Abstract
Background
This article provides a summary of the 2011 ERA–EDTA Registry Annual Report (available at www.era-edta-reg.org).
Methods
Data on renal replacement therapy (RRT) for end-stage renal disease (ESRD) from national and regional renal registries in 30 countries in Europe and bordering the Mediterranean Sea were used. From 27 registries, individual patient data were received, whereas 17 registries contributed data in aggregated form. We present the incidence and prevalence of RRT, and renal transplant rates in 2011. In addition, survival probabilities and expected remaining lifetimes were calculated for those registries providing individual patient data.
Results
The overall unadjusted incidence rate of RRT in 2011 among all registries reporting to the ERA–EDTA Registry was 117 per million population (pmp) (n = 71.631). Incidence rates varied from 24 pmp in Ukraine to 238 pmp in Turkey. The overall unadjusted prevalence of RRT for ESRD on 31 December 2011 was 692 pmp (n = 425 824). The highest prevalence was reported by Portugal (1662 pmp) and the lowest by Ukraine (131 pmp). Among all registries, a total of 22 814 renal transplantations were performed (37 pmp). The highest overall transplant rate was reported from Spain, Cantabria (81 pmp), whereas the highest rate of living donor transplants was reported from Turkey (39 pmp). For patients who started RRT between 2002 and 2006, the unadjusted 5-year patient survival on RRT was 46.8% [95% confidence interval (CI) 46.6–47.0], and on dialysis 39.3% (95% CI 39.2–39.4). The unadjusted 5-year patient survival after the first renal transplantation performed between 2002 and 2006 was 86.7% (95% CI 86.2–87.2) for kidneys from deceased donors and 94.3% (95% CI 93.6–95.0) for kidneys from living donors.
Keywords: end-stage renal disease, incidence, prevalence, renal replacement therapy, survival
Introduction
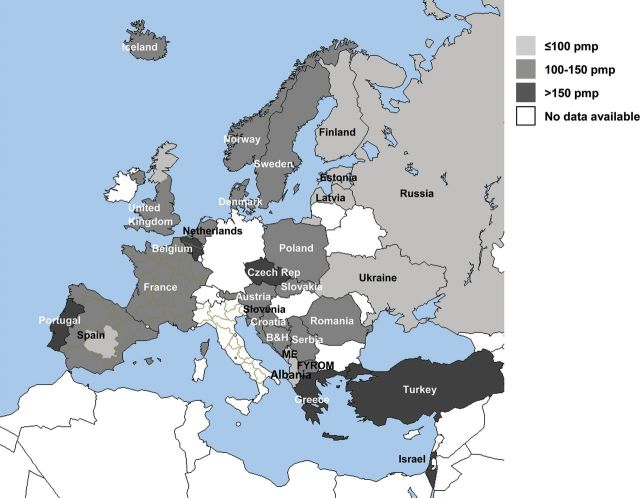
This summary of the 2011 ERA–EDTA (European Renal Association–European Dialysis and Transplant Association) Registry Annual Report includes data on renal replacement therapy (RRT) for end-stage renal disease (ESRD) using 44 data sets from national and regional renal registries in 30 countries in Europe and those bordering the Mediterranean Sea (Figure 1). Data sets with individual patient data were received from 27 national and regional registries in 15 countries, whereas 17 national registries from 17 countries contributed data in aggregated form.
Fig. 1.
Incidence of RRT pmp at Day 1, among all national and regional renal registries in 30 countries reporting to the ERA–EDTA Registry in 2011. B&H: Bosnia and Herzegovina; FYROM: Former Yugoslav Republic of Macedonia; ME: Montenegro. The incidence data for Czech Republic, Slovakia and Turkey represent dialysis patients only.
The analyses on incidence and prevalence and also on transplant rates were based on data from countries and regions that provided individual patient data or aggregated data, while the survival analysis and the calculation of expected remaining lifetimes were solely based on individual patient records. More detailed data than those presented in the current paper were published in the full 2011 ERA–EDTA Registry Annual Report [1], which is available online at www.era-edta-reg.org.
The incidence of RRT for ESRD
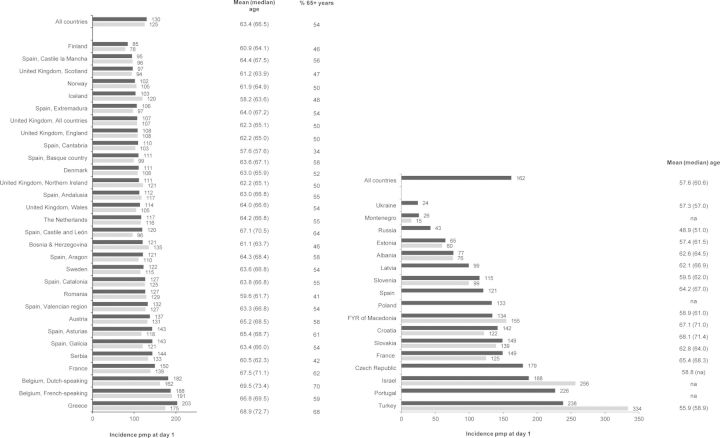
In 2011, a total number of 71 631 patients started RRT for ESRD among all registries reporting to the ERA–EDTA Registry. The total population covered by these registries was 615 million, resulting in an unadjusted incidence rate of 117 per million population (pmp). The highest unadjusted incidence rates were reported from Turkey (238 pmp), Portugal (226 pmp) and Greece (203 pmp), whereas the lowest unadjusted incidence rates were reported from Ukraine (24 pmp), Montenegro (26 pmp) and Russia (43 pmp). The incidence rate standardized for the EU27 population was also highest in Turkey (334 pmp). The mean age at the start of RRT was 63.4 years for countries or regions providing individual patient data and 60.0 years for countries providing aggregated data. There was a wide variation in the mean age at the start of RRT across countries, ranging from 47.9 years in Albania to 69.5 years in the Dutch-speaking part of Belgium. In registries providing individual patient data, the percentage of patients of 65 years and older at the start of RRT was 54%, ranging from 34% in Spain, Cantabria to 70% in Belgium (Dutch-speaking part) (Figure 2).
Fig. 2.
Incidence of RRT pmp at Day 1 in 2011, unadjusted (black bars) and standardized to the age and gender distribution of the EU27 population (grey bars). In addition, mean and median age (years) and percentage of patients aged 65 years and older at RRT initiation are presented. Included are data from renal registries providing individual patient data (left panel) and aggregated data (right panel). The incidence data for Czech Republic, Slovakia and Turkey represent dialysis patients only.
Table 1 summarizes the unadjusted incidence rate of RRT per million age-related population (pmarp) at Day 1 by age group. Particularly in the oldest age category of 75 years and older at the start of RRT, there was a huge variation in incidence rates, ranging from 191 pmarp in Finland to 907 pmarp in the Dutch-speaking part of Belgium.
Table 1.
