Abstract
Background
Characteristics and outcomes of patients with heart failure and reduced ejection fraction (HFrEF) receiving care at Veterans Affairs (VA) vs. non-VA hospitals have not been previously reported.
Methods and Results
In the randomized controlled Beta-Blocker Evaluation of Survival Trial (BEST; 1995–1999), of the 2707 (bucindolol=1353; placebo=1354) patients with HFrEF (EF ≤35%), 918 received care at VA hospitals, of which 98% (n=898) were men. Of the 1789 receiving care at non-VA hospitals, 68% (n=1216) were men. Our analyses were restricted to these 2114 male patients. VA patients were older with higher symptom and comorbidity burdens. There was no significant between-group difference in unadjusted primary endpoint of 2-year all-cause mortality (35% VA vs. 32% non-VA; hazard ratio {HR}, 1.09; 95% confidence interval {CI}, 0.94–1.26), which remained unchanged after adjustment for age and race (HR, 1.00; 95% CI, 0.86–1.16) or multivariable-adjustment including cardiovascular morbidities (HR, 0.94; 95% CI, 0.80–1.10). There was no between-group differences in cause-specific mortalities or hospitalizations. Chronic kidney disease, pulmonary edema, left ventricular EF <20% and peripheral arterial disease were significant predictors of mortality for both groups. African America race, New York Heart Association class IV symptoms, atrial fibrillation and right ventricular EF <20% were associated with higher mortality among non-VA hospital patients only; however, these differences from VA patients were not significant.
Conclusions
Patients with HFrEF receiving care at VA hospitals were older and sicker; yet their risk of mortality and hospitalization was similar to those younger and healthier receiving care at non-VA hospitals.
Keywords: VA hospital, non-VA hospital, systolic heart failure, outcome, BEST trial
The Veterans Health Administration (VHA) is the largest integrated health care system in the United States that provides comprehensive care to over 8 million veterans each year. It is estimated that within the VHA system every year about ten thousand patients are hospitalized with a primary discharge diagnosis of heart failure (HF).1 Research sponsored by the VHA and conducted among veterans with HF receiving care at Veterans Affairs (VA) Medical Centers has made a major contribution to the field of evidence-based HF care.2–7 This evidence is often extrapolated to the general HF population. Similarly, evidence derived from the general HF population is often extrapolated to veterans with HF. However, little is known about characteristics and prognostic similarities and differences between HF patients receiving care within and outside the VHA system.
Health care needs of veterans have been suggested to be different from that of non-veterans and in part relates to their life-style in service, combat exposure and extended overseas deployments.8 Veterans are reported to have a higher prevalence of comorbidities and cardiovascular risk factors such as smoking and substance abuse than non-veterans.9, 10 These differences may in part explain differential outcomes between VA and non-VA hospitals. For example, hospitalized veterans with a primary discharge diagnosis of acute myocardial infarction (AMI) have been shown to have a higher comorbidity burden than their Medicare counterparts, and yet have similar mortality.11 Similarly, among hospitalized veterans with a primary discharge diagnosis of HF, African Americans have been found to have better survival that is not fully explained by comorbidity burden or differences in healthcare utilization.12 The Beta-Blocker Evaluation of Survival Trial (BEST), a randomized controlled trial of bucindolol, a beta-adrenergic-receptor blocker, in patients with advanced chronic systolic HF or HF with reduced ejection fraction (HFrEF), enrolled patients from both VA and non-VA institutions and is unique for a comparative study of patients treated for HF in VA versus non-VA hospitals. Therefore, the objective of the current study was to compare baseline characteristics and outcomes of HFrEF patients enrolled in the BEST trial receiving care at VA vs. non-VA hospitals.
Methods
Data Sources and Study Population
Funded by the National Heart, Lung, and Blood Institute (NHLBI) and the Department of Veterans Affairs Cooperative Studies Program, BEST was a randomized controlled trial (RCT) of the beta-blocker bucindolol in HFrEF patients with left ventricular EF ≤35% and New York Heart Association (NYHA) class III (92%) or IV (8%) symptoms.13 It was conducted at 30 VA sites and 60 non-VA sites in the United States and Canada between May 1995 and December 1998, and 2708 patients were randomly assigned to either bucindolol (n=1354) or placebo (n=1354) and followed up for the primary endpoint of all-cause mortality.13, 14 The trial was terminated on July 29, 1999 by the data and safety monitoring board citing the “totality of evidence regarding the usefulness of beta-blocker treatment derived from BEST and other studies.”13 The BEST protocol was approved by the institutional review board of each participating site and the current analysis was approved by institutional review board of the University of Alabama at Birmingham.
At that time, the mean duration of follow-up was 2 years and during that period, all-cause mortality occurred in 33% and 30% of patients in the placebo and bucindolol groups, respectively (hazard ratio {HR}, 0.90; 95% confidence interval {CI}, 0.78–1.02; p=0.10). However, there was a significant reduction in the risk of the secondary endpoint of cardiovascular death in the bucindolol group (HR, 0.86; 95% CI, 0.74–0.99). Further, there was a significant reduction in the risk of the primary endpoint of all-cause death in the bucindolol group among Caucasian patients (HR, 0.86; 95% CI, 0.74–0.99), but not among African Americans (HR, 1.17; 95% CI, 0.89–1.53).13
For the purpose of the current analysis, we used a public-use version of the BEST data obtained from the NHLBI that included data on 2707 participants.15–19 One patient declined to be part of the completely de-identified public-use version of the data. Of the 2707 BEST participants, 918 were recruited from VA hospitals, of which 898 (98%) were men. Of the 1789 patients receiving care in non-VA hospitals, 1216 (68%) were men. We restricted our analysis to 2114 (898 + 1216) male participants.
