Abstract
Background : In the last decades, children’s and adolescents’ obesity and overweight have increased in European Countries. Unhealthy eating habits and sedentary lifestyle have been recognized to determine such an epidemic. Schools represent an ideal setting to modify harmful behaviors, and physical activity could be regarded as a potential way to avoid the metabolic risks related to obesity. Methods : A systematic review of the literature was carried out to summarize the evidence of school-based interventions aimed to promote, enhance and implement physical activity in European schools. Only randomized controlled trials were included, carried out in Europe from January 2000 to April 2014, universally delivered and targeting pupils aged between 3 and 18 years old. Results : Forty-seven studies were retrieved based either on multicomponent interventions or solely physical activity programs. Most aimed to prevent obesity and cardiovascular risks among youths. While few studies showed a decrease in BMI, positive results were achieved on other outcomes, such as metabolic parameters and physical fitness. Conclusion : Physical activity in schools should be regarded as a simple, non-expensive and enjoyable way to reach all the children and adolescents with adequate doses of moderate to vigorous physical activity.
Keywords: European countries, obesity prevention, physical activity, school-based intervention
BACKGROUND
The optimal dose of moderate-to-vigorous physical activity (MVPA) recommended by guidelines to ensure children’s healthy growth and to avoid the risk of metabolic and cardiovascular diseases is 60 minutes/day 5 days/week [1]. Furthermore, sport participation has been associated to psychological and social health benefits for youths, like increase self-esteem, low depression and anxiety, and even suicide behavior protection [2]. School-based interventions are worldwide aimed to promote children’s wellbeing [3], and to avoid the risk of mental disorders and the stigmatization of those affected [4].
According to the latest report of the World Health Organization (WHO), one of three/four children and adolescents in Europe is overweight or obese [5]. Eating unhealthy foods, a decrease in physical activity, and a global increase in sedentary activities were suggested to be causes for the rise of the youths’ obesity epidemic in European Countries.
While not in every European Country do children have meals at school, all European pupils have on average two hours per week of compulsory physical education in their academic curriculum. Moreover, schools generally have gyms, but also schoolyards, and even classrooms, which might be used to exercise. Thus, schools should be regarded as an ideal place to modify unhealthy habits, and a natural setting to learn, promote and enhance physical activity.
METHODS
We carried out a systematic review of the literature to summarize the evidence of the effectiveness of school-based physical activity interventions from trials carried out in European Countries since 2000.
A search for relevant papers was performed on PubMed, Google Scholar and Scopus using the following keywords: school or school-based or schoolchildren, and physical activity or exercise or fitness, and intervention or program. A further search was performed in the bibliography of the selected papers.
Only randomized controlled trials were included, carried out from January 2000 to April 2014 as school-based interventions, focused on physical activity promotion, advice, awareness, facilitation, implementation, targeted samples of preschoolers, schoolchildren or adolescent students (aged 3 to 18 years old). Because the focus of our review, we included in qualitative analysis only studies carried out in European Countries.
RESULTS
We identified 310 titles by searching on PubMed, and 20 further titles by other sources (Google Scholar, bibliographies of selected papers); no additional title was found on Scopus. Among these, 114 full texts were assessed for eligibility, and 47 papers were included in qualitative analysis (see the PRISMA flowchart for the process of inclusion, Fig. 1). Table 1 shows the main characteristics of the included studies.
Fig. (1).
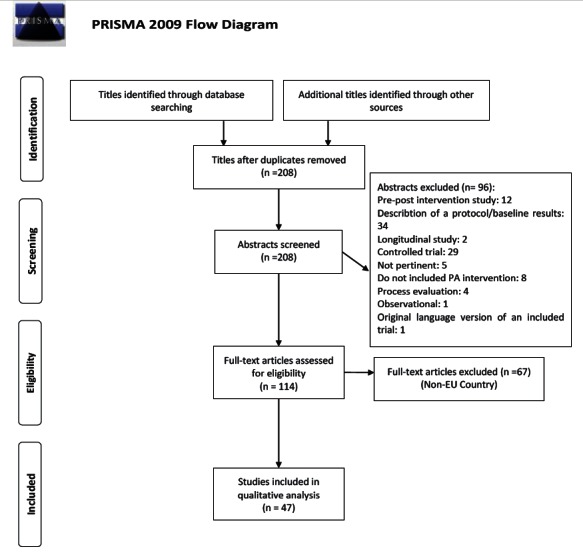
Process of inclusion of studies for qualitative review.
Table 1.
General characteristics of the included trials.
| Author(s) | Country | Year of Publication | Name of Trial | Participants | Type of Intervention | Pa Intervention | Type of Control | Who Delivered |
Duration |
|---|---|---|---|---|---|---|---|---|---|
| PeÑalvo JL, et al. | SPAIN | 2013 | The Program SI! | 2062 preschoolers (3-5 y) |
Multicomponent (dietary habits, physical activity patterns, human body and heart, and management of emotions) | Classrooms materials (including different resources such as healthy tales, educational games and audio-visuals), take-home activities with families, and activities organized within the school’s annual Health Fair. | Usual school curriculum | Trained teachers |
1 year |
| Tarro L, et al. |
SPAIN |
2014 |
the EdAl (EducaciÓ en AlimentaciÓ) study |
1939 primary schoolchildren (8.4±0.6 y) |
Primary-school-based program promoting healthy lifestyle, including dietary and physical activity recommendations, conducted by university students acting as "health promoting agents" (HPAs), focused on eight lifestyle topics covered in 12 activities (1 hour/activity/session) | The intervention program consisted of three components: 1. Classroom practice by HPA to highlight healthy lifestyle habits 2. Teaching practice by HPA using books designed to include the nutritional objectives 3. Parental activities included with their children In each of 12 activities (1 h/activity), the classroom practice consisted of three components: 1. Experimental development of activities regarding each healthy lifestyle habit 2. Assessment of activity performed in classroom 3. An activity developed for use at home |
Usual school curriculum |
University Medicine or Health Science trained students (as a part of their curriculum) | 3 academic years |
| Ardoy DN, et al. | SPAIN | 2010 2011 2013 |
EDUFIT (EDUcational for FITness Study) | 67 middle school students (12-14 y) | Enhanced program of Physical Education |
Exp Group 1: 4 sessions of PE/week Exp Group 2: 4 session of high intensity PE/week | Usual Physical Education Program (2 session of PE/week, 55 minutes each) | School PE teachers | 4 months |
| LlarguÉs E, et al. |
SPAIN |
2011 2012 |
AVall study |
704 primary schoolchildren (5-6 y) (enrolled) |
Promotion of healthy eating habits and physical activity by means of the educational methodology Investigation, Vision, Action and Change (IVAC) | 3 hours/week to develop activities related to PA (games, crafts) |
Usual school curriculum |
Trained teachers |
2 years + 2 years follow up |
| MartÌnez VizcaÌno V, et al. Moya MartÌnez et al. |
SPAIN |
2008 2011 |
The Movi Program |
1044 primary schoolchildren (9.4 y mean age) |
PA after school program intervention |
3 PE lessons/week of 90 minutes each of recreational, non-competitive PA. Each 90-min session included 15 min of stretching, 60 min of aerobic resistance and 15 min of muscular strength/resistance exercises. On average, these exercises required physical activity of moderate intensity throughout the 90 min of each session. |