Incidence of RRT at Day 1 in 2011 by age group as pmarp and percent of patients, unadjusted
| Country/region providing individual patient data | 0–19 years |
20–44 years |
45–64 years |
65–74 years |
75+ years |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| pmarp | % | pmarp | % | pmarp | % | pmarp | % | pmarp | % | |
| Austria | 9.3 | 1 | 38.8 | 10 | 152.1 | 31 | 391.4 | 27 | 527.3 | 31 |
| Belgium | ||||||||||
| Dutch-speakinga | 45.5 | 8 | 147.6 | 23 | 464.5 | 24 | 907.1 | 46 | ||
| French-speakinga | 53.3 | 10 | 226.6 | 31 | 578.3 | 24 | 813.9 | 35 | ||
| Bosnia and Herzegovina | 8.0 | 2 | 41.6 | 12 | 191.9 | 40 | 354.2 | 30 | 497.8 | 16 |
| Denmark | 5.1 | 1 | 46.7 | 13 | 135.9 | 33 | 314.6 | 28 | 386.8 | 24 |
| Finland | 9.0 | 2 | 34.0 | 13 | 114.9 | 39 | 245.8 | 28 | 191.1 | 18 |
| France | 7.4 | 1 | 41.3 | 9 | 153.9 | 27 | 403.6 | 22 | 648.8 | 40 |
| Greece | 6.4 | 1 | 40.6 | 7 | 181.8 | 24 | 563.9 | 27 | 874.4 | 41 |
| Iceland | 22.3 | 6 | 62.8 | 21 | 102.4 | 24 | 381.8 | 24 | 425.6 | 24 |
| Norway | 9.6 | 2 | 45.5 | 15 | 130.1 | 33 | 285.1 | 23 | 383.8 | 27 |
| Romania | 8.2 | 1 | 52.1 | 16 | 215.6 | 42 | 395.8 | 26 | 276.8 | 15 |
| Serbia | 6.0 | 1 | 56.7 | 13 | 221.7 | 44 | 406.9 | 26 | 293.3 | 16 |
| Spain | ||||||||||
| Andalusia | 5.4 | 1 | 37.6 | 13 | 142.8 | 31 | 415.4 | 29 | 387.4 | 26 |
| Aragon | 4.1 | 1 | 41.4 | 12 | 134.1 | 29 | 408.8 | 29 | 308.6 | 29 |
| Asturias | 13.0 | 1 | 35.3 | 8 | 144.9 | 30 | 409.0 | 28 | 373.0 | 33 |
| Basque Country | 10.4 | 2 | 42.1 | 13 | 107.3 | 27 | 356.1 | 30 | 296.5 | 28 |
| Cantabriaa | 75.1 | 25 | 163.4 | 42 | 221.6 | 17 | 176.6 | 17 | ||
| Castile and Leona | 37.4 | 10 | 111.9 | 26 | 307.4 | 25 | 352.4 | 39 | ||
| Castile-La Manchaa | 33.7 | 13 | 120.9 | 30 | 392.5 | 32 | 233.7 | 24 | ||
| Catalonia | 7.3 | 1 | 42.2 | 13 | 154.8 | 30 | 396.0 | 25 | 443.0 | 30 |
| Extremadura | 9.1 | 2 | 38.3 | 13 | 130.5 | 31 | 271.6 | 22 | 324.0 | 32 |
| Galicia | 15.9 | 2 | 53.6 | 13 | 170.1 | 32 | 329.3 | 24 | 345.8 | 30 |
| Valencian region | 14.8 | 2 | 40.3 | 12 | 167.6 | 32 | 377.1 | 25 | 463.3 | 29 |
| Sweden | 7.8 | 1 | 48.2 | 13 | 149.4 | 31 | 317.1 | 26 | 406.3 | 28 |
| The Netherlands | 6.7 | 1 | 40.4 | 11 | 135.9 | 32 | 353.7 | 27 | 473.8 | 28 |
| UK, all countriesa | 52.7 | 17 | 139.2 | 33 | 300.0 | 25 | 342.8 | 25 | ||
| Englanda | 53.8 | 17 | 140.3 | 33 | 303.6 | 25 | 344.8 | 25 | ||
| Northern Irelanda | 46.5 | 14 | 162.0 | 35 | 354.6 | 26 | 408.7 | 24 | ||
| Scotland | 10.2 | 2 | 42.2 | 15 | 125.5 | 36 | 265.4 | 25 | 276.9 | 22 |
| Walesa,b | 55.1 | 15 | 133.4 | 31 | 272.8 | 24 | 382.4 | 30 | ||
| All countries | 5.3 | 1 | 46.0 | 12 | 155.7 | 31 | 369.5 | 25 | 476.7 | 30 |
pmarp: per million age-related population.
aPatients <20 years of age are not reported.
bThe incidence of RRT is slightly underestimated, for details see the UK Renal Registry Report 2012.
We performed a separate analysis for children treated with RRT based on data from a selection of registries. As the numbers of children starting RRT were low, we present the incidence for the years 2010 and 2011 combined (Table 2). A more detailed overview of paediatric RRT data in Europe can be found at www.espn-reg.org.
Table 2.
Incidence of RRT at Day 1 for the period 2010–11 among patients aged 0–19 years, by age group, as counts (N) and pmarp, unadjusted
| Cohorta | All 0–19 years | 0–4 years | 5–9 years | 10–14 years | 15–19 years |
|---|---|---|---|---|---|
| N (pmarp) | N (pmarp) | N (pmarp) | N (pmarp) | N (pmarp) | |
| All countries | 626 (8.2) | 150 (7.9) | 71 (3.7) | 139 (7.4) | 266 (13.4) |
pmarp: per million age-related population.
aBased on data from Austria, Bosnia and Herzegovina, Denmark, Finland, France, Greece, Iceland, Norway, Romania, Serbia, Spain (Andalusia), Spain (Aragon), Spain (Asturias), Spain (Basque Country), Spain (Catalonia), Spain (Extremadura), Spain (Galicia), Spain (Valencian region), Sweden, the Netherlands and UK (Scotland).
Tables 3 and 4 present the incidence of the different treatment modalities including haemodialysis (HD), peritoneal dialysis (PD) and (pre-emptive) renal transplantation at Day 91 after the start of RRT. Whereas the incidence rates of HD were highest in Turkey (194 pmp), Portugal (187 pmp) and Greece (170 pmp), the incidence rates of PD were highest in Sweden (34 pmp), Iceland (31 pmp) and Denmark (30 pmp). For patients living with a functioning graft at Day 91 of RRT, the highest incidence rates were observed in Norway (15 pmp) and the Netherlands, Spain, Catalonia and Iceland (for all 13 pmp).
Table 3.
