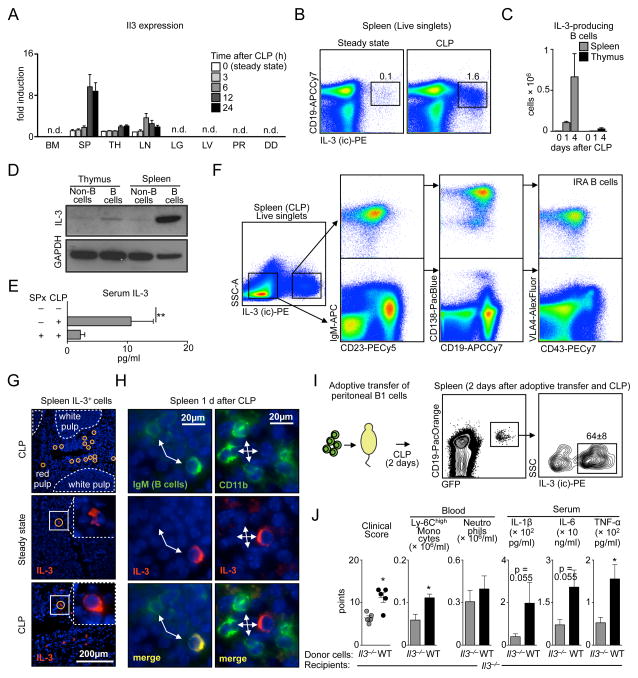
Activated T cells (16) and thymic epithelial cells (17) produce IL-3 in the steady state, but the cytokine’s source in sepsis is unknown. mRNA profiling identified the spleen, thymus, and lymph nodes as hubs of basal Il3 expression. After CLP, Il3 mRNA progressively increased in the spleen, followed by the thymus and lymph nodes, with no signal in the bone marrow, lung, liver, peritoneum, or duodenum (Fig. 3A). By flow cytometry (Fig. 3B, C) and Western blots (Fig. 3D), IL-3+ cells were CD19+ B cells. According to ELISA, IL-3 levels increased in serum after CLP (Fig. 3E) but to a lesser extent in spenectomized mice (Fig. 3E).
Figure 3. IRA B cells are major sources of IL-3 in sepsis.
(A) Il3 mRNA expression in the indicated organs during steady state and 3, 6, 12, and 24 h after CLP (n = 6–8). (B) Identification of IL-3 producing cells in the spleen 4 d after CLP. (C) Enumeration of IL-3-producing B cells in spleen and thymus in steady state and 1 and 4 days after CLP (n = 5). (D) Western blot showing IL-3 expression by B cells and non-B cells sorted from the spleen and thymus 1d after CLP. (E) IL-3 serum levels in steady state and 1 day after CLP with and without splenectomy (SPx) (n = 3–6). (F) Flow cytometric plots show the phenotype of IL-3+ and IL-3− cells retrieved from the spleen after CLP. A representative plot of n = 5 is shown. (G) Immunofluorescence microscopy of spleen tissue in the steady state and 1 day after CLP. (H) Co-staining of representative IL-3+ cells with IgM. (I) Adoptive transfer of 1.5 × 106 peritoneal B1 B cells from GFP+ mice into WT mice subjected to CLP at the time of cell transfer. Representative plots from flow cytometric analysis of n = 3 mice are shown. (J) Adoptive transfer of 3 × 106 peritoneal B1 B cells from WT or Il3−/− mice to the peritoneum of Il3−/− recipients subjected to CLP. Data show the clinical score, number of Ly-6Chigh monocytes, neutrophils, and serum cytokines 1 d after CLP (n = 5). (*P<0.05, **P<0.01). Error bars indicate means ± SEM. Significance was assessed by Kruskal-Wallis test with Dunn’s multiple comparison test (E); and Mann-Whitney test (J).
