Abstract
Background: Tobacco smoking is more prevalent among the elderly than among the young, and the elderly also have the most frequent contact with the health care system. The aim of this study was to evaluate the effectiveness of the Gold Standard Program, which is an intensive six-week smoking cessation program, on continuous self-reported abstinence rates after six months, on participants over the age of 60 years in a real life setting. Methods: This was a retrospective cohort study from the national Danish smoking cessation database. Results: The database registered 7369 participants over the age of 60 years (range 60–82) and 24,294 below 60 years (range 15–59). Continuous abstinence rate after six months was 37% for the elderly compared to 35% for the younger (p < 0.05). The significant variables for continuous abstinence were: living with another adult (OR 1.10), prior professional recommendation for smoking cessation (OR 1.12), being compliant with program (OR 1.35) and being abstinent at end of course (OR 13.3). Conclusions: Participants over the age of 60 years had significantly higher continuous abstinence rates after six months than the participants less than 60 years. It is never too late for health professionals to recommend and educate patients about smoking cessation programs even if they are over 60 years of age.
Keywords: smoking cessation intervention, elderly, intensive program, Gold Standard Program (GSP), continuous abstinence, prospective cohort study, national database, Denmark
1. Introduction
Tobacco smoking is the biggest cause of illness and pre-mature death in the Western part of the world [1]. Worldwide it is estimated that more than five million people die from tobacco-related disease each year [2]. In Denmark the amount of daily smokers have diminished from 30% in 2000 to 17% in 2013 and approximately 1%–2% of Danish smokers successfully quit smoking each year [3]. Unfortunately there has not been an equal reduction in the amount of tobacco sold. A possible explanation for this could be that it was mainly the smokers who had the least tobacco consumption who succeeded in quitting smoking. Also, the reduction of smokers in Denmark has been more modest when compared to the other Nordic countries. Considering the age distribution, smoking seems most prevalent among 50–59 year-old Danes with 26% being daily smokers, whereas among citizens 60 years or older 16% are daily smokers [3].
It is a clinical experience that health professionals are less persuasive in recommending smoking cessation for patients over the age of 60, simply because they think this group of patients have smoked for too long and are not likely to quit at this age. But the people with the most frequent contact with the health care system are those over 60 years of age and therefore it is the group of smokers where there is the greatest potential for health care professionals to recommend, educate and influence them for smoking cessation programs. Thus, it is highly relevant to investigate the effect of smoking cessation intervention among this group.
The positive effects of smoking cessation have been shown for many years regarding almost all functions of the body from pulmonary function [4,5], reducing risk of cancer [6,7] and coronary disease [8,9,10], and intensive smoking cessation programs also have a positive effect on reducing the risks of having postoperative complications [11,12].
The aim of this study was to evaluate the effectiveness of intensive smoking cessation intervention programs (The Gold Standard Program, GSP) on continuous self-reported abstinence six-months after intended quit date on people from 60 years of age, and comparing this group of participants to the participants under the age of 60 years, as well as all participants in the Smoking Cessation Database. Furthermore we wanted to analyze selected variables gathered in the Smoking Cessation Database for a possible association with continuous abstinence.
2. Methods
2.1. Design
This is an observational cohort study using data from the Danish Smoking Cessation Database [13].
2.2. Setting
The Smoking Cessation Database is a database where more than 350 units in all 5 regions of Denmark contribute with data from smoking cessation programs. Both primary care facilities and hospitals are contributors to the database.
2.3. Material
Data have been collected in the Smoking Cessation Database since 2001. Since 2006 all entries has been identified with a unique 10-digit personal identification number (PIN) and therefore the database could be searched for doublets and for patients attending the program more than once. All participants gave written consent before entering the program.