Incidence of RRT pmp at Day 91 after the start of RRT in 2011 for countries and regions providing individual patient data, by treatment modality, unadjusted
| Country/region | All (pmp) | HD (pmp) | PD (pmp) | Tx (pmp) | Unknown/missing (pmp) |
|---|---|---|---|---|---|
| Austria | 126.0 | 109.3 | 12.8 | 3.8 | 0 |
| Belgium | |||||
| Dutch-speakinga | 164.8 | 144.4 | 16.9 | 3.5 | 0 |
| French-speakinga | 166.3 | 141.7 | 17.8 | 4.9 | 1.9 |
| Bosnia and Herzegovina | 107.7 | 102.6 | 5.0 | 0 | 0 |
| Denmark | 104.9 | 67.5 | 30.1 | 6.7 | 0.5 |
| Finland | 82.8 | 60.5 | 22.1 | 0.2 | 0 |
| France | 137.3 | 114.4 | 15.7 | 6.6 | 0.6 |
| Greece | 182.6 | 169.6 | 12.5 | 0.6 | 0 |
| Iceland | 103.4 | 59.6 | 31.3 | 12.5 | 0 |
| Norway | 96.3 | 62.4 | 18.6 | 15.3 | 0 |
| Romania | 104.5 | 94.8 | 7.9 | 1.8 | 0 |
| Serbia | 132.3 | 116.7 | 13.8 | 1.8 | 0 |
| Spain | |||||
| Andalusia | 107.9 | 90.2 | 13.6 | 4.0 | 0 |
| Aragon | 115.7 | 94.2 | 17.8 | 3.7 | 0 |
| Asturias | 137.2 | 100.2 | 29.9 | 7.1 | 0 |
| Basque Country | 108.7 | 77.7 | 28.3 | 2.7 | 0 |
| Cantabriaa | 104.5 | 65.7 | 28.6 | 10.1 | 0 |
| Castille and Leona | 116.0 | 90.5 | 22.7 | 2.7 | 0 |
| Castille-La Manchaa | 94.4 | 75.5 | 17.5 | 1.4 | 0 |
| Catalonia | 122.2 | 92.3 | 16.9 | 13.0 | 0 |
| Extremadura | 105.2 | 87.8 | 17.4 | 0.0 | 0 |
| Galicia | 137.7 | 104.6 | 28.6 | 4.5 | 0 |
| Valencian region | 128.8 | 104.2 | 21.7 | 2.9 | 0 |
| Sweden | 108.8 | 65.9 | 34.0 | 8.9 | 0 |
| The Netherlands | 108.4 | 76.1 | 18.9 | 13.3 | 0 |
| UK, all countriesa | 100.6 | 70.9 | 21.8 | 7.9 | 0 |
| Englanda | 101.3 | 70.3 | 22.4 | 8.6 | 0 |
| Northern Irelanda | 104.5 | 80.7 | 17.5 | 6.3 | 0 |
| Scotland | 90.6 | 69.5 | 17.1 | 4.0 | 0 |
| Walesa,b | 108.9 | 80.2 | 24.1 | 4.6 | 0 |
| All countries | 119.3 | 94.7 | 18.1 | 6.3 | 0.2 |
HD, haemodialysis; PD, peritoneal dialysis; Tx, renal transplant.
aPatients <20 years of age are not reported.
bThe incidence of RRT is slightly underestimated, for details see the UK Renal Registry Report 2012.
Table 4.
Incidence of RRT pmp at Day 91 after the start of RRT in 2011 for countries providing aggregated patient data, by treatment modality, unadjusted
| Country | All (pmp) | HD (pmp) | PD (pmp) | Tx (pmp) | Unknown/missing (pmp) |
|---|---|---|---|---|---|
| Albania | 70.8 | 66.5 | 2.5 | 1.8 | 0 |
| Croatia | 132.1 | 117.6 | 12.8 | 1.6 | 0 |
| Czech Republica | 137.4 | 128.8 | 8.6 | 0 | |
| Estonia | 60.4 | 35.8 | 17.2 | 7.5 | 0 |
| France | 128.2 | 110.0 | 11.9 | 6.3 | 0 |
| FYR of Macedonia | 121.2 | 120.7 | 0.5 | 0.0 | 0 |
| Israel | 175.9 | 157.7 | 12.0 | 6.2 | 0 |
| Latvia | 86.5 | 78.5 | 8.0 | 0.0 | 0 |
| Montenegro | 12.9 | 12.9 | 0.0 | 0.0 | 0 |
| Portugalb | 209.8 | 186.5 | 21.3 | 2.0 | 0 |
| Slovakiaa | 127.3 | 123.1 | 4.3 | 0 | |
| Slovenia | 105.3 | 99.9 | 4.9 | 0.5 | 0 |
| Turkeya | 208.9 | 194.3 | 14.7 | 0 | |
| All countries | 161.8 | 146.4 | 12.6 | 4.6 | 0.0 |
HD, haemodialysis; PD, peritoneal dialysis; Tx, renal transplant.
aData represent dialysis patients only.
bOnly pre-emptive transplantations (at Day 1) are included.
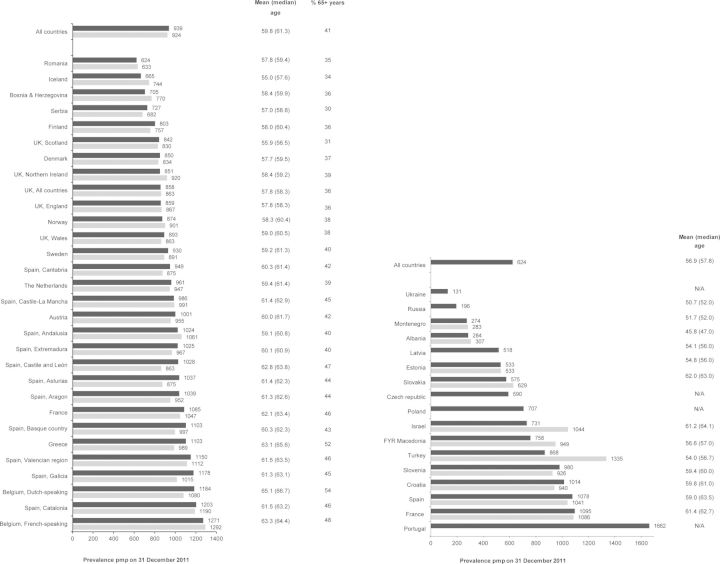
The prevalence of RRT for ESRD
On 31 December 2011, there were 425 824 RRT patients in all registries reporting to the ERA–EDTA Registry, corresponding to a prevalence of 692 pmp. As shown in Figure 3, the unadjusted prevalence of RRT pmp was highest in Portugal (1662 pmp), Belgium (French-speaking) (1271 pmp) and Spain, Catalonia (1203 pmp). On the other hand, Ukraine (131 pmp) and Russia (196 pmp) reported the lowest unadjusted prevalence. The prevalence of RRT standardized for the EU27 population was highest in Turkey (1335 pmp). On 31 December 2011, the overall mean age was 59.8 years among countries providing individual patient data and 56.9 years among countries providing aggregated data. The mean age ranged from 47.0 years in Albania to 65.4 years in Portugal. The mean percentage of prevalent patients aged 65 years and older in registries providing individual patient data was 41%, with a range from 30% in Serbia to 54% in Belgium (Dutch-speaking part) (Figure 3).
Fig. 3.
Prevalence of RRT pmp on 31 December 2011, unadjusted (black bars) and standardized to the age and gender distribution of the EU27 population (grey bars). In addition, mean and median age (years) are presented. Included are data from renal registries providing individual patient data (left panel) and aggregated data (right panel). The prevalence data for Czech Republic, Israel and Slovakia represent dialysis patients only. In Romania, the prevalence of RRT is underestimated by ∼3%, due to an estimated 30% underreporting of patients living with a functioning graft.
