Abstract
Objectives. To investigate the views of parents, clinicians, and children pertaining to prescribing decisions for acute childhood infection in primary care. Methods. A systematic review of qualitative studies. Meta-ethnographic methods were used, with data drawn from the primary studies in an interpretive analysis. Results. A total of 15 studies met the inclusion criteria. The literature was dominated by concerns about antibiotic over-prescription. Children's views were not reported. Clinicians prescribed antibiotics when they felt pressured by parents or others (e.g. employers) to do so, when they believed there was a clear clinical indication, but also when they felt uncertain of clinical or social outcomes they prescribed “just in case”. Parents wanted antibiotics when they felt they would improve the current illness, and when they felt pressure from daycare providers or employers. Clinicians avoided antibiotics when they were concerned about adverse reactions or drug resistance, when certain they were not indicated, and when there was no perceived pressure from parents. Parents also wished to avoid adverse effects of antibiotics, and did not want antibiotics when they would not relieve current symptoms. Some parents preferred to avoid medication altogether. Within paediatric consultations, parents sought a medical evaluation and decision. Primary care clinicians want satisfied parents and short consultations. Conclusions. Antibiotic prescriptions for childhood infections in primary care often result from “just in case” prescribing. These findings suggest that interventions which reduce clinician uncertainty regarding social or clinical outcomes and provide strategies to meet parents’ needs within a short consultation are most likely to reduce antibiotic prescribing.
Key Words: Anti-bacterial agents, child, general practice, primary health care, qualitative research, systematic review, United Kingdom
What is known is that inappropriate medication of childhood infection, particularly overuse of antibiotics, is a concern. Primary care clinicians report feeling pressured by parents to prescribe antibiotics. What this study adds is that:
Clinicians often prescribe antibiotics “just in case”, when they feel uncertain about clinical or social outcomes. In contrast, antibiotics are avoided where there is concern about adverse effects or drug resistance, or where parents do not ask for them.
Parents want prescriptions when they believe they will improve the current illness, but also wish to avoid adverse effects and sometimes have a “no treatment” preference.
Within paediatric consultations, the medical examination in itself is reassuring to parents. Primary care clinicians want satisfied parents, but they also want shorter consultations.
Reducing uncertainty regarding social or clinical outcomes might reduce “just in case” prescribing.
Introduction
Prescription decisions in primary care matter because of the scale of prescribing. In England alone nearly a billion prescriptions were issued by primary care in 2010, of which nearly 50 million were for infections [1]. Over-prescription of antibiotics for self-limiting illness is a significant problem for health services, contributing to drug resistance [2–5] and re- consultation for minor illness [6]. There is particular concern regarding overuse of antibiotics for children with self-limiting illness [7,8]. At the same time, severe infections are sometimes missed by clinicians and prescriptions not issued [9,10]. Similarly, non-specific abdominal pain in childhood is often under-investigated and over-medicated in primary care [11].
The factors that affect the decision to prescribe are likely to be important for determining responses to both over-prescribing and under-prescribing. The views of clinicians and patients (in this case parents and children) will influence the decision to prescribe, and a better understanding of the views of parents, clinicians, and children regarding prescriptions for minor childhood illness in primary care is needed. Findings from individual studies are useful in moving forward knowledge in the field, but qualitative studies by their nature often have restricted sample sizes, offer a view unique to the particular circumstances of included participants, and reflect the particular interpretations of one group of study authors [12]. These qualities are integral to the phenomenological and interpretive approach of qualitative research [13], but can mean it is more difficult to know whether the findings are also likely to be pertinent at another time and place. Systematic reviews (SR) of qualitative studies are useful in synthesizing across studies to find common themes, a broader range of views and experiences, and the bringing together of different viewpoints.
We know of no reviews of the views of both clinicians and parents with regard to the use of prescriptions for any acute minor illness in children. A previous SR considered clinicians’ views regarding the use of antibiotics for respiratory tract infections (RTIs) only and did not focus on children [14]. A SR of parents’ views regarding home care decisions did not focus on prescription medication and needs updating [15].
Our objective was to review the literature on the views, beliefs, and attitudes of parents, children, and prescribing clinicians that influenced prescribing decisions for acute childhood infection in primary care.
Material and methods
We followed Cochrane Qualitative and Implementation Methods Group guidance in the conduct of the review [16], including a broader search strategy than might be usual in systematic reviews of effectiveness studies and use of an expert group including clinicians to guide our methodological decisions.
Search strategy for the identification of studies
Search terms for prescriptions or antibiotics were combined with terms for acute childhood infection, parents or clinicians, and qualitative methods (see Supplemental File). An information specialist developed a pre-planned, comprehensive search strategy in Medline and adapted it for use in other databases. Eight electronic databases were searched for studies published before October 2012: MEDLINE, EMBASE, CINAHL, PsycINFO, SSCI, SIGLE, Dissertation Express databases, and the NHS economic evaluation database. In addition, hand searching was carried out in Social Science and Medicine, Sociology of Health and Illness, British Journal of General Practice, Journal of Family Practice, and Health Expectations, which were identified by our Steering Committee and management group as most likely to publish relevant articles. We used forward citation tracking and screened reference lists of included studies.
