Abstract
Decompression illness is a rare but serious complication of diving caused by intravascular or extravascular gas bubble formation. We report the first case of acute kidney injury in a 27-year-old diver following three rapid ascents. He presented with transient neurological symptoms and abdominal pain followed by rapidly progressive acute kidney injury (creatinine peak 1210 µmol/L) due to arterial air emboli. He received supportive care and 100% oxygen followed by hyperbaric therapy and recovered fully. Arterial air emboli caused by rapid decompression can affect multiple organs including the kidneys. Early transfer to a hyperbaric unit is important as complications may present delayed.
Keywords: acute kidney injury, arterial air embolism, decompression illness, pulmonary barotrauma
Background
Decompression illness is caused by intravascular or extravascular gas bubble formation following rapid reduction in environmental pressure as seen with diving accidents. It comprises two different pathophysiological syndromes: decompression sickness and arterial air embolism caused by pulmonary barotrauma [1]. Decompression sickness can occur when a diver's time at depth leads to supersaturation of dissolved gases (usually nitrogen) and bubble formation during decompression. When the rate of ambient pressure reduction exceeds the rate of inert gas washout from tissue, formation of gas bubbles in the extravascular tissue may lead to tissue injury, vessel obstruction and organ dysfunction [2]. Arterial air embolism occurs when expanding gas ruptures alveolar capillaries (pulmonary barotrauma) and enters the arterial circulation as a result of rapid decompression. This is typically seen with rapid uncontrolled ascents especially in the setting of breath-holding or the presence of an underlying lung disease (with reduced compliance). Pulmonary barotrauma occurs in ∼4% of recreational divers who present with decompression illness [3]. Clinical manifestations depend on the site of embolization. Typical manifestations include cerebral symptoms (weakness, numbness, confusion or unconsciousness, seizure, visual disturbances, headaches and vertigo) when bubbles rupture into vessels, or respiratory symptoms (pleuritic chest pain due to pneumothorax or pneumomediastinum) when bubbles rupture into pleural spaces. However, other sites including muscles, mesenteric circulation, cardiovascular system and, as shown in the following case, the kidneys may also be involved.
Case report
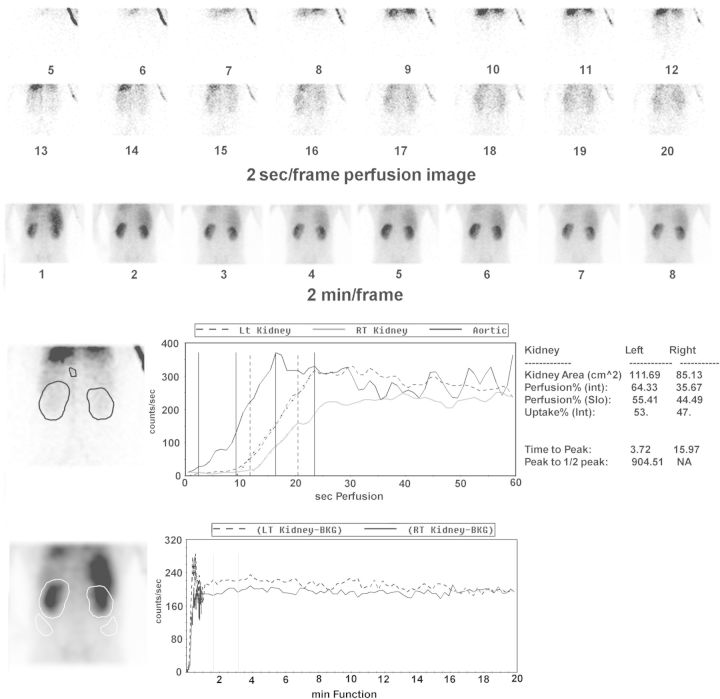
We report the first case of acute kidney injury caused by arterial air embolism injury in a 27-year-old Caucasian recreational diver following three rapid ascents. He was spear fishing on surface supply hookah at a depth of 15 metres for around 15 min when strong currents took him up to the surface whilst he was holding his breath attempting to reload his speargun. He had another two attempts to rescue his gear from the seafloor, but he was taken up by the swell each time. During the third ascent he became confused and when reaching the surface, his vision became blurred and he was unable to move his limbs. Rescued to the boat, he was made to rest in a supine position. On arrival at the local hospital he was normotensive and his neurological symptoms resolved within a few hours. Due to initial pleuritic chest pain, a computer tomography was performed which showed normal lung parenchyma and no evidence of pneumothorax or pneumomediastinum. Nine hours after the incident, he developed diffuse abdominal pain with an initial lactate 10.8 mmol/L. Further imaging to look for ischaemic gut was not performed as he responded well to initial therapy consisting of 100% oxygen, analgesia with paracetamol and fentanyl (two doses, each 25 µg intravenously) and intravenous hydration and his lactate level returned to normal within a few hours. Due to rapidly evolving acute kidney injury, he was transferred to a tertiary hospital for hyperbaric therapy on Day 2 post-diving accident (initial creatinine 120 µmol/L, 987 µmol/L on Day 2 and peak at 1210 µmol/L on Day 4). The diagnosis of ischaemic-induced acute tubular necrosis (ATN) was supported by a high fractional urinary sodium excretion of 5.5%, elevated lactate dehydrogenase [486U/L (125–250)], normal urine sediment and urinary tract ultrasound and a MAG3 scan in keeping with ATN (Figure 1). The absence of myoglobinuria and only moderately elevated creatine kinase [maximum 893U/L (30–170)] made rhabdomyoloysis-induced ATN unlikely. Other causes of acute kidney injury were excluded by physical examination and comprehensive history. He received supportive care with intravenous hydration, sodium bicarbonate combined with a total of seven sessions of HBO and recovered fully without needing dialysis (Figure 2).