Table 5 summarizes the unadjusted prevalence of RRT pmarp at 31 December 2011 by age group. Like for the incidence, the most pronounced variation in prevalence was observed in the highest age category (≥75 years), ranging from 918 pmp in Serbia to 4112 pmp in Dutch-speaking Belgium. The prevalence for the age group 0–19 years, averaged for 2010 and 2011, is presented in Table 6.
Table 5.
Prevalence of RRT on 31 December 2011 by age group as pmarp and percent of patients, unadjusted
| Country/region providing individual patient data | 0–19 years |
20–44 years |
45–64 years |
65–74 years |
75+ years |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| pmarp | % | pmarp | % | pmarp | % | pmarp | % | pmarp | % | |
| Austria | 59.8 | 1 | 448.5 | 15 | 1527.0 | 42 | 2556.4 | 25 | 2081.1 | 17 |
| Belgium | ||||||||||
| Dutch-speakinga | 421.1 | 11 | 1459.0 | 34 | 2945.6 | 23 | 4060.6 | 31 | ||
| French-speakinga | 513.3 | 14 | 1844.5 | 38 | 3666.6 | 22 | 4111.6 | 26 | ||
| Bosnia and Herzegovina | 25.1 | 1 | 344.4 | 17 | 1259.4 | 45 | 1605.3 | 23 | 2429.7 | 13 |
| Denmark | 63.7 | 2 | 539.3 | 20 | 1316.7 | 41 | 1851.8 | 22 | 1787.6 | 15 |
| Finland | 99.3 | 3 | 401.1 | 16 | 1278.1 | 45 | 1945.5 | 23 | 1273.8 | 13 |
| France | 44.6 | 1 | 513.5 | 15 | 1550.3 | 38 | 2676.3 | 21 | 2978.5 | 25 |
| Greece | 49.9 | 1 | 430.4 | 14 | 1432.8 | 34 | 2755.7 | 25 | 3059.6 | 27 |
| Iceland | 78.1 | 3 | 493.4 | 26 | 1011.0 | 37 | 2004.6 | 20 | 1543.0 | 14 |
| Norway | 67.4 | 2 | 491.5 | 19 | 1415.7 | 41 | 2357.5 | 22 | 1930.4 | 16 |
| Romania | 28.0 | 1 | 325.3 | 21 | 1118.2 | 44 | 1616.5 | 22 | 1193.0 | 13 |
| Serbia | 23.2 | 1 | 427.6 | 20 | 1252.1 | 49 | 1620.2 | 20 | 917.5 | 10 |
| Spain | ||||||||||
| Andalusia | 49.4 | 1 | 505.2 | 19 | 1668.0 | 40 | 2868.5 | 22 | 2465.8 | 18 |
| Aragon | 32.6 | 1 | 437.1 | 15 | 1612.6 | 40 | 2521.1 | 21 | 2101.0 | 23 |
| Asturias | 45.4 | 1 | 467.6 | 15 | 1408.0 | 40 | 2216.0 | 21 | 1923.8 | 23 |
| Basque Country | 83.5 | 1 | 500.2 | 16 | 1567.8 | 40 | 2805.1 | 24 | 2049.0 | 19 |
| Cantabria | 431.6 | 16 | 1440.6 | 42 | 2558.0 | 23 | 1701.3 | 19 | ||
| Castile and Leona | 418.4 | 14 | 1481.8 | 39 | 2131.7 | 20 | 2093.6 | 27 | ||
| Castile-La Manchaa | 425.0 | 16 | 1583.4 | 38 | 2992.9 | 23 | 2193.7 | 22 | ||
| Cataloniaa | 65.6 | 1 | 488.0 | 16 | 1815.2 | 38 | 3353.3 | 23 | 3220.1 | 23 |
| Extremadura | 31.7 | 1 | 501.0 | 17 | 1667.7 | 42 | 2266.8 | 19 | 2071.8 | 21 |
| Galicia | 43.3 | 1 | 537.2 | 16 | 1679.1 | 38 | 2651.5 | 23 | 2112.4 | 22 |
| Valencian region | 70.2 | 1 | 455.0 | 15 | 1717.8 | 38 | 3007.7 | 23 | 3178.7 | 23 |
| Sweden | 70.6 | 2 | 465.7 | 16 | 1507.2 | 41 | 2210.5 | 24 | 1786.0 | 16 |
| The Netherlands | 63.0 | 2 | 497.6 | 18 | 1335.1 | 41 | 2275.8 | 22 | 2235.3 | 17 |
| UK, all countriesa | 563.7 | 22 | 1412.9 | 42 | 1912.7 | 20 | 1699.6 | 16 | ||
| Englanda | 560.8 | 22 | 1423.2 | 42 | 1937.9 | 20 | 1701.7 | 16 | ||
| Northern Irelanda | 545.5 | 22 | 1375.5 | 39 | 2222.9 | 21 | 2252.3 | 18 | ||
| Scotland | 72.4 | 2 | 589.9 | 23 | 1340.8 | 43 | 1636.1 | 18 | 1445.1 | 13 |
| Walesa | 582.2 | 20 | 1390.3 | 41 | 1814.5 | 20 | 1810.9 | 18 | ||
| All countries | 34.6 | 1 | 484.6 | 18 | 1450.4 | 40 | 2308.8 | 22 | 2283.4 | 20 |
pmarp; per million age-related population.
aPatients <20 years of age are not reported.
Table 6.
Prevalence of RRT on 31 December 2011 among patients aged 0–19 years, by age group, as counts (N) and pmarp, unadjusted
| Cohorta | All 0–19 years | 0–4 years | 5–9 years | 10–14 years | 15–19 years |
|---|---|---|---|---|---|
| N (pmarp) | N (pmarp) | N (pmarp) | N (pmarp) | N (pmarp) | |
| All countries | 2111 (52.8) | 206 (20.9) | 321 (32.3) | 565 (57.4) | 1019 (98.9) |
pmarp; per million age-related population.
aBased on data from Austria, Bosnia and Herzegovina, Denmark, Finland, France, Greece, Iceland, Norway, Romania, Serbia, Spain (Andalusia), Spain (Aragon), Spain (Asturias), Spain (Basque Country), Spain (Catalonia), Spain (Extremadura), Spain (Galicia), Spain (Valencian region), Sweden, the Netherlands and UK (Scotland).
Tables 7 and 8 show that the prevalence of HD on 31 December 2011 was highest in Portugal (986 pmp) and Greece (819 pmp) and lowest in Ukraine (98 pmp), Montenegro (137 pmp) and Russia (141 pmp). For PD, the prevalence was highest in Spain, Galicia (102 pmp) and Spain, Basque Country (94 pmp), whereas the lowest prevalence of this treatment modality was reported in Montenegro (9.7 pmp) and FYR of Macedonia and Russia (both 13 pmp). Finally, the prevalence of patients living with a functioning graft was highest in Spain, Basque Country (645 pmp), Spain, Catalonia (636 pmp) and Norway (629 pmp).
Table 7.