Usual school curriculum |
PE Teachers |
24 weeks |
| Brandstetter S, et al. |
GERMANY |
2012 |
URMEL-ICE (Ulm Research on Metabolism, Exercise, and Lifestyle Intervention in Children) |
1119 children (7-8 y) |
29 teaching lessons, 2 short exercise blocks per day and 6 family homework lessons on PA, TV time and soft drink consumption | 2 short exercise breaks/day |
Usual school curriculum |
Teachers |
1 year |
| Siegrist M, et al. |
GERMANY |
2013 |
the JuvenTUM project |
826 primary schoolchildren (8.4 ± 0.7 years) |
Children: 10 health-related lessons at school over a period of 1 year Parents and teachers: two and three educational health-related lessons, respectively, and also received 10 newsletters on health issues. | Monthly lessons lasting 45 min with three parts: a warm-up of 10 min with running, playing running games at high intensity, 30 min exercises to improve body awareness and self-esteem with conversation in class about health-related topics, and 5 min relaxation exercises. | Usual school curriculum |
Trained teachers |
1 year |
| Walther C, et al. |
GERMANY |
2009 |
188 children, aged 11.1+/-0.7 years |
PA intervention |
Daily school exercise (daily lesson of 45 minutes each, with at least 15 minutes of endurance training). | Usual Physical Education Program (2 PE lessons/week of 45 minutes each) | PE Teachers |
1 year |
|
| Graf C, et al. |
GERMANY |
2004 2005 2008 |
Children's Health InterventionaL Trial (CHILT) project | 668 primary schoolchildren (6.70 +/- 0.42 y) |
Multicomponent (health education and additional physical activity) program | Exercise daily performed at least once each morning during lessons for at least 5 minutes: 11 exercises on coordination, 7 devoted to posture and balance, 16 to relaxation techniques, 8 to rhythm and music, 10 to creative movement, 8 games relating to group participation and 8 practices for back training, aimed to increase total energy expenditure and to improve fundamental movement skills. | Usual school curriculum | Trained teachers | 20.8 ± 1.0 months |
| Kriemler S, et al., Hartmann T, et al. Meyer U, et al. |
SWITZERLAND |
2010 2011 2013 |
KISS (Kinder-Sportstudie) |
502 primary schoolchildren (6-7 and 11-12 y) |
Multicomponent physical activity program structuring the 3 existing PE lessons each week and adding 2 additional lessons/week, daily short activity breaks, and PA homework. |
2 additional PE lessons/week of 45 minutes + three to five daily short activity breaks (two to five minutes each) during academic lessons, plus daily PA home works (10 minutes). |
Usual Physical Education Program (2 session of PE/week) |
PE Teachers |
1 school year |
| Puder JJ, et al. Niederer I et al. |
SWITZERLAND | 2011 2013 |
The Ballabeina Study | 652 predominantly migrant preschool children (5 y) |
Multidimensional culturally tailored lifestyle intervention including PA, lessons on nutrition, media use (use of television and computers), sleep and adaptation of the built environment of the preschool class. | 4 sessions/week of 45 minutes each of PA, organized as playful games, aimed at increase aerobic fitness and coordination skills. | Usual school curriculum |
Teachers supported by health promoters |
9 months |
| Bergh IH, et al. Grydeland M et al. |
NORWAY |
2012 2013 |
the HEalth in Adolescents (HEIA) Study |
2165 schoolchildren 11 y (1580 consent) | Multicomponent (promoting physical activity, reduce sedentary behaviors, and improve dietary outcomes). | 10 minutes of PA/week, increase awareness of PA, stimulating PA both in school time and in leisure time. | Usual school curriculum | Trained teachers |
20 months |
| Ezendam NP, et al. |
NETHERLANDS |
2012 |
FATaintPHAT |
883 students (12-13 y). |
Web-based computer-tailored intervention aiming to increase physical activity, decrease sedentary behavior, and promote healthy eating |
15 minutes for each 8 lessons during 10 weeks for a Web-based intervention individual-tailored, with information, assessment and feedback for behavior, and options to develop intention to prompt specific goal setting and action planning. | Usual school curriculum |
Teachers |
10 weeks + 2 years follow up |
| Collard DC, et al. |
NETHERLANDS |
2010 |
iPlay intervention |
2210 primary schoolchildren (10-12 y) |
Multicomponent intervention for children, parents and teachers, improving knowledge, attitude, and self-efficacy toward PA injuries prevention |
5 minutes of exercise during PE classes, aimed to improve strength, speed, flexibility and coordination. | Usual Physical Education Program |
Trained PE teachers |
8 months |
| Singh AS, et al. |
NETHERLANDS |
2007 2009 |
Dutch Obesity Intervention in Teenagers (DOiT) |
1053 adolescents (mean age, 12.7 years). |
Multicomponent (individual and environmental): (1) reduction of the consumption of sugar-sweetened beverages, (2) reduction of energy intake derived from snacks, (3) decrease of levels of sedentary behavior, and (4) increase of levels of physical activity (i.e. active transport behavior and sports participation). | Funding for two weekly hours of additional physical activity, under the following conditions: (1) the lessons should be supervised by a physical education teacher; (2) the lessons should fit within the school schedule (no break between the last official school lesson and the additional lesson physical activity); (3) a minimum number of twelve lessons should be taught between November 2003 and April 2004; (4) easy accessible activities, i.e. no specific knowledge or physical conditions necessary; (5) adolescents should be physically active during a major part of the lesson; (6) activities during the lessons should encourage adolescents to increase their leisure time physical activity as well. | Usual school curriculum |
PE Teachers |
8 months |
| Bonsergent E, et al. |
FRANCE |
2013 |
PRomotion de l'ALIMentation et de l'ActivitÉ Physique (PRALIMAP) |
5458 high school students (15.6±0.7y) |
Multicomponent prevention strategies: education (nutritional knowledge and skills); environment (creation of a favorable environment by improving availability of "healthy" dietary items and physical activity); screening and care (detection of overweight/obesity and, if necessary, adapted care management). | The 3 strategies (group A) Educational and environmental strategies (group B) Educational and screening strategies (group C) Screening and environmental strategies (group E) Educational strategy alone (group D) Environmental strategy alone (group F) Screening strategy alone (group G) For overweight/obese students: 7 educational session 1.5 hours each, by physicians, dieticians, sport educators and psychologists |
No intervention (group H) |
Trained health education professional, high school nurses, external nutrition health network |
2 years |
| Thivel D, et al. |
FRANCE |
2011 |
457 primary schoolchildren (6-10 y) |
PA intervention |
120 min (two times for 60 min) of supervised physical exercise in addition to 2 h of Physical Education classes per week. 10-min warm-up followed by psychometric activities and exercises to improve coordination, flexibility, strength, speed, and endurance. The content of the program was designed to enhance pleasure and enjoyment during exercise. |
