Abstract
Cone-beam computed tomography (CBCT) is an advanced imaging modality that has high clinical applications in the field of dentistry. CBCT proved to be a successful investigative modality that has been used for dental and maxillofacial imaging. Radiation exposure dose from CBCT is 10 times less than from conventional CT scans during maxillofacial exposure. Furthermore, CBCT is highly accurate and can provide a three-dimensional volumetric data in axial, sagittal and coronal planes. This article describes the basic technique, difference in CBCT from CT and main clinical applications of CBCT.
Keywords: Cone-beam computed tomography, diagnostic imaging, spiral computed tomography, X-ray
Introduction
Cone beam computed tomography (CBCT) is a radiographic imaging method that allows accurate, three-dimensional (3D) imaging of hard tissue structures. CBCT is the most significant among the medical diagnostic imaging modalities that have emerged recently. This imaging modality is capable of providing sub-millimeter resolution (2 line pair/mm) images of higher diagnostic quality, with shorter scanning times (~60 s). Radiation exposure dose from CBCT is 10 times less than from conventional CT scans during maxillofacial exposure (68 µSv compared with 600 µSv of conventional CT)1 and also it has got great dimensional accuracy (only about 2% magnification). Increasing availability of this technology is now providing the dental clinician an imaging modality, which is capable of providing a 3D representation of the maxillofacial structures with minimal distortion and reduced radiation hazards.
Technical basis
The CBCT technique consists of the use of a round or rectangular cone shaped X- ray beam with a single 360° scan where the X-ray source and a reciprocating array of detector simultaneously move around the patient’s head, which is stabilized with a head holder. Single projection images, known as “basis” images, are acquired at certain degree intervals, which are similar to lateral cephalometric radiographic images, each slightly offset from one another. The series of such basis projection images is referred to as the projection data, on which software programs incorporating sophisticated algorithms are applied to generate a 3D volumetric data set, which can be used to provide primary reconstruction images in all three orthogonal planes (axial, sagittal, and coronal).
CBCT versus spiral CT
The fundamental difference between CBCT and spiral CT is that CBCT utilizes a cone shaped beam and an area detector and that captures a full volume of image in a single rotation where patient movement is not required. On the other hand, spiral CT makes use of a narrowly collimated, fan-shaped X-ray beam and a linear group of detectors. Here, the patient has to be moved continuously along the gantry while the X-ray beam rotates around the patient. In most of the dental offices conventional CT has not been widely utilized due to the high radiation dosage, the cost of the procedure, proximity to a CT center and a dentist’s unfamiliarity with interpreting CT results. The use of CBCT can negate these concerns and allow for improved diagnosis and patient safety.2 On comparison with CT, CBCT has high accuracy and sensitivity and can capture the maxilla and mandible in a single rotation of the X-ray source.3-5
Clinical Applications in the Maxillofacial Region
CBCT has gained increased acceptance as a 3D imaging modality offering an alternative to CT especially in the maxillofacial area.6
Applications in oral and maxillofacial surgery
Most important application of CBCT in oral and maxillofacial surgery is to investigate the exact 3D location of jaw pathologies like benign or malignant tumors, inflammatory bone lesions,7 to assess impacted teeth, to investigate the exact location of supernumerary teeth and to assess their relation to vital structures,8 to demarcate changes in the cortical and trabecular bone in cases of bisphosphonate-associated necrosis of the jaws, and to evaluate bone grafts. CBCT is also used to investigate the pathologies related to paranasal sinuses, and to assess obstructive sleep apnoea.9 Since the images of CBCT are collected as a combination of several two-dimensional (2D) slices, this technique is superior in overcoming superimpositions and is helpful in calculating surface distances. These superior features have made CBCT the technique to go for the investigations of mid-facial fracture and in inter-operative visualization of the facial bones after fracture. Furthermore, as CBCT is not a magnetic resonance technique, it is the best option for intra-operative evaluation during procedures involving gun-shot wounds. CBCT is considered to be a better imaging modality in assessing metal fragments in the face in cases of fragments embedded from automobile or industrial accidents, gunshot and for localizing retained broken dental needles. It is widely used in planning orthognathic and orthomorphic surgeries. Regardless of the low soft-tissue contrast of CBCT images, it is considered to be superior to spiral CT in depicting soft-tissue calcifications, such as carotid atherosclerosis, tonsilloliths and sialoliths. Small calcifications are easier to be identified on a CBCT scan than panoramic or intraoral radiographs, and these calcifications can be important diagnostic clues for some types of cysts and tumors (e.g. Pindborg tumor, Gorlin cyst).10 CBCT has invaluable applications in the evaluation of dental age, arch segment positioning, cleft size, morphology of the defect, the volume of graft material necessary for repair, stability of the arch after grafting, the quality of the bone graft over a period, and the effect on overall facial growth in cleft lip and palate cases.11 Contrast-enhanced CBCT images have been widely used in treatment adaptation for tumor visualization and may lead to improved treatment outcome in the case of radiotherapy patients.12