Inclusion criteria
Study focus: Studies which considered parent, child, or clinician views, attitudes, beliefs, knowledge, and values in relation to any prescriptions for medicines to treat acute minor childhood illness. Studies with general population samples were included where views towards prescribing for children were included and explicitly reported (and in these cases only data regarding paediatric consultations were extracted).
Design: Studies using qualitative methods (e.g. interviews, focus groups, observations) to collect and analyse data. Studies had to report direct quotes from parents and/or clinicians or themes, concepts, and ideas in analysis to ensure we were identifying empirical, qualitative work (and excluding discussion papers, surveys, and opinion pieces).
Setting: Studies based in or concerning any Primary Health Care settings (including general or family practices and walk-in-centres) in any country belonging to the Organisation for Economic Co-operation and Development and published in any language.
Population: Parents of children aged between three months and 12 years, children in the same age group, and clinicians with authority to prescribe for children in this age group with acute minor illnesses.
Exclusion criteria
(a)Studies that included only quantitative reports of attitudes using closed questions (e.g. surveys). (b) Studies where views were in the context of children with concomitant long-term conditions.
Selection of studies
The title and abstracts of the first 1000 hits were independently screened (using translations where necessary) by two researchers and results were compared and discussed to refine selection criteria in an iterative process. Once double screening was producing no differences in selection, one researcher screened the remainder of all searches. Final selection was undertaken independently by two researchers reviewing full texts of relevant papers.
Data extraction and critical appraisal approach
Data extraction was conducted by two researchers working independently. We assessed study quality considering the primary marker, context sensitivity, sampling strategy, data quality, theoretical adequacy, generalizability, and typicality [17], these judgements are explained and summarized in Table II. We also considered whether any studies were fatally flawed (that is, the quality of the research was judged as so poor that it should not be included) and no studies were excluded on this basis.
Synthesis of findings
We undertook an interpretive analysis, producing a new understanding of the data drawn from the primary studies using meta-ethnographic methods [18]. First order (reflecting participants’ understandings) and second order (reflecting authors’ interpretations) concepts identified from the primary studies were compared across studies, grouping those that were conceptually similar under third-order constructs “translating” the studies into each other. We followed guidance from Noblit & Hare [19] in incorporating the studies in chronological order. The synthesis was an iterative process: third-order constructs were developed in discussion between the researchers, considering reciprocal (where concepts support each other), refutational (where concepts are contested), and line of argument (interpreting across the complete set of constructs) [19].
Results
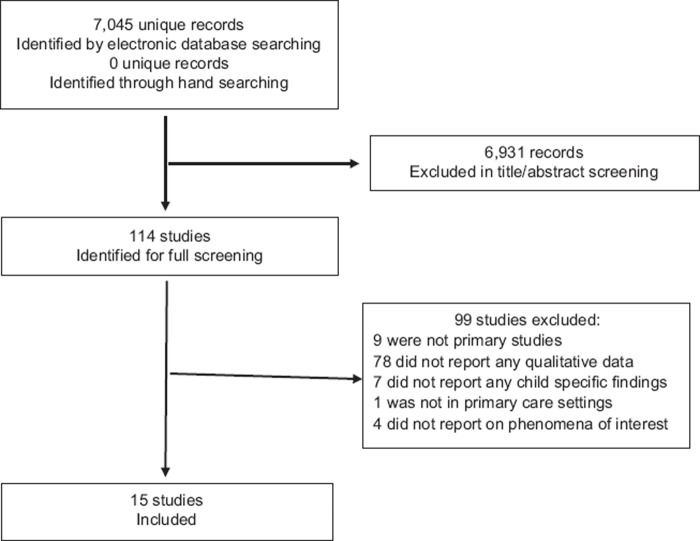
Searches of electronic resources yielded 7045 records of which 114 were retrieved in full text. While most were published in English, 12 were published in other languages. Online translation services together with review by native speakers were used to decide on inclusion. Fifteen studies met our inclusion criteria. Figure 1 shows the flow of studies including reasons for exclusion.
Figure 1.
Flow chart of inclusion. Literature search and study descriptions.
The main features of the included studies are shown in Table I. Six studies were carried out in the UK [20–25], three in Iceland [26–28], two in the USA [29,30], and one each in France [31], Norway [32], and New Zealand [33], while one compared the views of GPs in the UK, France, Poland, Spain, and Belgium regarding interventions to reduce antibiotic use [14]. Five considered patients in primary care with any presentation [25–27,30,33], seven only those with RTIs [14,20–22,29,31,32], two with conjunctivitis [23,24] and one with otitis media [28].
Table I.