Usual Physical Education Program |
Sports Sciences students, supervised by a member of the investigation staff. |
6 months |
|
| Simon C, et al. |
FRANCE |
2008 |
‘Intervention Centered on Adolescents’ Physical activity and Sedentary behavior’ (ICAPS) |
954 schoolchildren (12 y) |
Physical activity promotion by changing attitudes through debates and attractive activities, and by providing social support and environmental changes encouraging physical activity. |
PA activities, academic or less formal during breaks, organized by physical educators without any restrictive competitive aspect. Enjoyment of participation was highlighted to help the less confident children to develop the competences needed to adopt an active lifestyle. Sporting events and ‘cycling to school’ days were organized. Parents and educators were encouraged to provide support to enhance the adolescents’ physical activity level through regular meetings. |
Usual Physical Education Program (3 lessons/week each of 50 minutes) |
PE Teachers |
4 years |
| De Coen V, et al. |
BELGIUM |
2012 |
POP (Prevention of Overweight among Pre-school and schoolchildren | 1589 pre-primary and primary schoolchildren (3-6 y) |
Multicomponent (PA and healthy nutrition) |
Awareness for PA |
Usual school curriculum |
Teachers |
2 years |
| Haerens L, et al. |
BELGIUM |
2006 2007 |
2840 students (12-15 y) |
Physical activity and healthy eating intervention, including an environmental and computer-tailored component, with parental involvement. |
Extra physical activities, after school physical activities, sports material availability, a computer tailored intervention. 2 intervention groups: 1) with parent involvement (I+P) 2) without parent involvement (I) |
Usual school curriculum |
School staff |
2 years |
|
| Kipping RR, et al. |
UK |
2008 |
Active for Life year 5 |
679 children (5 y) |
16 lessons on healthy eating, physical activity and reducing TV viewing |
Nine PE lessons, the children played games based on the food groups using photographs of food that reinforced the theory taught in the nutrition lessons. | Usual school curriculum |
Trained teachers |
5 months |
| Sahota P, et al. |
UK |
2001 |
APPLES (Active Program Promoting Lifestyle Education in Schools) |
636 primary schoolchildren (7-11 y). |
Multidisciplinary Teacher training, modification of school meals, and the development of school action plans targeting the curriculum, physical education, tuck shops, and playground activities. | Promoting PA at school and at individual level | Usual school curriculum |
Trained teachers |
1 school year |
| Butcher Z, et al. |
UK | 2007 | |
177 primary schoolchildren (9 y) (data available for 141) | School-based program on PA with feedback (pedometer) |
Feedback plus information (FB+I) group: pedometer plus information on how to increase their step by day; Feedback (FB): only pedometer | Usual school curriculum |
Team researchers, teachers |
1 school week (5 days) |
| Hardman CA, et al. |
UK |
2011 | Fit 'n' Fun Dude |
386 primary schoolchildren (7-11 y) |
Physical activity intervention for children that comprised peer-modeling, pedometer step goals and tangible rewards. |
full intervention, where children received "Fit 'n' Fun Dude" peer-modeling materials (a song, a series of letters, a poster, a physical activity diary) and were given daily pedometer goals to receive rewards (balls, freesbee and erasers); no-rewards intervention, where children received peer-modeling materials and pedometer goals but rewards were not used |
Children wore pedometers with no further intervention. |
Researchers |
14 weeks |
| Chatzisarantis NL, & Hagger MS. |
UK |
2009 | 215 pupils (14,8 y) |
School-based intervention to change pupils' physical activity intentions and self-reported leisure-time physical activity behavior, based on self-determination theory |
PE teachers were instructed to use a autonomy-supportive interpersonal style by provide positive feedback and acknowledge the difficulties of PE classes, and to enhance sense of choice by using neutral modal operators when communicating rationale, positive feedback and acknowledge difficulties |
PE teachers were instructed to provide rationale by using the same list of meaningful arguments of the teachers in intervention group, but they were not instructed to enhance sense of choice by using neutral modal operators, nor to be empathetic and acknowledge difficulties | Trained teachers |
5 weeks |
|
| Magnusson KT, et al. |
ICELAND |
2011 2012 |
321 primary schoolchildren (7 y) |
Multi-component physical activity program, including re-structuring three physical education lessons each week and adding two extra lessons a week, daily short activity breaks, and physical activity homework | 1 additional PE session/week, specifically tailored to suit all children while maintaining a high level of intensity. |
Usual Physical Education Program (2 session of PE/week) |
PE Teachers |
2 years |
|
| Sacchetti R, et al. |
ITALY | 2013 | SAMBA project (Sorveglianza dell'AttivitÀ Motoria nei Bambini) | 497 schoolchildren (8-9 y) |
Enhanced program of Physical Education |
30 minutes/day of moderate to vigorous (in the schoolyard) or moderate (in the classroom) PE in adjunction to the usual PE | Usual Physical Education Program (2 session of PE/week, 50 minutes each) | Teachers supported by Physical Education teacher |
2 years |
| AraÚjo-Soares V, et al. |
PORTUGAL | 2009 |
291 adolescents (12- 16 y, mean age 12.3 y) |
Multicomponent intervention program designed to enhance levels of physical activity in adolescents, based on Social Cognitive Theory and Self Regulation Theory, including PA, a parent session, healthy eating, prevention of sexually transmitted diseases, prevention of smoking, alcohol and illicit drugs use. | Two classroom-based sessions of 90 minutes each and related homework |
Usual school curriculum |
Trained PE teachers, school psychologists |
12 weeks +3 and 9 months follow up |
|
| Angelopoulos PD, et al. |
GREECE | 2009 |
CHILDREN study |
656 schoolchildren (10 y) |
Intervention based on the Theory of Planned Behavior questionnaire, focused on overcoming the barriers in accessing physical activity areas, increasing the availability of fruits and vegetables and increasing parental support. |
Several motivational methods and strategies were used for increasing knowledge, increasing skills and self-efficacy, achieving better self-monitoring, changing attitudes and beliefs, and changing social influence. Parental support was required to encourage their children to be more active. | Usual school curriculum |
Trained teachers |
1 year |
| Marcus C, et al. |
SWEDEN | 2009 | STOPP (school and after school care-based obesity prevention program) | 3135 primary schoolchildren (6-10 y) |
Multicomponent (healthy eating habits and Physical Activity) |
Physical activity increased by 30 min/day during school time and sedentary behavior restricted during after school care time. | Usual school curriculum |
Teachers |
4 years |
Exp group= Experimental group; PA= Physical Activity; PE= Physical Education.
