Abstract
The effects of fat-soluble vitamin supplementation on cardiovascular disease (CVD) risk are not clear. Therefore, we performed a meta-analysis to quantify effects of fat-soluble vitamin supplements on fasting flow-mediated vasodilation (FMD) of the brachial artery, a validated marker to assess CVD risk. Randomized placebo-controlled trials (RCTs) were identified by a systematic search till July 2014. Seven RCTs studying the effects of vitamin E supplements (range: 300 to 1800 IU per day) and nine RCTs examining the effects of vitamin D supplements, that involved, respectively, 303 and 658 adults, were included. No studies with carotenoid or vitamin K supplements were found. Vitamin E supplementation increased FMD vs. control by 2.42% (95% CI: 0.46% to 4.37%; p = 0.015). No effects of vitamin D supplementation were found (0.15%; 95% CI: −0.21% to 0.51%; p = 0.41). These effects did not depend on subject characteristics, treatment characteristics or technical aspects of the FMD measurement. However, no dose-response relationship was evident for vitamin E, statistical significance depended on one study, while the levels of supplement were far above recommended intakes. The current meta-analysis, therefore, does not provide unambiguous evidence to support the use of fat-soluble vitamin supplements to improve fasting FMD in adults.
Keywords: flow-mediated vasodilation, fat-soluble, vitamin D, vitamin E, meta-analysis
1. Introduction
Observational studies have found inverse associations between the use of fat-soluble vitamin supplements and cardiovascular disease (CVD) risk. However, data from intervention trials are in general disappointing, while for some of the fat-soluble vitamins hardly any data are available [1]. Alternatively, effects of these essential micronutrients on validated markers of CVD, such as vascular function markers can be studied [2]. Measurements of vascular endothelial function, which is a powerful predictor of atherosclerotic disease progression and cardiovascular event rates [3], may indeed be useful to demonstrate CVD benefits [4]. Unfortunately, results of studies on the effects of fat-soluble vitamin supplementation on flow-mediated vasodilation (FMD) of the brachial artery, which is considered as the non-invasive gold standard technique to assess vascular endothelial function [5], were not consistent.
Several papers have therefore summarized the results for vitamin E and vitamin D. Montero and colleagues concluded that longer-term antioxidant vitamin supplementation could improve endothelial function in non-obese adults [6], but (i) only studies involving subjects with type II diabetes were included and (ii) effects of vitamin E could not be untangled from the known positive relationship between vitamin C and endothelial function [7]. Further, Min [8] and Liu et al. [9] reviewed clinical studies focusing on vitamin D supplementation and endothelial function, but results were equivocal. Also, quantitative estimates of effect sizes were lacking [8,9] and results of several relevant clinical trials were not included [8]. We therefore performed a meta-analysis of randomized placebo-controlled trials (RCTs) on the effects of fat-soluble vitamin supplementation on fasting FMD in adults. Further, the impact of (i) subject characteristics; (ii) treatment characteristics; and (iii) technical aspects of the FMD measurement on the effects observed on FMD was examined.
2. Experimental Section
The present meta-analysis was reported according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [10].
2.1. Search Strategy
Potentially relevant studies were identified by a systematic search of Medline, Embase and the Cochrane Library database (Cochrane Central Register of Clinical Trials) till July 2014. The following search terms were used to search in titles and abstracts: (vitamin or supplement or calciferol or tocopherol or tocotrienol or retinol or carotenoid or carotene) and (flow mediated vasodilation (or vasodilatation or dilation or dilatation) or endothelial (or endothelium) dependent vasodilation (or vasodilatation or dilation or dilatation) or endothelial (or endothelium) function (or dysfunction) or FMD or vascular reactivity or brachial artery). The search was limited to studies in humans and to the English language. Reference lists from the selected articles were also screened manually for potentially relevant publications.
2.2. Selection of Trials
Randomized placebo-controlled trials, which investigated the relationship between fat-soluble vitamin supplementation and fasting FMD of the brachial artery with parallel and crossover designs, were selected.
The selection was performed in two steps. First, titles and abstracts were screened. Studies were selected if they met the following inclusion criteria: human intervention study with adults, intervention with fat-soluble vitamin supplements as experimental variable, no intentional co-intervention that made it impossible to estimate the effect of fat-soluble vitamin supplementation, and assessment of fasting vascular endothelial function by measuring FMD. In the second step, full-texts of the selected articles were read and studies were excluded based on the following criteria: no full text available (conference abstracts), missing data on FMD, no appropriate measures of variability reported, intentional co-intervention and no suitable placebo control treatment (prospective cohort studies). Both authors (Peter J. Joris and Ronald P. Mensink) completed the systematic literature search independently. When inconclusive, eligibility was discussed until consensus was reached.
2.3. Data Extraction
For each of the selected studies, data were extracted using a custom-made database including identification of the study (first author’s name and year of publication), study design (parallel or crossover), subject characteristics (sample size, age, gender, body mass index (BMI), baseline FMD level, and health status), treatment characteristics (type of vitamin supplements, total supplement dose and duration of follow-up), technical aspects of the FMD measurement (position of cuff and time of occlusion) and FMD values with accompanying measures of variance. For vitamin E, doses in mg were transformed into international units (IU) [11].
2.4. Statistical Analysis
Statistical analyses were performed using Stata 12.1 software (Stata Corporation, College Station, TX, USA). The FMD response was quantified as the maximal percentage change in post occlusion arterial diameter relative to baseline diameter, which is the diameter of the brachial artery before the introduction of a flow stimulus in the artery. The post occlusion arterial diameter is the diameter observed within minutes of reperfusion following the release of an inflated cuff.
For crossover trials, the net response in FMD was calculated by subtracting the mean FMD value at the end of the control period from the mean FMD value at the end of the treatment period. For parallel studies, mean changes in the control group were subtracted from mean changes in the intervention group. Mean changes were defined as the difference between measurements before (start-of-the-study values) and after the study (end-of-the-study values). For trials in which different doses of vitamin supplements were supplied or that performed FMD measurements more than one time during the study, multiple study arms were considered.
As described in [12], summary estimates of weighted mean differences (WMDs) in FMD and 95% confidence intervals (CIs) were calculated using fixed-effect meta-analyses and visualized using forest plots. The inverse of the variance (1/SE2) (SE = within-study variance) was used as weight factor. Heterogeneity was evaluated using the Cochran’s Q test (p < 0.1 indicates statistical significant heterogeneity) and quantified using the I2 statistic [13,14,15], i.e., the percentage of variability in effect estimate that is due to heterogeneity rather than sampling error. An I2 value above 50% indicates relevant heterogeneity between studies [16]. In case of heterogeneity, random-effect meta-analyses were used as described by DerSimonian and Laird [14].