Description of included studies (in date order).
| First author, date | Focus on antibiotic prescribing | Location | Parent sample | Clinician sample | Illness | Study focus |
| Clarke 1989 [20] | No | Leeds, UK Urban |
Families | None | RTI & febrile illness | To investigate how parents from different ethnic groups manage their children's RTIs & fevers & their consultation with GPs. Face-to-face interviews |
| Butler 1998 [21] | Yes | Cardiff, UK | 5 mothers | 21 GPs [1–28 years as principles] |
Sore throat | To better understand reasons antibiotics are prescribed for sore throats. Face-to-face interviews |
| Barden 1998 [29] | Yes, and in context of overuse | Atlanta, USA Urban | 29 parents | 22 physicians | URTI | To assess the attitudes and assumptions of physicians and parents regarding antimicrobial use and misuse. Focus groups |
| Elwyn 1999 [22] | Yes, and in context of overuse | Cardiff, UK Urban | 2 mothers 1 father |
1 GP | Tonsillitis | To examine the “shared-decision-making” model in situations of conflict over preferred treatments. Discourse analysis of recorded consultations |
| Arrol 2002 [33] | Yes, and in context of overuse | Auckland, New Zealand Urban | Parents consulting for children | 13 physicians | General | To explore issues and attitudes regarding delayed prescription use from the perspectives of family physicians and patients. Face-to-face interviews |
| Bjornsdottir 2002 [26] | Yes | Iceland Urban & rural | None | 10 GPs | General | This study aims at understanding GPs’ decision-making when deciding whether or not to prescribe antibiotics. Face-to-face interviews |
| Jonsson 2002 [28] | No | Iceland Urban | 17 mothers, 6 fathers | None | Otitis media | To explore the views and feelings of parents of pre-school children with newly diagnosed acute otitis media towards the disease and its diagnosis and treatment. Face-to-face interviews |
| Pradier 2003 [31] | Yes, and in context of overuse | France | 8 groups of parents | 2 groups of GPs 1 group of paediatricians 2 groups of pharmacists |
Feverish nasopharyngitis | To explore ways of modifying attitudes and behaviours of doctors (GPs and paediatricians), parents, and pharmacists towards the over-prescription of antibiotics. Focus groups |
| Everitt 2003 [23] | Yes | UK | 11 mothers | None | Conjunctivitis | To explore patients’ understanding of conjunctivitis and its management. Face-to-face interviews |
| Petursson 2005 [27] | Yes, and in context of overuse | Iceland Urban & rural | None | 16 GPs | General | To explore reasons given by Icelandic GPs for non-pharmacological prescribing. Face-to-face interviews |
| Larson 2006 [30] | Yes | New York, USA Urban |
25 mothers | 3 health care professionals 2 pharmacy employees |
General | To describe the knowledge, attitudes, beliefs, and practices of Latino community members regarding the use of antibiotics. Focus groups |
| Rose 2006 [24] | Yes, and in context of overuse | Sheffield & Berkshire, UK | None | 39 GPs | Conjunctivitis | To investigate the non-clinical determinants of the management of acute infective conjunctivitis in children. Telephone interviews |
| Hawkings 2008[25] | Yes | South Wales, UK | Adults, of whom 9 were mothers | None | General | To achieve a deeper understanding of the use of antibiotics in the community. Face-to-face interviews |
| Hoye 2010 [32] | Yes, and in context of overuse | Norway | None | 33 GPs | RTIs | To explore Norwegian GPs’ views and experiences of delayed antibiotic prescribing in patients with URTIs. Focus groups |
| Tonkin-Crine 2011 [14] | Yes, and in context of overuse | UK, France, Poland, Spain, Belgium | None | 52 GPs | RTIs | To elicit GPs’ views on strategies for antibiotic prescribing. Face-to-face and telephone interviews |
More than 300 individuals, including 86 mothers, 15 fathers, and 207 clinicians (usually GPs), were included in these studies (sample sizes were not always reported for specific participant groups). Six studies included the views of parents and clinicians [21,22,29–31,33], five those of clinicians only [14,24,26,27,32], and four those of parents only [20,23,25,28]. No study included the views of children. Study appraisals are presented in Table II.
Table II.
Study appraisal.