Outcomes
The primary outcome of the current analysis was all-cause mortality, which was also the primary endpoint of the BEST trial. Secondary outcomes included cardiovascular, HF and AMI deaths, sudden cardiac death, and hospitalizations due to all causes and worsening HF.
Statistical Analysis
Baseline characteristics between the two groups were compared using Chi square and student t-test. Cox proportional hazard models were used to compare outcomes among patients in VA versus non-VA hospitals. After unadjusted and age-race-adjusted associations were examined, we constructed a multivariable-adjusted model, additionally adjusting for body mass index, smoking, HF duration, coronary artery disease, diabetes, hypertension, atrial fibrillation, peripheral vascular disease, chronic kidney disease, randomization to bucindolol, use of ACE inhibitors or angiotensin-receptor blockers, digoxin, and diuretics, NYHA class symptoms, left and right ventricular EF, cardiothoracic ratio, pulmonary edema, heart rate, systolic and diastolic blood pressure, hemoglobin, serum creatinine and serum cholesterol. We repeated the last step (multivariable-adjusted) for the secondary outcomes except for AMI for which only age and race were used as covariates due to the small number of events.
We then separately examined predictors of death among patients receiving care at VA vs. non-VA hospitals using a multivariable Cox regression model in which age, sex, race, NYHA class, coronary artery disease, diabetes, hypertension, atrial fibrillation, peripheral vascular disease, chronic kidney disease, randomization to bucindolol, pulmonary edema, and left and right ventricular EF were used as covariates. Finally, we examined the VA vs. non-VA differences in the primary outcome by randomization groups (bucindolol vs. placebo) and by racial groups (Caucasians vs. African Americans). Data analyses were performed using IBM SPSS for Windows, Rel. 22. (IBM Corp. Released 2013. Armonk, NY). The level of significance was set at <0.05, two sided 95% confidence interval levels.
Results
Baseline Characteristics
Patients had a mean age of 61 years and 21% were African Americans. The average age of the patients receiving care in the VA hospitals was 4 years older than that of patients receiving care at non-VA hospitals and there were more African Americans among the patients treated in a VA hospital (Table 1). Patients in the VA hospitals were also more likely to be smokers, have a higher prevalence of coronary artery disease, peripheral arterial disease, hypertension and diabetes, and jugular venous distension (Table 1). They also had a higher prevalence of regional wall motion abnormalities but similar left ventricular EF (Table 1). The median (interquartile range) duration of HF for patients receiving care at VA vs. non-VA hospitals was 40 (15–76) and 35 (12–70) months, respectively.
Table 1.
Baseline patient characteristics of BEST participants with advanced chronic systolic heart failure receiving care at the Veterans Affairs (VA) vs. non-VA hospitals
| N (%) or mean (±SD) | Non-VA hospitals (n=1,216) |
VA hospitals (n=898) |
p value | |
|---|---|---|---|---|
| Age, years | 59 (±13) | 63 (±11) | <0.001 | |
| African American | 241 (20) | 206 (23) | 0.085 | |
| Current smoker | 205 (17) | 201 (22) | 0.002 | |
| New York Heart Association class III | 1127 (93) | 805 (90) | 0.014 | |
| Clinical findings | ||||
| Body mass index, kg/m2 | 37 (±8) | 37 (±8) | 0.895 | |
| Heart rate, beats per minute | 81 (±13) | 81 (±13) | 0.487 | |