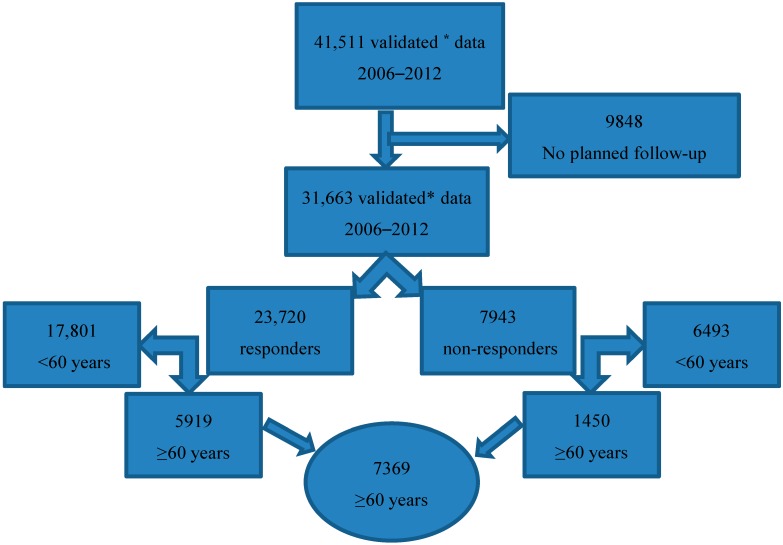
In this study we included participants attending the GSP in Denmark in the seven-years period January 2006 through December 2012, and where follow-up was intended. Analyses were conducted for participants in three pre-defined groups termed “elderly” (≥60 years), “young” (<60) and “all”. Before the analysis, the data was validated by searching for doublets and non-existing personal identification numbers and these were excluded from further analysis. After validating the data, the participants where follow-up was not intended were excluded (Figure 1).
Figure 1.
Flow-chart for the study population according to definition of age and responders vs. non-responders. * Validated data: doublets and non-existing personal identification number are excluded.
The Smoking Cessation Database documents for each patient among others: The setting, the region in which the participant lives in, payment modality and whether the smoking cessation program is individual or group based. It also documents age, amount smoked per day, pack-years, Fagerström Test for Nicotine Dependence [14], previous attempts to quit, living with smoker vs. not living with smoker, compliant or non-compliant with program, way of recommendation, occupational position, level of education, and living status. For complete list of data collected, see Table 1.
Table 1.
Data collected by the Danish Smoking Cessation Database.
| Setting: | Hospitals and Pharmacies. County or Municipality. |
|---|---|
| Living Region: | Capital of Copenhagen, Zealand, Southern Denmark, Central Denmark, North Denmark. |
| Payment modality: | No free medication, free medication for a few days, free medication for <5 weeks or 5 weeks medication free of charge. |
| Smoking cessation program: | Individual or group based. |
| Age: | At entering program. |
| Amount smoked per day: | Cigarettes, pipes, cigars, others smoked per day. |
| Pack-years: | (Cigarettes per day × years of smoking)/20. |
| Fagerström Test for Nicotine Dependence 0–10 points: | 0 point = No dependence. 1–2 point = Low dependence. 3–4 point = Low to moderate dependence. 5–6 point = Moderate dependence. 7–10 point = High dependence. |
| Quit attempts: | Number of prior attempts to quit. |
| Living status (socially): | Living with adult (>18 years), smoker, children. |
| Compliant or Non-Compliant with program: | Defined as attending >75% of meetings vs. <75% |
| Way of recommendation: | Self-referred or referred by health-professional. |
| Occupational position: | Working, disability, pensioner, retired, unemployed, student, other. |
| Level of education: | Primary school, high school, skilled craftsman, short, medium or longer higher education, other. |
| Living status (housing): | Home ownership, rental, other. |
| Smoking status at end of program: | Abstinent, continuous smoker, unknown status. |
The follow-up consisted of a telephone interview where 4 attempts were made to reach the patient where at least one call was during the evening. If the patient was not reached following this procedure the patient was reported as a non-responder.
2.4. Intervention
Since 2001 the Gold Standard Program (GSP) has been the smoking cessation program of choice in Denmark. It is an intensive smoking cessation program developed by the National Cancer Society and the National Stop Smoking Centre [15]. It was developed to uniform and optimize smoking cessation nationwide. It consists of a program with 5 meetings (individual or group-based) over 6 weeks with a pre-defined schedule of motivational conversation, education of the hazards of smoking, risks of relapse, thoughts and reflections on quitting, challenges during smoking cessation and ways to prevent relapse. All patients are scored according to the Fagerström test during the first meeting and are free to choose different kinds of nicotine replacement under the guidance of the smoking cessation instructor. The GSP is normally offered free of charge by the Danish municipalities and regions but most patients must themselves pay for nicotine replacement. To further enable their smoking cessation a telephone hotline is available so the patients can call in between meeting sessions.