Identifying B cells as sources of IL-3 prompted testing whether IL-3-producing B cells resemble IRA B cells (fig. S8A), whose GM-CSF product protects against sepsis and pneumonia via polyreactive IgM (18, 19). Phenotypic profiling showed that splenic IL-3 producers were IgMhigh CD23low CD19+ CD138high CD43+ VLA4+ (Fig. 3F and fig. S8B), as well as CD5int LFA1+ CD284+ CD11blow/− (fig. S8C). This phenotype matches that of IRA B cells (18–20). The remaining, non-B IL-3-positive cells in spleen and thymus were CD4+ T cells, CD8+ T cells, and non-T, non-B cells (fig. S8D).
By comparing IL-3 and GM-CSF, which are two IRA B cell products, we determined that the growth factors are not interdependent: in response to CLP, the spleens of Csf2−/− mice accumulated IL-3-producing IRA B cells whereas Il3−/− mice accumulated GM-CSF-producing IRA B cells (fig. S9A). On the one hand, in contrast to GM-CSF (19), IL-3 was not essential to IgM production (fig. S9B, C). On the other hand, unlike IL-3, GM-CSF was dispensable to emergency myelopoiesis (fig. S9D, E). The IL-3-producing IRA B cells were readily visualized by immunofluorescence and increased in frequency after CLP (Fig. 3G, H and fig. S10). Thus, IRA B cells can both protect against and aggravate sepsis, depending on the particular growth factor they produce.
Peritoneal B1 cells relocate to the spleen after peritoneal LPS challenge (21) and differentiate to IRA B cells (18). To determine if IL-3+ B cells arise similarly, we transferred B1 cells from the peritoneum of naive GFP+ mice into the peritoneum of WT mice. Two days after peritoneal LPS challenge, IL-3+ (Fig. 3I) and GM-CSF+ B cells (fig. S11) accumulated in the spleen, indicating peritoneal B cell relocation, splenic accumulation, and IRA B cell differentiation. To test whether IL-3-producing B cells are important in sepsis, we transferred peritoneal B1 B cells from WT or Il3−/− mice into Il3−/− mice subjected to CLP and found increased monocyte levels, cytokine levels, and morbidity in WT B cell recipients (Fig. 3J). Overall, the data show that IL-3-producing IRA B cells induce emergency myelopoiesis and potentiate septic shock in a mouse sepsis model.
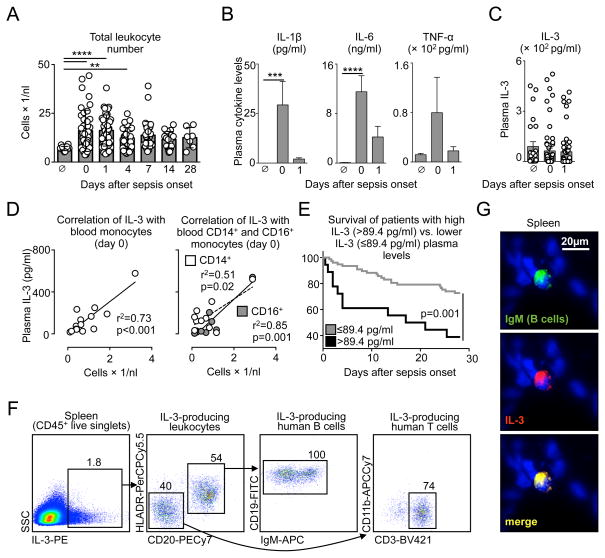
Because the validity of mouse sepsis models as mirrors of human disease has been challenged (22, 23), we sought to determine whether our experimental findings correlate with the pathogenesis of human sepsis. First, we retrospectively analyzed plasma from a cohort of septic patients (RAMMSES cohort, n=60 (Table S1)) (24) and found that IL-3 levels during the first 24 h after onset of sepsis predicted death: patients with IL-3 plasma levels >87.4 pg/ml at admission had a poor prognosis (fig. S12A, B and Table S2). We therefore decided to test, in a new prospective cohort (SEPIL-3 cohort, n=37 (Table S3)), whether IL-3 and blood monocytes correlate. In septic patients monitored over 28 d, blood leukocyte numbers peaked at onset of sepsis and decreased slowly thereafter (Fig. 4A). The increase associated with a sharp spike of plasma cytokines (Fig. 4B). Compared to healthy volunteers, mean IL-3 in septic patient plasma did not differ (Fig. 4C). Nevertheless, the detectable levels of IL-3 correlated with circulating monocyte levels in septic patients (Fig. 4D). Kaplan-Meier survival analysis showed that patients with plasma levels of >89.4 pg/ml had poor prognosis (fig. S13 and Table S4), thus confirming the RAMMSES cohort. Pooling the cohorts showed the impact of IL-3 on survival to be even more striking (odds ratio: 4.979; CI: 1.680–14.738 and p=0.001 for the Kaplan-Meier survival curve) (Fig. 4E). The association remained significant after adjusting for prognostic parameters in multivariate analyses (Table S5), whereas multivariate logistic regression analyses consistently showed improvement in death prediction when IL-3 was included, as shown by a reduction of the Aikake Information Criterion (AIC) and an increase of the pseudo-R2 (Table S6). We also conducted flow cytometry and immunofluorescence on human spleens from patients undergoing splenectomy. By flow cytometry, we found CD20+ HLADRint CD19high IgMint/high B and CD3+ T cells to be producers of IL-3 (Fig. 4F and fig. S14A). On tissue sections, human spleens contained IL-3-producing CD19+ and IgM+ B cells (Fig. 4G and fig. S14B, C), suggesting that IL-3-producing IRA B cells amplify inflammation in humans as well as mice (fig. S15).
Figure 4. IL-3 is an independent early predictor for outcome in human sepsis.
(A) Total leukocyte number in non-septic people and in septic patients at the time of sepsis onset (0) and 1, 4, 7, 14, and 28 days later. (B) Plasma levels of IL-1β, IL-6, and TNFα in non-septic people and in septic patients at the time of sepsis onset and 1 day later (n=40). (C) IL-3 plasma levels in healthy people and in patients at sepsis onset and 1 day later. (D) Correlation of IL-3 plasma levels with total blood monocytes, and with CD14+ and CD16+ blood monocytes in septic patients with measurable IL-3 plasma levels. (E) Kaplan-Meier analysis showing survival of patients in the RAMMSES and SEPIL-3 studies with IL-3 at >89.4 pg/ml (top quintile, measured within 1 day after sepsis onset) vs. patients with IL-3 ≤ 89.4 pg/ml. (F) Representative flow cytometry plot of n = 2 showing identity of IL-3-producing human splenocytes. (G) Immunofluorescence of human spleen showing IL-3 producing B cells in high magnification (60x). Representative immunofluorescence section of n=6 is shown (*P<0.05, ****P<0.0001). Error bars indicate means ± SEM. Significance was assessed by One-way ANOVA with Tukey’s multiple comparison test (A,C); Pearson correlation test (D); and logrank (E). Data in A–D are from the SEPIL-3 cohort; data in E are pooled from RAMMSES and SEPIL-3 cohorts.
Mortality from sepsis ranges between 30–50% and is rising due to drug-resistant organisms, a growing elderly population, and increased incidence of immunosuppression (25–28). The failures of anti-Toll like receptor 4, recombinant activated protein C, and anti-TNFα therapies in clinical trials necessitate a rethinking of sepsis’ pathophysiology (6, 29–33). Because many early phase inflammatory cytokines operate concurrently and redundantly, identifying upstream triggers may generate therapies with broad downstream benefits. Altogether, the evidence shown here supports the hypothesis that IL-3 mediates experimental and human sepsis, is a major upstream orchestrator of the septic inflammatory phase, and can be harnessed for therapeutic intervention.
