Abstract
Purpose
The purpose of this study was to calibrate the items for the Communicative Participation Item Bank (CPIB) using Item Response Theory (IRT). One overriding objective was to examine if the IRT item parameters would be consistent across different diagnostic groups, thereby allowing creation of a disorder-generic instrument. The intended outcomes were the final item bank and a short form ready for clinical and research applications.
Methods
Self-report data were collected from 701 individuals representing four diagnoses: multiple sclerosis, Parkinson’s disease, amyotrophic lateral sclerosis and head and neck cancer. Participants completed the CPIB and additional self-report questionnaires. CPIB data were analyzed using the IRT Graded Response Model (GRM).
Results
The initial set of 94 candidate CPIB items were reduced to an item bank of 46 items demonstrating unidimensionality, local independence, good item fit, and good measurement precision. Differential item function (DIF) analyses detected no meaningful differences across diagnostic groups. A 10-item, disorder-generic short form was generated.
Conclusions
The CPIB provides speech-language pathologists with a unidimensional, self-report outcomes measurement instrument dedicated to the construct of communicative participation. This instrument may be useful to clinicians and researchers wanting to implement measures of communicative participation in their work.
Keywords: Communicative participation, Item Response Theory, Outcomes measurement
Introduction
Outcome measurement in the field of adult communication disorders has recently been influenced by two major trends – patient-reported outcome (PRO) measurement and Item Response Theory (IRT). PRO is simply defined as measurement of any aspect of health status that comes directly from the patient without interpretation by a healthcare provider or anyone else (Food and Drug Administration, 2009). Without such measures, the impact of any condition cannot be fully captured. PROs are particularly useful in the field of rehabilitation where physical or physiologic markers are not available for many critical aspects of disabling conditions. They are used to capture data that are either not observable or where the patient is in the best position to assess the construct, such as well-being or satisfaction. In clinical practice, PROs can be used as screening or monitoring tools, as aids in shared decision making, and as a means of facilitating communication in multidisciplinary teams (Greenhalgh, 2009). PRO measures are not new to the field of speech-language pathology. They are available for many conditions including aphasia (Doyle, McNeil, Hula, & Mikolic, 2003), dysarthria (Donovan, Kendall, Young, & Rosenbek, 2008), voice disorders (Hogikyan & Sethuraman, 1999; Jacobson et al., 1997; Ma & Yiu, 2001), and stuttering (Yaruss & Quesal, 2006; Zraick, Atcherson, & Brown, 2012), as some representative examples.
PRO instruments are particularly well suited to measuring a construct referred to as ‘communicative participation.’ Communicative participation is defined as taking part in life situations where knowledge, information, ideas or feelings are exchanged (Eadie et al., 2006). It is based on the concept of participation as “involvement in life situations” that is one component of the World Health Organization’s (WHO) International Classification of Functioning, Disability and Health (ICF) (World Health Organization, 2001). Communicative participation specifically addresses the communication that occurs in the various life situations and roles in which people are engaged. People with communication disorders are at risk for restricted communicative participation if they are not able to successfully navigate communication situations in the ‘real world’ and therefore fulfill their life roles. While participation could be evaluated from several different perspectives, many researchers and clinicians agree that assessment of participation must include patient-report because only the person living with the health condition experiences the unique combination of physical, environmental, social, and personal factors that shape participation outcomes (Brown et al., 2004; M. Law, 2002; Perenboom & Chorus, 2003; Whiteneck, 1994). For clinicians and researchers aligned with the ICF framework, communicative participation is gaining attention as a critical intervention target and outcomes indicator to ensure that speech-language pathology interventions make a relevant and meaningful difference in the lives of clients.
For the past several years, our research group has been developing a PRO targeting communicative participation called the Communicative Participation Item Bank (CPIB) (Baylor, Yorkston, Eadie, Miller, & Amtmann, 2009; Yorkston et al., 2008). The CPIB is an instrument designed for community-dwelling adults across different communication disorders and life situations. The items ask about the extent to which the respondent’s condition interferes with participation in a wide range of speaking situations such as talking to people you do not know, talking on the telephone to get information, ordering a meal in a restaurant, and talking in groups of people, to name a few examples. The CPIB focuses on communicative participation in speaking situations (as opposed to other communication modalities) for two reasons. First, prior research has suggested that different communication modalities may represent different constructs, and therefore, including other modalities (e.g., writing) in the instrument may make the scores difficult to interpret (Doyle, Hula, McNeil, Mikolic, & Matthews, 2005). Second, the CPIB was intended to be applicable across a range of disorders including speech and voice disorders as well as mild-moderate language or cognitive disorders. Verbal communication is a modality that is likely to be affected across most communication disorders, whereas items that ask about communication modalities such as reading and writing would not necessarily be relevant to many speech and voice-disorder populations.
The CPIB has been developed following the approach used by the NIH Patient-Reported Outcomes Measurement Information Systems (PROMIS) network (Fries, Bruce, & Cella, 2005). The first step was to conduct a review of PRO instruments existing at the time the project was initiated. The purpose of this review was to examine the extent to which the construct of communicative participation was included in speech-language pathology instruments (Eadie et al., 2006). The conclusions reached from that review were that while the construct of communicative participation was represented among the items of several speech-language pathology instruments, no instrument was dedicated to the construct of communicative participation. Existing instruments likely confounded the measurement of participation with other constructs such as physical symptoms or emotional coping. After developing a preliminary item set, the CPIB items underwent qualitative review in cognitive interviews (DeWalt, Rothrock, Yount, & Stone, 2007; Willis, 2005) with adults representing a range of communication disorders (Baylor, Burns, Eadie, Britton, & Yorkston, 2011; Yorkston et al., 2008; Yorkston et al., 2007). Based on feedback from participants in these studies, the items were modified to improve the reliability, face validity and relevance of the items for the target populations.
The CPIB then underwent initial psychometric analyses in a sample of individuals with spasmodic dysphonia (SD: Baylor et al., 2009)). Following the guidelines of PROMIS (Cella et al., 2007; Reeve et al., 2007), the analysis of the CPIB with the SD sample was conducted using a Rasch model which is similar to a 1-parameter IRT model. IRT is increasingly used in health sciences to develop, evaluate, and improve PRO instruments. IRT is a set of statistical methods utilizing a family of mathematical models to estimate latent traits (constructs or characteristics of a person that cannot be directly observed) based on the psychometric characteristics of each item (e.g., item difficulty and item discrimination) and the characteristics of the responder (the level of the latent trait or ability). IRT item banks are recommended for their qualities of measurement precision, flexibility and efficiency (Cook, O'Malley, & Roddey, 2005). IRT instruments often consist of an item bank, a large set of items that are calibrated to an underlying scale (typically the logit scale) representing a range of abilities or levels of a latent trait. IRT instruments are typically administered by choosing a subset of items from the item bank that will most precisely estimate the latent trait of each respondent. The item subsets can be chosen by computer algorithms in computerized adaptive testing (Cook et al., 2005), or in the generation of targeted short forms. Tutorials are available on IRT in general (de Champlain, 2010; Embretson & Reise, 2000; Reeve et al., 2007; Revicki & Cella, 1997), and on applications of IRT in speech-language pathology in particular (Baylor, Hula et al., 2011).
The initial Rasch analyses of the CPIB conducted with the SD sample mentioned above showed favorable results (Baylor et al., 2009). The CPIB represented a sufficiently unidimensional item set. A large set of items performed well according to IRT criteria, and represented a range of levels along the trait continuum (different levels of communicative participation restrictions). One limitation of this prior study, however, was that it evaluated the function of the CPIB in a single population. One of the key goals for the CPIB is that it will be applicable across a range of communication disorders in adults. This is important so that the CPIB can be used in research and clinical applications for comparing participation restrictions and intervention outcomes across disorders. Before the CPIB can be used in multiple populations, further IRT analyses are required to examine if the psychometric properties of the items are consistent across populations. Once data are available from across multiple communication disorder populations, a final item bank and short forms can be developed.
This manuscript presents the methods and data for completing three critical steps in the continued development of the CPIB:
Conducting the IRT analyses needed to finalize item calibration for formation of the full CPIB item bank. Formation of the final item bank and presentation of the IRT item parameters will make available the data needed for future computerized adaptive testing (CAT) applications.
Conducting differential item functioning (DIF) analyses across different communication disorder populations to assess if the item bank is applicable across different disorders.
Generating a short form from the full item bank for immediate clinical application.
Methods
All methods were approved by the Institutional Review Board at the University of Washington.
Participants
Participants representing four medical diagnoses commonly associated with communication disorders were recruited to evaluate the function of the CPIB across different disorder groups. The four groups were multiple sclerosis (MS), Parkinson’s disease (PD), amyotrophic lateral sclerosis (ALS), and head and neck cancer (HNCA; oral, oral-pharyngeal or laryngeal cancer, and including those treated with laryngectomy). These groups were chosen for several reasons. First, they are adult-onset conditions, and therefore participants have experienced living as ‘typical’ communicators before the onset of the condition. That provides a perspective of change from which participants can evaluate the impact of the health condition on communicative participation. Because the impact of health conditions on communicative participation has not been directly compared between groups with acquired versus congenital conditions, the decision was made in this study to focus on acquired conditions. Second, the communication disorders associated with these conditions are largely motor speech and voice disorders. In this study, the goal was to target groups who were more likely to retain relatively strong language and cognitive skills because the sole method of data collection was self-report without the presence of a researcher to assist participants with the questionnaires. Finally, these four groups represent different speech and voice disorder characteristics with different trajectories (e.g., stable, slowly degenerative, more rapidly degenerative). This diversity was desired to examine the function of the CPIB items in varying populations.
Inclusion / Exclusion Criteria
Across all diagnostic groups, the inclusion criteria were adults age 18 or older who had been diagnosed with their medical condition at least three months prior to participation in the study. There were no restrictions on a minimum severity of disorder to qualify for participation, although the recruitment materials stated that the study was intended for individuals who felt that their ability to communicate had been affected by their medical condition. All participants needed to use speech for communication. Individuals could use augmentative or alternative communication (AAC) to supplement speech, but individuals who relied solely on AAC were not included out of concern that the relevance and appropriateness of the items in the CPIB have not yet been evaluated with AAC users. Individuals with laryngectomy could use any speech method. With regards to cognitive or linguistic function, instructions were included that the questionnaires were to be completed via self-report. While participants could receive assistance in the logistical aspects of filling out the questionnaires such as having items read to them or having someone mark their answers, the answers had to be the answers of the person with the communication disorder. If cognitive or language disorders prevented individuals from providing their own answers, the individual was excluded from the study. These issues were addressed in the screening process. There were no restrictions on treatment history although information about treatment history was collected for analysis in future studies. Participants were community-dwelling. Residents of skilled nursing facilities were not included because they are not likely engaged in the same communication situations as community-dwelling adults, and the items in the CPIB address community-based communication situations. The final inclusion criterion was English proficiency because the CPIB has not yet been translated into other languages.