Application in endodontics
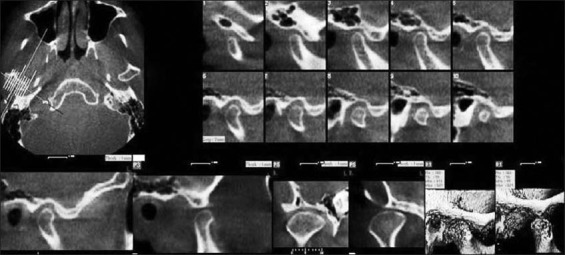
CBCT is an important investigative tool in diagnosing apical lesions supported by a few research studies that have shown that contrast-enhanced CBCT images can be used to differentiate between apical granulomas and apical cysts by measuring the lesion density.13 It has applications in cases of differentiating the lesions of endodontic and non-endodontic origin. Inconspicuous cases of vertical root fractures are best diagnosed with CBCT.14 It is more favored to periapical radiographs in the detection of fractures in mesiodistal or buccolingual directions, in the detection of horizontal root fractures, in the measurement of depth in dentin, for the better visualisation of fractured instrument and root perforation (Figure 1). Conventional 2D radiographs have limitations in detecting early stages of inflammatory root resorption, whereas CBCT has proved its potential in detecting these lesions in its early stage itself. In addition to detecting the presence of resorption in cases of external root resorption, CBCT is superior in detecting the extent of these lesions also.15 It can be used to measure the number of roots, to determine root morphology, root canals and accessory canals, and to establish their working lengths and angulations. It gives an accurate assessment of root canal fillings, helps in the detection of pulpal extensions in talon cusps and also helpful in detecting the position of fractured instruments. It is a reliable tool for the pre-surgical assessment of the propinquity of the tooth to adjacent vital structures, the size and extent of the lesion through very accurate measurements. In emergency cases requiring a tooth assessment after trauma, CBCT applications can aid in deriving a proper diagnosis to determine the most suitable treatment approach.
Figure 1.

Cone beam computed tomography image detecting the presence of fractured instrument and root perforation on a molar tooth.
Applications in implant dentistry
Greater accuracy of CBCT in measurements at lower radiation doses has made it a preferred option in implant dentistry.16 The incorporation of new software to construct surgical guides has further reduced the possibility of structural damage. CBCT provides reliable information that has led to improvements in case selection and aids in both qualitative and quantitative measurement of bone, which has led to a reduction in implant failure. Virtual implant planning using CBCT data empowers the clinicians to predict and visualize the end result before initiating treatment.17 The assessment of success of bone grafts and other post-treatment evaluations are also possible.
Applications in orthodontics
The applications of CBCT in cephalometric analysis with the introduction of a new software in orthodontic assessment has made CBCT, the tool of choice for assessing facial growth, age, airway function and disturbances in tooth eruption. CBCT is a reliable tool in assessing the proximity of the tooth to vital structures that may interfere with orthodontic treatment. CBCT acts as a useful visual guiding technique for safe insertion of these anchors as well as to evaluate the bone density before, during and after treatment, especially in cases that require the placement of tiny screw implants as temporary anchors. This imaging modality incorporates multiple different views of an object in one scan (e.g., frontal, right lateral, left lateral, 45°, and sub-mental views), which is an additional advantage. CBCT has the added advantage of self-correction of its images for magnification producing orthogonal images with a 1:1 ratio thus making it a more accurate option of investigation for the clinician.18 Recent studies have shown that the orthodontists had significant differences in perception of localization and root damage, and a substantially higher confidence in diagnosis and treatment planning with CBCT images than with routine radiographs such as panoramic, occlusal or periapical views.19,20
Applications in temporomandibular joint (TMJ) imaging
CBCT is highly effective tool to define the true position of the condyle in the fossa, thereby revealing the possibility of dislocation of the disk in the joint and the extent of translation of the condyle in the fossa (Figure 2). Due to its accuracy, CBCT facilitates easy measurement of the roof of the glenoid fossa and provides the ability to visualize soft tissue around the TMJ, thereby reducing the requirement for the use of magnetic resonance imaging in these cases. These advantages made CBCT, a valuable imaging device of choice in cases of trauma, pain and dysfunction, and fibro osseous ankylosis, as well as in the detection of condylar cortical erosion and cysts.21 The advanced 3D imaging features facilitates the safe application of the image-guided puncture technique, which is a treatment option for the TMJ disk adhesion.