COUNTRIES
European Countries involved in physical activity school-based interventions were Spain (9 papers), Switzerland (7 papers), UK and Germany (6 papers each), The Netherlands (4 papers), Belgium, France, and Norway (3 papers each), and Iceland (2 papers); one paper each was found from Italy, Sweden, Portugal, and Greece. The included studies showed the results of preventive/intervention programs carried out throughout Europe; in some cases, more articles related to the same program were found. All of these articles were included (Table 1).
PROGRAMS
From Spanish papers we identified the following programs: EDUFIT [34-36], AVall [14, 15], MOVI [38,39], EdAl [6] and the Program SI! [7].
From Germany, we found papers that showed the findings of three programs: URMEL-ICE [16], JuvenTUM [11], and CHILT [28, 29 and 30].
From The Netherlands, the results of the iPlay [48], DOiT [22,23] and FATaintPHAT [12] programs were reported.
From UK, the programs were APPLES [31,32], Active for Life 5 years [25] and Fit’n’Dude [47].
Switzerland papers showed the results of KISS [42-46] and Ballabeina Study [18, 19].
From France, we retrieved the results of ICAPS [37] and PRALIMAP [13].
All the papers from Norway were related to the HEIA Study [8-10].
One of the Belgian papers was referred to the POP trial [17].
The Italian paper showed the results of the SAMBA Project [33].
The Swedish study reported the results of STOPP trial [24].
Finally, from Greece were retrieved the results of the CHILDREN project [20].
Several papers did not refer to a named program.
TYPES OF PROGRAMS/INTERVENTIONS
A large majority of interventions were multicomponent, aimed at increasing healthy habits and/or to reduce unhealthy or at-risk behaviors. The components of those interventions concerned physical activity as well as dietary habits (such as increasing consumption of fruit and vegetables, and/or decreasing the consumption of sweet and soft drinks, and fat intake), and reducing sedentary behaviors [6-2].
Other studies focused on solely physical activity interventions [33-52]. Table 1 shows the type of programs of the included studies.
Multicomponent (Healthy Habits and Physical Activity) Interventions
Among the trials focused on multicomponent interventions, or healthy lifestyle interventions, 9 included a Physical Activity (PA) component, consisting on PA promotion, awareness, recommendation, stimulation, rather than an actual PA intervention [6,7,12,13,17,20,22,23,26,27,31,32]. Those interventions, in some cases, also included parental involvement or support in take-home activities [6,7,20], and/or attempted to change school environment [13,20,22, 23,26,27,31,32].
On the other hand, 8 interventions focused on healthy lifestyle intervention including an actual PA component, with parental support [11,16,21], social/environment changes/opportunities [8,9,10,14,15,18,19,24], or with a stronger individual component, consisting in enhanced Physical Education lessons in adjunction to healthy topics lessons [28-30].
The contents of such PA interventions widely varied. The JuvenTUM project used monthly lessons lasting 45 minutes, with three parts: a warm-up of 10 min with running, playing running games at high intensity, 30 min exercises to improve body awareness and self-esteem with conversation in class about health-related topics, and 5 min relaxation exercises [11]. The URMEL-ICE (Ulm Research on Metabolism, Exercise, and Lifestyle Intervention in Children) intervention used 2 short daily exercise blocks (each 5-7 minutes) [16]. Araujo-Soares and colleagues focused their PA intervention on two 90 minutes lessons of Physical Education and related homework [21]. The HEIA (Health In Adolescents) study included weekly activity breaks during academic lessons [8-10]. The AVall study provided 3 hours/week to develop activities related to PA (games, crafts) within the regular classes [14, 15]. The Ballabeina study enhanced PE regular lessons with 4 sessions/week of 45 minutes each of PA, organized as playful games, aimed at increasing aerobic fitness and coordination skills [18,19]. The STOPP (School and after school care-based Obesity Prevention Program) trial increased PA by 30 min/day during school time and restricted sedentary behavior during after school care time [24]. The CHILT (Children’s Health Interventional Trial)
project provided various combination of exercise daily performed at least once each morning during lessons for at least five minutes [28-30].
PA Interventions
Among the studies focused on solely PA school-based intervention, the most were devoted to enhancing moderate to vigorous PA [33-36,40-46,51], other developed interventions based on moderate, recreational, pleasant, non-competitive PA [37-39,52]; moreover, the Fit’n’Dude intervention [47] and the one by Butcher et al. [49] attempted to increase PA by using feedback (pedometers), without a direct PA intervention, while the iPlay intervention focused on a PA intervention aimed to prevent physical injuries during PA with a modified PE program [48], and Chatzisarantis and colleague aimed to modify teacher’s behavior during PE lessons [50].
Interventions enhancing moderate to vigorous PA were aimed to increase the usual PE programs. The SAMBA (Sorveglianza dell’Attività Motoria nei Bambini, i.e. Surveillance of Physical Activity in Children) project ensured 30 minutes/day of vigorous (in the schoolyard) or moderate (in the classroom) PA [33]. The EDUFIT (EDUcational for FITness Study) intervention provided 4 weekly sessions of 55 minutes each of PE, with a group exercising at high intensity [34-36]. Magnusson and colleagues restructured the existing PE lessons and added one additional lesson specifically tailored to maintain high intensity PA levels [40, 41]. The KISS trial focused on 2 additional PE weekly lessons, with at least 10 minutes of high intensity exercises, and 3-5 short daily activity breaks of 2-5 minutes each during academic lessons [42-46]. Walther and colleagues increased the usual PE program with daily lessons of 45 minutes each, with at least 15 minutes of endurance training [51].
