Abstract
Background
Few studies have evaluated the prevalence of severe hyperkalaemia in unselected patient populations. We identified all episodes of severe hyperkalaemia occurring in 1 year, and described patient demographics, clinical response and outcome. We also assessed junior doctor knowledge of its causes and significance.
Materials and methods
A retrospective interrogation of the database of the regional biochemical laboratory identified all episodes of severe hyperkalaemia (K≥ 6.5 mmol/L) occurring in 2011. The understanding of trainee doctors of the importance, causes and treatment of severe hyperkalaemia was assessed by structured questionnaire.
Results
Severe hyperkalaemia was recorded in 433 samples (365 patients) giving a prevalence of 0.11%. Thirty-six per cent of episodes occurred in patients under the care of a nephrologist, who were significantly younger than those not under the care of a nephrologist. In the nephrology cohort, 86% occurred in patients with chronic kidney disease (CKD), the majority of which had CKD Stage 5. In the non-nephrology cohort, only 65% occurred in the context of CKD, which was equally distributed between Stages 3 and 5 CKD. In both patient groups, roughly 50% of episodes occurred in association with acute kidney injury (AKI). Acute mortality (death within 48 h of documented severe hyperkalaemia) was higher in the non-nephrology compared with the nephrology cohort. Time to repeat serum potassium was influenced by the clinical setting with shorter time to repeat for acute care compared with ward settings. Assessment of trainee doctor's knowledge suggested significant deficiencies in relation to severe hyperkalaemia.
Conclusions
The prevalence of severe hyperkalaemia was low and occurred predominantly in the context of CKD and/or AKI. The majority of episodes occurred in patients not under the care of a nephrologist. Variability in time to repeat serum potassium levels suggested deficiencies in care, and assessment of trainee doctor’s knowledge suggests the need for further educational initiatives to highlight its importance.
Keywords: AKI, CKD, hyperkalaemia, potassium
Introduction
Hyperkalaemia is a potentially life-threatening condition due to the risk of ventricular arrhythmias and cardiac arrest when serum K+ is severely elevated [1, 2]. It is reported to be a common occurrence in hospitalized patients with an incidence of 1.1–10 patients per 100 hospitalized [3–5]. These studies, however, date back over 20 years. More recent studies have focused on hyperkalaemia in either specific disease cohorts or in hospitalized patients only [6]. It is well established that a major cause of hyperkalaemia is chronic renal injury with the associated interference with potassium excretion. Other high-risk cohorts which have been studied are patients with diabetes mellitus or congestive cardiac failure often superimposed on renal dysfunction and often aggravated or precipitated by medications interfering with potassium homeostasis [7–11]. Few recent studies however have examined the nature of severe hyperkalaemia in an unselected patient population. Due to changes in the demographics of the population and patients, and changes in drug prescribing patterns, it is likely that the causes and therefore the demographics of patients with hyperkalaemia have changed. We therefore sought in an unselected patient cohort to examine a consecutive series of hyperkalaemic patients identified from the biochemical records of all patients who had a measurement of serum potassium as part of a ‘routine’ request for measurement of ‘urea and electrolytes’ in a single health board in the UK.
A previous study of 35 adult hyperkalaemic hospitalized patients suggested that hyperkalaemia is generally mild (>5.5<6.5 mmol/L) and therefore not a contributor to patient mortality [11]. The adverse effects of hyperkalaemia on cardiac function are however concentration dependent. In recognition of this, we have collected data on patients with severe hyperkalaemia, defined as a serum potassium value of ≥6.5 mmol/L, as this level of potassium leads to telephone notification of the result to the clinical team looking after the patient. In addition to describing the basic characteristics of patients with severe hyperkalaemia, in contrast to previous studies we have also collected information of patient outcome and management according to the clinical area in which the episode of severe hyperkalaemia occurred. In light of previous studies, and also the findings of our study which have suggested that response by clinicians to hyperkalaemia is frequently suboptimal, in the second component of this study, we assessed the knowledge base of non-specialist/non-nephrology trainee medical staff within the hospital.
Materials and methods
Defining a cohort of patients with severe hyperkalaemia
The Medical Biochemistry Department database of the Cardiff and Vale University Health Board (serving a population of 466 000) was interrogated to gather retrospectively all serum potassium results requested for adult patients between 1 January and 31 December 2011. Using this database, we identified all patients over 18 years of age, who during 2011 had a serum potassium measurement ≥6.5 mmol/L. The reference range for our laboratory is 3.5–5.3 mmol/L. Sample requests generated from intensive care units or dialysis units were excluded.