Recruitment
Participants were recruited from across the United States. First, notices about the study were placed on listservs affiliated with the American Speech-Language Hearing Association. Speech-language pathologists (SLPs) on the listserv were asked if they would be willing to place fliers advertising the study in their clinics. Second, notices were placed in newsletters and on websites for support groups and organizations serving individuals with the diagnoses included in the study. Finally, the Washington Parkinson’s Disease Registry affiliated with the University of Washington was used to recruit individuals with PD. In all of these recruiting situations, clinical SLPs or staff affiliated with the support groups or organizations were not involved in the research. They assisted with making information about the study available to clients or organization members through postings in newsletters or on websites, but interested participants contacted the researchers directly for participation. Participants were paid $20 upon completion of the questionnaires. The recruitment goal was 200 participants per diagnostic group.
Data collection
Participants were asked to complete a battery of questionnaires. All questionnaires were self-report and asked about a range of experiences and symptoms associated with their health conditions in general and communication disorders in particular.
Questionnaire administration
Participants were offered the option of completing the questionnaires online or using paper forms according to their preference. Online data collection was conducted via the Assessment Center (assessmentcenter.net) website developed for NIH PROMIS (nihpromis.org). Participants who chose to complete the questionnaires on paper forms were mailed a questionnaire booklet with instructions for completing and returning the questionnaires, as well as a return stamped envelope.
Questionnaire battery
The primary focus of this study was the CPIB, the development of which is described in the introduction. For this study, the CPIB consisted of a set of 94 candidate items that had been chosen based on cognitive interviews (Baylor, Burns et al., 2011; Yorkston et al., 2008) and earlier psychometric analyses with a sample of individuals with SD (Baylor et al., 2009). The content of the full set of 94 candidate items examined in this study can be found in Table 1 and Appendix A. Table 1 presents those items from the candidate item set that were retained for the final item bank, and Appendix A presents the items that were ultimately removed from the item bank during this study. Item format can be viewed in the short form in Table 2 (which is also available as supplemental material on the journal website). Because the length of the CPIB raised concern about possible order effects for item presentation, efforts were made to implement different item orders across participants. The Assessment Center website randomized item order across participants who were using the website. Two versions of the paper questionnaires were created for each diagnostic group with the only difference between the two versions being two different randomized orders of the CPIB items.
The CPIB was the first questionnaire presented to all participants. Following the CPIB, participants were presented with additional questionnaires to collect information about their health and communication disorder symptoms. The following questionnaires were presented to all participants: 1) The Levels of Speech Usage rating scale (Baylor, Yorkston, Eadie, Miller, & Amtmann, 2008; Gray, Baylor, Eadie, Kendall, & Yorkston, 2012)} is a single-item scale on which respondents choose a category which best represents the level of speech demands they have in their daily activities. 2) A subset of eight items from the applied cognition section of the Neuro-QOL item banks (www.neuroqol.org) address reading and writing tasks in daily activities as well as tasks related to memory and problem solving. The CPIB addresses communication through speech, and the Neuro-QOL items were included to obtain information about other communication modalities as well as cognitive function. 3) The PROMIS Global Health instrument has 10 items that provide an overall indicator of physical and emotional health (Hays, Bjorner, Revicki, Spritzer, & Cella, 2009). 4) A demographic questionnaire included age, gender, marital status, living situation, geographic region, race / ethnicity, employment status, education history, time since onset of communication disorder, history of speech-language pathology services for the communication disorder, and presence of hearing loss or other significant medical concerns impacting daily activities.
Additional questionnaires were presented to each of the diagnostic groups asking about symptoms specific to that condition. The ALS Functional Rating Scale – Revised (ALSFRS-R) (Cedarbaum et al., 1999) was presented to the ALS, PD and MS groups. Although this questionnaire was originally designed for persons with ALS, the items do not directly refer to ALS but ask about a range of issues related to speech, swallowing, self-care, and mobility that were considered relevant to understanding the implications of neurologic conditions on performance of daily activities. The MS group received the mobility section of the self-report version of the Expanded Disability Status Scale (EDSS-S) (Bowen, Gibbons, Gianas, & Kraft, 1999; Kurtzke, 1983), a common measure used to indicate overall severity of MS. The PD group received the eight-item Parkinson’s Disease Questionnaire (PDQ-8) (Jenkinson, Fitzpatrick, Peto, Greenhall, & Hyman, 1997) which is a disease-specific questionnaire asking about health status related to PD. Finally, the HNCA group received the University of Washington Quality of Life (UW-QOL) questionnaire, version 4 (Rogers et al., 2002; Weymuller, Alsarraf, Yueh, Deleyiannis, & Coltrera, 2001), a health-related quality of life instrument for persons with head and neck cancer; the MD Anderson Dysphagia Inventory (MDADI), a dysphagia-specific quality of life instrument for persons with head and neck cancer (A. Chen et al., 2001); and the 10-item version of the Voice Handicap Index (VHI-10) (Rosen, Lee, Osborne, Zullo, & Murry, 2004). The data from the CPIB and the demographic questionnaires will be reported in this paper, as will the data from the speech item from the ALSFRS-R to provide an indication of speech disorder severity. Data from the remaining questionnaires will be reported in future papers.
Data analysis
Data from the Assessment Center website were downloaded in an Excel format. Data from the paper questionnaires were entered into Excel using a double entry system for reliability whereby two researchers entered the data independently and any discrepancies between the two entries were identified and resolved. The various software packages used to analyze the data will be described in the respective sections below.
Demographic Data
Descriptive analyses were completed for the demographic data using Excel and SPSS version 17 (SPSS, 2008).
IRT analyses
The Graded Response Model (GRM), a two-parameter model considering item difficulty and item discrimination was chosen for the IRT analyses (Samejima, 1969). IRTPRO software (Li, Thissen, & du Toit, 2011) was used except where specified otherwise. Most IRT item banks are based on two key assumptions – unidimensionality (the instrument measures only one trait or construct) and local independence (the probability of responding to an item is statistically independent of the probability of responding to any other item in the same instrument conditioned on the examinee’s ability; (Embretson & Reise, 2000). The data were first evaluated to ensure the assumptions of unidimensionality and local independence were met before proceeding to item calibration and additional analyses.
Unidimensionality
Unidimensionality was examined using an exploratory factor analysis (EFA) that included all 94 candidate items, and results were evaluated by examining the magnitude of eigenvalues. When calculating the ratio of the first to the second eigenvalue, a ratio of four or more indicates unidimensionality (Reeve et al., 2007). Alternatively, at least 20% of the variability on the first factor is desirable in determining unidimensionality (Reeve et al., 2007).
As a follow-up analysis, a single factor confirmatory factor analysis (CFA) was conducted to confirm unidimensionality. CFA model fit was evaluated using χ2, the Comparative Fit Index (CFI; (Bentler, 1980)), the Tucker-Lewis Index (TLI;Tucker & Lewis, 1973)), and the Root Mean Square Error of Approximation (RMSEA; (Steiger & Lind, 1980)). CFI and TLI values above .95 are preferable (Hu & Bentler, 1999), while RMSEA values of less than .08 are considered to be an acceptable fit (Browne & Cudeck, 1993). EFA and CFA were conducted using Mplus software 6.1(Muthen & Muthen, 1998).
Local dependence
Two indices were used to identify LD. The first method was to examine the residual correlation matrix after the first factor was removed in the factor analysis. Absolute values of residual correlations between items above .20 indicate possible LD. Second, Chen and Thissen’s (1997) IRT-based LD statistic was tested. According to that criterion, evidence of LD is suggested if the LD statistic for any pair of items is greater than or equal to 10. These LD statistics were generated using IRTPRO software (Li et al., 2011). When pairs or groups of items with LD were identified, one or more items from each group were removed, particularly when there was overlapping content among the items with LD. The three authors who are SLPs (CB, TE and KY) reviewed the item groups with LD to prioritize items for retention.
IRT analyses
Fitting the IRT model to the data involved examining item fit, the category response curves, and the item and test information functions.
Item fit
The goodness of fit of the GRM model was examined using the SS-Χ2 item fit statistic described by Orlando and Thissen (2000, 2003). A non-significant value (p > .05) suggests an acceptable result, indicating adequate model fit (Orlando & Thissen, 2000, 2003). Removal of items for poor item fit was an iterative process with items removed one at a time and the remaining items re-analyzed after each item removal. The decision for removal of each item was based on a combination of quantitative information in that items with poorer fit tended to be removed before items closer to the cut-off value, as well as qualitative information about item content based on feedback about the items received from participants in prior cognitive interviews regarding the importance or saliency of different situations in influencing their participation (Baylor, Burns et al., 2011; Yorkston et al., 2008).
Category response curves
Analysis of the category response curves involved visual inspection of the curves for each item to ensure that each category was the most likely to be selected by respondents at that certain level of communicative participation. The categories had already undergone major revisions in the prior study with individuals with SD, with a reduction from five to four response categories that functioned well (Baylor et al., 2009).
Test information function
The test information function was examined visually to assess the precision of measurement across the trait range. Values greater than 10 on test information functions are favorable because they are associated with reliability coefficients ≥ 0.90 and indicate high levels of reliability (Embretson & Reise, 2000). The goal was for the CPIB to have test information function values higher than 10 across the logit range from −3.0 – +3.0 logits so that the instrument would provide precise measurement across a broad range of the trait.
Differential item functioning (DIF)
DIF analyses were conducted to examine whether items functioned differently across the different diagnostic groups. If DIF is present, individuals in different groups will answer items differently even if they have the same trait level (Reeve et al., 2007). DIF can be used, therefore, to identify unwanted bias in items. In this study, one of the key research questions was if the CPIB items demonstrated DIF across the four diagnostic categories included in the study (MS, PD, HNCA, and ALS). Presence of meaningful DIF would suggest systematic differences across groups in the way that individuals respond to the items that would be unaccounted for by the trait level (communicative participation), and would indicate that different item sets or item parameters might be needed for different diagnostic groups. The absence of meaningful DIF would indicate that the same item sets and parameters could be used across diagnostic conditions and therefore a disorder-generic instrument could be developed.
For this study, only the three diagnostic groups of MS, PD and HNCA were included in the DIF analysis. The much smaller sample size for the ALS group (n=70) disqualified that group for inclusion in the DIF analysis. DIF was analyzed using the R software package Lordif (Choi, Gibbons, & Crane, 2011) which utilizes an ordinal logistic regression framework in calculating DIF (Crane, Gibbons, Jolley, & van Belle, 2006). Two criteria were considered in this study to detect meaningful DIF: 10% and 5% changes in beta (Crane, Van Belle, & Larson, 2004); (Crane et al., 2007); (Choi et al., 2011).