As it was evident that the type of vitamin supplement was an important source of heterogeneity, first a vitamin E and a vitamin D group were defined. Subgroup analyses were performed within each vitamin group to identify sources of heterogeneity between studies by comparing the summary results of the study arms grouped by subject characteristics (i.e., mean age, gender, baseline BMI, baseline FMD level and health status), treatment characteristics (i.e., type of vitamin supplement, total supplement dose and duration of follow-up) and technical aspects of the FMD measurement (position of cuff and time of occlusion). Median values of continuous variables were used as cutoff values to create the binary variables. Univariate meta-regression analysis was performed to investigate the effect of the dose of the vitamin supplement and other characteristics on the change in FMD. For all statistical analyses, two-sided tests were used. Statistical significance was set at p < 0.05. Publication bias was finally evaluated visually by inspecting the symmetry of funnel plots. The degree of funnel plot asymmetry was assessed with the Egger’s weighted regression test. Absence of publication bias is reflected in an intercept close to 0 with a corresponding p ≥ 0.05 [17].
3. Results
3.1. Search Results and Study Selection
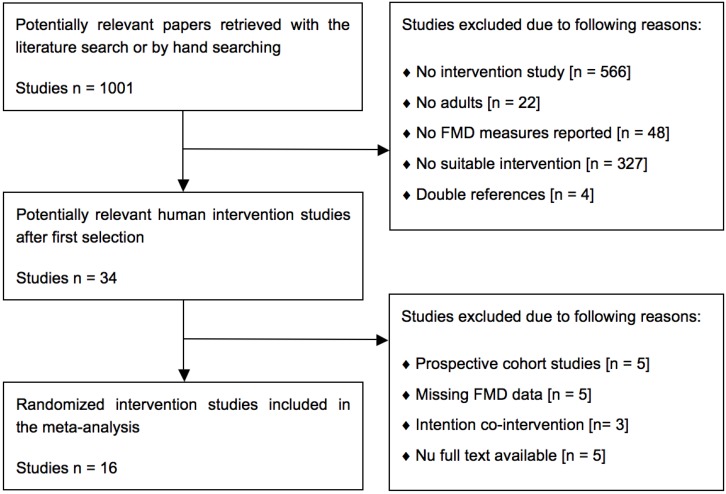
A total of 1001 potentially relevant papers were retrieved with the systematic search. Based on the predefined selection criteria, 967 papers were excluded for different reasons (Figure 1). The full texts of the remaining 34 articles were reviewed and eighteen papers were excluded for the following reasons: prospective cohort studies [18,19,20,21,22], missing data on FMD [23,24,25,26,27], no appropriate measures of variability reported [18], intentional co-intervention [28,29,30], or no full text available (five conference abstracts). A total of sixteen RCTs in adult volunteers with parallel [31,32,33,34,35,36,37,38,39,40,41,42,43,44,45] or crossover designs [46] met all the inclusion criteria and were finally included (Table 1). In seven studies, effects of vitamin E [31,32,35,37,38,39,46] were examined and in nine studies, those of vitamin D [33,34,36,40,41,42,43,44,45]. No intervention studies were found that examined the effects of carotenoid or vitamin K supplements.
Figure 1.
Flow diagram showing the study selection procedure of human intervention studies for the meta-analysis of fat-soluble vitamin supplements and endothelial function as measured by flow-mediated vasodilation (FMD), with the specification of reasons.
Table 1.
Overview of randomized placebo-controlled trials included in the meta-analysis.
| First Author and Year | Subject Characteristics | Treatment Characteristics | FMD Measurement Characteristics | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Design 1 | Number | Male (%) | Age (Y) | BMI (kg/m2) | Health Status | Treatment 2 | Dose 3 | Duration | Cuff | Occlusion | Baseline (%) | |||||||
| Randomized controlled trials (RCTs) with vitamin E supplements as experimental variable 4 | ||||||||||||||||||
| Borovničar, 2000 (31) | P | 22/22 | 100/100 | 45.0/45.0 | -/- | High cholesterol | Toco-acetate | 889 IU/day | 6 months | Distal | 4.0 min | 6.20/6.50 | ||||||
| Economides, 2005 (32) | P | 32/31 | 53.9/53.9 | 53.0/53.0 | 29.2/29.2 | Type I/II diabetes | All-racemic α-Toc | 1800 IU/day | 12 months | - | - | 5.80/5.80 | ||||||
| Economides, 2005 (32) | P | 34/32 | 53.9/53.9 | 53.0/53.0 | 29.2/29.2 | Type I/II diabetes | All-racemic α-Toc | 1800 IU/day | 6 months | - | - | 5.70/5.70 | ||||||
| Kugiyama, 1999 (35) | P | 35/35 | 40.0/45.7 | 59.8/60.1 | 23.1/23.1 | Chest pain | α-Toco-acetate | 300 IU/day | 4 weeks | Distal | 5.0 min | 5.04/5.02 | ||||||
| Neunteufl, 2000 (37) | P | 11/11 | 100/100 | 28.0/27.0 | -/- | Smokers | All-racemic α-Toc | 600 IU/day | 4 weeks | Proximal | 4.5 min | 5.30/6.40 | ||||||
| Paolisso, 2000 (38) | P | 20/20 | 45.0/60.0 | 58.3/56.7 | 27.6/27.4 | Type II diabetes | Vitamin E | 1333 IU/day | 8 weeks | Proximal | 5.5 min | 1.83/1.71 | ||||||
| Simons, 1999 (46) | CO | 20/- | 65.0/- | 57.0/- | 27.5/- | Healthy | RRR D-α-Toco | 1000 IU/day | 10 weeks | Distal | 4.5 min | 2.70/- | ||||||
| Skyrme-Jones, 2000 (39) | P | 20/21 | 47.6/45.0 | 23.0/28.0 | 24.3/25.5 | Type I diabetes | All-racemic α-Toc | 1000 IU/day | 3 months | - | 5.0 min | 2.60/2.40 | ||||||
| Randomized controlled trials (RCTs) with vitamin D supplements as experimental variable 5 | ||||||||||||||||||
| Gepner, 2012 (33) | P | 55/55 | 00.0/00.0 | 64.1/63.6 | 27.1/25.3 | Post-menopausal | Vitamin D3 | 2500 IU/day | 4 months | Distal | 5.0 min | 5.05/4.57 | ||||||
| Harris, 2011 (34) | P | 22/23 | 41.0/52.0 | 29.0/31.0 | 30.4/29.1 | African American | Vitamin D3 | 2000 IU/day | 16 weeks | Distal | 5.0 min | 7.23/6.55 | ||||||
| Longenecker, 2012 (36) | P | 30/15 | 83.3/66.7 | 47.0/10.0 | 28.0/27.0 | HIV-infected | Vitamin D3 | 4000 IU/day | 12 weeks | Distal | 5.0 min | 2.87/2.46 | ||||||
| Sugden, 2008 (40) | P | 17/17 | 58.8/47.1 | 64.9/63.5 | 31.7/31.7 | Type II diabetes | Vitamin D2 | 100K IU (0) | 8 weeks | Distal | 5.0 min | 6.38/7.28 | ||||||