Baseline serum creatinine values were sought from the same database for each patient, up to 3 months prior to the hyperkalaemic episode, and using the modification of diet in renal disease formula, the estimated baseline GFR was calculated. Patients with a baseline eGFR of ≤60 mL/min were classified as having pre-existing chronic kidney disease (CKD). In addition, the serum creatinine measurement taken at the time of the documented episode of severe hyperkalaemia was recorded and used to document the association of hyperkalaemia with acute kidney injury using the acute kidney injury network definition [12]. Electronic patient records were used to extract all documented comorbidities recorded for each patient prior to and up to the episode of severe hyperkalaemia.
Assessment of the knowledge base of non-specialist trainee medial staff
A questionnaire was distributed to trainee medical staff at two base hospitals served by the regional renal unit. The key areas covered by the questionnaire were significance, causes and treatment of hyperkalaemia (Table 4). The purpose of the questionnaire was explained by one of the co-authors and the questionnaire completed ‘on the spot’. Responses were evaluated against a panel of pre-defined ideal answers, with a maximum score of 33. Responses were collated and analysed according to the speciality of the junior doctor and also performance of the individual questions.
Table 4.
Score of attitude- and knowledge-based assessment by speciality of responding junior doctor
| Total | Med | Surg | A&E | GP | Anaes | O&G | Paeds | |
|---|---|---|---|---|---|---|---|---|
| N | 190 | 71 | 47 | 7 | 10 | 18 | 7 | 10 |
| Average score ± SD | 17.3 ± 5.1 | 19.3 ± 4.4 | 16.5 ± 5.2 | 16.4 ± 5.6 | 15.8 ± 2.9 | 19.2 ± 4.9 | 12.3 ± 6.6 | 15.8 ± 2.9 |
| % | 52.6 | 58.6 | 50.0 | 49.8 | 47.9 | 58.2 | 37.2 | 47.9 |
Statistical analysis was carried out by Student’s t-test, χ2-test and one-way ANNOVA as appropriate, and P < 0.05 was deemed statistically significant.
Results
During the 12-month period of data analysis, a total of 383 422 requests were made for the measurement of serum electrolytes (excluding paediatrics, intensive care and dialysis units). In the same time period, severe hyperkalaemia with potassium values of ≥6.5 mmol/L was recorded in 433 samples (in a total of 365 patients) giving an overall prevalence for severe hyperkalaemia of 0.11%.
Nephrology cohort
Of the patients with severe hyperkalaemia 36% occurred in patients under the care of nephrology, which represents 194 episodes. In the nephrology cohort, severe hyperkalaemia was documented in patients on the general nephrology ward in 56%, renal transplant unit (RTU, not exclusively transplant patients) in 28%, and in the outpatient department in 16% of the episodes.
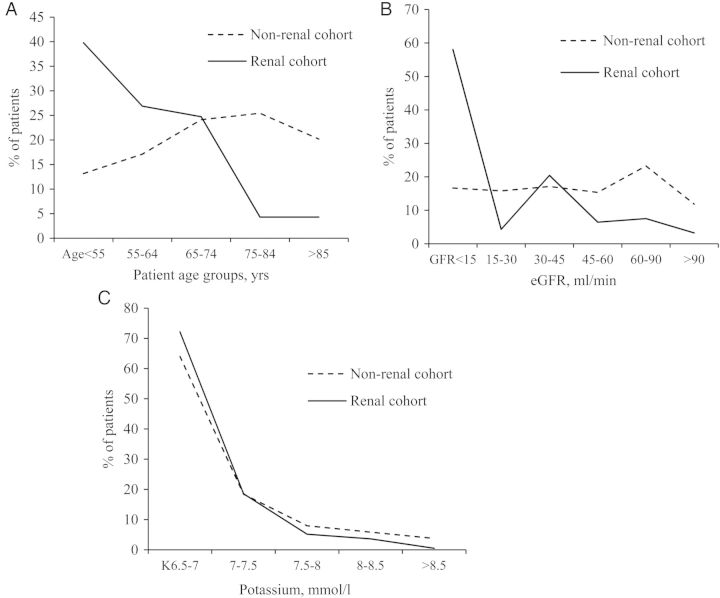
The average age of this nephrology cohort was 57.9 years (95% CI 55.0–60.8 years), reflecting the fact that the majority (67%) of the patients in this nephrology cohort where <65 years of age (Figure 1A). There was no difference in the age of the male and female patients within this cohort (Table 1). In 86% of the patients, severe hyperkalaemia occurred in the context of CKD (Table 2), and of those with CKD, 65% were classified as Stage 5 CKD (Figure 1B). As might be expected given the known higher incidence of CKD in males, there was a higher prevalence of male (61%) compared with female (39%) patients in the nephrology cohort with severe hyperkalaemia.
Fig. 1.
Prevalence (%) of severe hyperkalaemia in patients under the care of a nephrologist (solid line) or not under the care of a nephrologist (broken line) by age (A). eGFR interval (B) and serum potassium (C).
Table 1.