| Systolic blood pressure, mm Hg | 116 (±18) | 119 (±18) | <0.001 | |
| Diastolic blood pressure, mm Hg | 71 (±11) | 72 (±11) | 0.162 | |
| Jugular venous distension | 499 (41) | 488 (54) | <0.001 | |
| S3 gallop | 592 (49) | 298 (33) | <0.001 | |
| S4 gallop | 229 (19) | 149 (17) | 0.184 | |
| Pulmonary râles | 134 (11) | 167 (19) | <0.001 | |
| Hepatomegaly | 117 (10) | 145 (16) | <0.001 | |
| Lower extremity edema | 276 (49) | 290 (51) | <0.001 | |
| Past medical history | ||||
| Coronary artery disease | 722 (59) | 637 (71) | <0.001 | |
| ST segment elevation myocardial infarction | 388 (32) | 383 (43) | <0.001 | |
| Angina pectoris | 611 (50) | 538 (60) | <0.001 | |
| Hypertension | 657 (54) | 598 (67) | <0.001 | |
| Diabetes mellitus | 394 (32) | 356 (40) | 0.001 | |
| Chronic kidney disease | 439 (36) | 334 (37) | 0.616 | |
| Atrial fibrillation or flutter | 308 (25) | 263 (29) | 0.047 | |
| Hyperlipidemia | 505 (42) | 419 (47) | 0.021 | |
| Peripheral vascular disease | 168 (14) | 187 (21) | <0.001 | |
| Ventricular fibrillation | 116 (10) | 99 (11) | 0.275 | |
| Thromboembolic disease | 197 (16) | 166 (19) | 0.180 | |
| Valvular replacement | 53 (4) | 32 (4) | 0.373 | |
| Pacemaker | 124 (10) | 72 (8) | 0.095 | |
| Ablation | 25 (2) | 9 (1) | 0.079 | |
| Implanted cardioverter defibrillator | 52 (4) | 23 (3) | 0.043 | |
| Medications | ||||
| Bucindolol (by randomization) | 624 (51) | 444 (49) | 0.403 | |
| Angiotensin-converting enzyme inhibitor | 1171 (96) | 862 (96) | 0.732 | |
| Digitalis | 1137 (94) | 809 (90) | 0.004 | |
| Diuretics | 1126 (93) | 836 (93) | 0.671 | |
| Vasodilators | 519 (43) | 413 (46) | 0.132 | |
| Anticoagulants | 731 (60) | 539 (60) | 1.000 | |
| Laboratory values | ||||
| Hemoglobin, g/dL | 14 (±2) | 14 (±2) | 0.010 | |
| White blood cell count, 103/µL | 8 (±2) | 7 (±2) | 0.532 | |
| Platelet count, 103/µL | 214 (±72) | 215 (±64) | 0.653 | |
| Sodium, mEq/L | 138.7 (±3) | 139.4 (±3) | <0.001 | |
| Potassium, mEq/L | 4.34 (±0.46) | 4.33 (±0.51) | 0.818 | |
| Glucose, mg/dL | 132 (±77) | 136 (±70) | 0.130 | |
| Blood urea nitrogen, mg/dL | 26 (±16) | 25 (±15) | 0.110 | |
| Creatinine, mg/dL | 1.29 (±0.39) | 1.31 (±0.41) | 0.138 | |
| Magnesium, mEq/L | 1.76 (±0.23) | 1.74 (±0.25) | 0.018 | |
| Uric acid, mg/dL | 8 (±2) | 8 (±2) | 0.606 | |
| Bilirubin, mg/dL | 0.88 (±0.46) | 0.87 (±0.50) | 0.810 | |
| Alanine aminotransferase, IU/L | 27 (±16) | 27 (±16) | 0.686 | |
| Aspartate aminotransferase, IU/L | 28 (±21) | 27 (±21) | 0.235 | |
| Alkaline phosphatase, IU/L | 99 (±50) | 97 (±49) | 0.269 | |
| Protein, g/dL | 7.33 (±0.59) | 7.27 (±0.62) | 0.013 | |
| Albumin, g/dl | 4.14 (±0.40) | 4.03 (±0.45) | <0.001 | |
| Cholesterol, mg/dL | 192 (±45) | 191 (±51) | 0.456 | |
| Triglyceride, mg/dl | 212 (±194) | 206 (±314) | 0.593 | |
| International normalization ratio (INR) | 1.68 (±0.95) | 1.57 (±0.83) | 0.002 | |
| Partial thromboplastin time (PTT) | 32 (±8) | 31 (±11) | 0.022 | |
| Plasma norepinephrine, pg/mL | 534 (±311) | 508 (±317) | 0.067 | |
| Chest x-ray findings | ||||
| Pulmonary edema | 128 (11) | 125 (14) | 0.021 | |
| Cardiothoracic ratio | 55 (7) | 55 (7) | 0.836 | |
| Electrocardiographic findings | ||||
| Left ventricular hypertrophy | 271 (22) | 175 (20) | 0.119 | |
| Right ventricular hypertrophy | 11 (1) | 12 (1) | 0.344 | |
| Right bundle brunch block | 80 (7) | 73 (8) | 0.175 | |
| Atrial fibrillation | 144 (12) | 130 (15) | 0.084 | |
| Left bundle brunch block | 294 (20) | 183 (24) | 0.040 | |
| Right bundle brunch block | 80 (7) | 73 (8) | 0.175 | |