| Witham, 2010 (42) | P | 19/21 | 84.2/54.5 | 65.3/66.7 | 31.1/33.3 | Type II diabetes | Vitamin D3 | 100K IU (0) | 16 weeks | Distal | - | 5.10/5.40 | ||||||
| Witham, 2010 (42) | P | 18/21 | 65.0/54.5 | 63.3/66.7 | 29.7/33.3 | Type II diabetes | Vitamin D3 | 200K IU (0) | 16 weeks | Distal | - | 6.40/5.40 | ||||||
| Witham, 2010 (42) | P | 19/22 | 84.2/54.5 | 65.3/66.7 | 31.1/33.3 | Type II diabetes | Vitamin D3 | 100K IU (0) | 8 weeks | Distal | - | 5.10/5.40 | ||||||
| Witham, 2010 (42) | P | 17/22 | 65.0/54.5 | 63.3/66.7 | 29.7/33.3 | Type II diabetes | Vitamin D3 | 200K IU (0) | 8 weeks | Distal | - | 6.40/5.40 | ||||||
| Witham, 2012 (43) | P | 28/27 | 60.0/85.7 | 66.2/67.7 | 27.3/26.1 | History stroke | Vitamin D2 | 100K IU (0) | 16 weeks | Distal | 5.0 min | 6.90/5.60 | ||||||
| Witham, 2012 (43) | P | 29/27 | 60.0/85.7 | 66.2/67.7 | 27.3/26.1 | History stroke | Vitamin D2 | 100K IU (0) | 8 weeks | Distal | 5.0 min | 6.90/5.60 | ||||||
| Witham, 2013 (44) | P | 80/79 | 50.0/53.2 | 76.9/76.7 | 28.5/27.9 | High systolic BP | Vitamin D3 | 100K IU (3) | 12 months | Distal | 5.0 min | 5.10/5.10 | ||||||
| Witham, 2013 (44) | P | 80/79 | 50.0/53.2 | 76.9/76.7 | 28.5/27.9 | High systolic BP | Vitamin D3 | 100K IU (0) | 3 months | Distal | 5.0 min | 5.10/5.10 | ||||||
| Witham, 2013 (41) | P | 25/25 | 00.0/00.0 | 41.7/39.4 | 24.9/28.7 | South Asian | Vitamin D3 | 100K IU (0) | 8 weeks | Distal | 5.0 min | 8.20/8.70 | ||||||
| Witham, 2013 (41) | P | 25/25 | 00.0/00.0 | 41.7/39.4 | 24.9/28.7 | South Asian | Vitamin D3 | 100K IU (0) | 4 weeks | Distal | 5.0 min | 8.20/8.70 | ||||||
| Yiu, 2013 (45) | P | 50/50 | 54.0/46.0 | 65.8/64.9 | 25.8/25.1 | Type II diabetes | Vitamin D3 | 5000 IU/day | 12 weeks | Distal | 5.0 min | 3.39/3.40 | ||||||
1 Study design: randomized placebo-controlled parallel (P) or crossover (CO) trials; 2 Study treatments as described by the authors. Toc: tocopherol, Vitamin D2: oral ergocalciferol, Vitamin D3: oral cholecalciferol; 3 Doses in mg were transformed to international units (IU) according to vitamin E guidelines. Supplement received once (0) or every three months (3); 4 n = 7 intervention studies (experimental group/control group) with eight relevant study arms; 5 n = 9 intervention studies (experimental group/control group) with 15 relevant study arms.
3.2. Study Characteristics
In six parallel studies [31,32,35,37,38,39] and in one crossover [46] trial, effects of vitamin E were examined. These studies provided eight relevant study arms and included 303 subjects. The number of subjects per study ranged from 20 to 70, the mean age of the participants from 23.0 to 59.8 years, and the mean BMI from 23.1 to 29.2 kg/m2. The mean baseline FMD was 4.40% (range: 1.83% to 6.20%). Two studies included only men [31,37], whereas the proportion of men in the remaining studies ranged from 40.0% to 60.0%. In two studies, healthy elderly [46] or healthy smoking adults [37] were included, in three studies patients with diabetes [32,38,39], whereas in two studies subjects had hypercholesterolemia [31] or atypical chest pain [35]. Study duration varied between four weeks and twelve months, and the daily dose of vitamin E from 300 to 1800 IU (mean: 1090 IU/day; Table 1).
For vitamin D, nine RCTs with parallel designs [33,34,36,40,41,42,43,44,45] were identified including a total of fifteen study arms. In these studies, 658 subjects participated, 345 in the treatment groups and 313 in the control groups. The mean age of the subjects was 59.8 years (range: 29.0 to 76.9 years), BMI was 28.4 kg/m2 (range: 24.9 to 31.7 kg/m2), and half of the study population was men. In three studies, healthy women [33,41] or African American adults [34] were included; the other studies included subjects with type II diabetes [40,42,45], isolated systolic hypertension [44], HIV infection [36], or a history of stroke [43]. In two studies [40,43], a single dose of 100,000 IU of vitamin D2 was administered. The dose of the vitamin D3 supplement in the other studies ranged from 2000 to 5000 IU/day [33,34,36,45], or subjects received a total of 100,000 to 200,000 IU once or every three months [41,42,44]. Study duration ranged from four weeks to twelve months (Table 1).
3.3. Effect of Vitamin Supplementation on FMD
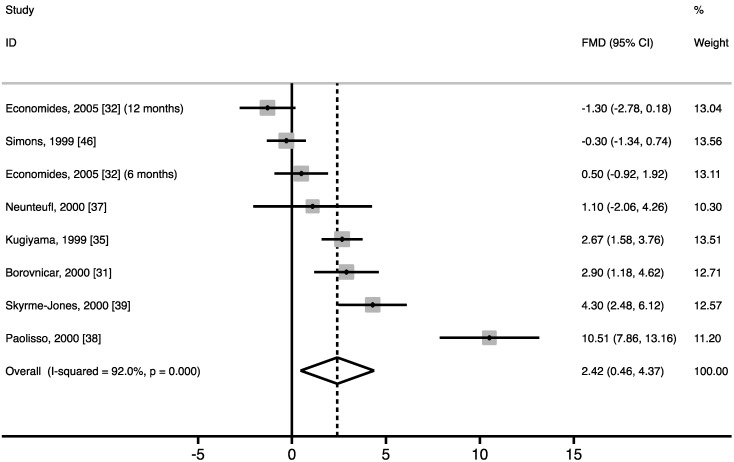
Vitamin E supplementation increased fasting FMD vs. control by 2.42% (95% CI: 0.46% to 4.37%; p = 0.015) (Figure 2), corresponding to a relative increase of approximately 50% compared with baseline FMD values. However, significant heterogeneity was found (I2 = 92.0%, p < 0.001). Results of the meta-regression analysis showed no linear dose-response relationship between the dose of the vitamin E supplement and the change in FMD (p = 0.774; Figure S1). Analyses were repeated after excluding the study of Paolisso and colleagues [38], which had the most pronounced effect (10.5%). The overall WMD in FMD decreased and nearly reached statistical significance (1.38%; 95% CI: −0.12% to 2.87%; p = 0.070). No linear dose-response relationship was found between the dose of the vitamin E supplement and the change in FMD (p = 0.161). Even though heterogeneity decreased, it remained significant (I2 = 85.8%, p < 0.001).