Who Delivered the Intervention
Generally, the interventions were delivered by teachers (usual classroom teachers, in the case of primary schoolchildren, or PE teachers, in the case of studies carried out in middle or high schools), specially trained for the purpose. In the EdAl study, University Medicine or Health Sciences students delivered the intervention as a part of their curriculum [6]. Similarly, Thivel and colleagues had Sports Science students, supervised by researchers’ team [52]. In the
PRALIMAP study, the intervention was delivered by health professionals and high school nurses [13]. Araujo-Soares et al. had trained PE teachers and school psychologist [21]. In the Fit’n’Dude study, the intervention was delivered by the researchers [47], while in the one carried out by Butcher et al. both the teachers and the researchers delivered the intervention [49]. In the case of the study performed by Haerens et al., it was the school staff to give out the intervention [26, 27] (Table 1).
CONTROL GROUPS
A large majority of the studies had control group that carried out the usual curriculum. In the Fit’n’Dude study, the control group wore pedometers with no further intervention [47], and Chatzisarantis & Hagger had PE teachers in the control group trained to provide rationale of PE lessons by using the same list of meaningful arguments of the teachers in the intervention group, without changing the way to teach [50] (Table 1).
SAMPLES
The populations in the selected studies widely ranged between 5458 (in the PRALIMAP intervention [13]) and 67 pupils (in the EDUFIT study [34-36]), with a mean (± SD) of 1145.76 ± 1126.28 (considering each intervention only one time). Four studies had preschooler samples [7, 17-19, 25], eight studies had middle school students [8-10,12,21-23,26,27,34-37,51], two had high school students [13,50], while the remaining had primary schoolchildren populations. All interventions were universally delivered, i.e. delivered for all the pupils in the classroom/school; nevertheless, one intervention (the PRALIMAP study) provided special care (screening and management) for obese students [13] (Table 1).
DURATION
The duration of the interventions varied between 1 school week (i.e. 5 days) [49] and 4 school years [24,39]; the mean (±SD) duration per intervention was 12.10±9.04 months. Moreover, the FATaintPHAT [12], the AVall [14, 15], the KISS [42, 46], the DOiT [22,23], the CHILT [28-30], and the one carried out by Araujo-Soares and colleagues [21] had a follow up, with duration between 9 months and 4 years (Table 1).
OUTCOMES AND ASSESSMENTS
Physical Activity interventions are generally aimed to prevent or reduce obesity and overweight. Thus, among the main outcomes declared by the authors of the selected papers, over 30 trials, 16 assessed a change in Body Mass Index (BMI) [6,13-25, 28-31,37-39,41,52]. Moreover, BMI was assessed as secondary outcome in 8 trials [8,11,12,33,35,44, 45,47,51].
A change in body fat, assessed by measuring waist circumference and/or skinfolds, and changes in the percentage of body composition, such as lean and fat mass (assessed by bioelectrical impedance analysis, or dual energy X-ray scan), was the primary outcome in four trials [38, 39,41,44,52] and a secondary outcome in eight [6, 11, 12, 16, 18, 19, 35, 37, 47]. Moreover, changes in bone composition, i.e. bone mineral content and density (assessed by dual energy X-ray scan) was the primary outcome in a secondary analysis of the KISS trial [42, 43].
The decrease of cardiovascular/metabolic risk factors, assessed by measuring fasting levels of total cholesterol, high-density lipoprotein cholesterol (HDLc), low-density lipoprotein cholesterol (LDLc) and triglycerides, glucose, insulin, blood systolic/diastolic pressure, was the main outcome in the EDUFIT study [34-36] and as secondary outcome in five other trials [20, 37, 39, 44, 51].
An increase in PA/decrease in sedentary habits (generally assessed by self-reported questionnaires, or by accelerometer/pedometer) was assessed as the main outcome in 14 trials [8, 11, 12, 16, 21, 24-27, 31, 41,44, 47, 49, 50], and a secondary outcome in other 7 [14, 15, 17, 19, 20, 23, 37, 42, 45].
Physical fitness, generally assessed by the 20 m shuttle run test, was considered the main outcome in 4 trials [18,35, 44, 51], and a secondary outcome in 5 trials [11, 12, 22,41, 52].
Three trials considered physical abilities/performance, measured by motor/coordination tests for children, evaluating balance, flexibility, coordination, agility, and muscle strength, as the main outcome [28-30, 33, 35], and two others as a secondary outcome [18,19, 51].
Moreover, several studies assessed changes in children’s behavior, attitudes and habits (such as sleep, eating behavior, screen viewing, playing outdoor, sweet beverages consumption) as a primary [7, 11, 12, 25, 31, 32] or a secondary outcome [6, 13, 15, 16, 17, 19, 20, 23, 24, 26].
Psychological outcomes, such as enjoyment in PA, self-efficacy, perceived support (from parents, teachers, school, friends), perceived social inclusion, were assessed as a primary outcome in the HEIA study [9, 10] and a secondary outcome in the studies performed by Araujo-Soares and colleagues [21] and Chatzisarantis & Hagger [50], as well as in the ICAPS study [37]. Quality of Life was as a primary outcome in the KISS study [44, 45], and a secondary outcome in the Ballabeina study [19]. The children’s psychological state, i.e. the presence of anxiety and depression, was a primary outcome in the APPLES study [31], and a secondary outcome in the PRALIMAP study [13].
Cognitive performance and academic achievement were considered as a secondary outcome in two studies [19, 34].
The cost-effectiveness of the intervention was the secondary outcome in the MOVI trial [39]. Table 2 shows main and secondary outcomes, assessment and results of the selected trials.
Table 2.