| First author, date | Primary marker: Is the aim of the research to explore subjective meanings of experience? |
Context sensitivity: Is the research design sensitive to the context in which study takes place? |
Sampling strategy: Is the sampling strategy described appropriate and informed by theory or context? |
Data quality: Are different sources of knowledge/understanding compared? |
Theoretical adequacy: Is process from theory to interpretation explicit? |
Generalizability and typicality: What claims are being made, and do they follow from the data? |
| Clarke 1989 [20] | Partly satisfied | Partly satisfied | Unclear | Partly satisfied | Satisfied | Satisfied |
| Butler 1998 [21] | Satisfied | Unclear | Satisfied | Satisfied | Satisfied | Satisfied |
| Barden 1998 [29] | Satisfied | Unclear | Unclear | Satisfied | Not satisfied | No claims |
| Elwyn 1999 [22] | Partly satisfied | Unclear | Satisfied | Partly satisfied | Satisfied | No claims |
| Arrol 2002 [33] | Satisfied | Unclear | Satisfied | Satisfied | ? | No claims |
| Bjornsdottir 2002 [26] | Satisfied | Unclear | Unclear | Satisfied | Satisfied | Satisfied |
| Jonsson 2002 [28] | Satisfied | Unclear | Satisfied | Satisfied | Satisfied | Unclear |
| Pradier 2003 [31] | ? | Unclear | Unclear | Satisfied | Not satisfied | Unclear |
| Everitt 2003 [23] | Satisfied | Unclear | Satisfied | Partly satisfied | Not satisfied | Satisfied |
| Petursson 2005 [27] | Satisfied | Unclear | Satisfied | Partly satisfied | Satisfied | No claims |
| Larson 2006 [30] | Satisfied | Unclear | Satisfied | Satisfied | Satisfied | Satisfied |
| Rose 2006 [24] | Partially satisfied | Unclear | Satisfied | Satisfied | Unclear | Not satisfied |
| Hawkings 2008 [25] | Satisfied | Satisfied | Satisfied | Unclear | Satisfied | Satisfied |
| Hoye 2010 [32] | Satisfied | Unclear | Unclear | Satisfied | Unclear | Satisfied |
| Tonkin-Crine 2011 [14] | Satisfied | ? | Satisfied | Satisfied | Not satisfied | Satisfied |
Studies were published between 1998 and 2011, and only two earlier studies [20,28] did not focus only on prescriptions for antibiotics (see study focus Table I). Thirteen asked specifically about antibiotic treatment, of which eight set this within the context of over-prescribing. This context influenced design, data collection, and analysis – for example, by including questions about perceptions of overprescribing [29], or by purposively sampling and comparing high and low prescribers [33]. Therefore findings reported here often concern antibiotic prescribing only.
Synthesis
Figure 2 provides an example of the process of identifying and translating constructs. Constructs emerged relating to beliefs and behaviours that influenced preferences and decisions regarding prescription of antibiotics for both parents and clinicians, along with consultation needs. These constructs are summarized in Table III, separated into views and perceptions that trigger a decision to prescribe, support a decision not to prescribe, and consultation needs for each of clinicians and parents.
Figure 2.
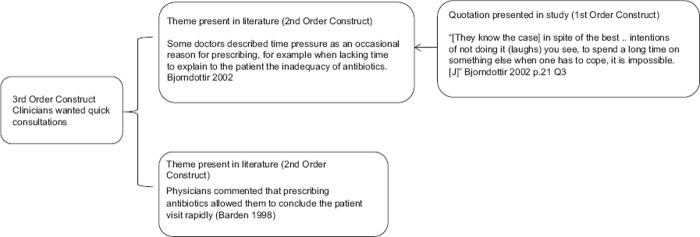
Examples of third-order development.
Table III.
Factors influencing prescription decision (third-order constructs).
| Influence on | Third order construct | Supporting sub themes |
| Clinician factors supporting decisions to prescribe | Just in case | Non-treatment is too risky where there is uncertainty about the consequences of not prescribing, uncertainty about a parent’s ability to cope, uncertainty about diagnosis [24,27] |
| Pressures from outside the consulting room | US based clinicians said incentives & free samples from pharmaceutical industry encouraged prescription [29] Requirement to end consultation quickly [26,29] Pressure to give antibiotics to allow return to work or daycare [24,26] Clinicians believed that use of day care and other group exposures were a major cause of antibiotic overuse because it led to frequent infections [29] |
|
| Clinically indicated | A green nasal discharge indicated antibiotics were needed [29] Antibiotic prescription can reduce parental anxiety [24,27,28,33] |
|
| Perceived pressure from parents | Potential for litigation, repeat consultations, visits to other doctors, late night calls, [14,29,31] To increase patient satisfaction and reinforce the doctor-patient relationship [29,31,14] Prescribing was ‘less stressful’ for the clinician than an ‘anxious and angry’ parent. [28, 33, 24, 27] Potential for litigation, repeat consultations, visits to other doctors, late night calls, [14, 29, 31] Clinicians felt that parental expectations for antibiotics was the principle factor that influenced them to prescribe antibiotics when not needed [27, 29] |
|
| Parent factors supporting decisions to prescribe | Prescription is needed | A minority of parents believed antibiotics would resolve symptoms and avoid repeat consultations and that they were needed when home management failed [21, 22, 29, 23, 24, 28] Because the current illness is bacterial [29] |
| External pressures | From day care providers/school or employment demands [22,23,29] | |
| Clinicians factors supporting decisions not to prescribe | Concern about adverse outcomes | Concern about adverse outcomes [22] |
| Lack of pressure to prescribe | Lack of perceived parental pressure [26,29,32] | |
| Certainty a prescription not needed | Near patient tests provided certainty a prescription is not needed [14] | |
| Concern about over prescription | Belief that they or their practice colleagues already overprescribe [29,31] | |
| Parent factors supporting decisions not to prescribe | No-intervention preference | Preference for a no-intervention approach [21,23,25,30] |
| Concern about side effects | Concern about adverse outcomes [22,23,25,28,29] | |
| Do not believe will be helpful | Belief the prescription will not improve symptoms [20,21] | |
| Clinician consultation needs | A good consultation | A good consultation is one which is quickly completed, and both parents and clinician are satisfied [24,29] |
| Parent education | To educate parents about illness/treatment [21, 29] | |
| Parent consultation needs | A medical assessment | A medical evaluation and medical information [20,23,28,29,31] |