Figure 2.
Forest plot of random controlled trials (RCTs) that investigated the effect of vitamin E supplements on flow-mediated vasodilation (FMD). The solid squares represent the weight of individual studies and the diamond represents the weighted mean difference (WMD) in FMD (calculated using random-effect meta-analyses). In all studies combined, vitamin E increased FMD vs. control by 2.42% (95% CI: 0.46% to 4.37%; p = 0.015). After excluding the study by Paolisso and colleagues [38], the overall WMD nearly reached statistical significance (1.38%; 95% CI: −0.12% to 2.87%; p = 0.070).
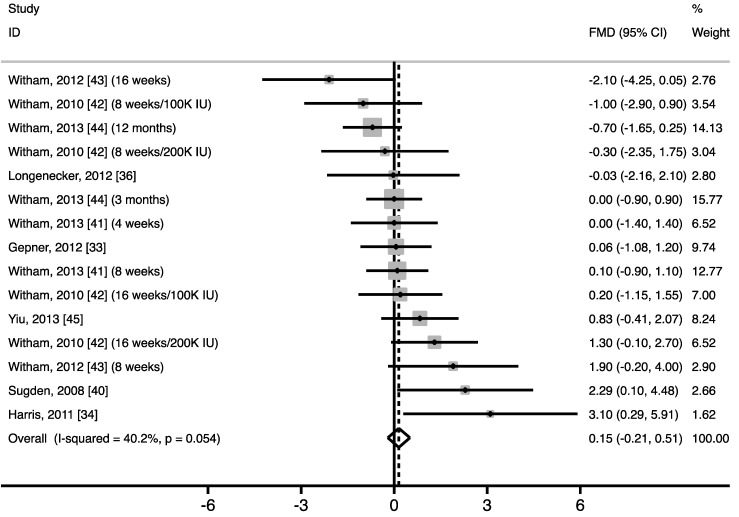
Vitamin D supplementation did not significantly improve fasting FMD of the brachial artery vs. control (0.15%; 95% CI: −0.21% to 0.51%; p = 0.41) (Figure 3). Between-study heterogeneity nearly reached statistical significance (I2 = 40.2%, p = 0.054). After using only results of the last measurement for trials that performed FMD measurements more than one time during the study [41,42,43,44], similar results were found for the overall WMD (0.33%; 95% CI: −0.34% to 1.00%; p = 0.34). Heterogeneity, however, became statistically significant (I2 = 52.5%, p = 0.026).
Figure 3.
Forest plot of random controlled trials (RCTs) that investigated the effect of vitamin D supplements on flow-mediated vasodilation (FMD). The solid squares represent the weight of individual studies and the diamond represents the weighted mean difference (WMD) in FMD (calculated using fixed-effect meta-analyses). In all studies combined, vitamin D did not increase FMD (WMD: 0.15%; 95% CI: −0.21% to 0.51%; p = 0.41).
3.4. Subgroup Analyses
Subgroup analyses were performed within each vitamin group to evaluate if subject characteristics, treatment characteristics or technical aspects of the FMD measurement were related to the effects observed (Table 2). None of the predefined variables resulted in significantly different effects of fat-soluble vitamin supplement intake on FMD between the subgroups. Further, the impact of baseline plasma 25-hydroxyvitamin D (25(OH)-D) concentrations and vitamin D-induced changes in 25(OH)-D was investigated, but no association with the change in fasting FMD was found (data not shown).
Table 2.
Subgroup analyses for the effect of fat-soluble vitamin E and vitamin D supplementation on fasting flow-mediated vasodilation (FMD) in adults.
| Study Characteristic | Mean | Stratification Variable | No of Study Arms | WMD (%) 1 | 95% CI (%) | p-value Difference |
|---|---|---|---|---|---|---|
| Study arms with vitamin E supplements as experimental variable 2 | ||||||
| Mean age (years) 3 | 47.1 | ≤53.0 | 5 | 1.48 | −0.59 to 3.55 | 0.372 |
| >53.0 | 3 | 4.08 | −0.25 to 8.41 | |||
| Gender (% male) 3 | 63.2 | ≤53.9 | 5 | 3.17 | 0.25 to 6.10 | 0.500 |
| >53.9 | 3 | 1.17 | −1.14 to 3.49 | |||
| Baseline BMI (kg/m2) 3 | 26.8 | ≤27.5 | 3 | 2.15 | −0.43 to 4.72 | 0.828 |
| >27.5 | 3 | 3.11 | −2.39 to 8.60 | |||
| Baseline FMD (%) 3 | 4.40 | ≤5.17 | 4 | 4.10 | 0.71 to 7.50 | 0.219 |
| >5.17 | 4 | 0.74 | −1.16 to 2.63 | |||
| Health status | - | Healthy | 2 | −0.16 | −1.15 to 0.82 | 0.390 |
| Diseased | 6 | 3.10 | 0.67 to 5.54 | |||
| Dose (100 IU/day) 3 | 10.9 | ≤10.0 | 5 | 2.14 | 0.35 to 3.93 | 0.764 |
| >10.0 | 3 | 3.11 | −2.39 to 8.60 | |||
| Study duration (weeks) 3 | 16.8 | ≤11.0 | 4 | 3.39 | −0.19 to 6.97 | 0.523 |
| >11.0 | 4 | 1.56 | −0.83 to 3.94 | |||
| Position cuff | - | Distal | 3 | 1.40 | 0.71 to 2.09 | 0.341 |
| Proximal | 2 | 6.63 | 4.60 to 8.66 | |||
| Occlusion duration (min) 4 | 4.67 | ≤4.50 | 3 | 1.17 | −1.14 to 3.49 | 0.158 |
| >4.50 | 3 | 5.65 | 1.77 to 9.54 | |||
| Study arms with vitamin D supplements as experimental variable 4 | ||||||
| Mean age (years) 3 | 59.8< 44.9 | ≤64.9 | 8 | 0.45 | −0.09 to 0.98 | 0.263 |
| >64.9 | 7 | −0.10 | −0.59 to 0.38 | |||
| Gender (% male) 3 | 50.4 | ≤58.8 | 8 | 0.14 | −0.28 to 0.56 | 0.805 |
| >58.8 | 7 | 0.18 | −0.49 to 0.85 | |||
| Baseline BMI (kg/m2) 3 | 28.4 | ≤28.5 | 9 | −0.02 | −0.43 to 0.39 | 0.226 |
| >28.5 | 6 | 0.68 | −0.05 to 1.40 | |||
| Baseline FMD (%) 3 | 5.89 | ≤6.38 | 8 | 0.02 | −0.43 to 0.47 | 0.550 |
| >6.38 | 7 | 0.38 | −0.22 to 0.97 | |||
| Health status | - | Healthy | 4 | 0.23 | −0.42 to 0.87 | 0.820 |
| Diseased | 11 | 0.12 | −0.31 to 0.55 | |||
| Type of vitamin 5 | - | Vitamin D2 | 3 | 0.70 | −0.54 to 1.94 | 0.521 |
| Vitamin D3 | 12 | 0.10 | −0.27 to 0.47 | |||
| Study duration (weeks) 3 | 13.9 | ≤12.0 | 9 | 0.26 | −0.21 to 0.73 | 0.675 |
| >12.0 | 6 | −0.01 | −0.56 to 0.55 | |||
| Position cuff | - | Distal | 15 | 0.15 | −0.21 to 0.51 | - |
| Proximal | 0 | - | - | |||
| Occlusion duration (min) 4 | 5.00 | ≤5.00 | 11 | 0.12 | −0.28 to 0.52 | - |
| >5.00 | 0 | - | - | |||
1 WMD: Weighted mean difference in flow-mediated vasodilation; 2 n = 7 Intervention studies with eight relevant study arms; 3 Study arms were divided into subgroups based on their medians; 4 n = 9 intervention studies with 15 relevant study arms; 5 Vitamin D2: oral ergocalciferol, Vitamin D3: oral cholecalciferol.