| PR interval, millisecond | 183 (±42) | 187 (±38) | 0.053 | |
| QRS duration, millisecond | 129 (±36) | 126 (±33) | 0.048 | |
| Q-T interval (corrected), millisecond | 443 (±45) | 439 (±46) | 0.022 | |
| Old anterior Q-wave AMI | 207 (17) | 198 (22) | 0.004 | |
| Old lateral Q-wave AMI | 94 (8) | 89 (10) | 0.078 | |
| Old inferior-posterior Q-wave AMI | 156 (13) | 175 (20) | <0.001 | |
| Radionuclide ventriculography (MUGA Scan) | ||||
| Left ventricular ejection fraction, % | 23 (±7) | 23 (±7) | 0.911 | |
| Right ventricular ejection fraction, % | 34 (±12) | 33 (±11) | 0.032 | |
| Regional wall motion abnormalities | 635 (54) | 889 (61) | 0.002 | |
| Global wall motion abnormalities | 922 (79) | 700 (79) | 0.969 | |
| Peak flow rate, end diastolic volume per second | 1.27 (±0.83) | 1.13 (±0.64) | <0.001 | |
Outcomes in the VA vs. Non-VA Hospitals
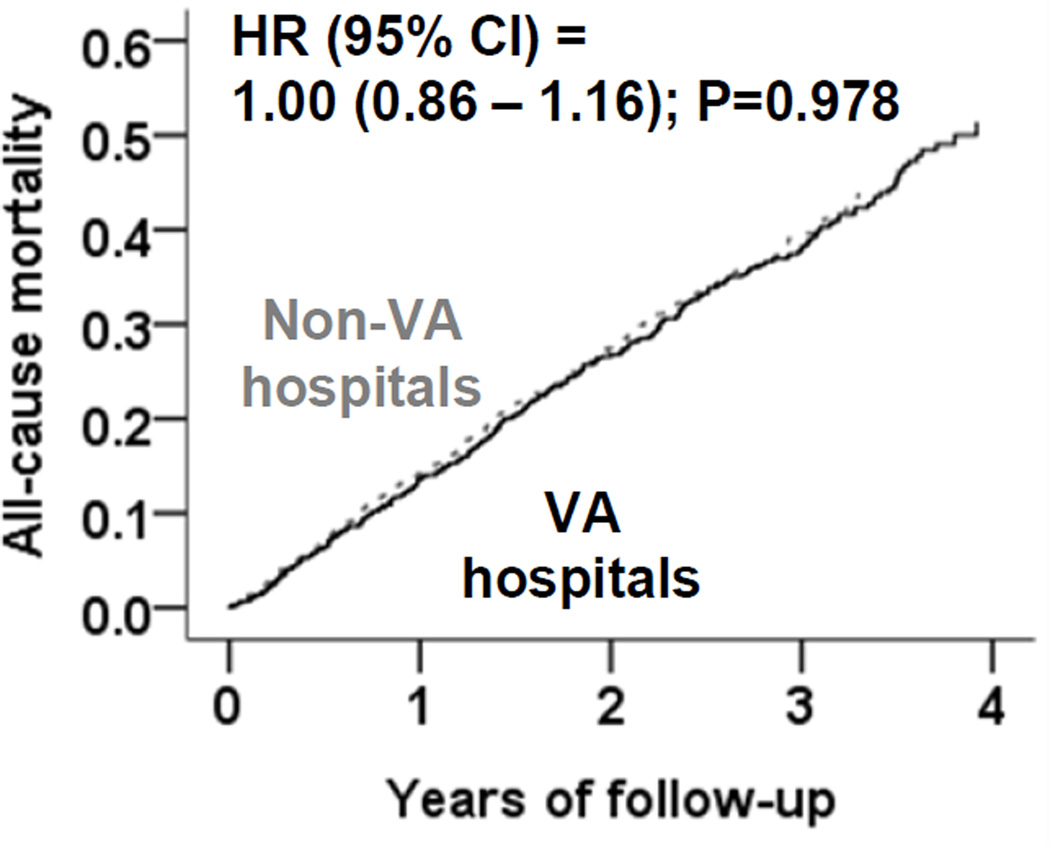
During an average of 2 years of follow-up, all-cause mortality occurred in 35% and 32% of patients receiving care in the VA and non-VA hospitals, respectively (unadjusted hazard ratio HR associated with VA hospitals, 1.09; 95% confidence interval CI, 0.94–1.26; Table 2). This association remained unchanged after adjustment for age and race (HR, 1.00; 95% CI, 0.86–1.16; Figure and Table 2) or multivariable-adjustment (HR, 0.94; 95% CI, 0.80–1.10). Among BEST participants randomized to the bucindolol group, 34% and 30% of VA and non-VA patients, respectively, died, (multivariable-adjusted HR associated with VA hospitals, 0.93; 95% CI, 0.74–1.17) while among BEST participants randomized to the placebo group, 36% and 33% of VA and non-VA patients, respectively, died (multivariable-adjusted HR, 0.93; 95% CI, 0.74–1.15). Similarly, among Caucasian BEST participants, 34% and 31% of VA and non-VA patients, respectively, died (multivariable-adjusted HR, 1.01; 95% CI, 0.84–1.21), while among African American BEST participants, 36% and 34% of VA and non-VA patients, respectively, died (multivariable-adjusted HR, 0.79; 95% CI, 0.55–1.14). HRs and 95% CIs for other outcomes associated with VA patients are displayed in Table 3. Compared to patients treated in the non-VA hospitals, those treated in the VA hospitals had a trend toward a lower risk of HF death or HF hospitalization. Although the risk for AMI death was higher among VA hospital patients, there were only 14 events.
Table 2.
All-cause mortality in BEST participants with advanced chronic systolic heart failure receiving care at the Veterans Affairs (VA) vs. non-VA hospitals
| Hazard ratio (95% confidence interval); p values | ||
|---|---|---|
| Non-veterans (n=1,216) | Veterans (n=898) | |
| Unadjusted mortality, n (%) | 383 (32%) | 313 (35%) |
| Step 1: Unadjusted | 1.00 (Reference) | 1.09 (0.94 – 1.26); p=0.274 |
| Step 2: Step 1 + age, race (African American) | 1.00 (Reference) | 1.00 (0.86 – 1.16); p=0.978 |
| Step 3: Step 2 + past medical history, medications, clinical findings* | 1.00 (Reference) | 0.94 (0.80 – 1.10); p=0.448 |
Includes body mass index, smoking, duration of heart failure, CAD, diabetes, hypertension, atrial fibrillation, PAD, CKD, randomization to bucindolol, ACE inhibitor or ARB, digoxin, diuretic, NYHA class, LVEF, RVEF, cardiothoracic ratio, pulmonary edema, pulse, systolic and diastolic blood pressure, hemoglobin, serum creatinine, serum cholesterol and plasma norepinephrine
Figure.
Age-race-adjusted mortality among BEST participants with advanced chronic systolic heart failure receiving care at the Veterans Affairs (VA) vs. non-VA hospitals
Table 3.