Basic demographics of patients with severe hyperkalaemia
| Total | Females | Males | |
|---|---|---|---|
| Nephrology cohort | |||
| Number of patients (%) | 132 | 51 (39) | 81 (61) |
| Average age (years) | 57.9 (95% CI 55.0–60.8) | 57.6 (95% CI 53.3–61.9) | 58.1 (95% CI 54.4–61.9) |
| Non-nephrology cohort | |||
| Number of patients (%) | 233 | 108 (46) | 125 (54) |
| Average age (years) | 71.2 (95% CI 69.8–73.7) | 71.2 (95% CI 68.5–73.9) | 71.2 (95% CI 68.5–73.9) |
Table 2.
Association of severe hyperkalaemia with CKD and AKI
| Nephrology cohort | Non-nephrology cohort | ||
|---|---|---|---|
| Association with CKD | 114 of 132 | 151 of 233 | P < 0.0001 |
| Association with AKI | 71 of 132 | 119 of 233 | P = 0.04 |
| Association with acute-on-chronic renal injury | 56 of 71 | 73 of 119 | P = 0.01 |
| No CKD and No AKI | 3/132 | 35 of 233 | P < 0.0001 |
| Mean K+ mmol/L | 6.9 (95% CI 6.8–6.92) | 7.0 (95% CI 6.9–7.1) | P = 0.003 |
In this nephrology cohort, severe hyperkalaemia associated with AKI (as defined by the AKI network, dependent on change in creatinine, and including both AKI and acute on chronic kidney injury) occurred in 54% of the patients (Table 2). Within this group, AKI on a background of CKD represents 79% of patients classified as having AKI. The documented incidence of severe hyperkalaemia in the context of AKI was no different between the two ward settings, RTU 57% versus Gen Neph 59%, P = 0.9). Only a small minority of patients in the nephrology cohort had a documented episode of severe hyperkalaemia in the absence of either CKD or AKI (3/132 = 2%).
Non-nephrology cohort
Of all the severe hyperkalaemic events, 239 were recorded in a total of 233 patients not under the care of a nephrologist, thus representing 64% of all the severe hyperkalaemic episodes. Severe hyperkalaemia in the non-nephrology cohort occurred in the setting of acute admissions in 35% and non-acute wards in 52% (medical ward 34%, surgical ward 17%) of the episodes. The remainder of the hyperkalaemic episodes occurred either in the context of the hospital outpatient department (nine patients) or following investigations requested by a primary care physician (three patients).
This non-nephrology cohort was significantly older than the nephrology cohort (Table 1) with an average age of 71.2 years (95% CI 69.8–73.7 years, P < 0.0001 versus nephrology). In contrast to the nephrology cohort, in the non-nephrology cohort, the prevalence of hyperkalaemia increased with age (Figure 1A). As with the nephrology cohort, there was a predominance of male patients (male = 54%, female = 47%, P = 0.14 compared with the distribution in the nephrology cohort). In 65% of the patients, severe hyperkalaemia occurred in the context of CKD (Table 2), which was significantly lower than the proportion with CKD in the nephrology cohort (P < 0.0001). Unlike the nephrology cohort, the patients were distributed equally across all CKD stages (Figure 1B). Within the non-nephrology cohort, the patients with CKD and hyperkalaemia were significantly older than those with no CKD and hyperkalaemia (CKD 75.2 years 95% CI 73.2–77.3 years versus non-CKD 65.4 years 95% CI 61.6–69.2 years, P < 0.0001).
In this non-nephrology cohort, hyperkalaemia occurred in the context of AKI in 51% of patients (Table 2) which is no different to the proportion of hyperkalaemic patients with AKI in the nephrology cohort (P = 0.4). In the non-nephrology cohort, 61% of those with AKI (73/119) occurred in the context of pre-existing CKD. The distribution of hyperkalaemic patients with CKD was equal between the group with AKI 61% and no AKI 52% (P = 0.5).
Unlike the cohort under the care of nephrology in the non-nephrology cohort, a significant proportion of severe hyperkalaemic episodes (15%) was documented in patients with neither CKD nor AKI (35 of 233 versus 3/132 in the Neph cohort (P < 0.001), such that roughly half of those with normal renal function were hyperkalaemic in the absence of AKI.
Despite the difference in the patient demographics between the nephrology and non-nephrology cohort, the distribution of serum potassium values was similar in the nephrology and non-nephrology cohorts (Figure 1C). However, the mean potassium value in the non-nephrology cohort was significantly higher than in the nephrology cohort (non-Neph 7.0 mmol/L 95% CI 6.9–7.1 versus Neph 6.9 mmol/L 95% CI 6.8–6.92, P = 0.003).