Outcomes, assessment and main results of the included studies.
| Author(s), year | Name of trial | Main outcomes | Secondary outcomes | Assessment | Results |
|---|---|---|---|---|---|
| PeÑalvo et al., 2013 |
The Program SI! |
Children's change in knowledge, attitudes and habits (KAH) |
Parents', teachers' and school environment's change in knowledge, attitudes and habits |
Questionnaires (KAH-diet, KAH-physical activity, and KAH-human body; for children: Test of Emotional Comprehension (TEC) assessed by psychologists |
Increased children's KAH scores, both overall (3.45, 95% CI, 1.84-5.05) and component-specific (Diet: 0.93, 95% CI, 0.12-1.75; Physical activity: 1.93, 95% CI, 1.17-2.69; Human body: 0.65, 95% CI, 0.07-1.24) score. No difference on emotions. |
| Tarro et al., 2014 |
The EdAl (EducaciÓ en AlimentaciÓ) study |
BMI |
BMI z-score, waist circumference, eating habits and Physical Activity |
Anthropometric measurements, questionnaires (Krece Plus Questionnaire for eating patterns, and AVall Questionnaire for PA) |
At 28 months, obesity prevalence decreased in boys in the intervention compared to the control group (p= 0.02). BMI z-score was significantly lower in the intervention group compared to controls (overall: p < 0.001; boys: p < 0.001; girls: p < 0.001). For pre- versus post-intervention, the BMI z-score increase was significant only in boys in the control group (p= 0.015). Waist circumference changed significantly between the first and third year of the study in the intervention and control groups (p= 0.043). At 28 months, BMI was not statistically different in the intervention and control groups (p= 0.381). The incidence of overweight was significantly higher in the control group than in the intervention group (p= 0.021), particularly in boys in the control group compared to boys in the intervention group (p= 0.011). Girls did not present significant differences between the control and intervention groups. Remission of excess weight was not significantly different between the intervention and control groups, nor in relation to gender. The percentage of pupils that perform >5 hours/week PA significantly increased in the intervention group (boys: p< 0.001; girls: p= 0.005), while did not in the control group. In the intervention group, the percentage of pupils consuming pastry before setting off for school and in the mid-morning break decreased (respectively p= 0.005 and p< 0.001). In the control group, the percentage of pupils consuming pastries in the mid-morning break also decreased (p= 0.002) while the consumption of fruit or natural juice increased (p= 0.05). There were no significant differences between groups with respect to other nutritional habits. |
| Ardoy et al., 2011 |
EDUFIT (EDUcational for FITness Study) |
Fasting levels of total cholesterol, high-density lipoprotein cholesterol (HDLc), low-density lipoprotein cholesterol (LDLc) and triglycerides | Cardiorespiratory fitness, BMI, skinfold thicknesses |
Blood samples, anthropometric measurements and shuttle run test |
The intervention did not positively affect cardio-metabolic parameters except for LDLc, that was marginally yet significantly reduced in EG2 compared with the CG (p = 0.04); no differences were observed however for the LDLc/HDLc ratio. No significant effects were observed in EG1. |
| LlarguÉs et al., 2011 and 2012 |
The AVall Study | BMI | Changes in PA and food habits |
Anthropometric measurements, questionnaires |
At the end of the study period of 2 years, the intervention group presented a lower increase of the BMI (p<0.001) than controls. In the intervention group, there was a non-significant increase in nut intake (p=0.056) and also a slight reduction of daily time devoted to sedentary activities (p=0.061). |
| Martinez VizcaÌno et al., 2011 |
The MOVI Program | BMI, triceps skin-fold thickness (TST), percentage fat mass, blood lipides |
Anthropometric measurements, bioimpedenzometry, blood samples |
There were no differences in BMI between the intervention and control groups. Compared with controls, intervention children showed a decrease in TST in both boys (p<0.001) and girls (p<0.001), as well as a reduction in the percentage of body fat in girls (p=0.02). The intervention boys exhibited a decrease in apolipoprotein (apo) B levels (p=0.03) and an increase in apo A-I levels (p<0.001). Blood lipid results in girls were very similar. No changes in total cholesterol, triglycerides or blood pressure were associated with the intervention in either sex, except for an increase in diastolic blood pressure (p=0.03) in the intervention versus control boys. | |
| Moya Martinez et al., 2011 |
The MOVI Program | BMI, triceps skin-fold thickness (TST), percentage fat mass, blood lipides |
Cost effectiveness of the intervention |
Anthropometric measurements, bioimpedenzometry, blood samples |
The intervention costs totaled 125,469.75€, representing 269.83 €/year/child. The usual after-school care was estimated at 844,56 €/year/child. Intervention children showed a decrease in TST (p<.001). Intervention children with body mass index (BMI) between the percentiles 25 and 75 showed a decrease in the percentage of body fat (p<.001), and those with a BMI percentile>75 showed a decrease in TST (p<.001), and percentage of body fat (p<.05). |
| Brandstetter et al., 2012 |
URMEL-ICE (Ulm Research on Metabolism, Exercise, and Lifestyle Intervention in Children) |
BMI |
Waist circumference and skinfold thickness, child's behavior (soft-drinks consumption, playing outdoor frequency, TV watching) |
Anthropometric measurements, parent's questionnaire |
There was not statistically significant effect of the intervention on BMI, but on waist circumference (-0.85; 95% confidence interval (95% CI) -1.59 to -0.12) and subscapular skinfold thickness (-0.64; 95% CI -1.25 to -0.02). After additional adjustment for individual time lag between baseline and follow-up, these effects were reduced to -0.60 (95% CI -1.25 to 0.05) and -0.61 (95% CI -1.26 to 0.04) and lost their statistical significance. |
| Siegrist et al., 2013 |
The JuvenTUM project |
Daily PA |
BMI, waist circumference, physical fitness, media consuption |
Daily physical activity (≥ 60 min/day), physical fitness (Munich Fitness Test, six-item test battery), and anthropometric data | Physical activity and physical fitness increased in IS, but it failed to reach significant intervention effects. Nevertheless, a reduction in waist circumference was observed for all children (p< 0.001). This effect was more pronounced in overweight children (> 90th percentile, p < 0.001). |
| Walther et al., 2009 |
Change in VO2max |
BMI, BMI–standard deviation score, blood pressure, heart rate, coordination, total cholesterol, low-density lipoprotein, high-density lipoprotein cholesterol, and triglycerides; circulating endothelial progenitor cells (CPCs), migratory function of CPCs |
Anthropometric measurements, tredmill exercise test with spirometry, Body Coordination Test for Children, blood sample |