Similar to methods used by Cook et al., (2011), the impact of DIF on CPIB scores was evaluated by re-calibrating the items to the GRM model using the DIF adjusted item parameters for each diagnostic group. Then the person scores were re-calculated using the DIF adjusted parameters. Finally, the DIF-adjusted person scores were compared to the original person scores (i.e., when not accounting for DIF) using a Pearson correlation to examine the strength of the association between the original and the DIF-adjusted scores. A high correlation would suggest that adjusting for DIF would make a negligible difference in the person scores, and any DIF could be ignored. In that case, item parameters calculated when combining all groups together could be used without concern for significant impact on scoring. Low correlations between DIF-adjusted and non-DIF-adjusted scores would suggest that the DIF would make a meaningful difference on final scores and that the group-specific item parameters should be used.
Developing a short form
The long-term goal for the CPIB is for the item parameters to be used in computerized adaptive testing (CAT) applications. Until a CAT application is available, short forms can be constructed and utilized via either paper-and-pencil or computer administration. After finalizing the item bank for the CPIB, this study continued on to generate a short form with the goal of having a general form that would be appropriate for a wide range of communication situations across a wide range of participation levels. Items were selected based on a combination of statistical analyses and judgment by the SLP authors regarding item content. Items were chosen to represent a range of communication experiences encountered by most community-dwelling adults. In terms of statistical properties, the goal was to compile an item set with the most favorable test information function possible, meaning the highest information possible across a broad range of trait levels. The effective range of measurement (i.e., the range of the trait that was measured with sufficient precision) was given priority over amount of information at the peak to achieve the goal of adequate measurement across a wide range of the trait. Item selection proceeded in an iterative manner, with the test information functions of various item sets compared visually. The number of items for the short form was set at ten to achieve a balance between having a large enough item set to represent a range of communication situations while keeping response burden low.
Once the items were chosen for the short form, reliability between the full 46-item set and the 10-item short form was evaluated. A new set of person scores (theta) was generated using just the items included on the short form. The strength of association between person scores for the full 46-item set and the 10-item short form was evaluated using a Pearson correlation. Finally, a scoring guide for the 10-item short form was generated using the software IRTScore (Flora & Thissen, 2002).
Results
Participants
Descriptive demographic information is presented for each diagnosis and for the total sample in Appendix B. Key findings are summarized in this section. Across all four diagnoses, 1001 participants enrolled in the study. Questionnaires were returned by 779 participants. Returned questionnaires were screened to ensure that participants met the inclusion criteria and that they were not missing more than 10% of responses for the CPIB to ensure adequate data for analysis. Seventy-eight of the returned questionnaires were removed from the study for not meeting one of the above criteria. Of the initial 1001 participants, 701 returned completed, usable questionnaires for a final response rate of 70.0%. Of these 701 questionnaires included in the analysis, 458 (65.3%) were completed using the online questionnaires and 243 (34.7%) were completed using the paper questionnaire format.
The mean age of participants across all diagnoses was 58.8 years (SD 12.4) with a range of 24–99 years. The sample consisted of 320 (45.7%) males and 380 (54.2%) females (one participant did not report gender). Within each diagnosis, gender distribution represented typical patterns. For example, there were proportionately more females in the MS group and more males in the HNCA group. The sample was predominately Caucasian (92.2%), with the second most commonly selected race / ethnicity category being “more than one race” at 2.7%. The majority of participants were married or currently in a committed relationship (73.5%). The majority of participants (80.2%) lived with family including spouse, children or other relatives. Geographic representation was calculated according to the United States divisions used in reporting census data (http://www.census.gov/geo/www/us_regdiv.pdf; retrieved February, 2012). The south and west regions of the United States each contributed approximately one-third of the participants. Most of the remaining participants were in the northeast or midwest regions. The relatively large representation of non-US participants in the HNCA group was due to participation from individuals in Canada.
For employment, 25.9% of participants were in paid employment including full-time, part-time or in-home business employment. 40.9% of participants had stopped working due to their medical conditions. Stopping working due to medical concerns was the most commonly selected employment category for all diagnostic groups except for the HNCA group. Retirement unrelated to medical conditions was the most common employment category for the HNCA participants. The sample was highly educated with 58.0% of participants completing either undergraduate or graduate college degrees.
The mean time since diagnosis of medical condition was 9.0 years (SD 8.4) with a wide range from less than one year to 60 years. The MS group had the longest time since diagnosis with a mean of 12.2 years, while the ALS group had the shortest duration with a mean of 3.4 years. Participants were asked if they had a history of hearing loss or other medical conditions that, in their opinion, affected their participation in their daily activities. Hearing loss was reported by 245 (35.0%) participants. The presence of other medical conditions significant enough to impact daily activities was reported by 288 (41.1%) participants. The most commonly reported conditions included depression, back and neck problems, arthritis, diabetes, cardiac problems, bowel and bladder problems, asthma, and mobility issues.
Appendix C presents a summary of self-reported speech disorder severity for the MS, PD and ALS groups, as well as communication mode for the HNCA participants. The most commonly endorsed severity category, chosen by almost half of the participants (48.5%), was the middle in a range of five categories described as, “I sometimes have to repeat words to be understood.” Participants were asked if they had received speech-language pathology services, and 258 (36.8%) reported that they had. Participants with MS were least likely to have received speech-language pathology services (11.1% of participants with MS), and those with HNCA were the most likely to have received services (60.4% of participants with HNCA).
IRT analyses
Unidimensionality
The EFA produced 6 factors with eigenvalues greater than 1. The ratio of the first eigenvalue to the second eigenvalue was approximately 15:1, and the first factor explained 63% of the total variability. The two-factor EFA solution based on the default Mplus promax rotation (i.e., oblique) indicated that the correlation between two factors was 0.74. These results support the hypothesis that the items are sufficiently unidimensional, and this was tested further with a one-factor CFA. Fit values for the one-factor CFA of the 94 CPIB items were: χ2 (4277, N = 701) = 14869.31, p < .01; CFI = 0.933; TLI = 0.931; and RMSEA = 0.059.
Local dependence
When evaluated with the one-factor CFA, 11 item-pairs had an absolute value of the residual correlation greater than .20 suggesting local dependence. In addition, 62 item-pairs exceeded 10 on Chen and Thissen’s (1997) LD statistics. At this stage, 23 items from locally dependent groups were removed. The one-factor CFA was then repeated. Fit values for the one-factor CFA for the remaining 71 CPIB items were excellent: χ2 (2414, N = 701) = 8119.11, p < .01; CFI = 0.953; TLI = 0.951; and RMSEA = 0.058. Residual correlations were also examined, and no item-pairs had an absolute value of the residual correlation greater than .20. However, 9 item-pairs still showed an LD statistic larger than 10. Additional items were removed and the analyses were repeated until the items were reduced to a set that met the assumptions of unidimensionality and local independence. Through this iterative process, 33 items were recommended for removal. The SLP authors decided to retain five of those items, however, based on the content of the items which was deemed either unique and not captured by other items, or because they were of central importance to individuals’ experiences based on prior cognitive interviews (Baylor, Burns et al., 2011; Yorkston et al., 2008). The five items that were retained even with evidence of LD, and the reasons for retaining these items were as follows: The items “Talking with people at home about things that need to get done around the house,” and “Talking about a plan for daily activities with people who help you at home” were retained because they address communication in the home environment which is often regarded as a more comfortable communication environment with familiar people and situations. Keeping these items would specifically address situations that might be on the ‘easier’ end of the communicative participation continuum to ensure as broad of a range of measurement as possible in the item set. The item, “Telling someone how to do something,” was kept because it represented a more difficult task of giving specific information or instructions that might have to be more precise than casual or social conversation. The item, “Talking to family or friends on the phone,” was kept for further analysis because the phone had been a situation of critical importance for many participants in prior cognitive interviews (Baylor, Burns et al., 2011; Yorkston et al., 2008), and the authors wanted to represent a variety of phone situations in the item bank. Finally, “Talking with people when you are tired,” was retained because of reports from prior cognitive interview participants of the significant impact of fatigue on communication. At the end of the analysis for LD, therefore, 28 items had been removed and 66 items were retained for further analyses. Appendix A, section A lists the items that were removed due to LD.
Item fit
Of the 66 items remaining after the local dependence analyses, twenty items were removed due to poor item fit resulting in an item set of 46 items for further analysis. Appendix A, section B lists the items that were removed due to poor item fit. Table 1 presents the final 46 items in the item bank along with their item parameters (discrimination and category thresholds) and fit statistics.
Category response curves
A visual inspection of the category response curves was conducted, but no items were removed during this step. One item, “Expressing thanks or appreciation” showed category response curves that were marginal, but because this item had met the criteria for item fit, it was retained in the item bank.
Information function
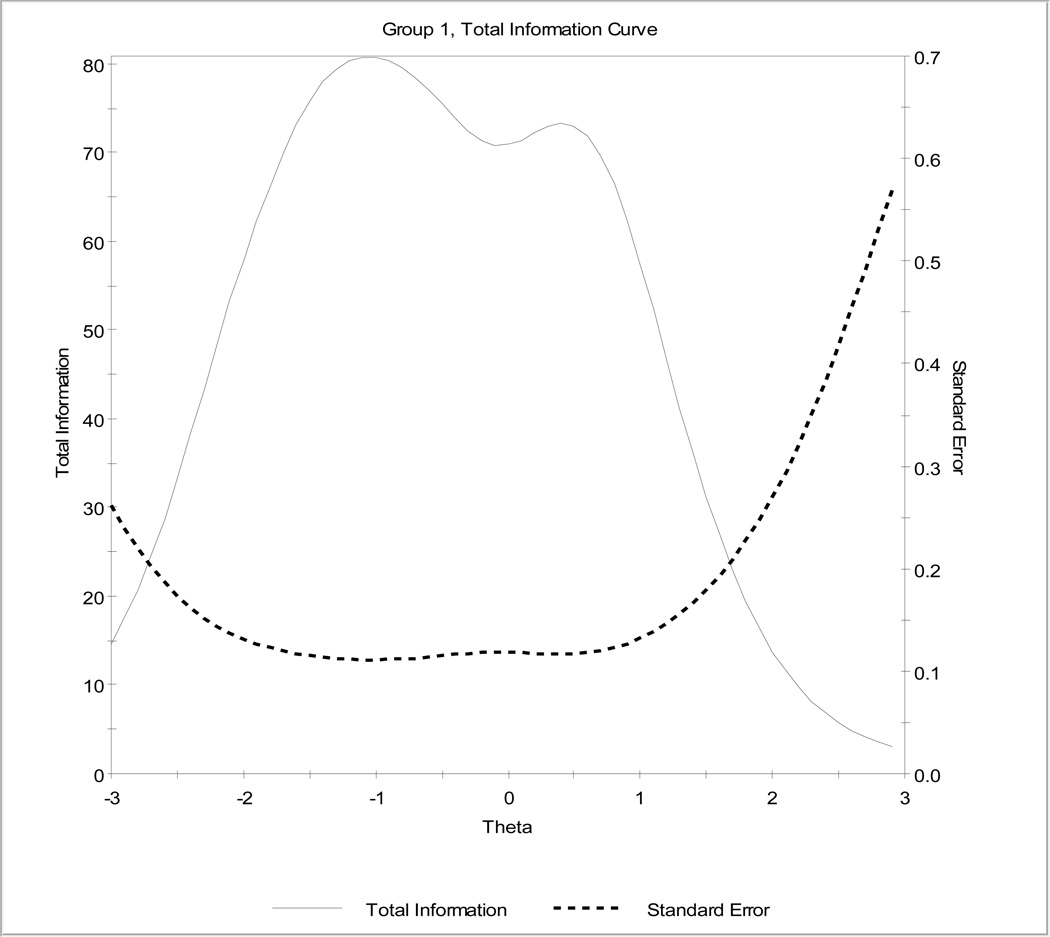
Figure 1 contains the test information function for the 46 items included in the final CPIB item bank. The final item bank shows strong reliability (information >10) in the range from −3.0 to just above +2.0 logits. The test information function suggests that the item bank measures with less precision at very high levels of participation (people who report very low levels of interference in participation).