Multivariable-adjusted cause-specific mortalities and hospitalizations among BEST participants with advanced chronic systolic heart failure receiving care at the Veterans Affairs (VA) vs. non-VA hospitals
| Outcomes | Events (%) | Unadjusted HR (95% CI); p value |
Multivariable-adjusted* HR (95% CI); p value |
|
|---|---|---|---|---|
| Cardiovascular mortality | ||||
| Non-veterans | 332 (27) | 1.00 (Reference) | 1.00 (Reference) | |
| Veterans | 264 (29) | 1.06 (0.90–1.25); p =0.475 | 0.92 (0.74–1.10); p =0.359 | |
| Heart failure mortality | ||||
| Non-veterans | 127 (10) | 1.00 (Reference) | 1.00 (Reference) | |
| Veterans | 90 (10) | 0.94 (0.72–1.23); p =0.652 | 0.76 (0.57–1.02); p =0.067 | |
| Sudden cardiac death | ||||
| Non-veterans | 166 (14) | 1.00 (Reference) | 1.00 (Reference) | |
| Veterans | 144 (16) | 1.17 (0.93–1.46); p =0.180 | 1.05 (0.83–1.33); p =0.664 | |
| Mortality due to acute myocardial infarction | ||||
| Non-veterans | 6 (1) | 1.00 (Reference) | 1.00 (Reference) | |
| Veterans | 14 (2) | 3.09 (1.19–8.06); p =0.021 | 3.12 (1.19–8.19); p =0.021** | |
| All-cause hospitalization | ||||
| Non-veterans | 746 (61) | 1.00 (Reference) | 1.00 (Reference) | |
| Veterans | 583 (65) | 1.09 (0.98–1.21); p =0.120 | 0.99 (0.88–1.10); p =0.868 | |
| Heart failure hospitalization | ||||
| Non-veterans | 471 (39) | 1.00 (Reference) | 1.00 (Reference) | |
| Veterans | 347 (39) | 0.96 (0.84–1.08); p =0.609 | 0.88 (0.76–1.02); p =0.092 | |
Adjusted for age, race, body mass index, smoking, duration of heart failure, CAD, diabetes, hypertension, atrial fibrillation, PAD, CKD, randomization to bucindolol, ACE inhibitor or ARB, digoxin, diuretic, NYHA class, LVEF, RVEF, cardiothoracic ratio, pulmonary edema, pulse, systolic and diastolic blood pressure, hemoglobin, serum creatinine, serum cholesterol and plasma norepinephrine
Adjusted for age and race only.
Predictors of Outcomes in the VA vs. Non-VA Hospitals
Significant common predictors for all-cause mortality for patients receiving care in the VA and non-VA hospitals were chronic kidney disease, peripheral arterial disease, pulmonary edema and left ventricular EF <20% (Table 4). Although African American race, NYHA class IV symptoms, atrial fibrillation, and right ventricular EF <20% were significant predictors of death only among patients receiving care at non-VA hospitals, none of these differences were statistically significant.
Table 4.
Predictors of all-cause mortality among of BEST participants with advanced chronic systolic heart failure receiving care at the Veterans Affairs (VA) vs. non-VA hospitals
| Hazard ratio* (95% confidence interval); p value | ||
|---|---|---|
| Non-veterans (n=1,216) | Veterans (n=898) | |
| Age (every year increase) | 1.01 (1.00 – 1.02); p=0.017 | 1.01 (0.999 – 1.02); p=0.080 |
| African American | 1.44 (1.10 – 1.89); p=0.008 | 1.14 (0.86 – 1.50); p=0.358 |
| NYHA Class IV | 1.43 (1.03 – 1.99); p=0.034 | 1.20 (0.58 – 1.68); p=0.285 |
| Coronary artery disease | 1.13 (0.89 – 1.42); p=0.321 | 1.33 (0.997 – 1.77); p=0.053 |
| Diabetes mellitus | 1.16 (0.93 – 1.45); p=0.180 | 1.13 (0.900 – 1.43); p=0.287 |
| Hypertension | 0.81 (0.65 – 1.00); p=0.050 | 1.10 (0.854 – 1.43); p=0.448 |
| Atrial fibrillation | 1.44 (1.15 – 1.81); p=0.001 | 1.09 (0.849 – 1.39); p=0.512 |
| Peripheral arterial disease | 1.70 (1.31 – 2.20); p<0.001 | 1.33 (1.03 – 1.72); p=0.028 |
| Chronic kidney disease | 1.51 (1.21 – 1.87); p<0.001 | 1.76 (1.38 – 2.23); p=<0.001 |
| Bucindolol | 0.89 (0.73 – 1.09); p=0.268 | 0.88 (0.706 – 1.10); p=0.270 |
| Pulmonary edema | 1.54 (1.16 – 2.04); p=0.003 | 1.60 (1.18 – 2.16); p=0.002 |
| LV ejection fraction <20% | 1.45 (1.17 – 1.79); p=0.001 | 1.61 (1.27 – 2.05); p<0.001 |
| RV ejection fraction <20% | 1.76 (1.33 – 2.33); p<0.001 | 0.91 (0.63 – 1.32); p=0.620 |
Discussion
Findings from the current study demonstrate that patients with advanced systolic HF receiving care at VA hospitals were older and had a higher baseline symptom and morbidity burden, yet we observed no evidence of a higher all-cause mortality or all-cause hospitalization among these patients when compared with those receiving care at non-VA hospitals. We also observed that patients receiving care at the VA hospitals had a trend toward a lower risk of HF death or HF hospitalization. In addition, major risk factors for mortality were similar between patients receiving care at the VA and non-VA hospitals. Patients receiving care at non-VA hospitals had additional risk factors that were not observed among VA patients, although these differences were not statistically significant. To the best of our knowledge, this is the first comparative study of health and outcomes of patients with advanced HFrEF receiving care at VA vs. non-VA hospitals.