Prevalence of RRT pmp on 31 December 2011 for countries and regions providing individual patient data, by treatment modality, unadjusted
| Country/region | All (pmp) | HD (pmp) | PD (pmp) | Tx (pmp) | Unknown/missing (pmp) |
|---|---|---|---|---|---|
| Austria | 1001.5 | 458.9 | 42.3 | 500.3 | 0.0 |
| Belgium | |||||
| Dutch-speakinga | 1184.4 | 631.1 | 62.3 | 491.1 | 0.0 |
| French-speakinga | 1271.0 | 674.4 | 61.3 | 531.0 | 4.3 |
| Bosnia and Herzegovina | 705.0 | 632.0 | 26.2 | 46.5 | 0.3 |
| Denmark | 850.5 | 358.6 | 89.4 | 398.6 | 3.9 |
| Finland | 802.7 | 267.8 | 61.1 | 473.8 | 0.0 |
| France | 1085.5 | 572.3 | 43.2 | 462.2 | 7.7 |
| Greece | 1103.1 | 818.7 | 63.8 | 220.5 | 0.0 |
| Iceland | 664.5 | 203.8 | 50.2 | 410.6 | 0.0 |
| Norway | 874.0 | 207.7 | 37.6 | 628.7 | 0.0 |
| Romania | 624.1 | 506.5 | 70.4 | 47.0 | 0.2 |
| Serbia | 726.7 | 567.5 | 57.0 | 101.7 | 0.6 |
| Spain | |||||
| Andalusia | 1024.2 | 470.4 | 44.0 | 509.7 | 0.1 |
| Aragon | 1038.7 | 422.1 | 40.1 | 576.5 | 0.0 |
| Asturias | 1037.5 | 387.4 | 62.9 | 587.2 | 0.0 |
| Basque Country | 1102.9 | 364.1 | 93.7 | 645.1 | 0.0 |
| Cantabria | 948.6 | 323.5 | 74.1 | 545.9 | 5.1 |
| Castille and Leona | 1028.5 | 426.7 | 69.7 | 522.3 | 9.8 |
| Castille-La Manchaa | 985.5 | 404.0 | 50.0 | 526.8 | 4.7 |
| Cataloniaa | 1202.6 | 519.1 | 47.1 | 636.4 | 0.0 |
| Extremadura | 1024.6 | 505.1 | 58.6 | 460.9 | 0.0 |
| Galicia | 1178.4 | 531.1 | 101.5 | 545.8 | 0.0 |
| Valencian region | 1150.0 | 629.4 | 57.3 | 463.3 | 0.0 |
| Sweden | 929.9 | 323.2 | 87.1 | 519.6 | 0.0 |
| The Netherlands | 911.2 | 324.1 | 60.7 | 526.4 | 0.1 |
| UK, all countriesa | 857.7 | 375.3 | 62.3 | 419.7 | 0.3 |
| Englanda | 859.1 | 376.2 | 63.8 | 418.7 | 0.4 |
| Northern Irelanda | 850.7 | 412.4 | 45.3 | 393.0 | 0.0 |
| Scotland | 841.6 | 360.7 | 50.3 | 430.6 | 0.0 |
| Walesa | 892.8 | 367.2 | 70.8 | 454.5 | 0.3 |
| All countries | 946.6 | 473.3 | 58.2 | 413.1 | 2.0 |
HD, haemodialysis; PD, peritoneal dialysis; Tx, renal transplant.
aPatients <20 years of age are not reported.
Table 8.
Prevalence of RRT pmp on 31 December 2011 for countries providing aggregated patient data, by treatment modality, unadjusted
| Country | All (pmp) | HD (pmp) | PD (pmp) | Tx (pmp) | Unknown/missing (pmp) |
|---|---|---|---|---|---|
| Albania | 284.0 | 194.6 | 15.4 | 74.0 | 0.0 |
| Croatia | 1013.5 | 615.4 | 50.6 | 347.5 | 0.0 |
| Czech Republica | 590.0 | 541.0 | 49.0 | ||
| Estonia | 532.8 | 179.1 | 51.5 | 302.2 | 0.0 |
| France | 1094.8 | 569.5 | 40.5 | 484.8 | 0.0 |
| FYR Macedonia | 758.2 | 674.6 | 12.9 | 70.7 | 0.0 |
| Israela | 730.7 | 687.6 | 43.1 | 0.0 | |
| Latvia | 517.8 | 195.3 | 46.4 | 276.1 | 0.0 |
| Montenegro | 274.2 | 137.1 | 9.7 | 127.4 | 0.0 |
| Poland | 706.7 | 438.4 | 27.7 | 240.6 | 0.0 |
| Portugal | 1661.9 | 985.5 | 66.7 | 609.7 | 0.0 |
| Russia | 195.7 | 141.3 | 12.9 | 41.5 | 0.0 |
| Slovakiaa | 574.9 | 557.7 | 17.2 | 0.0 | |
| Slovenia | 980.0 | 656.4 | 29.2 | 294.3 | 0.0 |
| Spain | 1078.0 | 480.4 | 56.8 | 537.5 | 3.3 |
| Turkeyb | 868.2 | 709.5 | 63.3 | 95.4 | 0.0 |
| Ukrainec | 130.8 | 97.7 | 16.0 | 17.2 | 0.0 |
| All countries | 623.8 | 392.7 | 33.4 | 206.6 | 0.4 |
HD, haemodialysis; PD, peritoneal dialysis; Tx, renal transplant.
aData represent dialysis patients only.
bThe number of patients living with a functioning graft is underestimated.
cData do not include Kiev city.
Renal transplants performed
The overall number of renal transplants performed in 2011 among all registries reporting to the ERA–EDTA Registry was 22 814 (37 pmp). Of those, a total of 16 118 (26 pmp) renal transplants were performed using deceased donor kidneys, 6 059 (9.9 pmp) using a living donor kidneys and for 637 (1.0 pmp) transplants the donor type was unknown. Tables 9 and 10 report that the highest overall transplant rates were reported from Spain, Cantabria (81 pmp) and Spain, Catalonia (77 pmp). Rates of living donor kidney transplants were highest in Turkey (39 pmp), Iceland (35 pmp), the Netherlands and UK, Northern Ireland (both 26 pmp).
Table 9.
Renal transplants performed pmp in 2011 for countries and regions providing individual patient data, by donor type, unadjusted
| Country/region | All (pmp) | Living donor (pmp) | Deceased donor (pmp) | Unknown donor type (pmp) |
|---|---|---|---|---|
| Austria | 44.6 | 5.5 | 39.2 | 0 |
| Belgium | ||||
| Dutch-speakinga | 39.7 | 3.0 | 36.5 | 0.2 |
| French-speakinga | 44.6 | 3.6 | 40.7 | 0.2 |
| Bosnia and Herzegovina | 6.3 | 4.6 | 1.7 | 0 |
| Denmark | 41.4 | 15.8 | 23.1 | 2.5 |
| Finland | 32.7 | 2.4 | 30.3 | 0 |
| France | 43.6 | 3.4 | 40.1 | 0.1 |
| Greece | 17.8 | 4.6 | 13.2 | 0 |
| Iceland | 34.5 | 34.5 | 0 | 0 |
| Norway | 61.0 | 14.7 | 46.2 | 0 |
| Romaniab | 8.1 | 3.0 | 3.7 | 1.4 |
| Serbia | 15.6 | 6.1 | 9.5 | 0 |
| Spain | ||||
| Andalusia | 49.9 | 49.9 | ||
| Aragon | 57.9 | 6.7 | 51.2 | 0 |
| Asturias | 49.9 | 8.3 | 41.6 | 0 |
| Basque Country | 55.3 | 0 | 55.3 | 0 |
| Cantabria | 80.9 | 10.1 | 70.8 | 0 |
| Castille and Leona | 40.4 | 0 | 40.4 | 0 |
| Castille-La Manchaa | 38.7 | 38.7 | ||
| Cataloniaa | 76.8 | 18.7 | 58.1 | 0 |
| Extremadura | 46.9 | 2.7 | 41.5 | 2.7 |
| Galicia | 53.1 | 8.6 | 44.5 | 0 |
| Valencian region | 37.5 | 1.6 | 36.0 | 0 |
| Sweden | 45.2 | 19.5 | 25.7 | 0 |
| The Netherlands | 51.6 | 26.4 | 25.2 | 0 |
| UK, all countriesa | 43.7 | 16.4 | 27.3 | 0 |
| Englanda | 43.9 | 16.7 | 27.0 | 0 |
| Northern Irelanda | 63.0 | 26.0 | 37.0 | 0 |
| Scotland | 32.2 | 10.1 | 22.1 | 0 |
| Walesa | 48.6 | 12.6 | 36.1 | 0 |
| All countries | 41.5 | 9.8 | 29.5 | 2.2 |
We used data from NHS Blood and Transplant Service for UK.