| A necessary appointment | Don't want to “bother” the doctor unnecessarily [22] | |
| “Appropriate“ treatment | To receive “appropriate” treatment as recommended by a doctor [20–23,29,31] | |
| A medical decision | A medical decision (which could be that no treatment was necessary) [21,23,29,20,21,33] |
Views and perceptions that trigger a decision/preference to prescribe
Four factors triggered decisions to prescribe among clinicians: perceived pressure from parents; perceived pressure from outsider the consulting room, a belief they should be prescribed “just in case“; and where clinicians believed they were clearly indicated. Perceived pressure from parents was reported as the principle reason to prescribe in several studies [14,27,29], although this did not necessarily imply a stated expectations or desire. This perceived pressure could also result from parental anxiety [24,27,28,33], fear of litigation, and concern for the consequences for the doctor–patient relationship (including re-consultation). Perceived external pressure came from educators, employers [24,26,29], and in the US study from drugs companies [29]. The only clear indications for prescribing antibiotics given by clinicians in these studies was “green nasal discharge” [29] and as a “treatment” for high parental anxiety. In addition to these positive decisions to prescribe, there were a number of contexts within which clinicians prescribed “just in case”. Where they felt over-prescription was not a problem, or not a problem for them (e.g. located in secondary care) they felt there was no reason not to prescribe [29]. Where clinicians felt uncertain of the consequences of not prescribing they would also sometimes prescribe. This occurred both where diagnosis was unclear, and also where they were uncertain that parents could manage the illness themselves, particularly where there was no continuity of care so doctor and parent did not know each other [27].
Two factors drove parents to certainly want a prescription. In line with clinician reports, some parents reported that pressure from daycare providers and employers meant they wanted antibiotics to reduce the risk of absence, or to reduce the risk of infection [22,23,29]. Parents also wanted antibiotics where they believed they were efficacious for their child's current illness: they would improve the severity or duration of symptoms including pain [22,24,28,29], reduce the likelihood they would need to return to the doctor [22,29], or in one study that conjunctivitis would persist and be transmitted to others without treatment [23].
Views and perceptions that support a decision/preference not to prescribe
Concerns regarding adverse effects and antibiotic resistance discouraged clinicians from prescribing [22], as did concerns regarding over-prescription in general [29,31]. Where clinicians did not feel there was pressure from parents to give a prescription, this enabled them to avoid prescribing antibiotics [26,29,32]. GPs in France and Poland used near-patient tests to reduce uncertainty concerning diagnosis [14].
A “no treatment” preference among parents was reported in several studies and this decreased demand for antibiotics. Parents wanted to monitor their child's illness, and were happy to hear that antibiotics were not required [21,23,25,30]. For some, resistance to prescriptions was explicitly linked to concerns about harmful effects of antibiotics or medicines in general [23,25,28] and to fears that antibiotics would produce resistance within their own child and thus he/she would not benefit from future treatment [25,28,29]. Some parents in one study reported deliberately limiting consumption of prescribed antibiotics [25]. Parents could feel unhappy when they received antibiotics but not the reassurance or information they wanted, or if the symptoms they were concerned about (e.g. pain) were not addressed [20,21].
Consultation needs
Some of the factors influencing decisions to prescribe related to the consultation needs of parents and clinicians as described in this group of studies. Where the needs of these two parties were at odds, this seemed to feature in antibiotic prescribing decisions. Parent needs were threefold; they wanted a medical examination and evaluation [20,23,28,29], they wanted a medical decision [14,20–33], and finally (depending on this decision) they wanted appropriate treatment [20–23,29,31]. Importantly, where they felt they had received a good evaluation parents were happy to accept clinicians’ advice and decisions even where this differed from their expectations. They trusted the clinicians’ greater knowledge of the problems they were experiencing. Clinicians needed a consultation that was quickly completed and where both parents and clinician were satisfied with the outcome [24,29]. They also wanted to educate parents to understand that antibiotics were not necessary [21,29], but found this difficult to achieve [21]. The pressure to keep consultations short meant some gave in order to bring consultations to a rapid conclusion [26,29].
Discussion
Principal findings
Across these studies clinicians described limited occasions when they were certain about the prescription decision (either to prescribe or not to prescribe). More often, clinicians reported prescribing when uncertainty existed either because of the lack of diagnosis, or uncertainty regarding the social, health, or legal consequences of not prescribing and therefore took a “just in case” approach. Clinicians also report prescribing under pressure, when factors other than clinical presentation (parents, employers, drugs companies, time for consultation) pushed them into prescribing. All of these factors increased the likelihood they would prescribe, even when they did not believe antibiotics were clinically indicated. Some parents wanted a prescription because they believed it would improve their child's illness. But parents were also concerned to get appropriate advice or treatment for their child, and some preferred to avoid medicines if possible. Parents sought a thorough medical assessment from a doctor they trusted, and were satisfied with treatment decisions which differed from their expectations where this was the case.