Fig. 1.
Tc-99m-MAG3 scan performed on Day 4 post-diving accident: the first two panels show the perfusion of both kidneys over 32 s (2 s/frame) and the third panel shows tracer concentration (reflecting renal function) over 16 min (2 min/frame). The top graph (renogram) shows normal perfusion of the left and right kidney and the bottom graph illustrates tracer retention in the left and right kidney in keeping with acute tubular necrosis.
Fig. 2.
Time line of creatinine (µmol/L) and clinical symptoms.
Discussion
Decompression illness due to arterial air embolism following rapid ascent is a serious diving complication and can present with multi-organ involvement including the kidneys as demonstrated in this case. Upon rescue onto the support boat the patient was positioned supine whilst the boat was rocking in the waves, which may have contributed to embolization at multiple sites, including the central nervous system, the mesenteric circulation, as suggested by elevated lactate and abdominal pain and the kidneys. The diagnosis of decompression illness is made on clinical grounds since gas bubbles are rarely detectable on imaging [1]. The most common symptoms of decompression sickness are localized pain, numbness/paresthesia and muscular weakness, typically presenting within the first 24 h, whereas symptoms of air embolism from pulmonary barotrauma occur immediately upon ascent [4, 5]. Although no diagnostic blood test exists for air embolism, widespread air embolization has been reported to result in elevated serum creatine kinase of up to 900 U/L [6], as was the case in our patient. The distinction between pulmonary barotrauma and decompression sickness is sometimes difficult and generally unnecessary as recompression is the treatment of choice for both. When hyperbaric therapy is not readily available, the best first aid treatment comprises administration of 100% oxygen and supportive care. However, early transfer to a hyperbaric treatment unit is important as symptoms may evolve over time as shown in our patient. Hyperbaric oxygen (HBO) leads to quick elimination of gas bubbles by reducing bubble size via increased pressure (Boyle's Law), increasing the inert gas partial pressure gradients between tissue and alveolar gas (increased nitrogen washout) and also oxygenates ischaemic tissue and exerts an anti-inflammatory effect [1, 7, 8]. The addition of non-steroidal anti-inflammatory drugs such as tenoxicam may decrease the number of HBO sessions required as shown in a randomized trial [8], but their use does no longer make part of the routine treatment and was not an option for our patient in the setting of acute kidney injury. HBO results in complete resolution of symptoms in most cases, whereas mild residual symptoms may persist in a few and serious complications in a minority of cases. The primary goal, however, remains the prevention of pulmonary barotrauma, a potentially fatal complication of diving. Divers should be screened during dive medical for conditions predisposing to barotrauma (airway obstruction, bullae, reduced lung compliance) and diving courses emphasize the importance of controlled ascent and avoiding breath-holding.
Authors' contribution
A.V.: patient diagnosis and management, literature search and writing of the paper; J.J.: patient management; A.W.: patient management; literature search and writing of the paper; N.B.: patient management; literature search and writing of the paper; and P.F.: management, literature search and writing of the paper.
Conflict of interest statement
None declared.
Acknowledgements
We thank Professor Harvey Turner and Philip Calais for providing the nuclear images of the Tc-99m-MAG 3 scan.
References
- 1.Vann RD, Butler FK, Mitchell SJ, et al. Decompression illness. Lancet. 2011;377:153–164. doi: 10.1016/S0140-6736(10)61085-9. [DOI] [PubMed] [Google Scholar]
- 2.Russi EW. Diving and the risk of barotrauma. Thorax. 1998;53(Suppl 2):S20–S24. doi: 10.1136/thx.53.2008.s20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pollock NW. Annual Diving Report: 2008 Edition. Durham, NC: Divers Alert Network; 2008. [PubMed] [Google Scholar]
- 4.Bove AA. Medical disorders related to diving. J Intensive Care Med. 2002;17:75–86. [Google Scholar]
- 5.US Navy Diving Manual. NAVSEA 00994 LP001 9010. Washington, DC: U.S. Government Printing Office; 1993. pp. 122–122. [Google Scholar]
- 6.Smith R, Neuman T. Elevation of serum creatine kinase in divers with arterial gas embolism. N Engl J Med. 1994;330:19–24. doi: 10.1056/NEJM199401063300104. [DOI] [PubMed] [Google Scholar]
- 7.Sumen G, Cimsit M, Eroglu L. Hyperbaric oxygen treatment reduces carrageenan-induced acute inflammation in rats. Eur J Pharmacol. 2001;431:265–268. doi: 10.1016/s0014-2999(01)01446-7. [DOI] [PubMed] [Google Scholar]
- 8.Bennett MH, Lehm JP, Mitchell SJ, et al. Recompression and adjunctive therapy for decompression illness: a systematic review of randomized controlled trials. Anesth Analg. 2010;111:757–762. doi: 10.1213/ANE.0b013e3181cdb081. [DOI] [PubMed] [Google Scholar]