2.5. Outcome
The primary outcome was continuous self-reported abstinence 6 months after the date of intended quit date, or if one such did not exist, the last smoking cessation treatment date.
2.6. Statistical Analysis
Statistical analysis was done by using SPSS version 22. A univariate analysis was performed for the categorical and continuous variables listed in Table 2 and were assessed using the cross-table methods with Fisher’s exact test (two sided). This was done for all three pre-defined groups, “Elderly ≥ 60 years”, “Young < 60” and ‘All’. For the group of participants ≥ 60 years of age, the variables with a p-value < 0.1 were considered significant to be included in further analysis.
Table 2.
Characteristics in numbers (N) and six months continuous abstinence rates given in percent (%) for all (including non-responders) and for responders only for both elderly, young and all.
| Variables | Elderly: 60–82 Years. | Young: 15–59 Years. | All: 15–82 Years. | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | All N = 7369 (%) | Responders N = 5919 (%) | N | All N = 24,294 (%) | Responders N = 17,801 (%) | N | All N = 31,663 (%) | Responders N = 23,720 (%) | |
| Gender | |||||||||
| Male | 3138 | 31 | 38 | 9415 | 26 | 36 | 12,553 | 27 | 37 |
| Female | 4231 | 29 | 36 | 14,879 | 24 | 33 | 19,110 | 25 | 34 |
| Setting | |||||||||
| Hospital | 764 | 29 | 36 | 2321 | 25 | 35 | 3085 | 26 | 35 |
| Other | 6605 | 29 | 37 | 21,973 | 25 | 34 | 28,578 | 26 | 36 |
| Program | |||||||||
| Individual | 1116 | 31 | 41 | 3129 | 27 | 39 | 4245 | 28 | 39 |
| Group | 6178 | 29 | 36 | 20,833 | 24 | 33 | 27,011 | 25 | 34 |
| Smoking | |||||||||
| 0-20 pack- years | 1,001 | 34 | 42 | 10,027 | 25 | 36 | 11,028 | 26 | 36 |
| >20 pack-years | 6,026 | 28 | 36 | 13,281 | 25 | 33 | 19,307 | 26 | 34 |
| Fagerström 1–4 | 2951 | 32 | 39 | 7940 | 29 | 38 | 10,891 | 29 | 39 |
| Fagerström 5–10 | 4193 | 27 | 34 | 15,580 | 22 | 31 | 19,773 | 23 | 32 |
| 0-9 cig. per day. | 884 | 34 | 43 | 1942 | 33 | 44 | 2826 | 33 | 44 |
| 10–19 | 2,508 | 32 | 39 | 8650 | 26 | 36 | 11,158 | 28 | 37 |
| 20–29 | 2809 | 28 | 35 | 10,196 | 23 | 32 | 13,005 | 24 | 33 |
| 30–39 | 781 | 26 | 32 | 2356 | 21 | 29 | 3131 | 22 | 30 |
| +40 | 387 | 24 | 31 | 1156 | 20 | 28 | 1543 | 21 | 29 |
| Heavy smoker * | |||||||||
| Yes | 6157 | 28 | 36 | 16,893 | 24 | 32 | 23,050 | 25 | 39 |
| No | 1212 | 34 | 43 | 7401 | 28 | 38 | 8613 | 29 | 33 |
| Region | |||||||||
| Capital | 2698 | 28 | 35 | 9050 | 24 | 33 | 11,748 | 25 | 37 |
| Northern | 371 | 30 | 40 | 1145 | 26 | 36 | 1516 | 26 | 37 |
| Middle | 1610 | 29 | 37 | 5496 | 24 | 34 | 7106 | 25 | 35 |
| Southern | 1448 | 32 | 38 | 5212 | 26 | 35 | 6660 | 28 | 36 |
| Sealand | 1242 | 30 | 38 | 3391 | 25 | 34 | 4633 | 27 | 35 |
| Living with adult | |||||||||
| Yes | 3063 | 33 | 40 | 14,389 | 26 | 36 | 17,452 | 28 | 37 |
| No | 4238 | 27 | 34 | 9631 | 22 | 31 | 13,869 | 24 | 32 |
| Living with smoker | |||||||||
| Yes | 1932 | 30 | 36 | 8785 | 23 | 32 | 10,717 | 25 | 33 |
| No | 5382 | 29 | 37 | 15,322 | 26 | 35 | 20,704 | 27 | 36 |
| Professional recommend | |||||||||
| Yes | 2035 | 32 | 41 | 10,083 | 27 | 36 | 12,118 | 28 | 37 |
| No | 5334 | 28 | 35 | 14,211 | 24 | 32 | 19,545 | 25 | 33 |
| Compliant with program | |||||||||
| Yes | 5157 | 36 | 43 | 14,061 | 33 | 43 | 19,218 | 34 | 43 |
| No | 2212 | 14 | 19 | 10,233 | 13 | 19 | 12,445 | 13 | 19 |