Age is a powerful predictor of mortality in patients with HF,20, 21 and VA hospital patients in our study were on an average 4 years older than non-VA hospital patients. Despite their older age, VA hospital patients had a similar unadjusted mortality as that of non-VA hospital patients suggesting that VA hospital patients in fact had a relatively lower mortality. A potential explanation for this health benefit is that VA patients were biologically younger than their chronological age and their non-VA counterparts. A biological basis for lower mortality for VA patients may be supported by the later onset of HF in these patients. Among HF patients mean age often reflect the age of HF onset. For example, African American HF patients (vs. Caucasians) who have an early onset of HF,22 are also known to have a lower mean age.23, 24 In the age-adjusted model, this early-stage disease would be expected to explain in part the relative survival advantage of VA patients despite a higher symptom and comorbidity burden that has been shown to be associated with poor outcomes.25–29 A late-stage HF may also help explain the lower HF death and HF hospitalization among VA hospitals patients as pump failure is generally less common until HF is more advanced.30, 31,32 Other likely explanations for a relatively better outcomes for VA hospital HF patients are intense physical exercise during early military years and a more disciplined life-style thereafter. However, the latter notion is not supported by the higher prevalence of current smokers among the VA patients, which along with a higher prevalence of coronary heart disease may also suggest a survivor cohort effect as a potential explanation for better outcomes. Another potential explanation is differences in health care quality reported in VA compared with non-VA hospitals.11, 33
Prognostic parity between HFrEF patients receiving care at VA vs. non-VA hospitals is also reflected in the commonality of major risk factors for death between the two groups. For example, LVEF, CKD, pulmonary edema and peripheral arterial disease were significant predictors of death for both groups. The VA vs. non-VA disparity in some of the other risk factors, which were predictors only in the non-VA setting, are intriguing, and deserved further discussion. For example, there were similar number of African Americans in both groups, yet only in the non-VA setting, African Americans (vs. Caucasians) had higher risk of mortality. It is not clear why African American HF patients had worse outcome in the non-VA setting. However, within the VA system, among hospitalized real-world HF patients, African American (vs. Caucasians) HF patients have been shown to have lower risk-adjusted mortality that was not clearly explained by a differential healthcare utilization.12 The lack of a mortality benefit for African American VA HF patients in our study may potentially be explained by the smaller sample size of ambulatory RCT-eligible HFrEF patients. A similar heterogeneity in the effect of a low right ventricular EF was also observed despite rather similar baseline values. It has been suggested that the higher risk of death among African Americans in the BEST trial may in part be explained by their lower right ventricular EF.34
Several prior studies examined characteristics and outcomes of patients receiving care in the VA vs. non-VA hospitals and reported similar overall finding that despite a higher disease burden patients receiving care at VA hospitals have similar outcomes as those receiving care at non-VA hospitals.11, 35 However, to the best of our knowledge, this is the first report of a comprehensive comparison of characteristics and outcomes of patients with advanced HFrEF receiving care at the VA vs. non-VA settings. Findings of the current study are important as they provide potential insights regarding HF care across the VA and non-VA settings. The VA vs. non-VA differences in the risk factors for death, while intriguing, were not statistically significant and would need to be interpreted with caution.
Our study has several limitations. Patients in our study had an EF <35% and NYHA class III/IV and may not be generalizable to all HF patients. We had no data on depression, an important co-morbidity and risk factor. Also, BEST was conducted in the 1990s and the risk factor profile may have changed, especially the smoking rate has been reported to decline. Further, treatment practices for HFrEF have also changed during the ensuing years, although the changes would be expected to be similar in both the VA and non-VA settings. Since veterans may receive care in the non-VA settings and this may vary by patient age and duration of HF, which may influence some of the findings. Differences in HF etiology between the races may in part explain the differences in risk factors for outcome as African American HF patients are more likely to have hypertension, which may be associated with lower mortality but higher hospitalizations. Finally, it is possible that some veterans from the VA hospital group received care in non-VA hospitals, which may result in regression dilution, thus potentially underestimating the VA vs. non-VA outcome differences, and explaining the null findings observed in our study.
In conclusion, we observed that consistent with findings from other studies, despite older age and a higher symptom and cardiovascular morbidity burden, outcomes of HFrEF patients receiving care at VA hospitals were similar to those receiving care at non-VA hospitals, suggesting a relative survival benefit among these patients. Future studies need to examine if primary and secondary prevention of these cardiovascular comorbid conditions may further improve survival for patients with HF receiving care at VA and non-VA hospitals.
Acknowledgments
Sources of Funding
Dr. Ahmed was in part supported by grants (R01-HL085561 and R01-HL097047) from the National Heart, Lung, and Blood Institute (NHLBI), Bethesda, Maryland and an intramural support from the UAB Comprehensive Cardiovascular Center, Birmingham, Alabama
Footnotes
Disclosures
None.