Associated co-morbidities
Table 3 shows the comparison of comorbidities recorded for the severe hyperkalaemic patients in the nephrology and non-nephrology cohorts. The burden of comorbidity was higher in the non-nephrology cohort, with a mean number of 2.3 morbidities per patient compared with 1.9 in the nephrology cohort. Specifically, the incidence of all forms of heart disease (43.8 versus 31.9%, 4 P = 0.022), peripheral vascular disease (12.4 versus 1.4%, P = 0.0001) and a recorded diagnosis of malignancy (25.7 versus 14.6%, P = 0.01) was significantly more common in the non-nephrology cohort. There was no statistical difference in the incidence of hypertension (49.4 versus 56.9%, P = 0.1) or diabetes (35.2 versus 36.1%) between the two cohorts. In the non-nephrology, the incidence of severe hyperkalaemia associated with diabetes (P = 0.01), hypertension (P = 0.04) and heart disease (0.0002) was significantly lower in the cohort of patient with neither CKD nor AKI.
Table 3.
Documented comorbidities of patients with severe hyperkalaemia
| Non-nephrology cohort |
Nephrology cohort |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Whole group % (n) | CKD No AKI % (n) | CKD +AKI % (n) | No CKD No AKI % (n) | No CKD +AKI % (n) | Whole group % (n) | CKD No AKI % (n) | CKD +AKI % (n) | No CKD No AKI % (n) | No CKD +AKI % (n) | |
| Atrial fibrillation | 24 (55) | 30.4 (24) | 19.4 (14) | 13.9 (5) | 26.1 (12) | 9.7 (14) | 16.7 (5.1) | 5.1 (3) | 0 | 0 |
| Congestive cardiac failure | 17.2 (40) | 17.2 (14) | 22.2 (16) | 5.6 (2) | 17.4 (8) | 8.3 (12) | 7.6 (5) | 8.5 (5) | 0 | 13.3 (2) |
| Ischemic heart disease | 27 (62) | 38 (30) | 27.8 (20) | 8.3 (3) | 19.6 (9) | 24 (34) | 25.8 (17) | 28.8 (17) | 0 | 0 |
| Valvular heart disease | 7.3 (17) | 7.6 (6) | 11.1 (8) | 5.6 (2) | 2.2 (1) | 4.2 (6) | 6.1 (4) | 3.4 (2) | 0 | 0 |
| Cerebrovascular disease | 11.6 (27) | 8.9 (7) | 18.1 (13) | 0 | 15.2 (7) | 1.4 (2) | 3.0 (2) | 0 | 0 | 0 |
| Peripheral vascular disease | 12.4 (29) | 5.1 (4) | 27.8 (20) | 2.8 (1) | 8.7 (4) | 1.4 (2) | 1.5 (1) | 1.7 (1) | 0 | 0 |
| Hypertension | 49.4 (115) | 49.4 (39) | 59.7 (43) | 30.6 (11) | 47.8 (22) | 56.9 (82) | 45.5 (30) | 67.8 (40) | 50 (2) | 66.7 (10) |
| Diabetes | 35.2 (82) | 32.9 (26) | 44.4 (32) | 13.9 (5) | 41.3 (19) | 36.1 (52) | 34.8 (23) | 37.3 (22) | 25 (1) | 40 (6) |
| Hyperlipidaemia | 10.3 (24) | 13.9 (11) | 11.1 (8) | 2.8 (1) | 8.7 (4) | 9.7 (14) | 4.5 (3) | 11.9 (7) | 25 (1) | 20 (3) |
| Pulmonary disease | 12.0 (28) | 15.1 (12) | 9.7 (7) | 8.3 (3) | 13.0 (6) | 6.3 (9) | 7.6 (5) | 6.8 (4) | 0 | 0 |
| Liver disease | 4.7 (11) | 2.5 (2) | 1.4 (1) | 5.6 (2) | 13.0 (6) | 2.8 (4) | 0 | 6.7 (4) | 0 | 0 |
| Thyroid disease | 6.9 (16) | 11.4 (9) | 1.4 (1) | 5.6 (2) | 8.7 (4) | 4.9 (7) | 3.0 (2) | 5.1 (3) | 0 | 13.3 (2) |
| Malignancy | 25.7 (60) | 17.7 (14) | 27.8 (20) | 38.9 (14) | 26.1 (12) | 14.6 (21) | 16.7 (11) | 15.2 (9) | 0 | 6.7 (1) |
| No recorded comorbidity | 7.7 (18) | 5.1 (4) | 6.9 (5) | 16.7 (6) | 6.5 (3) | 6.9 (10) | 1.5 (1) | 11.9 (7) | 25 (1) | 6.7 (1) |
| No data available | 4.3 (10) | 2.8 (4) | ||||||||
Outcome/management
Time to repeat potassium was taken as an indication of the response to the laboratory generated alert of severe hyperkalaemia.