The significant effects of intervention estimated from ANCOVA adjusted for intraclass correlation were the following: increase of peak O(2) (3.7 mL/kg per minute; 95% confidence interval, 0.3 to 7.2) and increase of circulating progenitor cells evaluated by flow cytometry (97 cells per 1 x 10(6) leukocytes; 95% confidence interval, 13 to 181). No significant difference was seen for BMI standard deviation score (-0.08; 95% confidence interval, -0.28 to 0.13); however, there was a trend to reduction of the prevalence of overweight and obese children in the intervention group (from 12.8% to 7.3%). No treatment effect was seen for motor and coordinative abilities (4; 95% confidence interval, -1 to 8) and high-density lipoprotein cholesterol (0.03 mmol/L; 95% confidence interval, -0.08 to 0.14). | |
| Graf et al., 2004 |
Children's Health InterventionaL Trial (CHILT) project |
BMI, motor abilities |
Anthropometric measurements, body gross motor development test for children (KÖperkoordinationstest fÜr Kinder; KTK) and a 6-min run. |
The children were 6.70±0.42 y old, 122.72±5.36 cm tall and weighed 24.47±4.59 kg, the average BMI was 16.17±2.27 kg/m2. KTK showed an average motor quotient (MQ) of 93.49±15.01, the 6-min run an average of 835.24±110.87 m. Both tests were inversely correlated with BMI (KTK and BMI r=-0.164 (p<0.001); 6-min run and BMI r=-0.201 (p<0.001)); the group of overweight/obese children showed poorer results than the normal/underweight ones, even after adjustment for gender and age (in each case p<0.001). Children with the greatest extent of exercise achieved the highest MQ (p=0.035). | |
| Graf et al., 2005 |
Children's Health InterventionaL Trial (CHILT) project |
BMI, motor abilities |
Anthropometric measurements, lateral jumping and endurance performance by a 6-minute run. |
No difference in the prevalence of overweight and obesity was found between the intervention and control schools either at baseline or following intervention (each p> 0.05). The increase in the number of lateral jumps was significantly higher in the intervention group than in the controls (p< 0.001). For the 6-minute run the increase in distance run was significantly improved in intervention group (p= 0.020). Overweight and obese children in both groups produced significantly lower scores in coordination and endurance tasks than normal and underweight children during both examinations (each p≤ 0.001), adjusted for gender and age. | |
| Graf et al., 2008 |
Children's Health InterventionaL Trial (CHILT) project (4 year follow up) |
BMI, physical performance |
Anthropometric measurements, coordination test for children (balancing backwards, one-legged obstacle jumping, lateral jumping, sideways movements) and a 6-min run (endurance). |
No difference in the prevalence and incidence of overweight and obesity was found between the intervention and control schools before and after the intervention. Remission of overweight was higher in the intervention schools (23.2 vs. 19.2%), but not significant. An increase in coordination related to lateral jumping and balancing backwards was apparent in the intervention schools (respectively, p= 0.005 and p= 0.007), and the increase in endurance performance was higher in intervention schools (p= 0.055), adjusted for age, sex, baseline test result, and BMI at final examination. | |
| Kriemler et al., 2010 |
KISS (Kinder-Sportstudie) |
Body fat (sum of four skinfolds), aerobic fitness, physical activity (accelerometry), and quality of life (QoL). |
BMI and cardiovascular risk score (average z score of waist circumference, mean blood pressure, blood glucose, inverted HDL-cholesterol, and triglycerides). |
Anthropometric measurements, 20-m shuttle test (20–MST), accelerometer, Child Health Questionnaire (QoL), blood sample |
Children in the intervention group compared with controls showed a decrease in the z score of the sum of four skinfolds (p=0.009). In the intervention group, z scores for aerobic fitness increased more favourably (p=0.04), as well as moderate-vigorous PA in school (p<0.001), all day moderate-vigorous PA (p=0.03), and total PA in school (p=0.003). Z scores for overall daily PA, physical and psychological QoL did not change significantly. |
| Hartmann et al., 2010 a |
KISS (Kinder-Sportstudie) |
Quality of Life |
BMI |
Child Health Questionnaire |
Physical QoL in first graders and physical and psychosocial QoL in fifth graders were not affected by the intervention. In first graders, the PA intervention had a positive impact on psychosocial QoL (p < .05). Subpopulation analyses revealed that this effect was caused by an effect in urban (p < .05) and overweight first graders (p < .05). |
| Hartmann et al., 2010 b |
KISS (Kinder-Sportstudie) |
Perceived Physical Health, Fear of Negative Evaluation (FNE) |
Physical activity |
Child Health Questionnaire, Social Anxiety Scale for Children—Revised, accelerometer. |
Cross-sectional analyses indicated that children high in FNE exercised less, reported lower levels of PPH and had higher BMI z-scores (p<0.01). Using mixed linear models, the school-based PA intervention did not manage to reduce FNE scores. Overweight children demonstrated a greater increase in FNE (p<0.05) indicating that enhanced weight may be a risk factor for FNE. |
| Meyer et al., 2011 |
KISS (Kinder-Sportstudie) |
Bone Mineral Content (BMC) and Bone Mineral Density (BMD) |
Physical activity |
Dual-energy X-ray absorptiometry (DXA), accelerometer |
Compared to controls, children in intervention group showed statistically significant increases in BMC of total body, femoral neck, and lumbar spine (all p<0.05), respectively, and BMD of total body and lumbar spine (both p<0.01), respectively. There was no gender *group, but a pubertal stage *group interaction consistently favoring prepubertal children. |
| Meyer et al., 2013 |
KISS (Kinder-Sportstudie) 3 year follow up |
Bone Mineral Content (BMC) and Bone Mineral Density (BMD) |
Dual-energy X-ray absorptiometry (DXA) |
At follow-up, the intervention group showed significantly higher Z-scores of BMC at total body (p=0.015), femoral neck (p=0.042) and at total hip (p=0.016) and higher Z-scores of aBMD for total body (p=0.030) compared to controls, representing 6-8% higher values in favour of intervention groups. No differences could be found for the remaining bone parameters. For the subpopulation with baseline VPA (n=163), effect sizes became stronger after baseline VPA adjustment. After adjustment for baseline and current VPA (n=101), intervention effects were no longer significant, while effect sizes remained the same. | |
| Puder et al., 2011 |
The Ballabeina Study | Aerobic fitness, BMI |
Motor agility, balance, percentage body fat, waist circumference, physical activity, eating habits, media use, sleep, quality of life, and cognitive abilities. |
Anthropometric measurements, 20-m shuttle test (20–MST), accelerometer, dynamic and static balance tests, accelerometer, bioelectrical impedence, QoL questionnaire (PedsQL 4.0), attention and spatial working memory tests, eating, sleep and screen view habits questionnaires. |
Compared with controls, children in the intervention group had an increase in aerobic fitness at the end of the intervention (p=0.01) in motor agility (p=0.004), percentage body fat (p=0.02), and waist circumference (p=0.001), but no difference in BMI (p=0.31). There were also significant benefits in the intervention group in reported physical activity, media use, and eating habits, but not in the remaining secondary outcomes. |
| Niederer et al., 2013 |
The Ballabeina Study |
Aerobic fitness, BMI |
Sum of four skinfolds, waist circumference and motor agility. |