References
- 1.Heidenreich PA, Sahay A, Kapoor JR, Pham MX, Massie B. Divergent trends in survival and readmission following a hospitalization for heart failure in the veterans affairs health care system 2002 to 2006. J Am Coll Cardiol. 2010;56:362–368. doi: 10.1016/j.jacc.2010.02.053. [DOI] [PubMed] [Google Scholar]
- 2.Singh SN, Fisher SG, Carson PE, Fletcher RD. Prevalence and significance of nonsustained ventricular tachycardia in patients with premature ventricular contractions and heart failure treated with vasodilator therapy. Department of veterans affairs chf stat investigators. J Am Coll Cardiol. 1998;32:942–947. doi: 10.1016/s0735-1097(98)00338-6. [DOI] [PubMed] [Google Scholar]
- 3.Deedwania PC, Singh BN, Ellenbogen K, Fisher S, Fletcher R, Singh SN. Spontaneous conversion and maintenance of sinus rhythm by amiodarone in patients with heart failure and atrial fibrillation: Observations from the veterans affairs congestive heart failure survival trial of antiarrhythmic therapy (chf-stat). The department of veterans affairs chf-stat investigators. Circulation. 1998;98:2574–2579. doi: 10.1161/01.cir.98.23.2574. [DOI] [PubMed] [Google Scholar]
- 4.Singh SN, Fisher SG, Deedwania PC, Rohatgi P, Singh BN, Fletcher RD. Pulmonary effect of amiodarone in patients with heart failure. The congestive heart failure-survival trial of antiarrhythmic therapy (chf-stat) investigators (veterans affairs cooperative study no. 320) J Am Coll Cardiol. 1997;30:514–517. doi: 10.1016/s0735-1097(97)00157-5. [DOI] [PubMed] [Google Scholar]
- 5.Cohn JN, Johnson G. Heart failure with normal ejection fraction. The v-heft study. Veterans administration cooperative study group. Circulation. 1990;81:III48–III53. [PubMed] [Google Scholar]
- 6.Cohn JN, Archibald DG, Francis GS, Ziesche S, Franciosa JA, Harston WE, Tristani FE, Dunkman WB, Jacobs W, Flohr KH, et al. Veterans administration cooperative study on vasodilator therapy of heart failure: Influence of prerandomization variables on the reduction of mortality by treatment with hydralazine and isosorbide dinitrate. Circulation. 1987;75:IV49–IV54. [PubMed] [Google Scholar]
- 7.Cohn JN, Archibald DG, Ziesche S, Franciosa JA, Harston WE, Tristani FE, Dunkman WB, Jacobs W, Francis GS, Flohr KH, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a veterans administration cooperative study. N Engl J Med. 1986;314:1547–1552. doi: 10.1056/NEJM198606123142404. [DOI] [PubMed] [Google Scholar]
- 8.Brooks MS, Laditka SB, Laditka JN. Evidence of greater health care needs among older veterans of the vietnam war. Mil Med. 2008;173:715–720. doi: 10.7205/milmed.173.8.715. [DOI] [PubMed] [Google Scholar]
- 9.Hoerster KDLK, Simpson T, McFall M, Reiber G, Nelson KM. Health and health behavior differences: U.S. Military, veteran, and civilian men. Am J Prev Med. 2012;43:483–489. doi: 10.1016/j.amepre.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 10.Smith-Osborne A. Veterans administration health care policies as a protective mechanism supporting an expected life trajectory after military service. Soc Work Public Health. 2013;28:81–96. doi: 10.1080/19371918.2011.552038. [DOI] [PubMed] [Google Scholar]
- 11.Petersen LA, Normand SL, Daley J, McNeil BJ. Outcome of myocardial infarction in veterans health administration patients as compared with medicare patients. N Engl J Med. 2000;343:1934–1941. doi: 10.1056/NEJM200012283432606. [DOI] [PubMed] [Google Scholar]
- 12.Deswal A, Petersen NJ, Souchek J, Ashton CM, Wray NP. Impact of race on health care utilization and outcomes in veterans with congestive heart failure. J Am Coll Cardiol. 2004;43:778–784. doi: 10.1016/j.jacc.2003.10.033. [DOI] [PubMed] [Google Scholar]
- 13.The BEST Investigators. A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. New Engl J Med. 2001;344:1659–1667. doi: 10.1056/NEJM200105313442202. [DOI] [PubMed] [Google Scholar]
- 14.The BEST Investigators. Design of the beta-blocker evaluation survival trial (best) Am J Card. 1995;75:1220–1223. doi: 10.1016/s0002-9149(99)80766-8. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed MI, White M, Ekundayo OJ, Love TE, Aban I, Liu B, Aronow WS, Ahmed A. A history of atrial fibrillation and outcomes in chronic advanced systolic heart failure: A propensity-matched study. Eur Heart J. 2009;30:2029–2037. doi: 10.1093/eurheartj/ehp222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pawar PP, Jones LG, Feller M, Guichard JL, Mujib M, Ahmed MI, Roy B, Rahman T, Aban IB, Love TE, White M, Aronow WS, Fonarow GC, Ahmed A. Association between smoking and outcomes in older adults with atrial fibrillation. Arch Gerontol Geriatr. 2012;55:85–90. doi: 10.1016/j.archger.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.White M, Desai RV, Guichard JL, Mujib M, Aban IB, Ahmed MI, Feller MA, de Denus S, Ahmed A. Bucindolol, systolic blood pressure, and outcomes in systolic heart failure: A prespecified post hoc analysis of best. Can J Cardiol. 2012;28:354–359. doi: 10.1016/j.cjca.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Desai RV, Guichard JL, Mujib M, Ahmed MI, Feller MA, Fonarow GC, Meyer P, Iskandrian AE, Bogaard HJ, White M, Aban IB, Aronow WS, Deedwania P, Waagstein F, Ahmed A. Reduced right ventricular ejection fraction and increased mortality in chronic systolic heart failure patients receiving beta-blockers: Insights from the best trial. Int J Cardiol. 