Nephrology cohort
For the nephrology cohort, repeat measurement was undertaken in 188 of 192 episodes. Overall, in patients with severe hyperkalaemia and in which a repeat measurement was recorded, 37% were repeated on the same day as the hyperkalaemic episode and a further 41% on the following day. As expected, the time to repeat the potassium measurement in the OPD was longer than on either of the ward settings (OPD 12.2 ± 34.6, Gen Neph 3.92 ± 14.9, transplant, 2.76 ± 15.7, data presented as mean number of days ± SD, one-way ANNOVA P = 0.08).
There were three patient deaths within 48 h of documentation of hyperkalaemia, and in two of these no repeat measurement was available (in these two patients, the measured serum potassium was 6.7 and 6.6 mmol/L, and occurred in the context of patients with known CKD and an eGFR of 14 and 4 mL/min, respectively).
Non-nephrology cohort
Overall, in patients with severe hyperkalaemia and in which a repeat measurement was recorded, 45% were repeated on the same day as the hyperkalaemic episode and a further 35% on the following day. When separating the time to repeat potassium measurement by clinical setting, there was a significant difference in time to repeat (acute care 0.6 ± 0.89, ward 3.7 ± 20.6, OPD 57.3 ± 101.4, data presented as mean number of days ± SD, one-way ANNOVA P < 0.0001) and direct comparison also demonstrated a significant difference when comparing the time to repeat measurement in the acute care settings and the two (medical and surgical) non-nephrology ward settings (P = 0.05). There was no significant difference in time to repeat between nephrology ward and non-nephrology wards. As would be expected, the time to repeat potassium measurement in either the OPD (57 ± 110 days, n = 9) setting or in general practice (12 ± 11 days, n = 3) was longer than in either the acute or ward setting; however, as only a small number of patients had documented severe hyperkalaemia in these two settings, a meaningful statistical analysis was not appropriate.
In the non-nephrology cohort, 23 patients with documented severe hyperkalaemia had no record of a repeat measurement of potassium, which is significantly more than in the nephrology cohort (P = 0.002). For the non-nephrology cohort, there were 36 deaths within 48 h of documented severe hyperkalaemic event (distributed equally between acute care and ward settings), which was significantly greater than the acute (<48 h) mortality in the nephrology cohort (P < 0.0001). Of these 36 ‘acute deaths’ with severe hyperkalaemia, 26 were also associated with AKI. In these 36 patients, 18 (50%) had no repeat measurement, compared with a ‘no-repeat rate’ of 14% (2/14) for patients who survived >48 h but who died within 7 days of a severe hyperkalaemic episode (P = 0.017). The mean potassium for those who died within 48 h was greater than those who died >48 h but <7 days, 7.22 mmol/L (95% CI 6.95–7.48) versus 6.85 mmol/L (95% CI 6.62–70.9, P = 0.5).
Attitudes and knowledge
Having highlighted differences in the response to severe hyperkalaemia in different clinical settings, we next sought to assess the working knowledge of doctors in all sub-consultant grades in terms of diagnosis and management. Questionnaires were completed by 190 trainees: 77 foundation, 51 core and 59 specialty trainees. Of those completing the questionnaires, 37% were physicians and a further 25% working in surgical specialities.
Table 4 gives the overall score (out of a possible 33) and scores broken down by specialities. For the whole cohort, the overall score was 17 (52.5%). There was however a significant difference across the specialities, with the medical specialities and anaesthetic trainees scoring significantly higher than the other trainees (P = 0.00001 one-way ANNOVA).
Table 5 gives the mean score of each of the questions. There was a significant difference in the performance of the individual questions (P < 0.00001 one-way ANNOVA), with the lowest scores obtained for the knowledge of the normal range of serum potassium, threshold for treating hyperkalaemia and knowledge of drugs which lead to hyperkalaemia.
Table 5.
Score of attitude and knowledgebased assessment by speciality question
| Question number (marks possible) | Mean score (±SD) | % of maximum possible score |
|---|---|---|
| Q1: What is the normal range for K in your hospital (1 mark) | 0.16 ± 0.4 | 16.4 |
| Q2: What level of K would you treat (2 marks) | 0.45 ± 0.6 | 22.5 |
| Q3: What are the ECG changes associated with hyperkalaemia (3 marks) | 1.95 ± 0.8 | 65.1 |
| Q4: Name five drugs causing hyperkalaemia (5 marks) | 2.2 ± 1.2 | 44.6 |
| Q5: Other than drugs give four other causes of hyperkalaemia (4 marks) | 2.1 ± 0.9 | 51.6 |
| Q6: What are key clinical assessments required in hyperkalaemic patients (2 marks) | 1.3 ± 0.6 | 64.0 |
| Q7: List the initial investigations of a severely hyperkalaemic patients (3 marks) | 1.9 ± 0.7 | 65.1 |
| Q8 (a) Name the treatment options for a patient with severe hyperkalaemia (5 marks). (b) What is the mode of action of the listed treatment? (5 marks) | 3.3 ± 1.2 | 66.5 |
| 2.3 ± 1.5 | 46.2 | |
| Q9: What would you consider to be indications for referral to a nephrologist? (3 marks) | 1.7 ± 0.9 | 57.1 |
Discussion
Overall, the incidence of severe hyperkalaemia in this unselected patient cohort was low. Although the incidence was lower than reported in the widely cited literature, which is now >20 years old [3–5], it is similar to the more recently reported incidence of severe hyperkalaemia (≥6.3 mmol/L) of 0.8% in a study of all K+ assays run by a single laboratory [13], with the discrepancy likely to be attributable to the fact that the study was confined to hospitalized patients, whereas we have analysed all samples irrespective of the source of the request.