| Employed | |||||||||
| Yes | 1267 | 31 | 40 | 17,335 | 27 | 36 | 18,602 | 27 | 36 |
| No | 5941 | 29 | 36 | 6321 | 20 | 29 | 12,262 | 24 | 33 |
| Attempts to quit | |||||||||
| No previous attempts | 3025 | 29 | 37 | 9310 | 24 | 33 | 12,335 | 25 | 34 |
| Previous attempts | 4124 | 30 | 37 | 14,591 | 26 | 35 | 18,715 | 27 | 35 |
| Abstinent at end of program | |||||||||
| Yes | 4120 | 48 | 57 | 11462 | 43 | 54 | 15582 | 44 | 55 |
| No | 2145 | 5 | 7 | 6380 | 4 | 7 | 8525 | 5 | 7 |
* Heavy smoker defined as: smoking ≥20 pack-year and/or consumption of ≥20 cigarettes a day and/or Fagerström nicotine dependence score of ≥7 points.
To identify the relative impact of the independent variables for continuous abstinence for the elderly, a logistic regression analysis was performed using the backward stepwise selection. In the multivariate analysis p < 0.05 was considered significant. The participants with “unknown” values (missing data) were excluded from the analyses. The numbers were considered small and acceptable for a real life study. All significant results are presented as odds ratios (OR) with 95% confidence intervals (CI).
All missing data and any loss of follow-ups were included, analyzed and reported according to the STROBE recommendations [16]. Data were also analyzed and reported according to the Russell Standards for RCTs [17], which assume that non-responders have relapsed and they are thereby included in the analysis as smokers, to ensure that this study can be compared to randomized studies. Therefore two columns for each of the three pre-defined groups are presented in Table 2; one column showing “All”, where non-responders are considered still smokers, and one column showing “Responders” only.
3. Results
In total 31,663 participants were entered in the database between the years 2006–2012. Of these, 7369 (23%) were 60 years or older when entering the GSP. Follow-up data was obtained from 5919 (80%) (termed responders), whereas 1450 (20%) could not be reached according to protocol (termed non-responders). See Figure 1.
The median age of the elderly participants was 65 years (range 60–82 years), of the young group was 45 years (range 15–59 years) and of all participants was 50 years (range 15–82 years).
For the participants attending the GSP and who were older than 60 years of age a total of 37% were continuous abstinent six month after the intended quit date. For the young, 35% were continuous abstinent after six months and for all the participants 36% were continuous abstinent after six month (p < 0.05). Among the elderly 38% of men and 36% of women were still abstinent after six months, whereas only 36% of the younger men and 33% of the younger women were abstinent after six months.
Participants among the elderly who had a smoking history of more than 20 pack-years (82%) had a continuous abstinence rate of 36% compared to those with <20 pack-years (18%) who had a continuous abstinence rate of 42% (p < 0.05). Among the young participants 55% had a smoking history of >20 pack-years and their abstinence rate was 33%.
A total of 5157 (70%) of the elderly were compliant with the GSP and their continuous abstinence rate after six months was 43% compared to an abstinence rate of only 19% for the 2837 participants that were not compliant with the program (p < 0.05). For the young, only 58% were compliant but the abstinence rate was similar (43%).