aPatients <20 years of age are not reported.
bThe transplantation activity reflects 70% of the total transplantation activity in the country, because there is underreporting of pre-emptive transplants.
Table 10.
Renal transplants performed pmp in 2011 for countries providing aggregated patient data, by donor type, unadjusted
| Country | All (pmp) | Living donor (pmp) | Deceased donor (pmp) | Unknown donor type (pmp) |
|---|---|---|---|---|
| Albania | 3.9 | 3.9 | 0.0 | 0.0 |
| Croatia | 53.7 | 7.5 | 43.6 | 2.6 |
| Czech Republic | 31.9 | 3.8 | 28.1 | 0.0 |
| Estonia | 32.8 | 2.2 | 30.6 | 0.0 |
| France | 46.3 | 4.7 | 41.6 | 0.0 |
| FYR of Macedonia | 3.0 | 3.0 | 0.0 | 0.0 |
| Israel | 52.4 | 16.5 | 26.8 | 9.1 |
| Latvia | 36.1 | 1.7 | 34.4 | 0.0 |
| Montenegro | 3.2 | 0.0 | 3.2 | 0.0 |
| Poland | 27.0 | 1.0 | 26.0 | 0.0 |
| Portugal | 50.2 | 4.4 | 45.7 | 0.0 |
| Russia | 6.8 | 1.3 | 5.6 | 0.0 |
| Slovakia | 23.9 | 2.4 | 21.5 | 0.0 |
| Slovenia | 22.4 | 0.0 | 22.4 | 0.0 |
| Spain | 52.9 | 6.6 | 46.3 | 0.0 |
| Turkey | 47.5 | 39.2 | 8.4 | 0.0 |
| Ukrainea | 1.4 | 0.8 | 0.6 | 0.0 |
| All countries | 27.5 | 8.0 | 19.3 | 0.2 |
We used data from the Slovak Centre of Organ Transplantation, the Organización Nacional de Trasplantes (ONT) and the Turkish Ministry of Health, for Slovakia, Spain and Turkey, respectively.
aData do not include Kiev city.
Patient and graft survival
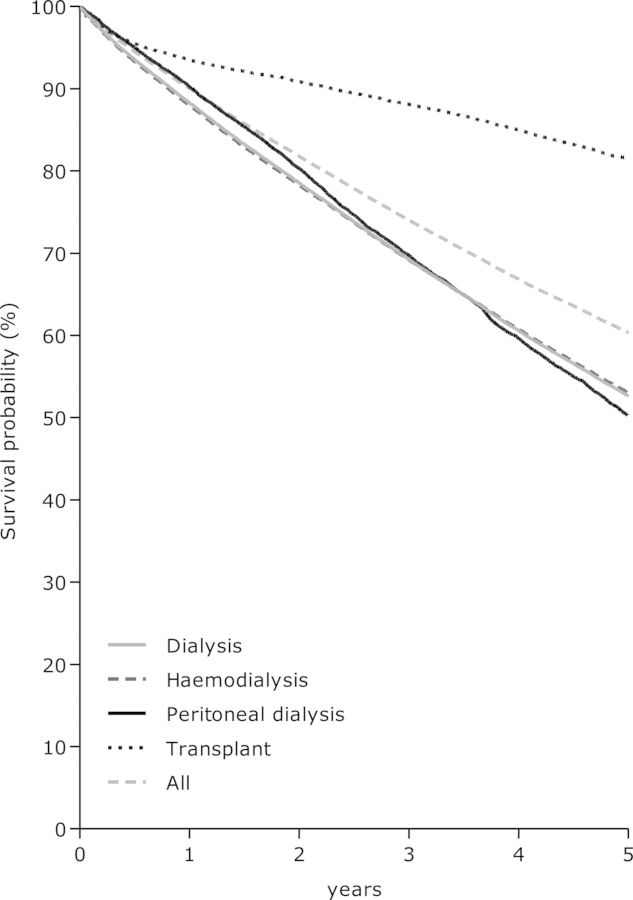
Survival analysis was performed using the data from 22 registries in 12 countries that provided individual patient records for the period from 2002 to 2009. The results of the unadjusted and adjusted survival analyses for all countries combined for all patients and for those aged 65 years and older are presented in Figure 4 and Table 11. The adjusted analyses for the total group of patients used fixed values for age, gender and distribution of primary renal disease, while the adjusted analyses in the group of patients ≥65 years were not adjusted for age. A more detailed description of the methods used for the survival analyses can be found in the Appendix.
Fig. 4.
Survival of incident dialysis patients and patients receiving a first renal transplant (between 2002 and 2006), from Day 91, by modality, adjusted for age, gender and primary diagnosis.
Table 11.