3.5. Publication Bias
The funnel plot for the effect of vitamin E supplementation did not reveal possible presence of publication bias (Figure S2) and the Egger’s weighted regression test also showed no funnel plot asymmetry (p = 0.20). Similar results were found after visual evaluation of the funnel plot for the effect of vitamin D supplementation and the Egger’s test (p = 0.24) did not reach statistical significance, indicating absence of publication bias (Figure S3).
4. Discussion
In this meta-analysis, data from seven RCTs studying the effects of vitamin E supplements and from nine RCTs examining the effects of vitamin D supplements on fasting FMD in adults were pooled. When all studies were included, we found that vitamin E supplementation increased FMD of the brachial artery by 2.42%, while no effect of vitamin D supplementation was found. However, significant heterogeneity was found among the vitamin E trials.
The putative positive effects of vitamin E on FMD may be due to increased scavenging of oxygen free radicals by vitamin E or via improved plasma antioxidant defenses [38]. This may lower the quenching effect of free radicals on nitric oxide (NO), thereby improving NO bioavailability and endothelial function. Several studies, but not all [47,48], have further suggested that vitamin E supplementation increases insulin sensitivity [49,50], which may also improve endothelial function [39]. However, based on our results, the use of vitamin E supplements to improve FMD should still be questioned. First, no linear dose-response relationship was evident, which would have been strong evidence for a causal relationship. Also, the level of vitamin E tested in RCTs included in our meta-analysis ranged from 300 to 1800 IU/day, which is far above recommended intakes of 30 IU/day [51]. In fact, concern has been raised about potential adverse effects. One meta-analysis indeed concluded that high-dose vitamin E supplementation may increase all-cause mortality in trials supplying daily doses over 400 IU, that involved adults with chronic diseases [52]. In another meta-analysis, vitamin E given singly or in combination with other antioxidant supplements was also found to increase mortality in randomized primary and secondary prevention trials when trials with low methodological quality were excluded [53]. Further, the increment in FMD was not longer statistically significant when the study with the most pronounced effect was excluded [38]. The most pronounced effect (10.5%) substantially differed from the overall WMD in FMD of 2.42%. However, in that study, subjects had the lowest mean baseline FMD (2.00%), suggesting that a very specific population was studied. Participants were type II diabetics, but it is not likely that this explains the large effects. Two other studies were also carried out in diabetic patients with both lower (1000 IU) [39] and higher daily doses (1800 IU) of vitamin E [32], but effects were never as large as observed by Paolisso and colleagues [38]. Considering these uncertainties, the present results should therefore not be interpreted as conclusive evidence to support the use of vitamin E supplements to improve FMD.
Prospective cohort studies have reported associations between vitamin D deficiency [54] or low plasma 25(OH)-D [55] and incident CVD. Although in vitro and animal studies have suggested a role of vitamin D supplements on endothelial function [56], we found no effects of vitamin D supplements on fasting FMD in adults. Another possible explanation for the inverse relation between vitamin D and CVD may be through effects on blood pressure. However, effects of vitamin D on blood pressure are also inconclusive [8]. In addition, calcium intakes may modify possible effects of vitamin D status on associated health benefits [57], and concomitant calcium intake may thus be required to observe positive effects of vitamin D supplementation on fasting vascular endothelial function.
Finally, a number of observational studies have reported an inverse association between carotenoid intake and CVD risk [58]. However, intervention trials using β-carotene supplements have not supported the hypothesis that β-carotene reduces CVD [53,58]. Unfortunately, we found no studies that examined the effects of carotenoid supplements on FMD. Further, an inverse association between vitamin K2 intake and coronary heart disease was found [59] and an increased dietary intake of vitamin K was also associated with a reduced risk of cardiovascular mortality [60]. However, results from intervention trials are lacking and none of the included trials investigated the effect of vitamin K supplementation on brachial reactivity.
Significant heterogeneity was found between vitamin E trials and results of previous studies were indeed inconsistent. It has been speculated that various factors, including the mean age of participants [32,61], vitamin supplement dose [23,32,61] or duration of the intervention [23,32,61], may explain these inconsistent results. However, none of these or other predefined variables accounted for the variable effect of vitamin E supplementation interventions on FMD. Montero and colleagues found that effects of antioxidant vitamin supplementation on endothelial function did depend on the BMI of subjects [6]. Positive effects were only found in non-obese subjects, which were explained by an insufficient capacity of oral vitamin E intakes to overcome increased levels of oxidative stress [62]. However, only studies involving subjects with type II diabetes were included and effects of antioxidant vitamin E and vitamin C could not be separated in the intervention studies selected. Further, measurements of vascular endothelial function from different vascular regions were pooled and effects on FMD as such were not quantified. After vitamin D supplementation, there were also no predefined characteristics that were significantly related to the effects observed on fasting FMD. In an additional analysis, no association with baseline plasma 25(OH)-D concentrations or vitamin D-induced changes in 25(OH)-D was found. However, heterogeneity among vitamin D studies did not reach statistical significance.
A possible limitation of our meta-analysis is the variability in experimental designs that may have contributed to the heterogeneity observed among the included studies. Further, comparability of FMD measurements between centers is low [63] and may be another source of heterogeneity. Even though technical aspects of the FMD measurement were not significantly related to the effects observed, better standardization of the FMD technique is required to reduce variability between trials included in the meta-analysis.
5. Conclusions
In conclusion, a causal relationship between high-dose vitamin E supplementation and improved fasting FMD cannot be ascertained from the present meta-analysis, while no effects of vitamin D supplementation were found. Therefore, the current meta-analysis does not provide unambiguous evidence to support the use of fat-soluble vitamin supplements to improve vascular endothelial function in adults and more research is required.