When the non-responders were included in the analyses—and categorized as having relapsed and therefore considered smokers—The continuous abstinence rates decreased in all three groups. Similarly, when non-responders were included the continuous abstinence rate after six months for the elderly was reduced to 30%, and for the young to 25% and for all to 26%.
The characteristics and abstinence rates of all three groups for responders only and for all are shown in Table 2.
The main differences between responders and non-responders in the group of the elderly were whether they were compliant with the program (responders 73%, non-responders 58%, p < 0.05), abstinent at end of program (responders 57%, non-responders 42%, p < 0.05) and whether they were in individual or group-based program (responders in group-based 85%, non-responders in group-based 82%, p < 0.05). Otherwise the two groups were equal and comparable in terms of gender, age, Fagerström and housing.
Table 3 shows the univariate and multivariate analysis with the variables for continuous abstinence after six months among the elderly. We found as significant factors in the final adjusted model: whether the participant lived with another adult (OR 1.10), if they had prior professional recommendation for smoking cessation (OR 1.12), if they were compliant with the program (OR 1.35) and whether they were abstinent at the end of the program (OR 13.3).
Table 3.
Primary outcome: Odds Ratios with 95% confidence intervals for continuous abstinence rates after six months for participants >60 years (non-responders seen as continuous smokers) for the univariate, multivariate and the final adjusted multivariate model.
| Variables: | N = 7369 | Univariate OR (CI) | Multivariate OR (CI) | Final adjusted OR (CI) | |
|---|---|---|---|---|---|
| Gender: | Female | 4231 | 1 | 1 | -- |
| Male | 3138 | 0.91 (0.82–1.01) | 1.00 (0.88–1.35) | ||
| Working: | No | 5941 | 1 | 1 | -- |
| Yes | 1267 | 0.90 (0.79–1.03) | 1.04 (0.88–1.23) | ||
| Living with adult: | No | 4238 | 1 | 1 | 1 |
| Yes | 3063 | 1.25 (1.18–1.33)* | 1.14 (1.00–1.29) * | 1.10 (1.00–1.23)* | |
| Setting: | Hospital | 764 | 1 | 1 | -- |
| Other | 6605 | 1.00 (0.85–1.15) | 1.08 (0.87–1.34) | ||
| Program: | Group based | 6178 | 1 | 1 | -- |
| Individual | 1116 | 1.10 (1.05–1.26)* | 1.03 (0.89–1.20) | ||
| Heavy smoker** | No | 1212 | 1 | 1 | -- |
| Yes | 6157 | 0.80 (0.71–0.91)* | 0.92 (0.80–1.07) | ||
| Professional recommendation: | No | 5334 | 1 | 1 | 1 |
| Yes | 2035 | 1.23 (1.10–1.37)* | 1.11 (0.98–1.28) | 1.12 (1.00–1.26)* | |
| Compliant with program: | No | 2212 | 1 | 1 | 1 |
| Yes | 5157 | 3.56 (3.12–4.07)* | 1.34 (1.10–1.65) * | 1.35 (1.03–1.62)* | |
| Non-smoker at end of program: | No | 2037 | 1 | 1 | 1 |
| Yes | 3951 | 17.1 (13.9–21.1)* | 13.8 (10.5–16.8) * | 13.3 (10.7–16.4) * |
OR Odds Ratio, CI Confidence Interval, * significant with P < 0.05. ** Heavy smoker defined as: smoking ≥20 pack-year and/or consumption of ≥20 cigarettes a day and/or Fagerström nicotine dependence score of ≥7 points.
4. Discussion
This study showed a high continuous abstinence rate for participants over the age of 60 years in the Danish Gold Standard Program for smoking cessation. Participants over the age of 60 actually had significantly higher continuous abstinence rates both compared to the participant under the age of 60 years, but also to all participants in the GSP. This shows an age group motivated for quitting their smoking habits and sticking with it.
The significant variables for continuous tobacco abstinence can be grouped in modifiable or non-modifiable variables. Of the four variables that were significant in this study population, there was only one non-modifiable variable. This was whether the participant lived with another adult (OR 1.10), which can only be taken note of.