Figure 1.
This is the test information function for the final item set of 46 items in the CPIB item bank. The solid line is the information function and the dotted line is the standard error curve.
Differential item function
Evaluating DIF using the criterion of beta change of 5% resulted in 23 items being identified as having DIF. These items are noted in Table 1. When the DIF-adjusted person scores were calculated, the Pearson correlation between the DIF-adjusted and non-DIF-adjusted scores was 0.995. The mean difference between DIF-adjusted and non-adjusted scores was −0.048 logits with a range of differences between adjusted and non-adjusted scores of −0.39 to +0.23 logits.
Using the DIF criterion of 10% beta change, only four items were identified as having meaningful DIF. These items are also identified in Table 1. The correlation between the original and adjusted scores was 1.00. The mean difference between DIF-adjusted and non-adjusted scores was −0.03 logits with a range of score differences from −0.22 to +0.16 logits.
Based on these results, the conclusion was reached that although statistically significant DIF was identified using the two criteria of beta change, the adjustments for DIF would result in negligible changes in person scores due to correlations between adjusted and non-adjusted scores greater than 0.99 in both situations. For this reason, the conclusion was reached that any DIF in this item set among the three diagnostic groups of MS, PD and HNCA could be disregarded, and a disorder-generic item set utilizing item parameters generated with all groups combined in this study could be utilized.
10-Item General Short Form
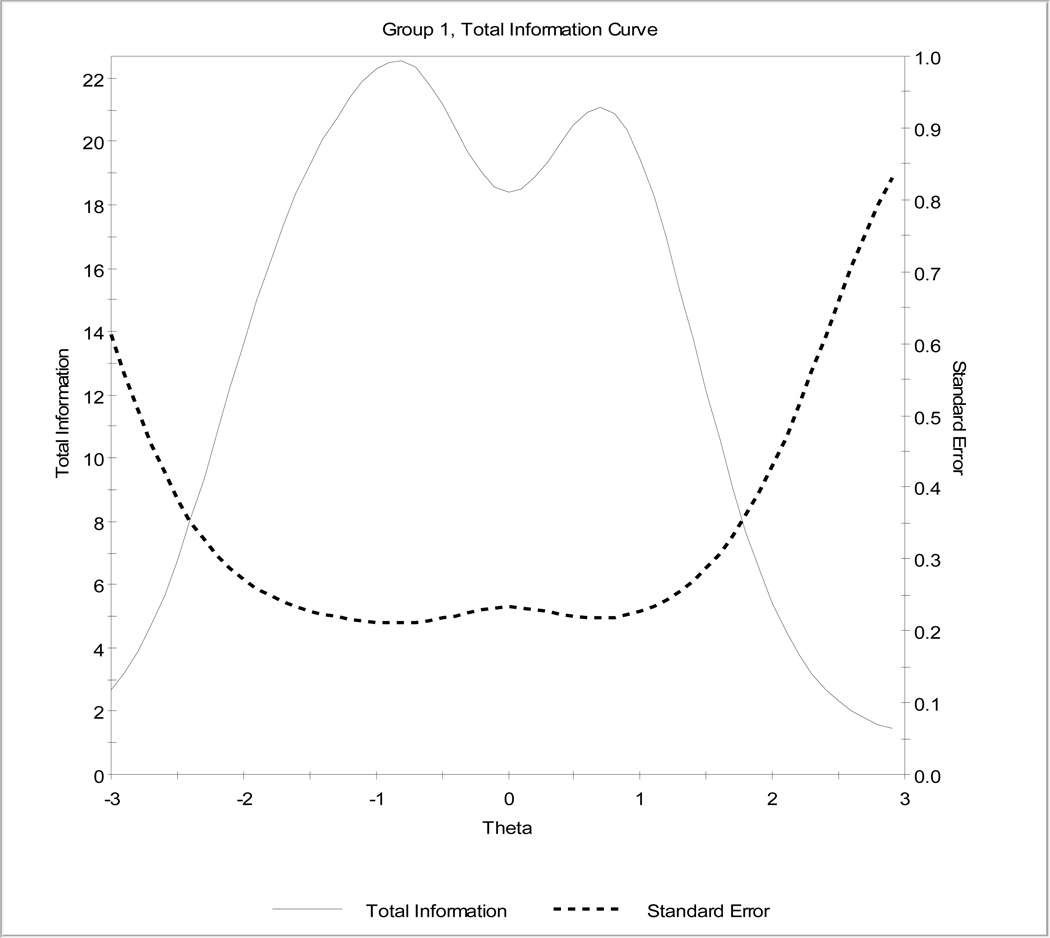
Once final items were chosen for the item bank, a 10-item short form was created. The General Short Form of the CPIB developed in this study is in Table 2. The items represent a range of communication situations commonly encountered by community-dwelling adults. The test information function for the short form is in Figure 2. When comparing the test information functions for the full 46-item bank and the 10-item short form, the general shape of the function is preserved in the short form. The short form naturally has less information because it has fewer items (the test information function is a summation of the information in the items in that particular item set). The short form does not cover as broad of a trait range as the full 46-item set, but this is to be expected due to limiting the short form to 10 items.
Figure 2.
This is the test information function for the 10-item General Short Form of the CPIB. Note that the overall shape of the function is similar to that for the full 46-item set although the amount of information in the short form (y axis) is lower because there are fewer items.
Person scores (theta) were obtained for the short form by conducting a new IRT analysis using IRTPRO (Li et al., 2011). The correlation between person scores on the full item bank and the short form was 0.971 (significant at p<.001) and suggests that the scores from the short form are almost identical to the scores based on the full item set.
Table 2 also presents a scoring guide for the short form. A summary score can be generated by adding up the values for each item. The values of each response category are as follows: Not at all = 3, A little = 2, Quite a bit = 1, and Very much = 0. This format results in high scores being more favorable (indicating less interference in participation). The total summary score can range from 0 – 30. A table providing conversions between summary scores and logit values was created using IRTScore (Flora & Thissen, 2002). The conversion table shows that the short form covers the theta range of −2.58 to +2.10 logits. The conversion table also presents a translation of the scores into T scores with a mean of 50 and standard deviation of 10 if standard scores are desired. The T score of 50 represents the mean level of communicative participation of the calibration sample. This score conversion table is applicable ONLY for the short form presented in this manuscript. Although IRT item banks have considerable flexibility in terms of being able to combine different sets of items for different testing purposes, a new score conversion table needs to be created for each unique item set because the relationship between summary scores and logit values will differ depending on the specific item set that is administered. Converting the summary score to the logits scale is recommended for several reasons. First, the logit scale approximates an equal interval scale which allows more valid mathematical operations on the scores (comparing differences between scores or averaging across scores). Second, if different item sets are used in future applications, summary scores cannot be compared directly across different item sets. Each item set has different measurement properties due to the unique parameters of each item in the set. These unique parameters are not captured in the summary score, but are taken into consideration when the scoring conversions to logits or standard scores are generated by IRT software. Valid comparisons across different item sets must therefore be made at the logit level or standard score level, not the summary score level.
Discussion
This study had three key purposes: 1) to calibrate the items and finalize the item set for the CPIB item bank, 2) to assess the ability of the CPIB to serve as a cross-disorder instrument, and 3) to generate a clinic-ready short form using one item subset from the CPIB. Over the course of the analyses, the initial set of 94 candidate CPIB items was reduced to a final item bank of 46 items. The item bank demonstrates strong evidence of unidimensionality and no evidence of local dependence. These findings suggest that the item set measures the intended construct of interference in communicative participation without the confounding influences of other constructs. All 46 items in the final item bank fit the GRM model, which also supports the validity of the items in that participant responses are based on communicative participation and not on other confounding variables. The test information function suggests that the item bank has a broad effective range of measurement, although measurement precision is not as strong at the very high end of the scale. This means that the item bank may be somewhat less precise for estimating communicative participation for people who are doing very well (reporting very little interference in communicative participation). Analyses of DIF across the three groups with adequate sample sizes (MS, PD, HNCA) suggested that there was evidence of statistically significant DIF on some items. However, the DIF–adjusted person scores were so highly correlated with non-DIF-adjusted scores that the authors concluded that accounting for DIF made no meaningful or clinically significant change in scoring.
One of the key products of this study, therefore, is the 46-item CPIB item bank. The item parameters reported in this paper provide the psychometric data that can be used for administering the CPIB, such as in a CAT application. Because a CAT application is not immediately available for clinical use, this paper also includes a 10-item short form that can be used in clinical situations now. The short form was constructed for the purpose of providing an instrument that will be applicable across a broad range of individuals. Items were selected to represent a variety of communication situations, and to represent a broad range of the trait. The short form does not cover as broad of a measurement range as the full item bank, as would be expected with the smaller number of items in the short form. A scoring conversion table is included for scoring and interpreting the short form (see Table 2).
The CPIB fills a gap in outcome measurement instruments available to speech-language pathologists. Having a unidimensional PRO instrument dedicated to the construct of communicative participation will facilitate advancement of both clinical and scholarly work in the area of communicative participation. Since the adoption of the WHO ICF (World Health Organization, 2001) by ASHA for preferred practice patterns (American Speech-Language-Hearing Association, 2004), communicative participation has received more attention as a critical component of clinical practice. Optimizing participation might be regarded as the ultimate outcome of intervention in that clients are able to do the things they want and need to do in their daily lives.