2013;163:61–67. doi: 10.1016/j.ijcard.2011.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meyer P, Desai RV, Mujib M, Feller MA, Adamopoulos C, Banach M, Lainscak M, Aban I, White M, Aronow WS, Deedwania P, Iskandrian AE, Ahmed A. Right ventricular ejection fraction <20% is an independent predictor of mortality but not of hospitalization in older systolic heart failure patients. Int J Cardiol. 2012;155:120–125. doi: 10.1016/j.ijcard.2011.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmed MI, Mujib M, Desai RV, Feller MA, Daniel C, Aban IB, Love TE, Deedwania P, Pitt B, Aronow WS, Ahmed A. Outcomes in younger and older adults with chronic advanced systolic heart failure: A propensity-matched study. Int J Cardiol. 2012;154:128–133. doi: 10.1016/j.ijcard.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wahle C, Adamopoulos C, Ekundayo OJ, Mujib M, Aronow WS, Ahmed A. A propensity-matched study of outcomes of chronic heart failure (hf) in younger and older adults. Arch Gerontol Geriatr. 2009;49:165–171. doi: 10.1016/j.archger.2008.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gambassi G, Agha SA, Sui X, Yancy CW, Butler J, Giamouzis G, Love TE, Ahmed A. Race and the natural history of chronic heart failure: A propensity-matched study. J Card Fail. 2008;14:373–378. doi: 10.1016/j.cardfail.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rathore SS, Foody JM, Wang Y, Smith GL, Herrin J, Masoudi FA, Wolfe P, Havranek EP, Ordin DL, Krumholz HM. Race, quality of care, and outcomes of elderly patients hospitalized with heart failure. JAMA. 2003;289:2517–2524. doi: 10.1001/jama.289.19.2517. [DOI] [PubMed] [Google Scholar]
- 25.Ahmed MI, Aronow WS, Criqui MH, Aban I, Love TE, Eichhorn EJ, Ahmed A. Effects of peripheral arterial disease on outcomes in advanced chronic systolic heart failure: A propensity-matched study. Circ Heart Fail. 2010;3:118–124. doi: 10.1161/CIRCHEARTFAILURE.109.866558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahmed A, Aban IB, Vaccarino V, Lloyd-Jones DM, Goff DC, Jr, Zhao J, Love TE, Ritchie C, Ovalle F, Gambassi G, Dell'Italia LJ. A propensity-matched study of the effect of diabetes on the natural history of heart failure: Variations by sex and age. Heart. 2007;93:1584–1590. doi: 10.1136/hrt.2006.113522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gheorghiade M, Flaherty JD, Fonarow GC, Desai RV, Lee R, McGiffin D, Love TE, Aban I, Eichhorn EJ, Bonow RO, Ahmed A. Coronary artery disease, coronary revascularization, and outcomes in chronic advanced systolic heart failure. Int J Cardiol. 2011;151:69–75. doi: 10.1016/j.ijcard.2010.04.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahmed A, Aronow WS, Fleg JL. Higher new york heart association classes and increased mortality and hospitalization in patients with heart failure and preserved left ventricular function. Am Heart J. 2006;151:444–450. doi: 10.1016/j.ahj.2005.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meyer P, Ekundayo OJ, Adamopoulos C, Mujib M, Aban I, White M, Aronow WS, Ahmed A. A propensity-matched study of elevated jugular venous pressure and outcomes in chronic heart failure. Am J Cardiol. 2009;103:839–844. doi: 10.1016/j.amjcard.2008.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carson P, Anand I, O'Connor C, Jaski B, Steinberg J, Lwin A, Lindenfeld J, Ghali J, Barnet JH, Feldman AM, Bristow MR. Mode of death in advanced heart failure: The comparison of medical, pacing, and defibrillation therapies in heart failure (companion) trial. J Am Coll Cardiol. 2005;46:2329–2334. doi: 10.1016/j.jacc.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 31.Zile MR, Gaasch WH, Anand IS, Haass M, Little WC, Miller AB, Lopez-Sendon J, Teerlink JR, White M, McMurray JJ, Komajda M, McKelvie R, Ptaszynska A, Hetzel SJ, Massie BM, Carson PE, Investigators IP. Mode of death in patients with heart failure and a preserved ejection fraction: Results from the irbesartan in heart failure with preserved ejection fraction study (i-preserve) trial. Circulation. 2010;121:1393–1405. doi: 10.1161/CIRCULATIONAHA.109.909614. [DOI] [PubMed] [Google Scholar]
- 32.Kheirbek RE, Alemi F, Citron BA, Afaq MA, Wu H, Fletcher RD. Trajectory of illness for patients with congestive heart failure. J Palliat Med. 2013;16:478–484. doi: 10.1089/jpm.2012.0510. [DOI] [PubMed] [Google Scholar]
- 33.Edes T, Shreve S, Casarett D. Increasing access and quality in department of veterans affairs care at the end of life: A lesson in change. J Am Geriatr Soc. 2007;55:1645–1649. doi: 10.1111/j.1532-5415.2007.01321.x. [DOI] [PubMed] [Google Scholar]
- 34.White M, Patel K, Caldentey G, Deedwania P, Ahmed A. Low right ventricular ejection fraction: A potential explanation for racial differences in mortality in advanced systolic heart failure in the best-blocker evaluation of survival trial. J Am Coll Cardiol. 2013;61 (10_S) [Google Scholar]
- 35.Kress DC, Kroncke GM, Chopra PS, Cohen DJ, Rasmussen PW, Nichols RD, Beatty ES, Berkoff HA. Comparison of survival in cardiac surgery at a veterans administration hospital and its affiliated university hospital. Arch Surg. 1988;123:439–443. doi: 10.1001/archsurg.1988.01400280045009. [DOI] [PubMed] [Google Scholar]