Two of the significant factors for a successful continuous abstinence were to do with the quality of the program and the motivation of the participants. Being compliant with the program, meaning attending the courses as planned, enhanced the chances for quitting the smoking habit (OR 1.35). This has also been shown for disadvantaged smokers, heavy smokers and pregnant smokers [18,19,20] and is of great importance for the individual smoking cessation sites. If the smoking cessation instructors can support the patient’s motivation and maintain good contact to the participants it is more likely they attend the planned meetings and thereby their success for quitting is greater. So the instructors giving the smoking cessation programs are of great importance. It could also be that it is the most motivated participant who are compliant with the program and thereby are better at quitting the tobacco.
Being abstinent at the end of the program is the greatest factor for continuous abstinence six months after (OR 13.3). This is not of great surprise, but it still gives a good inclination that if the smoking cessation programs are at their best, if the participants are motivated and therefore compliant with the program, more will be abstinent at the end of the program and therefore also continuous abstinent six months later. Together adding to the success of continuous abstinence. It is also interesting that of the participants who are still smokers at the end of the program, between 4%–7% report being abstinent after six months at follow-up (Table 2). This could be due to low motivation at end of program, smoking cessation date after end of program, or it could also possibly be reporting bias.
Also, professional recommendation did have an effect on continuous abstinence (OR 1.12). Even though the odds ratio is relatively small it still shows how important it is for general practitioners, hospital doctors and other health care personnel to inform patients about the risk of smoking, and ways to quit. Other studies, including a review of 42 trials, also show that life style consultations significantly increase the rate of smokers wanting to attend smoking cessation courses [21,22], and this in smokers who are not admitted to hospitals or are to be operated upon, so there could be good reason to believe that the “therapeutic opportunity” to encourage hospital admitted smokers are even greater than for the general population. It could be noted though that among fertile women (15–54 years) and among disadvantaged smokers attending the GSP the opposite has been shown with prior professional recommendation reducing the continuous abstinence rate. In these cohorts after controlling for other variables, such as pregnancy and other effect modifiers, the multivariate analysis showed a significant better continuous abstinence rate for the groups not receiving recommendation from health professionals prior to the smoking cessation program. This may be due to gender, educational and social related differences in attitudes and preferences of smoking cessation intervention, which has however not been investigated further [18,20].
Whether the participants attended group or individual programs was not a significant variable in the multivariate analysis for the elderly, even though other studies from the Danish Smoking Cessation Database show that the program had a significant influence in increasing the numbers of continuous abstinence, favoring individual programs over group programs [18,19,20], the opposite has also been shown [23].
Being older than 60 years should never imply that smoking cessation is too late. Back in the 90’s several predictors was identified in the elderly population highlighting the variables increasing smoking cessation in this specific population group. It was found that hospitalized patients were more inclined to smoking cessation, as well as being married to non-smoking spouse, motivation was important and their prior attempts of quitting was significant variables [24]. Designing programs targeted for the elderly population does seem to have potential for success, because when attending smoking cessation intervention programs designed to all, it is seen that smokers over the age of 60 years who participate, succeed better than younger participants. Cessation rates after four weeks are significantly higher for the elderly than the younger participants [25] and this also applies after one year [23]. So one might assume that if smoking cessation programs for the elderly were even more targeted, the quit rates could be even higher.
Using the knowledge obtained from registry-based studies can heighten the quality of the smoking cessation programs. Smoking cessation has plenty of health benefits for both the elderly as well as the young. Cardiovascular and even non-tobacco related cancer-mortality is diminished in former smokers compared to current smokers and some studies even show that the cardiovascular mortality in former smokers is similar to that of never-smokers [26,27].
We have to consider that there are both limitations as well as strengths to this study. The limitations of this study are in the selection of data, the registration of the data and possible selection bias. Being a registry-based study it has limitations compared to a randomized trial. Also, the abstinence rates are all based on self-reported data. This could give an overestimation of abstinence rates of 3%–6% [21,23]. The strengths of this study lie especially in the high number of participants included. Also, approximately 90% of all smoking cessation intervention sites in Denmark report to the Danish Smoking Cessation Database, giving a realistic characteristic of the participants with the normal background population and thereby minimizing the selection bias. Since the instructors are educated according to the same program this gives consistency in the meetings and conversations with the participants all over the country adding strength to the data collected. Statistical strength is also added since all non-responders are considered still-smokers when included in the analyses.
