A 26-year-old male was referred from elsewhere for the evaluation of oral ulcers, joint pains, renal failure and had already received 2 weeks of oral prednisone. His immunological evaluation showed positive anti nuclear and anti-double-stranded antibodies. Renal histology at our hospital was suggestive of diffuse proliferative lupus glomerulonephritis and the patient was put on oral prednisone (1 mg/kg/day) and received the first dose of pulse cyclophosphamide (CYP) therapy (750 mg intravenous).
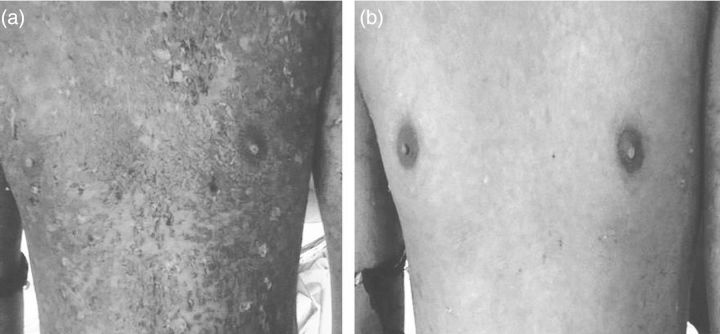
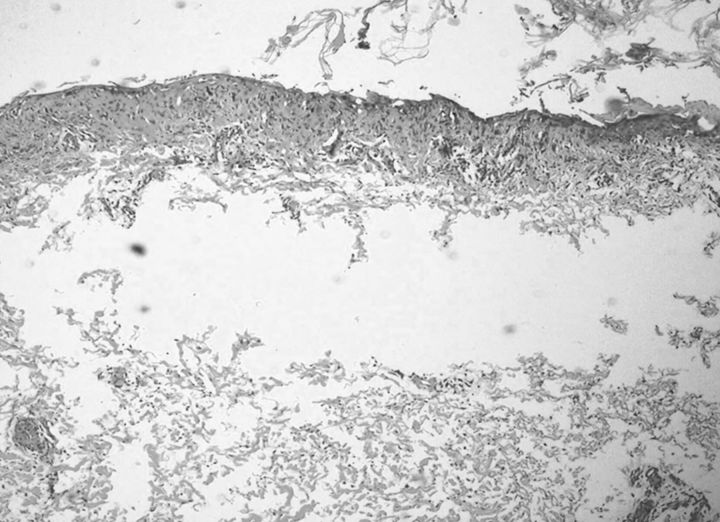
After 5 days of CYP therapy, he started complaining of generalized skin rash in the form of irregular erythematous eruptions with multiple scattered blisters all over the trunk, back and upper limbs (Figure 1a). At the time of admission to the isolation unit, he had moderate fever, signs of dehydration and pain around the skin lesions with marked sloughing, and laboratory work-up showed leukocytosis with normal renal parameters. Clinical evaluation revaeled positive Nikolsky's sign on the trunk and back, but mucous membranes were not involved. He was managed with intravenous fluids, proper wound care and started on amoxicillin–clavulinate until blood and urine cultures were negative. Biopsy from the skin lesions showed epidermal cell necrosis with detachment of the dermis from epidermis (Figure 2), and skin immuno-fluorescence was negative. That suggested a diagnosis of toxic epidermal necrolysis (TEN) with more than 30% of skin involvement and he was started on oral cyclosporine as an immunosuppressive therapy and continued the prednisone. One week of cyclosporine treatment resulted in a dramatic improvement in the skin lesions (Figure 1b), and the general condition of the patient improved as well.
Fig. 1.
(a) Skin lesions over trunk showing erythematous eruptions with extensive epidermal destruction and scattered blisters. (b) Complete improvement of skin lesions after cyclosporine treatment.
Fig. 2.
Histology from the skin lesions (H/E stain) showing epidermal cell necrosis with detachment of dermis from epidermis.
TEN is a rare but disastrous condition that commonly occurs as an idiosyncratic reaction to drugs like sulfonamides, antiepileptics, quinolones, allopurinol and anti-inflammatory drugs [1, 2]. It is thought to be an immune-related drug eruption leading to severe epidermal loss and associated with significant morbidity and mortality secondary to sepsis. Such aggressive skin eruptions have not been described with CYP [3]. In our case, blistering lesions along with full thickness epidermal destruction and necrosis developing after 5 days of CYP therapy suggests that it was the culprit drug as no other drug was incriminated from clinical history. The lesions differ from skin manifestation of lupus, and immuno fluorescence microscopy was also negative. The early use of cyclosporine and proper wound care resulted in significant improvement of the skin lesions [4]. Although CYP-induced TEN is an extremely rare event, from this case, we want to sensitize treating physicians regarding the occurrence of TEN following CYP and to remain more vigilant in the follow-up of patients receiving such offending drugs.
Authors’ contribution
The patient's clinical evaluation and management were done by all the authors of Nephrology Department. Pathological and laboratory work-up were done by A.V.V. The manuscript preparation and image collection were done by M.P.P.
Conflict of interest statement
None declared.
References
- 1.Roujeau JC, Kelly JP, Naldi L, et al. Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. N Engl J Med. 1995;333:1600–1607. doi: 10.1056/NEJM199512143332404. [DOI] [PubMed] [Google Scholar]
- 2.Mockenhaupt M. The current understanding of Stevens-Johnson syndrome and toxic epidermal necrolysis. Expert Rev Clin Immunol. 2011;6:803–813. doi: 10.1586/eci.11.66. [DOI] [PubMed] [Google Scholar]
- 3.Martin F, Lauwerys B, Lefèbvre C, et al. Side-effects of intravenous cyclophosphamide pulse therapy. Lupus. 1997;3:254–257. doi: 10.1177/096120339700600307. [DOI] [PubMed] [Google Scholar]
- 4.Reese D, Henning JS, Rockers K, et al. Cyclosporine for SJS/TEN: a case series and review of the literature. Cutis. 2011;87:24–29. [PubMed] [Google Scholar]