Supplementary Material
Acknowledgments
We thank M. Greene for secretarial assistance, Mike Waring and Adam Chicoine for sorting cells, and Kaley Joyes for editing the manuscript. The data presented in this manuscript are tabulated in the main paper and in the supplementary materials. This work was supported by NIH grants 5R01HL095612, R56-AI104695, and the Massachusetts General Hospital Howard M. Goodman Fellowship (F.K.S.). G.F.W. was supported by the German Research Foundation (WE4892/1-2 and 3-1). B.G.C. was supported by Société Française d’Anesthésie-Réanimation (SFAR), Institut Servier, Fondation Groupe Pasteur Mutualité, and Fulbright Scholarships (Monahan Foundation and Harvard French Scholarship Fund). M. Nairz was supported by an Erwin Schrodinger Fellowship of the Austrian Science Fund FWF (J3486-B13).
Footnotes
The authors declare no conflict of interest.
References and Notes
- 1.Yang YC, et al. Human IL-3 (multi-CSF): identification by expression cloning of a novel hematopoietic growth factor related to murine IL-3. Cell. 1986;47:3. doi: 10.1016/0092-8674(86)90360-0. [DOI] [PubMed] [Google Scholar]
- 2.Hapel AJ, Lee JC, Farrar WL, Ihle JN. Establishment of continuous cultures of thy1.2+, Lyt1+, 2-T cells with purified interleukin 3. Cell. 1981;25:179. doi: 10.1016/0092-8674(81)90242-7. [DOI] [PubMed] [Google Scholar]
- 3.Ihle JN, Pepersack L, Rebar L. Regulation of T cell differentiation: in vitro induction of 20 alpha-hydroxysteroid dehydrogenase in splenic lymphocytes from athymic mice by a unique lymphokine. J Immunol. 1981;126:2184. [PubMed] [Google Scholar]
- 4.Williams GT, Smith CA, Spooncer E, Dexter TM, Taylor DR. Haemopoietic colony stimulating factors promote cell survival by suppressing apoptosis. Nature. 1990;343:76. doi: 10.1038/343076a0. [DOI] [PubMed] [Google Scholar]
- 5.Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840. doi: 10.1056/NEJMra1208623. [DOI] [PubMed] [Google Scholar]
- 6.Hotchkiss RS, Monneret G, Payen D. Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol. 2013;13:862. doi: 10.1038/nri3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deutschman CS, Tracey KJ. Sepsis: Current Dogma and New Perspectives. Immunity. 2014;40(4):463. doi: 10.1016/j.immuni.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Materials and methods are available as supplementary materials on Science online.
- 9.Rittirsch D, Huber-Lang MS, Flierl MA, Ward PA. Immunodesign of experimental sepsis by cecal ligation and puncture. Nat Protoc. 2009;4:31. doi: 10.1038/nprot.2008.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jamur MC, Oliver C. Origin, maturation and recruitment of mast cell precursors. Front Biosci (Schol Ed) 2011;3:1390. doi: 10.2741/231. [DOI] [PubMed] [Google Scholar]
- 11.Voehringer D. Basophil modulation by cytokine instruction. Eur J Immunol. 2012;42:2544. doi: 10.1002/eji.201142318. [DOI] [PubMed] [Google Scholar]
- 12.Ronnberg E, et al. Mast cells are activated by Staphylococcus aureus in vitro but do not influence the outcome of intraperitoneal Staphylococcus aureus infection in vivo. Immunology. 2014 doi: 10.1111/imm.12297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet. 2005;365:63. doi: 10.1016/S0140-6736(04)17667-8. [DOI] [PubMed] [Google Scholar]
- 14.Ward PA. New approaches to the study of sepsis. EMBO Mol Med. 2012;4:1234. doi: 10.1002/emmm.201201375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kondo M, et al. Biology of hematopoietic stem cells and progenitors: implications for clinical application. Annu Rev Immunol. 2003;21:759. doi: 10.1146/annurev.immunol.21.120601.141007. [DOI] [PubMed] [Google Scholar]
- 16.Groopman JE, Molina JM, Scadden DT. Hematopoietic growth factors. Biology and clinical applications. N Engl J Med. 1989;321:1449. doi: 10.1056/NEJM198911233212106. [DOI] [PubMed] [Google Scholar]