5. Conclusions
Participants following the GSP for smoking cessation and who were over the age of 60 years old had a continuous abstinence rate after six months of 37%. This was a higher abstinence rate than participants less than the age of 60 and also higher than for all participants registered in the Danish Smoking Cessation Database. The significant variables for continuous smoking cessation six months after the program were living with another adult, having prior professional recommendation on smoking cessation and the risks of continuous smoking, being compliant with the program and being abstinent at the end of the program.
It is never too late for health professionals to recommend, educate and influence patients for attending smoking cessation programs, even if they are over 60 years of age. This actually only increase the success rate for quitting compared to the younger age groups and they still gain important health benefits compared to continuous smokers.
Acknowledgments
Thank you to all the smoking cessation instructors who contribute with data to the Danish Smoking Cessation Database and to Mette Rasmussen for managing the database and providing data ready for analysis. Also thank you to Bolette Pedersen for her statistical support on several occasions.
Author Contributions
Hanne Tønnesen, Torben V. Schroeder and Mette Kehlet designed the study. Mette Kehlet performed the analyses of the data. Mette Kehlet, Torben V. Schroeder and Hanne Tønnesen wrote the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Lim S.S., Vos T., Flaxman A.D., Danaei G., Shibuya K., Adair-Rohani H., Amann M., Anderson H.R., Andrews K.G., Aryee M., et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Global Report. [(accessed on 15 February 2015)]. Available online: http://whqlibdoc.who.int/publications/2012/9789241564434_eng.pdf?ua=1.
- 3.Danish Health and Medicines Authority. [(accessed on 15 February 2015)]. Available online: http://sundhedsstyrelsen.dk/en/health/tobacco.
- 4.Petty T.L. The history of COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 2006;1:3–14. doi: 10.2147/copd.2006.1.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Postma D.S., Bush A., van den Berge M. Risk factors and early origins of chronic obstructive pulmonary disease. Lancet. 2014;2014 doi: 10.1016/S0140-6736(14)60446-3. [DOI] [PubMed] [Google Scholar]
- 6.Becher H., Jockel K.H., Timm J., Wichmann H.E., Drescher K. Smoking cessation and nonsmoking intervals: Effect of different smoking patterns on lung cancer risk. Cancer Causes Control. 1991;2:381–387. doi: 10.1007/BF00054298. [DOI] [PubMed] [Google Scholar]
- 7.Pirie K., Peto R., Reeves G.K., Green J., Beral V. The 21st century hazards of smoking and benefits of stopping: A prospective study of one million women in the UK. Lancet. 2013;381:133–141. doi: 10.1016/S0140-6736(12)61720-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yusuf S., Hawken S., Ounpuu S., Dans T., Avezum A., Lanas F., McQueen M., Budaj A., Pais P., Varigos J., et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 9.Muller-Riemenschneider F., Meinhard C., Damm K., Vauth C., Bockelbrink A., Greiner W., Willich S.N. Effectiveness of nonpharmacological secondary prevention of coronary heart disease. Eur. J. Cardiovasc. Prev. Rehabil. 2010;17:688–700. doi: 10.1097/HJR.0b013e32833a1c95. [DOI] [PubMed] [Google Scholar]
- 10.Gellert C., Schottker B., Muller H., Holleczek B., Brenner H. Impact of smoking and quitting on cardiovascular outcomes and risk advancement periods among older adults. Eur. J. Epidemiol. 2013;28:649–658. doi: 10.1007/s10654-013-9776-0. [DOI] [PubMed] [Google Scholar]
- 11.Nasell H., Adami J., Samnegard E., Tonnesen H., Ponzer S. Effect of smoking cessation intervention on results of acute fracture surgery: A randomized controlled trial. J. Bone Joint Surg. Am. 2010;92:1335–1342. doi: 10.2106/JBJS.I.00627. [DOI] [PubMed] [Google Scholar]
- 12.Thomsen T., Tonnesen H., Moller A.M. Effect of preoperative smoking cessation interventions on postoperative complications and smoking cessation. Br. J. Surg. 2009;96:451–461. doi: 10.1002/bjs.6591. [DOI] [PubMed] [Google Scholar]
- 13.The Danish Smoking Cessation Database. [(accessed on 15 February 2015)]. Available online: http://www.scdb.dk.