Strengths and weaknesses of the study
This review is the first to consider the views of both parents and primary care clinicians regarding all prescriptions for minor acute childhood infection. The scope of this review is wide, which resulted in a diffuse search strategy but also enabled us to include the views of a large number of people from diverse contexts, and to draw on unpublished work and papers published in languages other than English.
One of the strengths of a systematic approach to reviewing is in the ability to comment on what is absent, as well as what is present in the literature. We noted that no studies included the views of children, and this is a weakness of the literature. Further, we noted that the literature was dominated by concerns about over-prescribing of antibiotics. The means there is a focus on clinicians’ perceptions regarding those occasions when they prescribe despite believing they are probably not clinically indicated. We do not know about those cases where clinicians believe they have made a clinically sound decision (either to prescribe or not) [34], so we cannot comment on whether or how these would differ.
In common with other reviews of qualitative research, in pooling findings across studies and methods we lose contextual details that may have relevance in understanding our findings. Our search strategy may have missed studies of interest where they did not mention words relating to prescriptions.
Comparison with literature
Previous studies have shown that parents do not always get what they need from primary care consultations. Reports suggest parents leave consultations with insufficient information on diagnosis and treatment options and feeling uncertain [35,36], and that poor clinical assessments and lack of access to health care contribute to hospitalization for RTI [10]. Our review suggests this dissatisfaction might arise when parents’ desire for a thorough medical evaluation conflicts with a clinician's desire for a speedy consultation or when it is interpreted by clinicians as anxiety or demands for antibiotics. Parental anxiety about child illness has been shown to increase the frequency of consultations and antibiotic use [37], but requests for medical evaluations and statements of concerns by parents may be misinterpreted as requests for treatment [27,38,39].
A recent study would agree with our findings. Brookes-Howell and colleagues considered parent satisfaction with prescribing decisions in four European countries. In 50 of the 63 cases examined, parents were satisfied with the prescription decision and their reasons were similar to those reported here: beliefs that particular symptoms needed antibiotics, that antibiotics were efficacious, and, in contrast, that medication should be avoided if possible. In common with our review, the authors note that parents are often ready to accept clinician decisions, even when they disagree with them, but that trust and open communication within the consultation are key to achieving this [40].
Meaning of the study
This review suggests that clinicians prescribe antibiotics “just in case” when faced with clinical uncertainty. This is important, because exhortations not to prescribe will not address this uncertainty. It is not certain which cases may develop complications and require hospitalization, or whether individual children might benefit from antibiotics [9,10,41].
This review further suggests that parental concerns or desire for a medical evaluation may be misinterpreted as a demand for medical treatment (a prescription), and that some parents prefer not to use medication for their children. It is important that clinicians check and address parental concerns, as this may reduce the perceived pressure to prescribe.
Good medicine includes emotional as well as clinical care [42] and guidance that clinicians explicitly address parental concerns already exists [43]. The findings of this study suggest how clinicians might better present responses to these. First, information on the natural history of an illness should respond to parents’ desire for information that is specific to this child on this occasion. Second, the physical examination in itself may be important for reassuring parents.
Acknowledgements
This paper summarizes independent research funded by the National Institute for Health Research (NIHR) under its Programme Grant for Applied Research (Grant Reference Number RP-PG-0608-10018). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
The authors would like to thank all authors of studies included in this review, Jo Abbot for assistance with database searches, and Debbie Allnock and Audrey Leonel for assistance with data extraction and translation.
This research on which this paper is based is part of the TARGET programme. The authors would like to thank the whole team, all have whom contribute to the research programme. The TARGET team consists of: Alastair D. Hay, Andrew Lovering, Brendan Delaney, Christie Cabral, Hannah Christensen, Hannah Thornton, Jenny Ingram, Jeremy Horwood, John Leeming, Margaret Fletcher, Matthew Thompson, Niamh Redmond, Patricia Lucas, Paul Little, Peter Blair, Peter Brindle, Peter Muir, Sandra Hollinghurst, Sue Mulvenna, Talley Andrews, and Tim Peters.
Declaration of interest
There are no conflicts of interest in connection with the paper. The authors alone are responsible for the content and writing of the paper.