Acknowledgments
The present study is funded by research grant CH001 from the TI Food and Nutrition, a public-private partnership on precompetitive research in food and nutrition. The public partners are responsible for the study design, data collection and analysis, decision to publish, and preparation of the manuscript. The private partners have contributed to the project through regular discussion.
Supplementary Files
Author Contributions
The authors’ responsibilities were as follows; Peter J. Joris: designed the study and conducted the literature review, performed the statistical analyses, interpreted the data, and wrote the manuscript; and Ronald P. Mensink: designed the study and conducted the literature review, interpreted the data, had overall responsibility for the study, and wrote the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Lichtenstein A.H. Nutrient supplements and cardiovascular disease: A heartbreaking story. J. Lipid Res. 2009;50:S429–S433. doi: 10.1194/jlr.R800027-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Widlansky M.E., Gokce N., Keaney J.F., Jr., Vita J.A. The clinical implications of endothelial dysfunction. J. Am. Coll. Cardiol. 2003;42:1149–1160. doi: 10.1016/S0735-1097(03)00994-X. [DOI] [PubMed] [Google Scholar]
- 3.Schachinger V., Britten M.B., Zeiher A.M. Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation. 2000;101:1899–1906. doi: 10.1161/01.CIR.101.16.1899. [DOI] [PubMed] [Google Scholar]
- 4.Cohn J.N., Quyyumi A.A., Hollenberg N.K., Jamerson K.A. Surrogate markers for cardiovascular disease: Functional markers. Circulation. 2004;109:31–46. doi: 10.1161/01.CIR.0000115207.45378.BC. [DOI] [PubMed] [Google Scholar]
- 5.Ellins E.A., Halcox J.P. Where are we heading with noninvasive clinical vascular physiology? Why and how should we assess endothelial function? Cardiol. Res. Pract. 2011;2011:870132. doi: 10.4061/2011/870132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Montero D., Walther G., Stehouwer C.D., Houben A.J., Beckman J.A., Vinet A. Effect of antioxidant vitamin supplementation on endothelial function in type 2 diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2014;15:107–116. doi: 10.1111/obr.12114. [DOI] [PubMed] [Google Scholar]
- 7.Ashor A.W., Lara J., Mathers J.C., Siervo M. Effect of vitamin C on endothelial function in health and disease: A systematic review and meta-analysis of randomised controlled trials. Atherosclerosis. 2014;235:9–20. doi: 10.1016/j.atherosclerosis.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Min B. Effects of vitamin D on blood pressure and endothelial function. Korean J. Physiol. Pharmacol. 2013;17:385–392. doi: 10.4196/kjpp.2013.17.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu Z.M., Woo J., Wu S.H., Ho S.C. The role of vitamin D in blood pressure, endothelial and renal function in postmenopausal women. Nutrients. 2013;5:2590–2610. doi: 10.3390/nu5072590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gotzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arab L., Barr S.I., Becking G.C. A Report of the Panel on Dietary Antioxidants and Related Compounds. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. National Academy Press; Washington, DC, USA: 2000. [Google Scholar]
- 12.Joris P.J., Zeegers M.P., Mensink R.P. Weight loss improves fasting flow-mediated vasodilation in adults: A meta-analysis of intervention studies. Atherosclerosis. 2014;239:21–30. doi: 10.1016/j.atherosclerosis.2014.12.056. [DOI] [PubMed] [Google Scholar]
- 13.Cochran W.G. The combination of estimates from different experiments. Biometrics. 1954;10:101–129. doi: 10.2307/3001666. [DOI] [Google Scholar]
- 14.DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 15.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 16.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Egger M., Davey S.G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Can M., Gunes M., Haliloglu O.A., Haklar G., Inanc N., Yavuz D.G., Direskeneli H. Effect of vitamin D deficiency and replacement on endothelial functions in Behçet's disease. Clin. Exp. Rheumatol. 2012;30:S57–S61. [PubMed] [Google Scholar]
- 19.Chitalia N., Ismail T., Tooth L., Boa F., Hampson G., Goldsmith D., Kaski J.C., Banerjee D. Impact of vitamin D supplementation on arterial vasomotion, stiffness and endothelial biomarkers in chronic kidney disease patients. PLoS One. 2014;9:e91363. doi: 10.1371/journal.pone.0091363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koh K.K., Blum A., Hathaway L., Mincemoyer R., Csako G., Waclawiw M.A., Panza J.A., Cannon R.O., 3rd. Vascular effects of estrogen and vitamin E therapies in postmenopausal women. Circulation. 1999;100:1851–1857. doi: 10.1161/01.CIR.100.18.1851. [DOI] [PubMed] [Google Scholar]
- 21.Stein J.H., Carlsson C.M., Papcke-Benson K., Aeschlimann S.E., Bodemer A., Carnes M., McBride P.E. The effects of lipid-lowering and antioxidant vitamin therapies on flow-mediated vasodilation of the brachial artery in older adults with hypercholesterolemia. J. Am. Coll. Cardiol. 2001;38:1806–1813. doi: 10.1016/S0735-1097(01)01650-3. [DOI] [PubMed] [Google Scholar]
- 22.Tarcin O., Yavuz D.G., Ozben B., Telli A., Ogunc A.V., Yuksel M., Toprak A., Yazici D., Sancak S., Deyneli O., et al. Effect of vitamin D deficiency and replacement on endothelial function in asymptomatic subjects. J. Clin. Endocrinol. Metab. 2009;94:4023–4030. doi: 10.1210/jc.2008-1212. [DOI] [PubMed] [Google Scholar]
- 23.Gazis A., White D.J., Page S.R., Cockcroft J.R. Effect of oral vitamin E (alpha-tocopherol) supplementation on vascular endothelial function in type 2 diabetes mellitus. Diabet Med. 1999;16:304–311. doi: 10.1046/j.1464-5491.1999.00049.x. [DOI] [PubMed] [Google Scholar]
- 24.Green D., OʼDriscoll G., Rankin J.M., Maiorana A.J., Taylor R.R. Beneficial effect of vitamin E administration on nitric oxide function in subjects with hypercholesterolaemia. Clin. Sci. (Lond) 1998;95:361–367. doi: 10.1042/CS19970304. [DOI] [PubMed] [Google Scholar]