Research has provided preliminary evidence that people with different communication disorders experience similar participation restrictions (Baylor, Burns et al., 2011). For example, people with different communication disorders face similar challenges in employment situations (Garcia, Laroche, & Barrette, 2002) and with communication in healthcare settings (J. Law, Bunning, Byng, Farrelly, & Heyman, 2005; Murphy, 2006; Nordehn, Meredith, & Bye, 2006; O'Halloran, Worrall, & Hickson, 2011). These similarities in participation restrictions across disorders have important implications for future clinical and scholarly work in the area of communicative participation. Given these similarities, there may be much to be gained in learning about participation restrictions and how to alleviate them by looking at this construct across disorders instead of focusing on a single communication disorder at a time. For example, would efforts focused on modifications of physical and social environments reduce barriers to participation across communication disorders in a way that direct intervention working on communication skills of the individuals with disorders may not achieve? With its ability to serve as a cross-disorder instrument, the CPIB may be a useful instrument in answering questions such as these.
Further studies are needed to fully validate the CPIB and to address limitations in this study. These limitations largely relate to using the CPIB with other populations not included in this study. For example, future research is needed to evaluate whether the CPIB is relevant to adults living in skilled nursing or other medical facilities because the items ask about communication in typical community-based environments. Items specifically tailored to situations in medical facilities may be more useful to those populations. In addition, the items may not be as relevant to adults in the very acute stage of a disorder (such as in acute care or inpatient rehabilitation) if they have not yet had the opportunity to experience living in their typical environments with the new communication disorder. The CPIB has also not yet been tested with people who depend solely on AAC for communication, with individuals who have more involved language or cognitive impairments, or with individuals who have congenital as opposed to acquired communication disorders. Ideally, a new DIF analysis would be completed with any new population to ensure that the psychometric properties are consistent across groups. While this may not be feasible, clinicians should be cautious in their use of the CPIB with populations that differ significantly in terms of severity or type of communication disorder than the populations included in this study.
In terms of its use as a tool to guide treatment planning and outcomes measurement, future research is needed to evaluate the ability of the CPIB to detect change over time and treatment, and to estimate clinically minimally important differences. Comparisons with existing PROs used in speech-language pathology are needed, as are comparisons with clinician-judged measures of disorder severity. These comparisons will clarify the relationships (or lack thereof) among impairment, activity, and participation, and will assist clinicians in understanding the contributions of participation-focused assessment to treatment planning.
Finally, although the CPIB provides an overall client-report of participation restrictions, it does not necessarily identify the source of those restrictions. Interference in participation may come from physical impairments limiting communication abilities, but it may also come from many other sources interacting with the communication disorder such as other health symptoms (and consequences of treatment such as medication or radiation effects), environmental conditions including communication partners, or even a client’s personal outlook (personal priorities or coping strategies) (Baylor, Burns et al., 2011; Becker et al., 2011; Eadie, 2003; Hartelius, Elmberg, Holm, Lovberg, & Nikolaidis, 2008; Howe, 2008; Howe, Worrall, & Hickson, 2008a, 2008b; Threats, 2007; Whitehill, Ma, & Tse, 2010). After administering the CPIB, clinicians must engage clients in deeper interviews about the situations in which they experience interference and what factors they feel contribute to participation restrictions. Clinicians will also want to continue with traditional measures of impairment and performance of communication skills to compare with measures of participation such as the CPIB to ensure a comprehensive approach to assessment and treatment of communication disorders (American Speech-Language-Hearing Association, 2004).
Table 1.
The final 46 items in the item bank with their item parameters, fit statistics and DIF results. The items are listed from highest to lowest item discrimination (slope). The category thresholds show the points on the trait range where there is a boundary between response categories. The fit statistics of χ2 and the significance level are provided. For fit statistics, non-significant results are desired to show that the item is a good fit to the model. Items marked with * are the items with the slightly different item stems as described in Table 1.
| Item | Slope | Category Thresholds | Fit Statistics | Items with DIF | ||||
|---|---|---|---|---|---|---|---|---|
| a | b1 | b2 | b3 | χ2 | Prob_χ2 | 5% beta Δ | 10% beta Δ | |
| Talking with people you know | 3.49 | −2.23 | −1.18 | 0.39 | 96.04 | 0.0600 | ||
| Communicating when you are out in your community (e.g. errands; appointments) |
3.33 | −1.63 | −0.69 | 0.83 | 94.61 | 0.4349 | X | |
| Asking questions in a conversation | 3.23 | −1.88 | −0.71 | 0.55 | 105.66 | 0.1930 | ||
| Having a conversation about a serious topic | 3.21 | −1.52 | −0.58 | 0.58 | 114.61 | 0.3372 | ||
| Starting a conversation with someone you know |
3.21 | −2.06 | −1.33 | 0.03 | 79.19 | 0.5370 | ||
| Communicating in a small group of people | 3.18 | −1.62 | −0.74 | 0.85 | 94.34 | 0.5582 | ||
| Giving personal advice to help a family member or friend |
3.15 | −2.05 | −1.02 | 0.27 | 97.79 | 0.3462 | ||
| Bringing up a new topic in casual conversations |
3.15 | −1.64 | −0.76 | 0.45 | 98.94 | 0.6742 | ||
| Talking with a clerk in a store about a problem with a bill or purchase |
3.10 | −1.38 | −0.55 | 0.67 | 123.61 | 0.1768 | X | |
| Talking with family or friends about something you are planning to do with them |
3.08 | −2.15 | −1.14 | 0.26 | 111.35 | 0.0828 | ||
| Negotiating | 2.98 | −1.18 | −0.33 | 0.89 | 119.97 | 0.3565 | ||
| Communicating with others where and when you choose |
2.93 | −1.57 | −0.67 | 0.72 | 115.08 | 0.3262 | X | |
| Sharing your opinion with family and friends | 2.91 | −1.94 | −0.98 | 0.33 | 95.45 | 0.6377 | ||
| Trying to persuade a friend or family member to see a different point of view |
2.81 | −1.38 | −0.38 | 0.80 | 130.54 | 0.2607 | ||
| Talking to a store clerk who is in a hurry | 2.78 | −1.27 | −0.25 | 0.94 | 133.43 | 0.2256 | X | |
| Talking with people you do NOT know | 2.77 | −1.22 | −0.37 | 0.90 | 125.48 | 0.3473 | X | |
|
*Would your condition interfere with asking for help from a stranger |
2.67 | −1.54 | −0.69 | 0.52 | 145.49 | 0.0498 | X | |
| Getting your turn in a fast-moving conversation |
2.64 | −0.72 | 0.34 | 1.44 | 125.17 | 0.4795 | X | |
| Giving someone DETAILED information | 2.61 | −1.13 | −0.18 | 1.07 | 128.09 | 0.3346 | ||
| Communicating when you need to say something quickly |
2.60 | −0.98 | 0.07 | 1.40 | 146.26 | 0.0840 | X | |
| Comforting a friend or family member | 2.59 | −2.38 | −1.25 | 0.01 | 105.37 | 0.2633 | ||
| Having a long conversation with someone you know about a book, movie, show or sports event |
2.59 | −1.31 | −0.38 | 0.89 | 127.01 | 0.3358 | X | |
| Communicating at social gatherings where you know most of the people |
2.54 | −1.71 | −0.67 | 0.92 | 133.14 | 0.1318 | X | |
| Answering questions from a doctor or health care provider who you know |
2.48 | −2.43 | −1.27 | 0.15 | 103.83 | 0.3497 | ||
| Greeting someone you know at a social gathering |
2.43 | −2.18 | −1.23 | 0.26 | 119.94 | 0.1674 | ||
|
*Would your condition interfere with giving directions to someone who is lost and has asked you for help |
2.42 | −1.47 | −0.54 | 0.84 | 149.10 | 0.1465 | ||
| Making new acquaintances | 2.37 | −1.33 | −0.49 | 0.78 | 127.89 | 0.6329 | X | |
| Communicating in a large group of people | 2.36 | −0.72 | 0.25 | 1.52 | 138.85 | 0.3922 | X | |
| Making small talk | 2.35 | −1.75 | −0.80 | 0.58 | 134.55 | 0.2059 | X | |
|
*Would your condition interfere if you were with someone you knew and needed to ask them for help right away |
2.25 | −2.52 | −1.35 | 0 | 119.37 | 0.1595 | X | |
| Communicating at home | 2.23 | −2.36 | −1.17 | 0.47 | 114.04 | 0.4020 | ||
| Getting your point across when you are upset | 2.21 | −0.83 | 0.27 | 1.37 | 135.00 | 0.6926 | X | |
| Making a witty or funny comment in a conversation |
2.21 | −1.57 | −0.62 | 0.69 | 139.41 | 0.4748 | ||
| Talking with important people in your life about your wishes regarding long-term planning |
2.19 | −1.75 | −0.87 | 0.32 | 161.72 | 0.0516 | ||
| Making a phone call to get information | 2.19 | −1.42 | −0.56 | 0.85 | 156.96 | 0.1845 | X | X |
| Sharing personal feelings with people who are close to you |
2.16 | −1.99 | −0.98 | 0.31 | 152.31 | 0.0702 | ||
| Making comments to family or friends about a TV show or movie you are watching together |
2.13 | −2.19 | −1.10 | 0.46 | 150.54 | 0.0595 | X | |
|
*Would your condition interfere with communicating during an emergency |
2.12 | −1.45 | −0.41 | 0.86 | 144.77 | 0.4669 | X | |
| Visiting with others in a public place (e.g. park, restaurant, sports activity) | 2.10 | −1.56 | −0.34 | 0.93 | 147.87 | 0.4177 | X | |
| Talking about an emotional issue with family or friends |
2.02 | −1.44 | −0.35 | 0.94 | 176.33 | 0.0498 | ||
| Expressing thanks or appreciation | 1.96 | −3.00 | −1.74 | −0.34 | 115.04 | 0.0900 | ||
| Having a conversation while riding in a car | 1.93 | −1.75 | −0.65 | 0.87 | 156.81 | 0.2197 | X | |
| Saying something to get someone’s attention | 1.93 | −1.68 | −0.47 | 0.66 | 179.84 | 0.0545 | X | X |
| Ordering a meal in a restaurant | 1.87 | −2.10 | −1.12 | 0.45 | 133.30 | 0.5013 | X | X |
| Having a conversation in a noisy place | 1.75 | −0.47 | 0.63 | 1.97 | 168.79 | 0.0619 | X | X |
| Taking a phone message | 1.61 | −1.89 | −1.01 | 0.48 | 175.39 | 0.1037 | ||
Items marked with (*) in Table 1 and Appendix A have a slightly different item stem: “Would your condition interfere with….” This modified wording is used for situations that would occur rarely.
Table 2. The Communicative Participation Item Bank – General Short Form and scoring guide. This short form is also available as supplemental material on the journal website.