References
- 1.The Health and Social Care Information Centre . Prescription cost analysis England 2010. Prescription items dispensed in the community in England and listed alphabetically within chemical entity by therapeutic class. Leeds: Health and Social Care Information Centre, Prescribing Support Unit; 2011. [Google Scholar]
- 2.Davies SC. Annual report of the Chief Medical Officer, Vol. 2, 2011: Infections and the rise of antimicrobial resistance. London: Department of Health; 2013. [DOI] [PubMed] [Google Scholar]
- 3.Committee SMA. The path of least resistance. London: Department of Health; 1998. [Google Scholar]
- 4.Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: Systematic review and meta-analysis. BMJ. 2010;340:c2096. doi: 10.1136/bmj.c2096. [DOI] [PubMed] [Google Scholar]
- 5.Kessel AS, Sharland M. The new UK antimicrobial resistance strategy and action plan. BMJ. 2013;346:f1601. doi: 10.1136/bmj.f1601. [DOI] [PubMed] [Google Scholar]
- 6.Little P, Gould C, Williamson I, Warner G, Gantley M, Kinmonth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: The medicalising effect of prescribing antibiotics. BMJ. 1997;315:350–2. doi: 10.1136/bmj.315.7104.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vinson DC, Lutz LJ. The effect of parental expectations on treatment of children with a cough: A report from ASPN. J Fam Pract. 1993;37:23–7. [PubMed] [Google Scholar]
- 8.Mangione-Smith R, McGlynn EA, Elliott MN, Krogstad P, Brook RH. The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatr. 1999;103:711–18. doi: 10.1542/peds.103.4.711. [DOI] [PubMed] [Google Scholar]
- 9.Grant CC, Harnden A, Mant D, Emery D, Coster G. Why do children hospitalised with pneumonia not receive antibiotics in primary care? Arch Dis Child. 2012;97:21–7. doi: 10.1136/archdischild-2011-300604. [DOI] [PubMed] [Google Scholar]
- 10.Francis NA, Crocker JC, Gamper A, Brookes-Howell L, Powell C, Butler CC. Missed opportunities for earlier treatment? A qualitative interview study with parents of children admitted to hospital with serious respiratory tract infections. Arch Dis Child. 2011;96:154–9. doi: 10.1136/adc.2010.188680. [DOI] [PubMed] [Google Scholar]
- 11.Gieteling MJ, Lisman-van Leeuwen Y, van der Wouden JC, Schellevis FG, Berger MY. Childhood nonspecific abdominal pain in family practice: Incidence, associated factors, and management. Ann Fam Med. 2011;9:337–43. doi: 10.1370/afm.1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mills E, Jadad AR, Ross C, Wilson K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. J Clin Epidemiol. 2005;58:1081–8. doi: 10.1016/j.jclinepi.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Ormston R, Spencer L, Barnard M, Snape D. The foundations of qualitative research. In: Ritchie J, Lewis J, McNaughtonNicholls C, Ormston R, editors. Qualitative research practice: A guide for social science students and researchers. 2nd ed. London: Sage; 2014. pp. 1–23. [Google Scholar]
- 14.Tonkin-Crine S, Yardley L, Coenen S, Fernandez-Vandellos P, Krawczyk J, Touboul P, et al. GPs’ views in five European countries of interventions to promote prudent antibiotic use. Br J Gen Pract. 2011;61:e252–61. doi: 10.3399/bjgp11X572445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neill SJ. Acute childhood illness at home: The parents’ perspective. J Adv Nurs. 2000;31:821–32. doi: 10.1046/j.1365-2648.2000.01340.x. [DOI] [PubMed] [Google Scholar]
- 16.Noyes J, Lewin S. Extracting qualitative evidence. In: Noyes J, Booth A, Hannes K, Harden A, Harris J, Lewin S, et al., editors. Supplementary guidance for inclusion of qualitative research in Cochrane Systematic Reviews of Interventions Version 1: Cochrane Collaboration Qualitative Methods Group. 2011. Chapter 5. [Google Scholar]
- 17.Popay J, Rogers A, Williams G. Rationale and standards for the systematic review of qualitative literature in health services research. Qual Health Res. 1998;8:341–51. doi: 10.1177/104973239800800305. [DOI] [PubMed] [Google Scholar]
- 18.Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12:181. doi: 10.1186/1471-2288-12-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Noblit G, Hare R. Meta-ethnography: Synthesising qualitative wtudies. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 20.Clarke A. Parental health beliefs and respiratory illness consultations at general practitioners, in multiethnic and multicultural areas. Leeds: University of Leeds; 1989. [Google Scholar]
- 21.Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: Qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ. 1998;317:637–42. doi: 10.1136/bmj.317.7159.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elwyn G, Gwyn R, Edwards A, Grol R. Is “shared decision-making” feasible in consultations for upper respiratory tract infections? Assessing the influence of antibiotic expectations using discourse analysis. Health Expect. 1999;2:105–17. doi: 10.1046/j.1369-6513.1999.00045.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Everitt H, Kumar S, Little P. A qualitative study of patients’ perceptions of acute infective conjunctivitis. Brit J Gen Pract. 2003;53:36–41. [PMC free article] [PubMed] [Google Scholar]