- 17.Dalloul AH, et al. Human thymic epithelial cells produce interleukin-3. Blood. 1991;77:69. [PubMed] [Google Scholar]
- 18.Rauch PJ, et al. Innate response activator B cells protect against microbial sepsis. Science. 2012;335:597. doi: 10.1126/science.1215173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weber GF, et al. Pleural innate response activator B cells protect against pneumonia via a GM-CSF-IgM axis. J Exp Med. 2014;211:1243. doi: 10.1084/jem.20131471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hilgendorf I, et al. Innate response activator B cells aggravate atherosclerosis by stimulating T helper-1 adaptive immunity. Circulation. 2014;129:1677. doi: 10.1161/CIRCULATIONAHA.113.006381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ha SA, et al. Regulation of B1 cell migration by signals through Toll-like receptors. J Exp Med. 2006;203:2541. doi: 10.1084/jem.20061041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seok J, et al. Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc Natl Acad Sci U S A. 2013;110:3507. doi: 10.1073/pnas.1222878110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Takao K, Miyakawa T. Genomic responses in mouse models greatly mimic human inflammatory diseases. Proc Natl Acad Sci U S A. 2014 doi: 10.1073/pnas.1401965111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brenner T, et al. Methylglyoxal as a new biomarker in patients with septic shock: an observational clinical study. Crit Care. 2014;18:683. doi: 10.1186/s13054-014-0683-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 26.Wood KA, Angus DC. Pharmacoeconomic implications of new therapies in sepsis. Pharmacoeconomics. 2004;22:895. doi: 10.2165/00019053-200422140-00001. [DOI] [PubMed] [Google Scholar]
- 27.Bosmann M, Ward PA. The inflammatory response in sepsis. Trends Immunol. 2013;34:129. doi: 10.1016/j.it.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coopersmith CM, et al. A comparison of critical care research funding and the financial burden of critical illness in the United States. Crit Care Med. 2012;40:1072. doi: 10.1097/CCM.0b013e31823c8d03. [DOI] [PubMed] [Google Scholar]
- 29.Dolgin E. Trial failure prompts soul-searching for critical-care specialists. Nat Med. 2012;18:1000. doi: 10.1038/nm0712-1000. [DOI] [PubMed] [Google Scholar]
- 30.Opal SM, et al. Confirmatory interleukin-1 receptor antagonist trial in severe sepsis: a phase III, randomized, double-blind, placebo-controlled, multicenter trial. The Interleukin-1 Receptor Antagonist Sepsis Investigator Group. Crit Care Med. 1997;25:1115. doi: 10.1097/00003246-199707000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Boomer JS, et al. Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA. 2011;306:2594. doi: 10.1001/jama.2011.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hotchkiss RS, Coopersmith CM, McDunn JE, Ferguson TA. The sepsis seesaw: tilting toward immunosuppression. Nat Med. 2009;15:496. doi: 10.1038/nm0509-496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ward PA. Immunosuppression in sepsis. JAMA. 2011;306:2618. doi: 10.1001/jama.2011.1831. [DOI] [PubMed] [Google Scholar]
- 34.Levy MM, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- 35.Ohmori K, et al. IL-3 induces basophil expansion in vivo by directing granulocyte-monocyte progenitors to differentiate into basophil lineage-restricted progenitors in the bone marrow and by increasing the number of basophil/mast cell progenitors in the spleen. J Immunol. 2009;182:2835. doi: 10.4049/jimmunol.0802870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Colvin GA, et al. Murine marrow cellularity and the concept of stem cell competition: geographic and quantitative determinants in stem cell biology. Leukemia. 2004;18:575. doi: 10.1038/sj.leu.2403268. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.