Instructions: The following questions describe a variety of situations in which you might need to speak to others. For each question, please mark how much your condition interferes with your participation in that situation. By “condition” we mean ALL issues that may affect how you communicate in these situations including speech conditions, any other health conditions, or features of the environment. If your speech varies, think about an AVERAGE day for your speech – not your best or your worst days.
| Not at all (3) |
A little (2) |
Quite a bit (1) |
Very much (0) |
|
|---|---|---|---|---|
| 1. Does your condition interfere with… …talking with people you know? |
〇 | 〇 | 〇 | 〇 |
| 2. Does your condition interfere with… …communicating when you need to say something quickly? |
〇 | 〇 | 〇 | 〇 |
| 3. Does your condition interfere with… …talking with people you do NOT know? |
〇 | 〇 | 〇 | 〇 |
| 4. Does your condition interfere with… …communicating when you are out in your community (e.g. errands; appointments)? |
〇 | 〇 | 〇 | 〇 |
| 5. Does your condition interfere with… …asking questions in a conversation? |
〇 | 〇 | 〇 | 〇 |
| 6. Does your condition interfere with… …communicating in a small group of people? |
〇 | 〇 | 〇 | 〇 |
| 7. Does your condition interfere with… …having a long conversation with someone you know about a book movie, show or sports event? |
〇 | 〇 | 〇 | 〇 |
| 8. Does your condition interfere with… … giving someone DETAILED information? |
〇 | 〇 | 〇 | 〇 |
| 9. Does your condition interfere with… …getting your turn in a fast-moving conversation? |
〇 | 〇 | 〇 | 〇 |
| 10. Does your condition interfere with… …trying to persuade a friend or family member to see a different point of view? |
〇 | 〇 | 〇 | 〇 |
Scoring guide for the CPIB General Short Form.
To score the short form, add the scores for the ten items to obtain a summary score (Not at all = 3; A little = 2; Quite a bit = 1; Very much = 0). The summary score will range from 0 – 30. High scores are more favorable (they indicate less interference in participation). Using the table below, the summary scores can be converted to IRT theta values (logit scale). On the logit scale, scores typically range from −3.0 to +3.0 with 0 logits representing the mean for the calibration sample. Again, high scores are preferable. The table also includes a conversion to standard T scores (mean = 50; standard deviation = 10). VERY IMPORTANT: This score translation table is ONLY valid for the 10-item short form presented in this manuscript. In IRT, the person score is based on the parameters of the individual items administered to that person. This scoring table has been generated using the item parameters for this short form. These parameters would differ for different items. A new score translation table must be created for any other item set. Furthermore, readers should remain aware that summary scores (adding up the points across items) from different item sets cannot be directly compared in a meaningful way, although IRT based (logit) scores can be directly compared between different short forms.
CPIB 10-Item General Short Form Scoring Table
| Summary | Theta | T score |
|---|---|---|
| 0 | −2.58 | 24.20 |
| 1 | −2.18 | 28.20 |
| 2 | −1.94 | 30.60 |
| 3 | −1.76 | 32.40 |
| 4 | −1.60 | 34.00 |
| 5 | −1.46 | 35.40 |
| 6 | −1.34 | 36.60 |
| 7 | −1.22 | 37.80 |
| 8 | −1.10 | 39.00 |
| 9 | −0.99 | 40.10 |
| 10 | −0.89 | 41.10 |
| 11 | −0.78 | 42.20 |
| 12 | −0.67 | 43.30 |
| 13 | −0.56 | 44.40 |
| 14 | −0.45 | 45.50 |
| 15 | −0.33 | 46.70 |
| 16 | −0.22 | 47.80 |
| 17 | −0.10 | 49.00 |
| 18 | 0.03 | 50.30 |
| 19 | 0.15 | 51.50 |
| 20 | 0.27 | 52.70 |
| 21 | 0.40 | 54.00 |
| 22 | 0.53 | 55.30 |
| 23 | 0.65 | 56.50 |
| 24 | 0.78 | 57.80 |
| 25 | 0.92 | 59.20 |
| 26 | 1.06 | 60.60 |
| 27 | 1.22 | 62.20 |
| 28 | 1.42 | 64.20 |
| 29 | 1.67 | 66.70 |
| 30 | 2.10 | 71.00 |
Acknowledgements
This study was made possible by funding from the National Institute for Deafness and other Communication Disorders (NIDCD; 1R03DC010044; PI - Baylor), and from the National Cancer Institute (NCI: 1R03CA132525-01A1; PI- Eadie). The authors would like to thank all of our participants who gave of their time and energy to complete the questionnaires. We also wish to thank all of the individuals who helped us recruit participants including speech-language pathologists and other healthcare providers, staff at the research and education organizations serving the groups represented, and volunteer support group leaders who shared information about the study with clients and group members. Finally, we would like to thank our student research assistants for their efforts in data collection and data entry including Christina Gray, Brittney Skrupky, Devon Sawin, Kristin Lamvik, Kathy Nagle, and Tiffany Elliott.
Appendix A
This table contains the items that were removed from the set of 94 candidate items either due to local dependence (Section A) or poor item fit (Section B).
| A. Items removed due to local dependence (28 items) | |
| Asking a stranger for directions | Having a friendly debate with someone you know |
| Calling out to someone far away from you to get their attention | Having a casual conversation with someone you do NOT know very well |
| Confiding in someone you know well | Having a conversation with the TV or radio on |
| Asking a familiar doctor or health care provider questions | Communicating when there are distractions around you |
| Telling family or friends about your day | Having a heated argument with someone |
| Asking for help from a family member or friend | Asking for help from someone at home |
| Talking on the phone to schedule an appointment (e.g. dentist, car repair) | Communicating in situations and activities that are important to you |
| Having a conversation when you are at a restaurant with a small group of people you know | Starting a conversation at a social gathering with someone you just met |
| Telling a funny story or joke | Introducing yourself to a stranger |
| Telling someone at home what you like and dislike | Having a casual conversation at mealtime at home |
| Communicating with someone who is NOT paying attention to you | Talking to someone who cannot see you (e.g., someone in another room, not facing the other person) |
| Answering the phone | Talking with a customer service person on the phone about a problem with a bill, purchase or service |
| Making a phone call for household business | Leaving a message on someone's phone |
| *Would your condition interfere with giving important information over the phone in an emergency | *Would your condition interfere with asking for help from a stranger when you are in a hurry |
| B. Items removed for poor item fit (20 items) | |
| Having a casual conversation | Resolving conflicts |
| Talking with a clerk in a store while he or she checks out your items | Asking your pharmacist questions about your medicines |
| Giving information to a repair person | Joining a conversation |
| Maintaining relationships with friends | Letting someone know what you need at the store |
| Discussing current events with people you know | Being polite when talking to people |
| Speaking softly in quiet places | Reading out loud to others (e.g., book, newspaper) |
| Telling a story at a social gathering | Telling someone how to do something |
| Talking with people at home about things that need to get done around the house | Talking with someone while you are walking together outside |
| Having a quiet, casual face-to-face conversation with someone you know | Talking about a plan for daily activities with people who help you at home |
| Talking with people when you are tired | Talking to family or friends on the phone |
See explanation in Table 1
Appendix B
Demographic information. Where tallies do not add to the total, the remainder is due to missing data. Missing data tallies were not included in the table to save space.
| MS | PD | HNCA | ALS | Total | |||
|---|---|---|---|---|---|---|---|
|
Enrollment and Completion |
Completed / Enrolled (% completion rate) |
216/304 (71.1%) |
218/318 (68.6%) |
197/240 (82.1%) |
70/139 (50.4%) |
701/1001 (70.0%) |
|
| Format | Online | 156/216 (72.2%) |
123/218 (56.4%) |
123/197 (62.4%) |
56/70 (80.0%) |
458/701 (65.3%) |
|
| Paper | 60/216 (27.8%) |
95/218 (43.6%) |
74/197 (37.6%) |
14/70 (20.0%) |
243/701 (34.7%) |
||
| Age (years) | Mean (SD) Range |
50.0 (9.6) 24–78 |
65.9 (10.0) 43–99 |
61.5 (12.3) 24–86 |
56.4 (10.0) 35–80 |
58.8 (12.4) 24–99 |
|
| Gender | Male | 39/216 (18.1%) |
119/218 (54.6%) |
121/197 (61.4%) |
41/70 (58.6%) |
320/701 (45.7%) |
|
| Female | 176/216 (81.5%) |
99/218 (45.4%) |
76/197 (38.6%) |
29/70 (41.4%) |
380/701 (54.2%) |
||
|
Employment Status (can choose more than one category) |
Full time paid | 44 (20.4%) |
20 (9.2%) |
35 (17.8%) |
7 (10.0%) |
106 (15.1%) |
|
| Part time paid | 21 (9.7%) |
15 (6.9%) |
18 (9.1%) |
3 (4.3%) |
57 (8.1%) |
||
| Home business | 4 (1.9%) |
6 (2.8%) |
8 (4.1%) |
1 (1.4%) |
19 (2.7%) |
||
| Volunteer | 45 (20.8%) |
19 (8.7%) |
30 (15.2%) |
3 (4.3%) |
97 (13.8%) |
||
| Homemaker / Stay at home parent |
18 (8.3%) |
14 (6.4%) |
15 (7.6%) |
2 (2.9%) |
49 (7.0%) |
||
| School / Training | 3 (1.4%) |
2 (0.9%) |
4 (2.0%) |
0 | 9 (1.3%) |
||
| Retired NOT due to medical condition |
8 (3.7%) |
83 (38.1%) |
71 (36.0%) |
12 (17.1%) |
174 (24.8%) |
||
| Not working due to medical condition |
98 (45.4%) |
88 (40.4%) |
56 (28.4%) |
45 (64.3%) |
287 (40.9%) |
||
| Not working – other reasons |
8 (3.7%) |
6 (2.8%) |
8 (4.1%) |
1 (1.4%) |
23 (3.3%) |
||
|
Marital Status |
Married / committed relationship |
158 (73.2%) |
180 (82.6%) |
121 (61.4%) |
56 (80.0%) |
515 (73.5%) |
|
| Single / Divorced / Widowed |
55 (25.5%) |
37 (17.0%) |
74 (37.6%) |
14 (20.0%) |
180 (25.7%) |
||
|
Living Situation |
With family | 176 (81.5%) |
193 (88.5%) |
132 (67.0%) |
61 (87.1%) |
562 (80.2%) |
|
| Alone | 32 (14.8%) |
18 (8.3%) |
60 (30.5%) |
6 (8.6%) |
116 (16.6%) |
||
| Roommate | 4 (1.9%) |
1 (0.5%) |
2 (1.0%) |
0 | 7 (1.0%) |
||
| Assisted Living | 1 (0.5%) |
3 (1.4%) |
0 | 1 (1.4%) |
5 (0.7%) |
||
| Other | 0 | 3 (1.4%) |
2 (1.0%) |
1 (1.4%) |
6 (0.9%) |
||
|
Education Level |
No high school | 1 (0.5%) |
0 | 4 (2.0%) |
0 | 5 (0.7%) |
|
| Some high school | 1 (0.5%) |
0 | 9 (4.6%) |
0 | 10 (1.4%) |
||
| High school graduate |
22 (10.2%) |
17 (7.8%) |
19 (9.6%) |
10 (14.3%) |
68 (9.7%) |
||
| Vocational / technical training |
14 (6.5%) |
7 (3.2%) |
7 (3.6%) |
5 (7.1%) |
33 (4.7%) |
||
| Some college | 59 (27.3%) |
39 (17.9%) |
66 (33.5%) |
14 (20.0%) |
178 (25.4%) |
||
| College graduate | 75 (34.7%) |
74 (33.9%) |
49 (24.9%) |
31 (44.3%) |
229 (32.7%) |
||
| Post-graduate (masters; PhD) |
44 (20.4%) |
81 (37.2%) |
42 (21.3%) |
10 (14.3%) |
177 (25.3%) |
||
|
Geographic Region |
Northeast | 18 (8.3%) |
25 (11.5%) |
32 (16.2%) |
3 (4.3%) |
78 (11.1%) |
|
| South | 96 (44.4%) |
52 (23.9%) |
55 (27.9%) |
22 (31.4%) |
225 (32.1%) |
||
| Midwest | 53 (24.5%) |
22 (10.1%) |
33 (16.8%) |
17 (24.3%) |
125 (17.8%) |
||
| West | 42 (19.4%) |
114 (52.3%) |
54 (27.4%) |
23 (32.9%) |
233 (33.2%) |
||
| Pacific (HI; AK) | 2 (0.9%) |
2 (0.9%) |
0 | 0 | 4 (0.6%) |
||
| Non-USA | 2 (0.9%) |
0 | 21 (10.7%) |
5 (7.1%) |
28 (4.0%) |
||
|
Time since Diagnosis (years) |
Mean (SD) Range |
12.2 (10.1) 1 – 60 |
8.1 (6.2) 0 – 45 |
8.4 (8.1) 0 – 45 |
3.4 (4.7) 0 – 30 |
9.0 (8.4) 0 – 60 |
|
|
History of hearing loss |
No hearing loss | 147 (68.1%) |
138 (63.3%) |
113 (57.4%) |
53 (75.7%) |
451 (64.3%) |
|
| Hearing loss but no use of aids / assistive devices |
62 (28.7%) |
54 (24.8%) |
63 (32.0%) |
15 (21.4%) |
194 (27.7) |
||
| Hearing loss – does use aids /devices |
7 (3.24%) |
24 (11.0%) |
18 (9.1%) |
2 (2.9%) |
51 (7.3%) |
||
|
Other medical conditions |
Presence of other significant medical conditions |
85 (39.4%) |
102 (46.8%) |
90 (45.7%) |
11 (15.7%) |
288 (41.1%) |
|
|
Prior speech pathology services |
Had received prior speech pathology services |
24 (11.1%) |
81 (37.2%) |
119 (60.4%) |
34 (48.6%) |
258 (36.8%) |
|
Appendix C
Self-reported speech severity using the speech item from the ALSFRS-R. Primary communication method for the HNCA participants. Where cells do not add to the total sample size, the remainder is missing data that is not included to save space.