- 25.Pinkney J.H., Downs L., Hopton M., Mackness M.I., Bolton C.H. Endothelial dysfunction in type 1 diabetes mellitus: Relationship with LDL oxidation and the effects of vitamin E. Diabet Med. 1999;16:993–999. doi: 10.1046/j.1464-5491.1999.00191.x. [DOI] [PubMed] [Google Scholar]
- 26.Shab-Bidar S., Neyestani T.R., Djazayery A., Eshraghian M.R., Houshiarrad A., Gharavi A., Kalayi A., Shariatzadeh N., Zahedirad M., Khalaji N., et al. Regular consumption of vitamin D-fortified yogurt drink (Doogh) improved endothelial biomarkers in subjects with type 2 diabetes: A randomized double-blind clinical trial. BMC Med. 2011;9:125. doi: 10.1186/1741-7015-9-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Witham M.D., Dove F.J., Khan F., Lang C.C., Belch J.J., Struthers A.D. Effects of vitamin D supplementation on markers of vascular function after myocardial infarction-a randomised controlled trial. Int. J. Cardiol. 2013;167:745–749. doi: 10.1016/j.ijcard.2012.03.054. [DOI] [PubMed] [Google Scholar]
- 28.Mah E., Pei R., Guo Y., Ballard K.D., Barker T., Rogers V.E., Parker B.A., Taylor A.W., Traber M.G., Volek J.S., et al. γ-Tocopherol-rich supplementation additively improves vascular endothelial function during smoking cessation. Free Radic. Biol. Med. 2013;65:1291–1299. doi: 10.1016/j.freeradbiomed.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 29.Motoyama T., Kawano H., Kugiyama K., Hirashima O., Ohgushi M., Tsunoda R., Moriyama Y., Miyao Y., Yoshimura M., Ogawa H., et al. Vitamin E administration improves impairment of endothelium-dependent vasodilation in patients with coronary spastic angina. J. Am. Coll. Cardiol. 1998;32:1672–1679. doi: 10.1016/S0735-1097(98)00447-1. [DOI] [PubMed] [Google Scholar]
- 30.Neunteufl T., Kostner K., Katzenschlager R., Zehetgruber M., Maurer G., Weidinger F. Additional benefit of vitamin E supplementation to simvastatin therapy on vasoreactivity of the brachial artery of hypercholesterolemic men. J. Am. Coll. Cardiol. 1998;32:711–716. doi: 10.1016/S0735-1097(98)00295-2. [DOI] [PubMed] [Google Scholar]
- 31.Borovnicar A., Keber I., Stavljenic Rukavina A., Yaletel Kragelj L. Improvement of early functional atherosclerotic changes in males with hypercholesterolemia after vitamin E supplementation. Pflugers Arch. 2000;440:R126–R128. doi: 10.1007/s004240000032. [DOI] [PubMed] [Google Scholar]
- 32.Economides P.A., Khaodhiar L., Caselli A., Caballero A.E., Keenan H., Bursell S.E., King G.L., Johnstone M.T., Horton E.S., Veves A. The effect of vitamin E on endothelial function of micro- and macrocirculation and left ventricular function in type 1 and type 2 diabetic patients. Diabetes. 2005;54:204–211. doi: 10.2337/diabetes.54.1.204. [DOI] [PubMed] [Google Scholar]
- 33.Gepner A.D., Ramamurthy R., Krueger D.C., Korcarz C.E., Binkley N., Stein J.H. A prospective randomized controlled trial of the effects of vitamin D supplementation on cardiovascular disease risk. PLoS One. 2012;7:e36617. doi: 10.1371/journal.pone.0036617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harris R.A., Pedersen-White J., Guo D.H., Stallmann-Jorgensen I.S., Keeton D., Huang Y., Shah Y., Zhu H., Dong Y. Vitamin D3 supplementation for 16 weeks improves flow-mediated dilation in overweight African-American adults. Am. J. Hypertens. 2011;24:557–562. doi: 10.1038/ajh.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kugiyama K., Motoyama T., Doi H., Kawano H., Hirai N., Soejima H., Miyao Y., Takazoe K., Moriyama Y., Mizuno Y., et al. Improvement of endothelial vasomotor dysfunction by treatment with alpha-tocopherol in patients with high remnant lipoproteins levels. J. Am. Coll. Cardiol. 1999;33:1512–1518. doi: 10.1016/S0735-1097(99)00057-1. [DOI] [PubMed] [Google Scholar]
- 36.Longenecker C.T., Hileman C.O., Carman T.L., Ross A.C., Seydafkan S., Brown T.T., Labbato D.E., Storer N., Tangpricha V., McComsey G.A. Vitamin D supplementation and endothelial function in vitamin D deficient HIV-infected patients: A randomized placebo-controlled trial. Antivir. Ther. 2012;17:613–621. doi: 10.3851/IMP1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Neunteufl T., Priglinger U., Heher S., Zehetgruber M., Soregi G., Lehr S., Huber K., Maurer G., Weidinger F., Kostner K. Effects of vitamin E on chronic and acute endothelial dysfunction in smokers. J. Am. Coll. Cardiol. 2000;35:277–283. doi: 10.1016/S0735-1097(99)00542-2. [DOI] [PubMed] [Google Scholar]
- 38.Paolisso G., Tagliamonte M.R., Barbieri M., Zito G.A., Gambardella A., Varricchio G., Ragno E., Varricchio M. Chronic vitamin E administration improves brachial reactivity and increases intracellular magnesium concentration in type II diabetic patients. J. Clin. Endocrinol. Metab. 2000;85:109–115. doi: 10.1210/jcem.85.1.6258. [DOI] [PubMed] [Google Scholar]
- 39.Skyrme-Jones R.A., O’Brien R.C., Berry K.L., Meredith I.T. Vitamin E supplementation improves endothelial function in type I diabetes mellitus: A randomized, placebo-controlled study. J. Am. Coll. Cardiol. 2000;36:94–102. doi: 10.1016/S0735-1097(00)00720-8. [DOI] [PubMed] [Google Scholar]
- 40.Sugden J.A., Davies J.I., Witham M.D., Morris A.D., Struthers A.D. Vitamin D improves endothelial function in patients with type 2 diabetes mellitus and low vitamin D levels. Diabet Med. 2008;25:320–325. doi: 10.1111/j.1464-5491.2007.02360.x. [DOI] [PubMed] [Google Scholar]
- 41.Witham M.D., Adams F., Kabir G., Kennedy G., Belch J.J., Khan F. Effect of short-term vitamin D supplementation on markers of vascular health in South Asian women living in the UK—A randomised controlled trial. Atherosclerosis. 2013;230:293–299. doi: 10.1016/j.atherosclerosis.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 42.Witham M.D., Dove F.J., Dryburgh M., Sugden J.A., Morris A.D., Struthers A.D. The effect of different doses of vitamin D(3) on markers of vascular health in patients with type 2 diabetes: A randomised controlled trial. Diabetologia. 2010;53:2112–2119. doi: 10.1007/s00125-010-1838-1. [DOI] [PubMed] [Google Scholar]