Although severe hyperkalaemia is commonly associated with renal impairment and therefore may be considered to lie within the domain of the nephrologist, it is of note that in our study, severe hyperkalaemia was more common in the non-nephrology cohort. Our study also confirms that the vast majority of severe hyperkalaemia occurs in the context of a hospital admission, with only 4.6% (11 of 239) hyperkalaemic events documented in a non-hospital environment (either OPD or primary care) in the non-nephrology cohort. Furthermore, even in those patients under the care of a nephrologist, severe hyperkalaemia was only seen in the outpatient setting in a small minority (16%).
Severe hyperkalaemia occurring in the nephrology and non-nephrology cohorts affects very different patient groups. For the nephrology cohort, severe hyperkalaemia tended to occur in a younger patient group and in the context of end-stage renal failure, whereas in the non-nephrology cohort, severe hyperkalaemia occurred in an older patient cohort and across all stages of renal disease. The high proportion of patients with CKD in the nephrology cohort is likely to account for the higher number of recurrent episodes of severe hyperkalaemia in the nephrology group with 194 episodes occurring in only 132 patients.
In both groups, although severe hyperkalaemia was associated with CKD in the majority, the proportion associated with CKD in the non-nephrology cohort was smaller. This might suggest that the contribution of medication to severe hyperkalaemia may be greater in this cohort. Due to the retrospective nature of the study, we were unable to determine medications prescribed at the time of documentation of hyperkalaemia. We were able to collect data on recorded comorbidities which are likely to indicate indirectly the prescription of medication which may potentially cause or aggravate hyperkalaemia. It is of note that there was a significantly higher burden of comorbidities in the non-nephrology cohort consistent with a higher rate of prescription of medication likely to pre-dispose to hyperkalaemia. This would be further supported by the significant proportion of episodes of severe hyperkalaemia in the non-nephrology cohort which occurred in the absence of either CKD or AKI. In this cohort, however, the incidence of severe hyperkalaemia was significantly lower in absence of renal disease and particularly in those with hypertension, heart disease or diabetes, groups which are likely to have a high burden of medication, suggesting that the most important factor is renal function and that mediation is likely to be an aggravating factor rather than the sole determinant of severe hyperkalaemia in the majority of patients.
Although as one might predict severe hyperkalaemia in the context of CKD was more common in the nephrology cohort, over two-thirds of patients in the non-nephrology cohort also experienced severe hyperkalaemia on a background of CKD. Much has been made of the role of the nephrologist in the care of patients with CKD, with initiatives such as automated eGFR reporting launched to highlight patients with modest degrees of CKD. Despite increasing numbers of patients being referred to a nephrologist following implementation of automated eGFR reporting [14–19], it is clear that only a minority of patients with CKD are seen by a nephrologist [20]. The large group of patients with CKD who are not under the care of a nephrologist remains a challenge. In our study, within the cohort of patients with severe hyperkalaemia, the mean serum potassium was lower in the nephrology cohort. This may be a further reflection of the benefit of early nephrology input, medication review and appropriate dietetic input [21]. As ∼5% of the adult population have moderate to advanced CKD [22, 23], clearly, referral of all patients would be inappropriate and, furthermore, nephrology services would be swamped [24]. The challenge therefore is to carefully select patients who are likely to most benefit from nephrology care such as those with rates of change of eGFR >5 mL/min/year or those with factors which need added input such as uncontrolled hypertension. To this, it may also be appropriate to add patients who are susceptible to hyperkalaemia.
The association of severe hyperkalaemia with AKI is to be expected. In both of our patient groups, severe hyperkalaemia was associated with AKI in over half of the episodes. As with CKD, this suggests that a large proportion of patients with AKI is not seen by a nephrologist. Improved outcomes following AKI have been reported even with minor degrees of AKI following specialist input [25]. Although the primary intention in carrying out this work was to focus on demographics and management of severe hyperkalaemia, the data also highlight a large cohort of patients with AKI and associated significant metabolic disturbance who are not under the care of nephrology.
