IgA nephropathy is the most common cause of idiopathic glomerulonephritis in the developed world. Although this disorder was initially thought to follow a benign course, it is now recognized that slow progression to end-stage renal disease occurs in up to 50% of affected patients. The two major clinical presentations of IgA nephropathy are gross hematuria and persistent asymptomatic microscopic hematuria with or without mild to moderate proteinuria, which can also be seen in nutcracker syndrome caused by nutcracker phenomenon. The nutcracker phenomenon refers to the compression of the left renal vein between the abdominal aorta and the superior mesenteric artery with impaired blood outflow accompanied by distention of the distal portion of the vein. Nutcracker syndrome is the clinical manifestation of nutcracker phenomenon characterized by a wide spectrum of symptoms, such as hematuria, orthostatic proteinuria, pain or gonadal vein syndrome, and varicoceles.
A 34-year-old Japanese woman with recurrent gross hematuria was referred to the clinic for further evaluation. Her medical history was unremarkable and she was not taking any medications. Her family and social history were non-contributory. On examination, she was afebrile with a pulse rate of 70/min and a blood pressure of 110/70 mmHg. Her physical examination was unremarkable. Results of urinalysis showed 2+ hematuria and 1+ proteinuria. Renal ultrasound of the kidneys showed left renal vein entrapment (Figure 1) and color Doppler assessment demonstrated aliasing at the site of compression (Figure 2). The anteroposterior diameter at the hilar portion divided by that at the aortomesenteric portion was 8.8, and the peak flow velocity at the aortomesenteric portion was 228 cm/s. She also underwent percutaneous kidney biopsy, which showed mild diffuse mesangial proliferation and matrix expansion. IgA nephropathy was diagnosed on the basis of immunofluorescence microscopic findings, which indicated isolated prominent globular deposits of IgA, C3 and IgM in the mesangium.
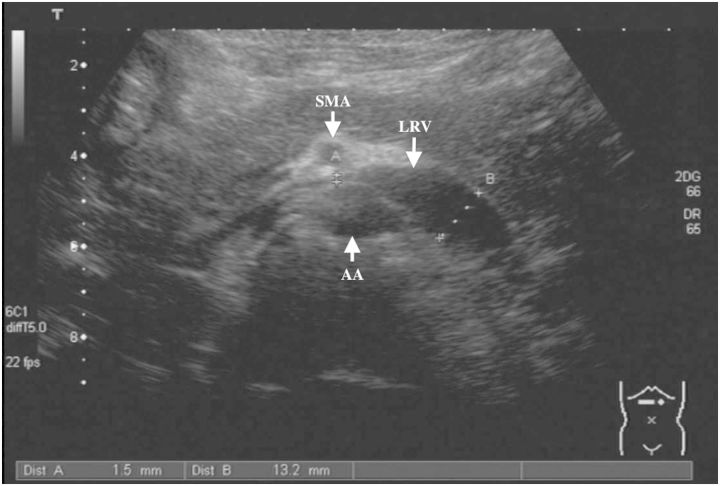
Fig. 1.
B-mode ultrasound of the left renal vein (LRV) showed a near 90% decrease in diameter as it crossed between the superior mesenteric artery (SMA) and abdominal aorta (AA). 377 × 261 mm (72 × 72 DPI).
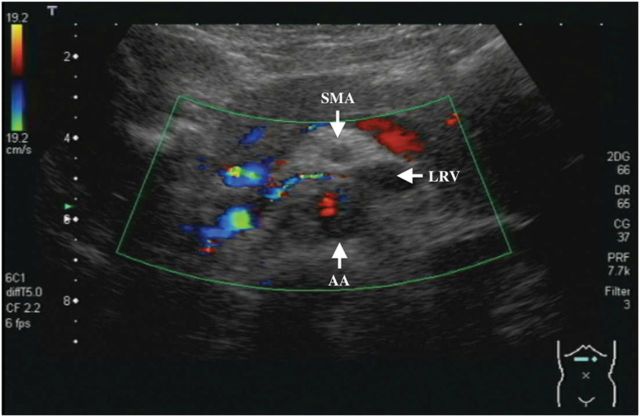
Fig. 2.