Figure 2.
Axial, sagittal, coronal and three-dimensional reconstructed cone beam computed tomography images of a normal temporomandibular joint depicting the condyle-fossa relationship in open and closed mouth position.
Applications in periodontics
CBCT has invaluable applications in the branch of periodontics. High measurement accuracy with minimal margins of error allows the use of CBCT in obtaining a detailed morphologic description of the bone, with measurement accuracy equal to that of direct measurement with a periodontal probe. The accurate assessment of furcation involvement and detection of buccal and lingual defects are possible where the value of conventional 2D radiography is limited. CBCT has made a remarkable contribution in an accurate assessment of intra-bony defects, dehiscence, fenestration defects and periodontal cysts. CBCT has also proved its supremacy in evaluating the outcome of regenerative periodontal therapy. It has made an important application that allows for the analysis of the buccal and lingual surfaces and an improved visualization of the depth, height and morphology of the defects (Figures 3 and 4).22
Figure 3.

Sagittal cone beam tomograms showing the measurements of the distances from the cementoenamel junction to the bottom of the defect in the distal surface of 27.
Figure 4.

Sagittal cone beam tomograms showing the measurements of the width of the defect in the distal surface of 27.
Applications in forensic dentistry
Dental age estimation is considered an important factor in the field of forensic science. Non-invasive method of dental age assessment can be performed using CBCT in which an estimate of the subject’s age can be derived from the subject’s pulp/tooth ratio. CBCT images of the face through routine scanning protocols are reliable for measuring soft tissue thickness in the oro facial region, and these images provide an adequate representation of the facial soft tissues.23
Conclusion
CBCT technology is increasingly accessible in dental practice. It hugely expands the fields for diagnosis and treatment possibilities for the patients. However, CBCT should only be used after careful consideration, especially about the patient exposure, where conventional 2D imaging techniques are not sufficient or where access to the technological processes such as guided surgery will improve patient management.
Footnotes
Conflicts of Interest: None
Source of Support: Nil
References
- 1.Loubele M, Bogaerts R, Van Dijck E, Pauwels R, Vanheusden S, Suetens P, et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol. 2009;71(3):461–8. doi: 10.1016/j.ejrad.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Howerton WB, Jr, Mora MA. Use of conebeam computed tomography in dentistry. Gen Dent. 2007;55(1):54–7. [PubMed] [Google Scholar]
- 3.Winter AA, Pollack AS, Frommer HH, Koenig L. Cone beam volumetric tomography vs. medical CT scanners. N Y State Dent J. 2005;71(4):28–33. [PubMed] [Google Scholar]
- 4.Honda K, Larheim TA, Maruhashi K, Matsumoto K, Iwai K. Osseous abnormalities of the mandibular condyle: Diagnostic reliability of cone beam computed tomography compared with helical computed tomography based on an autopsy material. Dentomaxillofac Radiol. 2006;35(3):152–7. doi: 10.1259/dmfr/15831361. [DOI] [PubMed] [Google Scholar]
- 5.Hashimoto K, Kawashima S, Araki M, Iwai K, Sawada K, Akiyama Y. Comparison of image performance between cone-beam computed tomography for dental use and four-row multidetector helical CT. J Oral Sci. 2006;48(1):27–34. doi: 10.2334/josnusd.48.27. [DOI] [PubMed] [Google Scholar]
- 6.Schulze D, Blessmann M, Pohlenz P, Wagner KW, Heiland M. Diagnostic criteria for the detection of mandibular osteomyelitis using cone-beam computed tomography. Dentomaxillofac Radiol. 2006;35(4):232–5. doi: 10.1259/dmfr/71331738. [DOI] [PubMed] [Google Scholar]
- 7.Macleod I, Heath N. Cone-beam computed tomography (CBCT) in dental practice. Dent Update. 2008;35(9):590–2. doi: 10.12968/denu.2008.35.9.590. 594. [DOI] [PubMed] [Google Scholar]