- 14.Heatherton T.F., Kozlowski L.T., Frecker R.C., Fagerstrom K.O. The fagerstrom test for nicotine dependence: A revision of the fagerstrom tolerance questionnaire. Br. J. Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 15.The Danish Cancer Society. [(accessed on 15 February 2015)]. Available online: www.cancer.dk/international.
- 16.von Elm E., Altman D.G., Egger M., Pocock S.J., Gotzsche P.C., Vandenbroucke J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting of observational studies. BMJ. 2007;335:806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.West R., Hajek P., Stead L., Stapleton J. Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction. 2005;100:299–303. doi: 10.1111/j.1360-0443.2004.00995.x. [DOI] [PubMed] [Google Scholar]
- 18.Neumann T., Rasmussen M., Ghith N., Heitmann B.L., Tonnesen H. The Gold Standard Programme: Smoking cessation interventions for disadvantaged smokers are effective in a real-life setting. Tob. Control. 2013;22 doi: 10.1136/tobaccocontrol-2011-050194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neumann T., Rasmussen M., Heitmann B.L., Tonnesen H. Gold standard program for heavy smokers in a real-life setting. Int. J. Environ. Res. Public Health. 2013;10:4186–4199. doi: 10.3390/ijerph10094186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rasmussen M., Heitmann B.L., Tonnesen H. Effectiveness of the gold standard programmes (GSP) for smoking cessation in pregnant and non-pregnant women. Int. J. Environ. Res. Public Health. 2013;10:3653–3666. doi: 10.3390/ijerph10083653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pisinger C., Vestbo J., Borch-Johnsen K., Thomsen T., Jorgensen T. Acceptance of the smoking cessation intervention in a large population-based study: The Inter 99 study. Scand. J. Public Health. 2005;33:138–145. doi: 10.1080/14034940410028370. [DOI] [PubMed] [Google Scholar]
- 22.Stead L.F., Buitrago D., Preciado N., Sanchez G., Hartmann-Boyce J., Lancaster T. Physician advice for smoking cessation. Cochrane. Database. Syst. Rev. 2013;2 doi: 10.1002/14651858.CD000165.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferguson J., Bauld L., Chesterman J., Judge K. The English smoking treatment services: One-year outcomes. Addiction. 2005;100:59–69. doi: 10.1111/j.1360-0443.2005.01028.x. [DOI] [PubMed] [Google Scholar]
- 24.Dale L.C., Olsen D.A., Patten C.A., Schroeder D.R., Croghan I.T., Hurt R.D., Offord K.P., Wolter T.D. Predictors of smoking cessation among elderly smokers treated for nicotine dependence. Tob. Control. 1997;6:181–187. doi: 10.1136/tc.6.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bauld L., Chesterman J., Ferguson J., Judge K. A comparison of the effectiveness of group-based and pharmacy-led smoking cessation treatment in Glasgow. Addiction. 2009;104:308–316. doi: 10.1111/j.1360-0443.2008.02446.x. [DOI] [PubMed] [Google Scholar]
- 26.LaCroix A.Z., Lang J., Scherr P., Wallace R.B., Cornoni-Huntley J., Berkman L., Curb J.D., Evans D., Hennekens C.H. Smoking and mortality among older men and women in three communities. N. Engl. J. Med. 1991;324:1619–1625. doi: 10.1056/NEJM199106063242303. [DOI] [PubMed] [Google Scholar]
- 27.Vollset S.E., Tverdal A., Gjessing H.K. Smoking and deaths between 40 and 70 years of age in women and men. Ann. Intern. Med. 2006;144:381–389. doi: 10.7326/0003-4819-144-6-200603210-00004. [DOI] [PubMed] [Google Scholar]