| Self-reported Speech Severity | |||||
|---|---|---|---|---|---|
| MS (n=216) |
PD (n=218) |
HNCA (n=197) |
ALS (n=70) |
Total (n=701) |
|
| Normal | 117 (54.2%) |
32 (14.7%) |
34 (17.3%) |
3 (4.3%) |
186 (26.5%) |
| Sounds different but people understand me | 37 (17.1%) |
40 (18.3%) |
61 (31.0%) |
11 (15.7%) |
149 (21.3%) |
| Sometimes have to repeat words to be understood |
59 (27.3%) |
140 (64.2%) |
92 (46.7%) |
49 (70.0%) |
340 (48.5%) |
| Use gestures, writing or drawing to help people understand my speech |
2 (0.9%) |
6 (2.8%) |
6 (3.0%) |
7 (10.0%) |
21 (3.0%) |
| Not understandable | 0 | 0 | 2 (1.0%) |
0 | 2 (0.3%) |
|
Primary Communication Method for HNCA Participants (n=197) |
|||||
| Natural speech (non-laryngectomy) | 72 (36.6%) | ||||
| Electrolarynx | 36 (18.3%) | ||||
| Esophageal speech | 17 (8.6%) | ||||
| Tracheo-esophageal puncture (TEP) | 64 (32.5%) | ||||
| High-tech AAC device | 0 | ||||
| Writing | 2 (1.0%) | ||||
Contributor Information
Carolyn Baylor, Department of Rehabilitation Medicine, University of Washington.
Kathryn Yorkston, Department of Rehabilitation Medicine, University of Washington.
Tanya Eadie, Department of Speech and Hearing Sciences, University of Washington.
Jiseon Kim, Department of Rehabilitation Medicine, University of Washington.
Hyewon Chung, Department of Education, Chungnam National University, Korea.
Dagmar Amtmann, Department of Rehabilitation Medicine, University of Washington.
References
- American Speech-Language-Hearing Association. Preferred practice patterns for the profession of speech-language pathology. 2004 Retrieved April 20, 2007, from http://www.asha.org/NR/rdonlyres/C589BA8F-5931-48AA-8E02-59CF989DC01F/0/v1PPPSLP.pdf. [PubMed]
- Baylor C, Burns M, Eadie T, Britton D, Yorkston K. A qualitative study of interference with communicative participation across communication disorders in adults. American Journal of Speech-Language Pathology. 2011;20:269–287. doi: 10.1044/1058-0360(2011/10-0084). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylor C, Hula W, Donovan N, Doyle P, Kendall D, Yorkston K. An introduction to Item Response Theory and Rasch models for speech-language pathologists. American Journal of Speech-Language Pathology. 2011;20:243–259. doi: 10.1044/1058-0360(2011/10-0079). [DOI] [PubMed] [Google Scholar]
- Baylor C, Yorkston K, Eadie T, Miller RM, Amtmann D. Developing the Communicative Participation Item Bank: Rasch analysis results from a spasmodic dysphonia sample. Journal of Speech Language and Hearing Research. 2009;52:1302–1320. doi: 10.1044/1092-4388(2009/07-0275). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylor C, Yorkston KM, Eadie TL, Miller R, Amtmann D. Levels of Speech Usage: A self-report scale for describing how people use speech. Journal of Medical Speech-Language Pathology. 2008;16(4):191–198. [PMC free article] [PubMed] [Google Scholar]
- Becker S, Strobl R, Cieza A, Grill E, Harreus U, Tschiesner U. Graphical modeling can be used to illustrate associations between variables describing functioning in head and neck cancer patients. Journal of Clinical Epidemiology. 2011;64:885–892. doi: 10.1016/j.jclinepi.2010.11.010. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Multivariate analysis with latent variables: Causal modeling. Annual Review of Psychology. 1980;31(1):419–456. [Google Scholar]
- Bowen J, Gibbons L, Gianas A, Kraft GH. Patient administered Expanded Disability Status Scale (EDSS-S) 1999 doi: 10.1177/135245850100700311. [DOI] [PubMed] [Google Scholar]
- Brown M, Dijkers MPJM, Gordon WA, Ashman T, Charatz H, Cheng Z. Participation Objective, Participation Subjective: A measure of participation combining outsider and insider perspectives. Journal of Head Trauma Rehabilitation. 2004;19(6):459–481. doi: 10.1097/00001199-200411000-00004. [DOI] [PubMed] [Google Scholar]
- Browne M, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long J, editors. Testing structural equation models. London: Sage; 1993. pp. 136–162. [Google Scholar]
- Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, et al. The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. Journal of the Neurological Sciences. 1999;169:13–21. doi: 10.1016/s0022-510x(99)00210-5. [DOI] [PubMed] [Google Scholar]
- Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH roadmap cooperative group during its first two years. Medical Care. 2007;45(5, Supplement 1):S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen A, Frankowski R, Bishop-Leone J, Hebert T, Leyk S, Lewin J, et al. The development and validation of a dysphagia-specific qualtiy-of-life questionnaire for patients with head and neck cancer: the M.D. Anderson Dysphagia Inventory. Archives of Otolaryngology -Head and Neck Surgery. 2001;127(7):870–876. [PubMed] [Google Scholar]
- Chen W-H, Thissen D. Local dependence indexes for item pairs using item response theory. Journal of Educational and Behavioral Statistics. 1997;22(3):265–289. [Google Scholar]
- Choi SW, Gibbons L, Crane PK. Lordif: An R package for detecting differential item functioning using iterative hybrid ordinal logistic regression / item response theory and Monte Carlo simulations. Journal of Statistical Software. 2011;39(8):1–30. doi: 10.18637/jss.v039.i08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook K, Bombardier C, Bamer A, Choi SW, Kroenke K, Fann JR. Do somatic and cognitive symptoms of traumatic brain injury confound depression screening? Archives of Physical Medicine and Rehabilitation. 2011;92:818–823. doi: 10.1016/j.apmr.2010.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook K, O’Malley KJ, Roddey TS. Dynamic assessment of health outcomes: time to let the CAT out of the bag? Health Services Research. 2005;40(5, Part II):1694–1711. doi: 10.1111/j.1475-6773.2005.00446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane PK, Gibbons L, Jolley L, van Belle G. Differential item functioning analysis with ordinal logistic regression techniques: DIF detect and difwithpar. Medical Care. 2006;44(11 Supplement 3):S115–S123. doi: 10.1097/01.mlr.0000245183.28384.ed. [DOI] [PubMed] [Google Scholar]
- Crane PK, Gibbons L, Ocepek-Weiklson K, Cook K, Cella D, Narasimhalu K, et al. A comparison of three sets of criteria for determining the presence of differential item functioning using ordinal logistic regression. Quality of Life Research. 2007;16(Supplement 1):69–84. doi: 10.1007/s11136-007-9185-5. [DOI] [PubMed] [Google Scholar]
- Crane PK, Van Belle G, Larson EB. Test bias in a cognitive test: differential item functioning in the CASI. Statistics in Medicine. 2004;23(2):241–256. doi: 10.1002/sim.1713. [DOI] [PubMed] [Google Scholar]
- de Champlain AF. A primer on classical test theory and item response theory for assessments in medical education. Medical Education. 2010;44(1):109–117. doi: 10.1111/j.1365-2923.2009.03425.x. [DOI] [PubMed] [Google Scholar]
- DeWalt DA, Rothrock N, Yount S, Stone AA. Evaluation of item candidates: The PROMIS qualitative item review. Medical Care. 2007;45(5, Supplement 1):1–10. doi: 10.1097/01.mlr.0000254567.79743.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan NJ, Kendall D, Young ME, Rosenbek JC. The Communicative Effectiveness Survey: preliminary evidence of construct validity. American Journal of Speech-Language Pathology. 2008;17(4):335–347. doi: 10.1044/1058-0360(2008/07-0010). [DOI] [PubMed] [Google Scholar]
- Doyle PJ, Hula WD, McNeil MR, Mikolic JM, Matthews C. An application of Rasch analysis to the measurement of communicative functioning. Journal of Speech Language and Hearing Research. 2005;48:1412–1428. doi: 10.1044/1092-4388(2005/098). [DOI] [PubMed] [Google Scholar]
- Doyle PJ, McNeil MR, Hula WD, Mikolic JM. The Burden of Stroke Scale (BOSS): validating patient-reported communication difficulty and associated psychological distress in stroke survivors. Aphasiology. 2003;17(3):291–304. [Google Scholar]
- Eadie TL. The ICF: A proposed framework for comprehensive rehabilitation of individuals who use alaryngeal speech. American Journal of Speech-Language Pathology. 2003;12(2):189–197. doi: 10.1044/1058-0360(2003/065). [DOI] [PubMed] [Google Scholar]
- Eadie TL, Yorkston KM, Klasner ER, Dudgeon BJ, Deitz J, Baylor CR, et al. Measuring communicative participation: a review of self-report instruments in speech-language pathology. American Journal of Speech-Language Pathology. 2006;15:307–320. doi: 10.1044/1058-0360(2006/030). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Embretson S, Reise SP. Item Response Theory for Psychologists. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2000. [Google Scholar]
- Flora D, Thissen D. IRTScore. Chapel Hill, NC: L.L. Thurstone Psychometric Laboratory, University of North Carolina at Chapel Hill; 2002. [Google Scholar]