Unadjusted and adjusted 1-, 2- and 5-year survival probabilities (95% confidence interval) from the first day of RRT for patients who started RRT between 2002 and 2006 and 1- and 2-year survival probabilities for patients who started RRT between 2005 and 2009
| Cohort 2002–06a |
Cohort 2005–09b |
||||
|---|---|---|---|---|---|
| 1 year | 2 years | 5 years | 1 year | 2 years | |
| Patient survival on RRT | |||||
| All patients | |||||
| Unadjusted | 81.1 (80.9–81.3) | 69.8 (69.6–70.0) | 46.8 (46.6–47.0) | 82.7 (82.5–82.9) | 72.0 (71.8–72.2) |
| Adjusted | 88.3 (88.1–88.5) | 79.9 (79.7–80.2) | 58.6 (58.2–59.0) | 89.3 (89.1–89.5) | 81.6 (81.3–81.9) |
| 65+ years | |||||
| Unadjusted | 73.2 (72.9–73.5) | 57.7 (57.5–58.0) | 28.0 (27.9–28.1) | 75.3 (75.0–75.6) | 60.7 (60.5–60.9) |
| Adjusted | 74.9 (74.5–75.2) | 59.8 (59.4–60.3) | 29.8 (29.4–30.3) | 76.9 (76.5–77.2) | 62.7 (62.3–63.1) |
| Patient survival on dialysis | |||||
| All patients | |||||
| Unadjusted | 80.4 (80.2–80.6) | 67.8 (67.6–68.0) | 39.3 (39.2–39.4) | 81.8 (81.6–82.0) | 69.8 (69.6–70.1) |
| Adjusted | 86.5 (86.2–86.7) | 76.9 (76.5–77.2) | 51.6 (51.1–52.1) | 88.0 (87.8–88.2) | 79.2 (78.9–79.5) |
| 65+ years | |||||
| Unadjusted | 73.1 (72.8–73.4) | 57.4 (57.2–57.7) | 26.8 (26.7–26.9) | 75.1 (74.9–75.4) | 60.3 (60.0–60.5) |
| Adjusted | 74.5 (74.1–74.9) | 59.2 (58.7–59.6) | 28.1 (27.7–28.6) | 76.6 (76.2–76.9) | 62.1 (61.7–62.5) |
| Patient survival after first transplant (deceased donor) | |||||
| All patients | |||||
| Unadjusted | 95.5 (95.1–95.8) | 93.5 (93.1–93.9) | 86.7 (86.2–87.2) | 95.9 (95.6–96.1) | 93.8 (93.5–94.2) |
| Adjusted | 97.2 (96.9–97.4) | 95.9 (95.6–96.2) | 91.3 (90.8–91.8) | 97.3 (97.0–97.5) | 95.9 (95.6–96.2) |
| 65+ years | |||||
| Unadjusted | 88.0 (86.4–89.4) | 83.6 (81.9–85.1) | 69.3 (67.6–70.9) | 90.3 (89.0–91.5) | 85.8 (84.3–87.1) |
| Adjusted | 89.1 (87.5–90.7) | 85.1 (83.3–86.9) | 71.7 (69.4–74.0) | 91.3 (90.0–92.6) | 87.2 (85.6–88.7) |
| Patient survival after first transplant (living donor) | |||||
| All patients | |||||
| Unadjusted | 98.0 (97.5–98.4) | 97.1 (96.5–97.5) | 94.3 (93.6–95.0) | 98.2 (97.9–98.5) | 97.4 (96.9–97.7) |
| Adjusted | 98.2 (97.8–98.6) | 97.4 (96.9–97.9) | 94.8 (94.1–95.6) | 98.6 (98.3–98.9) | 98.0 (97.6–98.4) |
| 65+ years | |||||
| Unadjusted | 93.8 (89.7–96.3) | 90.2 (85.7–93.4) | 80.9 (76.0–85.0) | 94.6 (92.0–96.4) | 91.7 (88.7–93.9) |
| Adjusted | 95.2 (92.2–98.2) | 93.2 (89.8–96.7) | 84.8 (79.9–90.0) | 95.5 (93.5–97.6) | 93.5 (91.1–96.0) |
| Graft survival after first transplant (deceased donor) | |||||
| All patients | |||||
| Unadjusted | 89.8 (89.3–90.2) | 86.8 (86.3–87.3) | 77.2 (76.7–77.8) | 90.4 (90.0–90.8) | 87.3 (86.9–87.8) |
| Adjusted | 91.0 (90.5–91.4) | 88.3 (87.8–88.9) | 79.6 (78.9–80.3) | 91.4 (91.0–91.9) | 88.7 (88.2–89.2) |
| 65+ years | |||||
| Unadjusted | 81.1 (79.4–82.7) | 76.3 (74.6–78.0) | 61.4 (59.8–62.9) | 84.0 (82.5–85.4) | 79.4 (77.9–80.9) |
| Adjusted | 82.0 (80.1–84.0) | 77.4 (75.3–79.6) | 62.9 (60.4–65.5) | 84.6 (82.9–86.3) | 80.2 (78.3–82.1) |
| Graft survival after first transplant (living donor) | |||||
| All patients | |||||
| Unadjusted | 94.7 (94.0–95.3) | 92.9 (92.1–93.6) | 86.9 (85.9–87.7) | 95.4 (94.8–95.8) | 93.5 (92.9–94.1) |
| Adjusted | 94.5 (93.8–95.3) | 92.7 (91.9–93.6) | 86.6 (85.5–87.7) | 95.3 (94.8–95.9) | 93.5 (92.9–94.2) |
| 65+ years | |||||
| Unadjusted | 90.2 (85.7–93.4) | 85.6 (80.7–89.3) | 77.8 (72.9–82.0) | 92.5 (89.6–94.6) | 89.2 (86.1–91.7) |
| Adjusted | 91.3 (87.4–95.4) | 88.2 (83.7–92.9) | 80.9 (75.5–86.7) | 93.2 (90.7–95.8) | 90.7 (87.8–93.6) |
aThese analyses were based on data from Austria, Belgium (Dutch-speaking), Belgium (French-speaking), Denmark, Finland, Greece, Iceland, Italy (Calabria), Norway, Spain (Andalusia), Spain (Asturias), Spain (Basque Country), Spain (Cantabria), Spain (Catalonia), Spain (Valencian region), Sweden, the Netherlands, UK (England/Wales) and UK (Scotland).
bThese analyses were based on data from Austria, Belgium (Dutch-speaking), Belgium (French-speaking), Denmark, Finland, Greece, Iceland, Italy (Calabria), Norway, Spain (Andalusia), Spain (Asturias), Spain (Basque Country), Spain (Cantabria), Spain (Castile-La Mancha), Spain (Catalonia), Spain (Extremadura), Spain (Valencian region), Sweden, the Netherlands, UK (England/Wales), UK (Northern Ireland) and UK (Scotland).
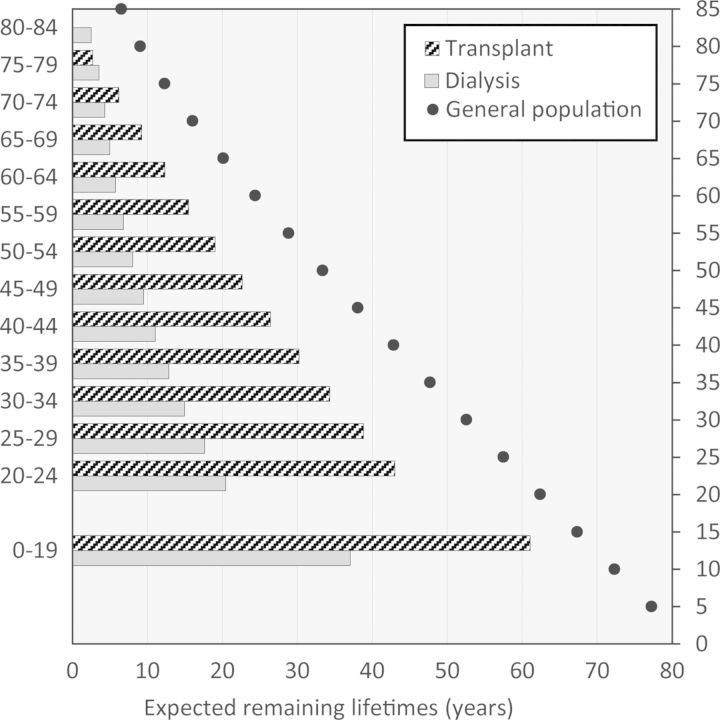
For the calculation of the expected remaining lifetimes, we used data from 18 national and regional renal registries in 11 countries that provided individual patient records for the period from 2000 to 2011. As is illustrated in Figure 5, the expected remaining lifetime for patients on RRT is much lower than for the general population. Particularly, the expected remaining lifetime of dialysis patients is strongly reduced when compared with that of transplant recipients, and it represents approximately one-third of the expected remaining lifetime of the general population. In addition to the RRT modality, age plays an important role: with a higher age, the reduction in expected remaining lifetime is less pronounced. In other words, the younger a patient the greater the reduction in expected remaining lifetime.