- 8.Tetradis S, Anstey P, Graff-Radford S. Cone beam computed tomography in the diagnosis of dental disease. J Calif Dent Assoc. 2010;38(1):27–32. [PubMed] [Google Scholar]
- 9.Naitoh M, Hirukawa A, Katsumata A, Ariji E. Evaluation of voxel values in mandibular cancellous bone: Relationship between cone-beam computed tomography and multislice helical computed tomography. Clin Oral Implants Res. 2009;20(5):503–6. doi: 10.1111/j.1600-0501.2008.01672.x. [DOI] [PubMed] [Google Scholar]
- 10.Ahmad M, Freymiller E. Cone beam computed tomography: Evaluation of maxillofacial pathology. J Calif Dent Assoc. 2010;38(1):41–7. [PubMed] [Google Scholar]
- 11.Quereshy FA, Savell TA, Palomo JM. Applications of cone beam computed tomography in the practice of oral and maxillofacial surgery. J Oral Maxillofac Surg. 2008;66(4):791–6. doi: 10.1016/j.joms.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 12.Søvik A, Rødal J, Skogmo HK, Lervåg C, Eilertsen K, Malinen E. Adaptive radiotherapy based on contrast enhanced cone beam CT imaging. Acta Oncol. 2010;49(7):972–7. doi: 10.3109/0284186X.2010.498433. [DOI] [PubMed] [Google Scholar]
- 13.Christiansen R, Kirkevang LL, Gotfredsen E, Wenzel A. Periapical radiography and cone beam computed tomography for assessment of the periapical bone defect 1 week and 12 months after root-end resection. Dentomaxillofac Radiol. 2009;38(8):531–6. doi: 10.1259/dmfr/63019695. [DOI] [PubMed] [Google Scholar]
- 14.Kajan ZD, Taromsari M. Value of cone beam CT in detection of dental root fractures. Dentomaxillofac Radiol. 2012;41(1):3–10. doi: 10.1259/dmfr/25194588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alshehri MA, Alamri H, Alshalhoub M. Applications of CBCT in dental practice: A literature review. Dent News. 2011;18:26–34. [PubMed] [Google Scholar]
- 16.Dreiseidler T, Mischkowski RA, Neugebauer J, Ritter L, Zöller JE. Comparison of cone-beam imaging with orthopantomography and computerized tomography for assessment in presurgical implant dentistry. Int J Oral Maxillofac Implants. 2009;24(2):216–25. [PubMed] [Google Scholar]
- 17.Worthington P, Rubenstein J, Hatcher DC. The role of cone-beam computed tomography in the planning and placement of implants. J Am Dent Assoc. 2010;141(Suppl 3):19S–24. doi: 10.14219/jada.archive.2010.0358. [DOI] [PubMed] [Google Scholar]
- 18.Vandenberghe B, Jacobs R, Bosmans H. Modern dental imaging: A review of the current technology and clinical applications in dental practice. Eur Radiol. 2010;20(11):2637–55. doi: 10.1007/s00330-010-1836-1. [DOI] [PubMed] [Google Scholar]
- 19.Kapila S, Conley RS, Harrell WE., Jr The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofac Radiol. 2011;40(1):24–34. doi: 10.1259/dmfr/12615645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haney E, Gansky SA, Lee JS, Johnson E, Maki K, Miller AJ, et al. Comparative analysis of traditional radiographs and cone-beam computed tomography volumetric images in the diagnosis and treatment planning of maxillary impacted canines. Am J Orthod Dentofacial Orthop. 2010;137(5):590–7. doi: 10.1016/j.ajodo.2008.06.035. [DOI] [PubMed] [Google Scholar]
- 21.Howerton WB, Jr, Mora MA. Advancements in digital imaging: What is new and on the horizon? J Am Dent Assoc. 2008;139(Suppl):20S–4. doi: 10.14219/jada.archive.2008.0354. [DOI] [PubMed] [Google Scholar]
- 22.de Faria Vasconcelos K, Evangelista KM, Rodrigues CD, Estrela C, de Sousa TO, Silva MA. Detection of periodontal bone loss using cone beam CT and intraoral radiography. Dentomaxillofac Radiol. 2012;41(1):64–9. doi: 10.1259/dmfr/13676777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fourie Z, Damstra J, Gerrits PO, Ren Y. Accuracy and reliability of facial soft tissue depth measurements using cone beam computer tomography. Forensic Sci Int. 2010;199(1-3):9–14. doi: 10.1016/j.forsciint.2010.02.018. [DOI] [PubMed] [Google Scholar]