- FDA, editor. Food and Drug Administration. Guidance for Industry: Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims. Silver Springs, MD; 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fries JF, Bruce B, Cella D. The promise of PROMIS: using item response theory to improve assessment of patient-reported outcomes. Clinical and Experimental Rheumatology. 2005;23(Suppl. 39):S53–S57. [PubMed] [Google Scholar]
- Garcia LJ, Laroche C, Barrette J. Work integration issues go beyond the nature of the communication disorder. Journal of Communication Disorders. 2002;35:187–211. doi: 10.1016/s0021-9924(02)00064-3. [DOI] [PubMed] [Google Scholar]
- Gray C, Baylor C, Eadie T, Kendall D, Yorkston K. The Levels of Speech Usage rating scale: comparison of client self-ratings with speech pathologist ratings. International Journal of Language and Communication Disorders. 2012;47(3):333–344. doi: 10.1111/j.1460-6984.2011.00112.x. [DOI] [PubMed] [Google Scholar]
- Greenhalgh J. The applications of PROs in clinical practice: what are they, do they work and why? Quality of Life Research. 2009;18(1):115–123. doi: 10.1007/s11136-008-9430-6. [DOI] [PubMed] [Google Scholar]
- Hartelius L, Elmberg M, Holm R, Lovberg A-S, Nikolaidis S. Living with Dysarthria: Evaluation of a self-report questionnaire. Folia Phoniatrica et Logopedica. 2008;60:11–19. doi: 10.1159/000111799. [DOI] [PubMed] [Google Scholar]
- Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Quality of Life Research. 2009;18:873–880. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogikyan ND, Sethuraman G. Validation of an instrument to measure voice-related quality of life (V-RQOL) Journal of Voice. 1999;13(4):557–569. doi: 10.1016/s0892-1997(99)80010-1. [DOI] [PubMed] [Google Scholar]
- Howe T. The ICF contextual factors related to speech-language pathology. International Journal of Speech-Language Pathology. 2008;10(1–2):27–37. [Google Scholar]
- Howe T, Worrall LE, Hickson LMH. Interviews with people with aphasia: Environmental factors that influence their community participation. Aphasiology. 2008a;22(10):1–29. [Google Scholar]
- Howe T, Worrall LE, Hickson LMH. Observing people with aphasia: Environmental factors that influence their community participation. Aphasiology. 2008b;22(6):618–643. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Jacobson BH, Johnson A, Grywalski C, Silbergleit A, Jacobson G, Benninger MS, et al. The Voice Handicap Index (VHI): Development and validation. American Journal of Speech-Language Pathology. 1997;6:66–70. [Google Scholar]
- Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N. The PDQ-8: development and validation of a short-form Parkinson’s disease questionnaire. Psychology and Health. 1997;12:805–814. [Google Scholar]
- Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An Expanded Disability Status Scale (EDSS) Neurology. 1983;33:1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- Law J, Bunning K, Byng S, Farrelly S, Heyman B. Making sense in primary care: leveling the playing field for people with communication difficulties. Disability and Society. 2005;20(2):169–184. [Google Scholar]
- Law M. Participation in the occupations of everyday life. The American Journal of Occupational Therapy. 2002;56(6):640–649. doi: 10.5014/ajot.56.6.640. [DOI] [PubMed] [Google Scholar]
- Li C, Thissen D, du Toit SHC. IRTPRO. Chicago, IL: SSI International; 2011. [Google Scholar]
- Ma EP-M, Yiu EM-L. Voice activity and participation profile: Assessing the impact of voice disorders on daily activities. Journal of Speech Language and Hearing Research. 2001;44:511–524. doi: 10.1044/1092-4388(2001/040). [DOI] [PubMed] [Google Scholar]
- Murphy J. Perceptions of communication between people with communication disability and general practice staff. Health Expectations. 2006;9:49–59. doi: 10.1111/j.1369-7625.2006.00366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen L, Muthen B. Mplus version 4.2. Los Angeles: 1998. [Google Scholar]
- Nordehn G, Meredith A, Bye L. A preliminary investigation of barriers to achieving patient-centered communication with patients who have stroke-related communication disorders. Topics in Stroke Rehabilitation. 2006;13(1):68–77. doi: 10.1310/5K2W-P6CD-EFDF-8HG4. [DOI] [PubMed] [Google Scholar]
- O’Halloran R, Worrall L, Hickson L. Environmental factors that influence communication between patients and their healthcare providers in acute hospital stroke units: an observational study. International Journal of Language and Communication Disorders. 2011;46(1):30–47. doi: 10.3109/13682821003660380. [DOI] [PubMed] [Google Scholar]
- Orlando M, Thissen D. Likelihood-based item fit indices for dichotomous item response theory models. Applied Psychological Measurement. 2000;24:50–64. [Google Scholar]
- Orlando M, Thissen D. Further investigation of the performance of SX2: An item fit index for use with dichotomous item response theory models. Applied Psychological Measurement. 2003;27:289–298. [Google Scholar]
- Perenboom RJM, Chorus AMJ. Measuring participation according to the International Classification of Functioning, Disability and Health (ICF) Disability and Rehabilitation. 2003;25(11–12):577–587. doi: 10.1080/0963828031000137081. [DOI] [PubMed] [Google Scholar]
- Reeve BB, Hays RD, Bjorner JB, Cook KF, Crane PK, Teresi JA, et al. Psychometric evaluation and calibration of health-related quality of life item banks. Medical Care. 2007;45(5 Suppl 1):S22–S31. doi: 10.1097/01.mlr.0000250483.85507.04. [DOI] [PubMed] [Google Scholar]
- Revicki DA, Cella DF. Health status assessment for the twenty-first century: item response theory, item banking, and computer adaptive testing. Quality of Life Research. 1997;6:595–600. doi: 10.1023/a:1018420418455. [DOI] [PubMed] [Google Scholar]
- Rogers S, Gwanne S, Lowe D, Humphris G, Yueh B, Weymuller EA. The addition of mood and anxiety domains to the University of Washington Quality of Life Scale. Head and Neck. 2002;24(6):521–529. doi: 10.1002/hed.10106. [DOI] [PubMed] [Google Scholar]
- Rosen CA, Lee AS, Osborne J, Zullo T, Murry T. Development and validation of the Voice Handicap Index-10. Laryngoscope. 2004;114(9):1549–1556. doi: 10.1097/00005537-200409000-00009. [DOI] [PubMed] [Google Scholar]
- Samejima F. Estimation of latent ability using a response pattern of graded scores. Psychometrika Monograph, No. 17. 1969 [Google Scholar]
- SPSS. SPSS 17.0 for Windows. Chicago: SPSS, Inc; 2008. [Google Scholar]
- Steiger JH, Lind JC. Statistically-based tests for the number of common factors; Paper presented at the Psychometric Society.1980. [Google Scholar]
- Threats T. Access for persons with neurogenic communication disorders: Influences of personal and environmental factors of the ICF. Aphasiology. 2007;21(1):67–80. [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Weymuller EA, Alsarraf R, Yueh B, Deleyiannis FWB, Coltrera MD. Analysis of the performance characteristics of the University of Washington Quality of Life instrument and its modification (UW-QOL-R) Archives of Otolaryngology - Head and Neck Surgery. 2001;127:489–493. doi: 10.1001/archotol.127.5.489. [DOI] [PubMed] [Google Scholar]
- Whitehill T, Ma EP-M, Tse F. Environmental barriers to communication for individuals with dysarthria. Journal of Medical Speech-Language Pathology. 2010;18(4):141–144. [Google Scholar]
- Whiteneck GG. Measuring what matters: Key rehabilitation outcomes. Archives of Physical Medicine and Rehabilitation. 1994;75:1073–1076. doi: 10.1016/0003-9993(94)90080-9. [DOI] [PubMed] [Google Scholar]
- Willis GB. Cognitive Interviewing: A tool for improving questionnaire design. Thousand Oaks, CA: Sage Publications, Inc; 2005. [Google Scholar]
- World Health Organization. International classification of functioning, disability and health: ICF. Geneva: World Health Organization; 2001. [Google Scholar]
- Yaruss JS, Quesal RW. Overall Assessment of the Speaker’s Experience of Stuttering (OASES): Documenting multiple outcomes in stuttering treatment. Journal of Fluency Disorders. 2006;31:90–115. doi: 10.1016/j.jfludis.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Yorkston K, Baylor C, Deitz J, Dudgeon BJ, Eadie T, Miller RM, et al. Developing a scale of communicative participation: a cognitive interviewing study. Disability and Rehabilitation. 2008;30(6):425–433. doi: 10.1080/09638280701625328. [DOI] [PubMed] [Google Scholar]
- Yorkston K, Baylor C, Klasner ER, Deitz J, Dudgeon BJ, Eadie T, et al. Satisfaction with communicative participation as defined by adults with multiple sclerosis: a qualitative study. Journal of Communication Disorders. 2007;40:433–451. doi: 10.1016/j.jcomdis.2006.10.006. [DOI] [PubMed] [Google Scholar]
- Zraick RI, Atcherson SR, Brown AM. Readability of patient-reported outcome questionnaries for use with persons who stutter. Journal of Fluency Disorders. 2012;37:20–24. doi: 10.1016/j.jfludis.2011.10.004. [DOI] [PubMed] [Google Scholar]