Fig. 5.
Expected remaining lifetimes of prevalent dialysis and renal transplant patients in 2010 and 2011 compared with the 2005 general population statistics.
Conflict of interest statement
None declared.
Acknowledgements
The ERA–EDTA Registry would like to thank the patients and staff of all the dialysis and transplant units who have contributed data via their national and regional renal registries. In addition, we thank the persons and organizations listed in the Appendix for their contribution to the work of the ERA–EDTA Registry. The ERA–EDTA Registry is funded by the European Renal Association–European Dialysis and Transplant Association (ERA–EDTA).
APPENDIX
Statistical methods
The results presented in Table 11 include the survival probabilities (%) of incident patients on RRT and of patients receiving a first renal transplant between 2002 and 2006 or between 2005 and 2009 with their 95% confidence intervals. Patients were followed until 31 December 2011. We used the Kaplan–Meier method to analyse the unadjusted patient survival, whereas the Cox regression model was used for the adjusted survival analyses for all patients and for the group of patients of aged 65 years and older.
For the analysis of patient survival on RRT, the first day of RRT was taken as the starting point and the event studied was death. Censored observations were recovery of renal function, loss to follow-up and end of follow-up time. In the Cox regression model for all patients, we adjusted for fixed values for age (60 years), gender (60% men) and primary renal disease (20% diabetes mellitus, 17% hypertension/renal vascular disease, 15% glomerulonephritis and 48% other cause). In the model for the patients aged ≥65 years, we used the same fixed values with the exception of age; in all Cox regression models used to analyse the survival in the older patients we did not adjust for age.
For the analysis of patient survival on dialysis, the first day on dialysis was the starting point, the event was death and reasons for censoring were recovery of renal function, loss to follow-up, end of follow-up time and renal transplantation. In the Cox regression model, we adjusted for fixed values of age (60 years), gender (60% men) and primary renal disease (20% diabetes mellitus, 17% hypertension/renal vascular disease, 15% glomerulonephritis and 48% other cause).
For the analysis of patient and graft survival after renal transplantation, the date of the first transplant was defined as the first day of follow-up. The event studied for the patient survival after transplantation was death, while for the graft survival the events were graft failure and death. Reasons for censoring were loss to follow-up and end of follow-up time. In the adjusted analyses in the total group, we adjusted for fixed values of age (45 years), gender (60% men) and primary renal disease (10% diabetes mellitus, 8% hypertension/renal vascular disease, 28% glomerulonephritis and 54% other cause).
Patients for whom age, gender or primary renal disease was missing were excluded from the analysis.
Affiliated registries
Albania: N. Thereska, A. Strakosha and N. Pasko; Austria: R. Kramar; Belgium, Dutch-speaking: H. Augustijn, B. De Moor and J. De Meester; Belgium, French-speaking: J.M. des Grottes and F. Collart; Bosnia–Herzegovina: H. Resić and B. Prnjavorac; Croatia: Croatian Registry for RRT, Croatian Regional Registries for RRT and Croatian Society for Nephrology, Dialysis and Transplantation; Czech Republic: I. Rychlík, J. Potucek and F. Lopot; Denmark: J.G. Heaf; Estonia: Ü. Pechter, M. Rosenberg and M. Luman; Finland: P. Finne and C. Grönhagen-Riska; France: M. Lassalle and C. Couchoud; FYR of Macedonia: O. Stojceva-Taneva; Greece: G.A. Ioannidis; Iceland: R. Palsson; Israel: R. Dichtiar, T. Shohat and E. Golan; Latvia: H. Cernevskis and V. Kuzema; Montenegro: M. Ratkovic, D. Radunovic and S. Ivanovic; Norway: T. Leivestad; Poland: B. Rutkowski, G. Korejwo and P. Jagodziński; Portugal: F. Macário, F. Nolasco and R. Filipe; Romania: G. Mircescu, L. Garneata and E. Podgoreanu; Russia: N.A. Tomilina and B.T. Bikbov; Serbia: Working group of Serbian RRT Registry and all of the Serbian renal units; Slovakia: V. Spustová, I. Lajdova and M. Karolyova; Spain, Andalusia: P. Castro de la Nuez; Spain, Aragon: J.I. Sanchez Miret and J.M. Abad Diez; Spain, Asturias: R. Alonso de la Torre, J.R. Quirós and E. Sanchez; Spain, Basque Country: Á. Magaz, J. Aranzabal, M. Rodrigo and I. Moina; Spain, Cantabria: M. Arias Rodríquez and O. García Ruiz; Spain, Castile and León: R. González and C. García-Renedo; Spain, Castile-La Mancha: G. Gutiérrez Ávila and I. Moreno Alía; Spain, Catalonia: E. Arcos Fuster, J. Comas Farnes and P.A. Montserrat; Spain, Extremadura: J.M. Ramos Aceitero and M.A. García Bazaga; Spain, Galicia: E. Bouzas-Caamaño and J. Sánchez-Ibáñez; Spain, Valencian region: O. Zurriaga Llorens and M. Ferrer Alamar; Spain: Spanish RRT National Registry at ONT, Spanish Regional Registries and Spanish Society of Nephrology; Sweden: K.G. Prütz, L. Bäckman, M. Evans, S. Schön, M. Stendahl and B. Rippe; the Netherlands: A. Hoitsma and A. Hemke; Turkey: G. Süleymanlar; Ukraine: M. Kolesnyk, G. Vladzievska and M. Kulyzkyi; UK, England/Northern Ireland/Wales: all the staff of the UK Renal Registry and of the renal units submitting data; UK, Scotland: all of the Scottish renal units.
ERA–EDTA Registry Committee Members
R. Vanholder, Belgium (ERA–EDTA President); C. Wanner, Germany (Chairman); F.J. Caskey, UK; F. Collart, Belgium; C. Couchoud, France; D. Fouque, France; J.W. Groothoff, the Netherlands; J.G. Heaf, Denmark; P. Ravani, Italy; I. Rychlik, Czech Republic; F. Schaefer, Germany; S. Schön, Sweden.
ERA–EDTA Registry Office Staff
K.J. Jager (Managing Director), R. Cornet, F.W. Dekker, A. Kramer, M.W.M. van de Luijtgaarden, M. Noordzij, M. Pippias, V.S. Stel, K.J. van Stralen and A.J. Weerstra.
References
- 1.ERA-EDTA Registry. Amsterdam, the Netherlands: Academic Medical Center, Department of Medical Informatics; 2013. ERA-EDTA Registry Annual Report 2011. [Google Scholar]