Flow in the left renal vein (LRV) was demonstrated by color Doppler assessment. Aliasing was seen at the site of compression. 349 × 234 mm (72 × 72 DPI).
To date, only six cases of concurrent left renal vein entrapment and idiopathic IgA nephropathy have been reported [1–5]: An 11-year-old Italian boy with postural proteinuria who developed gross hematuria [2], a 12-year-old German girl with microscopic hematuria [3], a 9-year-old Korean girl with isolated microscopic hematuria and recurrent gross hematuria [1], a 25-year-old Taiwanese woman with recurrent gross hematuria and left flank pain [4] and two Japanese, 20-year-old woman and 22-year-old man, who, in the context of a pharyngitis, developed gross hematuria and a tendency to microscopic hematuria with persisting proteinuria [5]. Four out of six cases were Asian and the remaining two cases were White.
We retrospectively reviewed all of the IgA nephropathy cases at our institution diagnosed between 2005 and 2012. Of 146 patients with IgA nephropathy, 10 had left renal vein entrapment, that is, a prevalence of 6.8% (Table 1). All patients had dysmorphic urinary red blood cells. Our report is the first to mention the prevalence of left renal vein entrapment in IgA nephropathy in Asian patients. The prevalence of IgA nephropathy varies between people of different ethnicities and is specifically higher in Asian patients. Renal venous congestion caused by left renal vein entrapment may induce both proteinuria and hematuria, which have been implicated as a cause of renal damage. Although a causal relationship between left renal vein entrapment and IgA nephropathy cannot be ruled out, the high prevalence of left renal vein entrapment in IgA nephropathy should be further investigated. It is especially important to evaluate whether the patients have nutcracker phenomenon before initiating treatment for IgA nephropathy as hematuria and proteinuria can be the symptoms of nutcracker syndrome.
Table 1.
Characteristics of patients with nutcracker phenomenon diagnosed in IgA nephropathy
| Age | Sex | U protein | U blood | RBC/HPF | Dysmorphic RBC | RBC casts | |
|---|---|---|---|---|---|---|---|
| No. 1 | 17 | F | 1+ | 2+ | 20–29 | Mod | − |
| No. 2 | 47 | M | 2+ | 3+ | 20–29 | Mod | + |
| No. 3 | 33 | F | 2+ | 2+ | 30–49 | Mod | − |
| No. 4 | 23 | F | − | 3+ | 100 | Mod | − |
| No. 5 | 49 | F | − | 2+ | 10–19 | Mild | − |
| No. 6 | 27 | M | 1+ | 2+ | 20–29 | Mod | + |
| No. 7 | 32 | F | − | 2+ | 20–29 | Mild | − |
| No. 8 | 31 | F | 1+ | 3+ | 50–99 | Mild | + |
| No. 9 | 34 | F | 1+ | 2+ | 5–9 | Mild | − |
| No. 10 | 49 | M | 2+ | 2+ | 5–9 | Mod | − |
Conflict of interest statement
None declared.
References
- 1.Shin JI, Park JM, Shin YH, et al. Nutcracker syndrome combined with IgA nephropathy in a child with recurrent hematuria. Pediatr Int. 2006;48:324–326. doi: 10.1111/j.1442-200X.2006.02212.x. [DOI] [PubMed] [Google Scholar]
- 2.Mazzoni MBM, Milani GP, Persico C, et al. Nutcracker phenomenon and idiopathic IgA nephropathy. NDT Plus. 2011 doi: 10.1093/ndtplus/sfr108. 1–1 doi:10.1093/ndtplus/sfr108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liebl R. Nutcracker phenomenon or nutcracker syndrome? Nephrol Dial Transplant. 2005;20 doi: 10.1093/ndt/gfh917. 2009–author reply 2009. [DOI] [PubMed] [Google Scholar]
- 4.Chen Y-M, Wang I-K, Ng KK, et al. Nutcracker syndrome: an overlooked cause of hematuria. Chang Gung Med J. 2002;25:700–705. [PubMed] [Google Scholar]
- 5.Ozono Y, Harada T, Namie S, et al. The ‘nutcracker’ phenomenon in combination with IgA nephropathy. J Int Med Res. 1995;23:126–131. doi: 10.1177/030006059502300207. [DOI] [PubMed] [Google Scholar]