The retrospective nature of the study prevented us from directly examining any interventions. We therefore used the time to repeat serum potassium measurement as a marker of awareness of the significance and also of action taken following notification of the abnormal result. The number of patients with no documented repeated measurement of serum potassium was higher in the non-nephrology patient group than the nephrology group. Acute mortality, defined for the purposes of this study as death within 48 h of documentation of severe hyperkalaemia was low in the nephrology cohort. In contrast, in the non-nephrology cohort, there were 36 deaths giving an acute death rate of 15%. Within this group, it is of note that compared with the whole group there was a disproportionately high proportion of patients who did not have a repeat measurement of serum potassium. We were however unable to determine cause of death nor the contribution of hyperkalaemia to the agonal event. It is of note however that a documented diagnosis of malignancy was more common in this group furthermore the burden of comorbidity being higher in this group would also suggest a sicker patient cohort to begin with. Without access to patient records, we were, however, unable to determine if the lack of repeated measurement of potassium reflects a conscious decision not to repeat the measurement in a group of sick patients with a higher incidence of ‘terminal illness’. Given that in 50% of the acute deaths, no repeat serum potassium was undertaken, it is likely however that at least in some of these cases, the severe hyperkalaemic episode was at least a contributing factor in the adverse patient outcome.
The medical management of hyperkalaemia is well described, and their relative effectiveness in terms of reduction in serum potassium has been recently reported [26]. In our study, for patients in which repeat potassium measurements were undertaken, it was apparent that the clinical area in which the event occurred affected the time to repeat measurement, with the time to repeat being significantly longer on all ward areas compared with the acute care settings. In the context of our hospital setting, acute care is characterized by early and repeated consultant/senior review, whereas ward based care on a day-to-day basis is directed by more junior medical staff with senior colleague input provided by structured formal wards rounds occurring two or three times per week with additional input as requested on an ad hoc basis. This model of care and the discrepancy between times to repeat between the two clinical care settings suggested that these differences were at least in part driven by a lack of appreciation of the severity of the problem by more junior members of the medical teams. This was directly addressed by our questionnaire of the attitudes and knowledge of junior medical staff. Our educational survey confirmed serious gaps in knowledge of severe hyperkalaemia. Although the results suggest a difference in knowledge across specialities, even in the best performing specialities overall scores revealed significant knowledge gaps. Of particular concern was the significant gaps in fundamental knowledge related directly to clinical management of patients, with questions related to threshold and mechanisms for treatment and drugs which cause hyperkalaemia being amongst those which performed worst.
Summary
In summary, overall prevalence of severe hyperkalaemia is low, with the majority of episodes occurring in hospitalized patients. Patients with severe hyperkalaemia under the care of a nephrologist are younger and tended to have CKD5 whilst in the non-nephrology cohort severe hyperkalaemia occurs across the whole range of renal function. We also identified deficiencies in the care of patients with severe hyperkalaemia and by the use of an educational survey highlighted gaps in the knowledge of non-specialist junior doctors in their knowledge of its management. This highlights the need to enhance the non-specialist understanding and awareness of the context and management of severe hyperkalaemia.
Authors’ Contribution
B.M.P. and S.M. collected and collated all the clinical data, Z.S. provided the raw data on all patients from which the patients with hyperkalaemia were identified, G.R. and M.C. undertook the assessment of trainee doctors knowledge, S.R. and A.O.P. designed the whole study and prepared the manuscript with additional input from all of the listed authors.
Conflict of Interest statement. None declared.