- 24.Rose PW, Ziebland S, Harnden A, Mayon-White R, Mant D, Oxford Childhood Infection Study Group Why do general practitioners prescribe antibiotics for acute infective conjunctivitis in children? Qualitative interviews with GPs and a questionnaire survey of parents and teachers. Fam Pract. 2006;23:226–32. doi: 10.1093/fampra/cmi101. [DOI] [PubMed] [Google Scholar]
- 25.Hawkings NJ, Butler CC, Wood F, Petursson P, Jonsson H, Haraldsson RH. Antibiotics in the community: A typology of user behaviours. Patient Educ Couns. 2008;73:146–52. doi: 10.1016/j.pec.2008.05.025. doi: 10.1016/j.pec.2008.05.025. Epub Jul 21. [DOI] [PubMed] [Google Scholar]
- 26.Bjornsdottir I, Hansen EH. Intentions, strategies and uncertainty inherent in antibiotic prescribing. Eur J Gen Pract. 2002;8:18–24. [Google Scholar]
- 27.Petursson P, Jonsson H, Haraldsson RH. GPs’ reasons for “non-pharmacological” prescribing of antibiotics: A phenomenological study. Scand J Primary Health Care. 2005;23:120–5. doi: 10.1080/02813430510018491. [DOI] [PubMed] [Google Scholar]
- 28.Jonsson H, Haraldsson R. Parents’ perspectives on otitis media and antibiotics: A qualitative study. Scand J Primary Health Care. 2002;20:35–9. doi: 10.1080/028134302317282725. [DOI] [PubMed] [Google Scholar]
- 29.Barden LS, Dowell SF, Schwartz B, Lackey C. Current attitudes regarding use of antimicrobial agents: Results from physicians’ and parents’ focus group discussions. Clin Pediatr. 1998;37:665–71. doi: 10.1177/000992289803701104. [DOI] [PubMed] [Google Scholar]
- 30.Larson EL, Dilone J, Garcia M, Smolowitz J. Factors which influence Latino community members to self-prescribe antibiotics. Nurs Res. 2006;55:94–102. doi: 10.1097/00006199-200603000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Pradier C, Dunais B, Ricort-Patuano C, Maurin S, Andreini A, Hofliger P, et al. The “Antibiotics Only When Necessary (C)” campaign and its implementation in the French Alpes-Maritimes subdivision. Médecine et Maladies Infectieuses. 2003;33:9–14. [Google Scholar]
- 32.Hoye S, Frich J, Lindboek M, Hawkings NJ, Butler CC, Wood F, et al. Delayed prescribing for upper respiratory tract infections: A qualitative study of GPs’ views and experiences. Brit J Gen Pract. 2010;60:907–12. doi: 10.3399/bjgp10X544087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arroll B, Kenealy T. Antibiotics for the common cold and acute purulent rhinitis. Cochrane Database of Systematic Reviews. 2005;((3)) doi: 10.1002/14651858.CD000247.pub2. [DOI] [PubMed] [Google Scholar]
- 34.Elstein AS, Schwartz A. Clinical problem solving and diagnostic decision making: Selective review of the cognitive literature. BMJ. 2002;324:729–32. doi: 10.1136/bmj.324.7339.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kai J. What worries parents when their preschool children are acutely ill, and why: A qualitative study. BMJ. 1996;313:983–6. doi: 10.1136/bmj.313.7063.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Akici A, Kalaca S, Ümit Ugurlu M, Oktay S. Prescribing habits of general practitioners in the treatment of childhood respiratory-tract infections. Eur J Clin Pharmacol. 2004; 60:211–16. doi: 10.1007/s00228-004-0749-9. [DOI] [PubMed] [Google Scholar]
- 37.Malin A, Hedinb K, Håkansson A, Mölstad S, Rodhea N, Peterssonb C. More physician consultations and antibiotic prescriptions in families with high concern about infectious illness: Adequate response to infection prone child or self-fulfilling prophecy? Fam Pract. 2007;24:302–7. doi: 10.1093/fampra/cmm016. [DOI] [PubMed] [Google Scholar]
- 38.Kumar S, Little P, Britten N. Why do general practitioners prescribe antibiotics for sore throat? Grounded theory interview study. BMJ. 2003;326:138. doi: 10.1136/bmj.326.7381.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Altiner A, Knauf A, Moebes J, Sielk M, Wilm S. Acute cough: A qualitative analysis of how GPs manage the consultation when patients explicitly or implicitly expect antibiotic prescriptions. Fam Pract. 2004;21:500–6. doi: 10.1093/fampra/cmh505. [DOI] [PubMed] [Google Scholar]
- 40.Brookes-Howell L, Wood F, Verheij T, Prout H, Cooper L, Hood K, et al. Trust, openness and continuity of care as key ingredients for acceptance of antibiotic prescribing decisions for children with RTIs: A four-country, primary care qualitative study. Fam Pract. 2013;3:102–10. doi: 10.1093/fampra/cmt052. [DOI] [PubMed] [Google Scholar]
- 41.Harnden A, Perera R, Brueggemann AB, Mayon-White R, Crook DW, Thomson A, et al. Respiratory infections for which general practitioners consider prescribing an antibiotic: A prospective study. Arch Dis Child. 2007;92:594–7. doi: 10.1136/adc.2007.116665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Di Blasi Z, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: A systematic review. Lancet. 2001;357:757–62. doi: 10.1016/s0140-6736(00)04169-6. [DOI] [PubMed] [Google Scholar]
- 43.NICE . Respiratory tract infections – antibiotic prescribing: Prescribing of antibiotics for self-limiting respiratory tract infections in adults and children in primary care. London: National Institute for Health and Clinical Excellence; 2008. [PubMed] [Google Scholar]