- 43.Witham M.D., Dove F.J., Sugden J.A., Doney A.S., Struthers A.D. The effect of vitamin D replacement on markers of vascular health in stroke patients—A randomised controlled trial. Nutr. Metab. Cardiovas. Dis. 2012;22:864–870. doi: 10.1016/j.numecd.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 44.Witham M.D., Price R.J., Struthers A.D., Donnan P.T., Messow C.M., Ford I., McMurdo M.E. Cholecalciferol treatment to reduce blood pressure in older patients with isolated systolic hypertension: The VitDISH randomized controlled trial. JAMA Intern. Med. 2013;173:1672–1679. doi: 10.1001/jamainternmed.2013.9043. [DOI] [PubMed] [Google Scholar]
- 45.Yiu Y.F., Yiu K.H., Siu C.W., Chan Y.H., Li S.W., Wong L.Y., Lee S.W., Tam S., Wong E.W., Lau C.P., et al. Randomized controlled trial of vitamin D supplement on endothelial function in patients with type 2 diabetes. Atherosclerosis. 2013;227:140–146. doi: 10.1016/j.atherosclerosis.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 46.Simons L.A., von Konigsmark M., Simons J., Stocker R., Celermajer D.S. Vitamin E ingestion does not improve arterial endothelial dysfunction in older adults. Atherosclerosis. 1999;143:193–199. doi: 10.1016/S0021-9150(98)00287-1. [DOI] [PubMed] [Google Scholar]
- 47.Shab-Bidar S., Mazloum Z., Mousavi-Shirazifard Z. Daily vitamin E supplementation does not improve metabolic and glycemic control in type 2 diabetic patients: A double blinded randomized controlled trial. J. Diabetes. 2013;5:57–58. doi: 10.1111/j.1753-0407.2012.00206.x. [DOI] [PubMed] [Google Scholar]
- 48.de Oliveira A.M., Rondo P.H., Luzia L.A., DʼAbronzo F.H., Illison V.K. The effects of lipoic acid and alpha-tocopherol supplementation on the lipid profile and insulin sensitivity of patients with type 2 diabetes mellitus: A randomized, double-blind, placebo-controlled trial. Diabetes Res. Clin. Pract. 2011;92:253–260. doi: 10.1016/j.diabres.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 49.Paolisso G., DʼAmore A., Giugliano D., Ceriello A., Varricchio M., DʼOnofrio F. Pharmacologic doses of vitamin E improve insulin action in healthy subjects and non-insulin-dependent diabetic patients. Am. J. Clin. Nutr. 1993;57:650–656. doi: 10.1093/ajcn/57.5.650. [DOI] [PubMed] [Google Scholar]
- 50.Paolisso G., di Maro G., Galzerano D., Cacciapuoti F., Varricchio G., Varricchio M., D’Onofrio F. Pharmacological doses of vitamin E and insulin action in elderly subjects. Am. J. Clin. Nutr. 1994;59:1291–1296. doi: 10.1093/ajcn/59.6.1291. [DOI] [PubMed] [Google Scholar]
- 51.Monsen E.R. Dietary reference intakes for the antioxidant nutrients: Vitamin C, vitamin E, selenium, and carotenoids. J. Am. Diet. Assoc. 2000;100:637–640. doi: 10.1016/S0002-8223(00)00189-9. [DOI] [PubMed] [Google Scholar]
- 52.Miller E.R., 3rd, Pastor-Barriuso R., Dalal D., Riemersma R.A., Appel L.J., Guallar E. Meta-analysis: High-dosage vitamin E supplementation may increase all-cause mortality. Ann. Intern. Med. 2005;142:37–46. doi: 10.7326/0003-4819-142-1-200501040-00110. [DOI] [PubMed] [Google Scholar]
- 53.Bjelakovic G., Nikolova D., Gluud L.L., Simonetti R.G., Gluud C. Mortality in randomized trials of antioxidant supplements for primary and secondary prevention: Systematic review and meta-analysis. JAMA. 2007;297:842–857. doi: 10.1001/jama.297.8.842. [DOI] [PubMed] [Google Scholar]
- 54.Wang T.J., Pencina M.J., Booth S.L., Jacques P.F., Ingelsson E., Lanier K., Benjamin E.J., DʼAgostino R.B., Wolf M., Vasan R.S. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117:503–511. doi: 10.1161/CIRCULATIONAHA.107.706127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dobnig H., Pilz S., Scharnagl H., Renner W., Seelhorst U., Wellnitz B., Kinkeldei J., Boehm B.O., Weihrauch G., Maerz W. Independent association of low serum 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels with all-cause and cardiovascular mortality. Arch. Intern. Med. 2008;168:1340–1349. doi: 10.1001/archinte.168.12.1340. [DOI] [PubMed] [Google Scholar]
- 56.Dalan R., Liew H., Tan A.W., Chew D.E., Leow M.K. Vitamin D and the endothelium: Basic, translational and clinical research updates. IJC Metab. Endocr. 2014;4:4–17. doi: 10.1016/j.ijcme.2014.06.003. [DOI] [Google Scholar]
- 57.Heaney R.P. Vitamin D and calcium interactions: Functional outcomes. Am. J. Clin. Nutr. 2008;88:541S–544S. doi: 10.1093/ajcn/88.2.541S. [DOI] [PubMed] [Google Scholar]
- 58.Voutilainen S., Nurmi T., Mursu J., Rissanen T.H. Carotenoids and cardiovascular health. Am. J. Clin. Nutr. 2006;83:1265–1271. doi: 10.1093/ajcn/83.6.1265. [DOI] [PubMed] [Google Scholar]
- 59.Geleijnse J.M., Vermeer C., Grobbee D.E., Schurgers L.J., Knapen M.H., van der Meer I.M., Hofman A., Witteman J.C. Dietary intake of menaquinone is associated with a reduced risk of coronary heart disease: The Rotterdam Study. J. Nutr. 2004;134:3100–3105. doi: 10.1093/jn/134.11.3100. [DOI] [PubMed] [Google Scholar]
- 60.Juanola-Falgarona M., Salas-Salvado J., Martinez-Gonzalez M.A., Corella D., Estruch R., Ros E., Fito M., Aros F., Gomez-Gracia E., Fiol M., et al. Dietary intake of vitamin K is inversely associated with mortality risk. J. Nutr. 2014;144:743–750. doi: 10.3945/jn.113.187740. [DOI] [PubMed] [Google Scholar]
- 61.Lu Q., Bjorkhem I., Wretlind B., Diczfalusy U., Henriksson P., Freyschuss A. Effect of ascorbic acid on microcirculation in patients with type II diabetes: A randomized placebo-controlled cross-over study. Clin Sci (Lond) 2005;108:507–513. doi: 10.1042/CS20040291. [DOI] [PubMed] [Google Scholar]
- 62.Sankhla M., Sharma T.K., Mathur K., Rathor J.S., Butolia V., Gadhok A.K., Vardey S.K., Sinha M., Kaushik G.G. Relationship of oxidative stress with obesity and its role in obesity induced metabolic syndrome. Clin. Lab. 2012;58:385–392. [PubMed] [Google Scholar]
- 63.De Roos N.M., Bots M.L., Schouten E.G., Katan M.B. Within-subject variability of flow-mediated vasodilation of the brachial artery in healthy men and women: Implications for experimental studies. Ultrasound Med. Biol. 2003;29:401–406. doi: 10.1016/s0301-5629(02)00709-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.