References
- 1.Perazella MA. Drug-induced hyperkalemia: old culprits and new offenders. Am J Med. 2000;109:307–314. doi: 10.1016/s0002-9343(00)00496-4. [DOI] [PubMed] [Google Scholar]
- 2.Weiner ID, Wingo CS. Hyperkalemia: a potential silent killer. J Am Soc Nephrol. 1998;9:1535–1543. doi: 10.1681/ASN.V981535. [DOI] [PubMed] [Google Scholar]
- 3.Moore ML, Bailey RR. Hyperkalaemia in patients in hospital. N Z Med J. 1989;102:557–558. [PubMed] [Google Scholar]
- 4.Paice B, Gray JM, McBride D, et al. Hyperkalaemia in patients in hospital. Br Med J (Clin Res Ed) 1983;286:1189–1192. doi: 10.1136/bmj.286.6372.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shemer J, Modan M, Ezra D, et al. Incidence of hyperkalemia in hospitalized patients. Isr J Med Sci. 1983;19:659–661. [PubMed] [Google Scholar]
- 6.An JN, Lee JP, Jeon HJ, et al. Severe hyperkalemia requiring hospitalization: predictors of mortality. Crit Care. 2012;16:R225. doi: 10.1186/cc11872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Acker CG, Johnson JP, Palevsky PM, et al. Hyperkalemia in hospitalized patients: causes, adequacy of treatment, and results of an attempt to improve physician compliance with published therapy guidelines. Arch Intern Med. 1998;158:917–924. doi: 10.1001/archinte.158.8.917. [DOI] [PubMed] [Google Scholar]
- 8.Jain N, Kotla S, Little BB, et al. Predictors of hyperkalemia and death in patients with cardiac and renal disease. Am J Cardiol. 2012;109:1510–1513. doi: 10.1016/j.amjcard.2012.01.367. [DOI] [PubMed] [Google Scholar]
- 9.Muzzarelli S, Maeder MT, Toggweiler S, et al. Frequency and predictors of hyperkalemia in patients ≥60 years of age with heart failure undergoing intense medical therapy. Am J Cardiol. 2012;109:693–698. doi: 10.1016/j.amjcard.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 10.Siamopoulos KC, Elisaf M, Katopodis K. Iatrogenic hyperkalaemia–points to consider in diagnosis and management. Nephrol Dial Transplant. 1998;13:2402–2406. doi: 10.1093/ndt/13.9.2402. [DOI] [PubMed] [Google Scholar]
- 11.Stevens MS, Dunlay RW. Hyperkalemia in hospitalized patients. Int Urol Nephrol. 2000;32:177–180. doi: 10.1023/a:1007135517950. [DOI] [PubMed] [Google Scholar]
- 12.Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rayan N, Baird R, Masica A. Rapid response team interventions for severe hyperkalemia: evaluation of a patient safety initiative. Hosp Pract (1995) 2011;39:161–169. doi: 10.3810/hp.2011.02.387. [DOI] [PubMed] [Google Scholar]
- 14.Akbari A, Swedko PJ, Clark HD, et al. Detection of chronic kidney disease with laboratory reporting of estimated glomerular filtration rate and an educational program. Arch Intern Med. 2004;164:1788–1792. doi: 10.1001/archinte.164.16.1788. [DOI] [PubMed] [Google Scholar]
- 15.Hemmelgarn BR, Zhang J, Manns BJ, et al. Nephrology visits and health care resource use before and after reporting estimated glomerular filtration rate. JAMA. 2010;303:1151–1158. doi: 10.1001/jama.2010.303. [DOI] [PubMed] [Google Scholar]
- 16.Hobbs H, Stevens P, Klebe B, et al. Referral patterns to renal services: what has changed in the past 4 years? Nephrol Dial Transplant. 2009;24:3411–3419. doi: 10.1093/ndt/gfp289. [DOI] [PubMed] [Google Scholar]
- 17.Jain AK, McLeod I, Huo C, et al. When laboratories report estimated glomerular filtration rates in addition to serum creatinines, nephrology consults increase. Kidney Int. 2009;76:318–323. doi: 10.1038/ki.2009.158. [DOI] [PubMed] [Google Scholar]
- 18.Phillips LA, Donovan KL, Phillips AO. Renal quality outcomes framework and eGFR: impact on secondary care. QJM. 2009;102:415–423. doi: 10.1093/qjmed/hcp030. [DOI] [PubMed] [Google Scholar]
- 19.Vickers JA, Sturdivant RL. Automated reporting of estimated glomerular filtration rate alters referral patterns to a nephrology clinic. Am J Med Sci. 2011;342:218–220. doi: 10.1097/MAJ.0b013e318225440e. [DOI] [PubMed] [Google Scholar]
- 20.Jones RK, Hampton D, O'Sullivan DJ, et al. Diabetes and renal disease: who does what? Clin Med. 2013;5:460–464. doi: 10.7861/clinmedicine.13-5-460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burton CJ, Feest TJ. Does referal to a renal clinic slow the progress of diabetic nephropathy? An audit of 100 consecutive referals. Nephrol Dial Transplant. 1998;13:A108. [Google Scholar]
- 22.Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 23.Drey N, Roderick P, Mullee M, et al. A population-based study of the incidence and outcomes of diagnosed chronic kidney disease. Am J Kidney Dis. 2003;42:677–684. doi: 10.1016/s0272-6386(03)00916-8. [DOI] [PubMed] [Google Scholar]
- 24.John R, Webb M, Young A, et al. Unreferred chronic kidney disease: a longitudinal study. Am J Kidney Dis. 2004;43:825–835. doi: 10.1053/j.ajkd.2003.12.046. [DOI] [PubMed] [Google Scholar]
- 25.Meier P, Bonfils RM, Vogt B, et al. Referral patterns and outcomes in noncritically ill patients with hospital-acquired acute kidney injury. Clin J Am Soc Nephrol. 2011;6:2215–2225. doi: 10.2215/CJN.01880211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fordjour KN, Walton T, Doran JJ. Management of hyperkalemia in hospitalized patients. Am J Med Sci. 2012 doi: 10.1097/MAJ.0b013e318279b105. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]