Anthropometric measurements, 20-m shuttle test (20–MST) |
Compared to their counterparts, overweight children (n = 130) had more beneficial effects on waist circumference (p for interaction= 0.001), and low fit children (n= 154) more beneficial effects on all adiposity outcomes (p for interaction≤0.03). The intervention effects on both fitness outcomes were not modified by BMI- or fitness-group (all p for interaction ≥0.2). |
| Bergh et al., 2012 a |
The HEalth in Adolescents (HEIA) Study |
Enjoyment, self-efficacy, perceived social support from parents, teachers and friends related to PA, perceived parental regulation of TV-viewing and computer/game-use and perceived social inclusion at schools |
Covariance analyses to assess overall effects and moderation by gender, weight status and parental education, mid-way and post-intervention. Covariance analyses were also used to examine the role of intervention dose received on change in the determinants |
At mid-way, enjoyment (p= .03), perceived social support from teachers (p= .003) and self-efficacy (p= .05) were higher in the intervention group. Weight status moderated the effect on self-efficacy, with a positive effect observed among the normal weight only. At post-intervention results were sustained for social support from teachers (p= .001), while a negative effect was found for self-efficacy (p= .02). Weight status moderated the effect on enjoyment, with reduced enjoyment observed among the overweight. Moderation effects for parental education level were detected for perceived social support from parents and teachers. Positive effects on several determinants were observed among those receiving a high as opposed to a low intervention dose. | |
| Bergh et al., 2012 b |
The HEalth in Adolescents (HEIA) Study |
Six theoretical mediators of the PA intervention: enjoyment of PA, self-efficacy, perceived social support from parents, friends and teachers, perceived environmental opportunities |
Questionnaire |
None of the personal, social or physical-environmental constructs targeted in the intervention were found to mediate the PA outcome. The only mediator positively affected by the intervention was perceived social support from teachers. The subgroup analyses revealed that this effect was present in girls and normal weight adolescents only. | |
| Grydeland et al., 2013 |
The HEalth in Adolescents (HEIA) Study |
Increase PA, decrease sedentary activities |
BMI |
Accelerometer, anthropometric measurements |
Intervention effect on overall physical activity at the level of p=0.05, with a net effect of 50 cpm (count per minute), increased from baseline to post intervention in favour of the intervention group. Subgroup analyses showed that the effect appeared to be more profound among girls (p=0.03) and among participants in the low-activity group (p<0.001), as compared to boys and participants in the high-activity group, respectively. Furthermore, the intervention affected physical activity among the normal weight group more positively than among the overweight, and participants with parents having 13-16 years of education more positively than participants with parents having either a lower or higher number of years of education. The intervention seemed to reduce sedentary activities among girls but not among boys. |
| Ezendam et al., 2012 |
FATaintPHAT | Self-reported behaviors (diet, physical activity, sedentary behavior), PA (at 4 months assessment) |
BMI, body fat and physical fitness (at 2 year follow up) |
Questionnaire, pedometer, anthropometric measurements, shuttle-run test |
The intervention had no effect on BMI and waist circumference. However, it was associated with lower odds (0.54) of drinking more than 400 mL of sugar-sweetened beverages per day and with lower snack intake (β = -0.81 snacks/d) and higher vegetable intake (β = 19.3 g/d) but also with a lower step count (β = -10 856 steps/wk) at 4-month follow-up. In addition, among students at risk, FATaintPHAT had a positive effect on fruit consumption (β = 0.39 g/d) at 4-month follow-up and on step count (β = 14 228 steps/wk) at 2-year follow-up but an inverse effect on the odds of sports participation (odds ratio, 0.45) at 4-month follow-up. No effects were found for sedentary behavior. |
| Collard et al., 2010 |
iPlay intervention |
PA IID (number of injuries per 1000 hours of sports participation) and injury severity |
Questionnaire, anthropometric measurements |
The IID (number of injuries per 1000 hours of sports participation) for total PA participation was 0.38 (95% CI, 0.31-0.46) in the intervention group, compared with 0.48 (95% CI, 0.38-0.57) in the control group. In the low active group, effects of the iPlay program were much larger, with a 50% reduction in total injuries (HR,0.47; 95% CI, 0.21-1.06) and a more than 50% reduction for sports injuries (HR,0.23; 95% CI, 0.07-0.75) and leisure time injuries (HR,0.43; 95% CI, 0.16-1.14). Children in the intervention group reported fewer severe injuries than those in the control group. The multilevel logistic regression analyses showed that there was no significant difference between the intervention and control groups in the percentage of children with sporting time lost. | |
| Singh et al. 2007 |
Dutch Obesity Intervention in Teenagers (DOiT) |
Waist and hip circumference, skinfolds, and BMI class |
Aerobic fitness |
Anthropometric measurements, 18 m shuttle run test |
Multilevel analyses showed significant differences in changes after the 8-month intervention period in favor of the intervention group with regard to hip circumference (mean difference, 0.53 cm; 95% confidence interval, 0.07 to 0.98) and sum of skinfolds among girls (mean difference, −2.31 mm; 95% confidence interval, −4.34 to −0.28). In boys, the intervention resulted in a significant difference in waist circumference (mean difference, −0.57 cm; 95% confidence interval, −1.10 to −0.05). No significant intervention effects were found related to BMI and aerobic fitness. |
| Singh et al. 2009 |
DOiT (Dutch Obesity Intervention in Teenagers) |
BMI, waist circumference, 4 skinfold thickness measurements |
Changes in dietary and physical activity behavior |
Anthropometric measurements, questionnaires |
The intervention remained effective in preventing unfavorable increases in important measures of body composition after 20-month follow-up in girls (biceps skinfold and sum of 4 skinfolds) and boys (triceps, biceps, and subscapular skinfolds). No significant effect was found on BMI. Consumption of sugar-containing beverages was significantly lower in intervention schools both after intervention (boys: -287 mL/d; 95% confidence interval [CI], -527 to -47; girls: -249; -400 to -98) and at 12-month follow-up (boys: -233; -371 to -95; girls: -271; -390 to -153). For boys, screen-viewing behavior was significantly lower in the intervention group after 20 months (-25 min/d; 95% CI, -50 to -0.3). No significant intervention effects on consumption of snacks or active commuting to school were found. |
| Bonsergent et al., 2013 |
PRALIMAP (PRomotion de l'ALIMentation et de l'ActivitÉ Physique) |
BMI percentile |
BMI z-score , prevalence of overweight and obesity, eating attitudes, anxiety and depression |
Anthropometric measurements, questionnaires (Eating Attitudes Test 40 (EAT-40) and Hospital Anxiety and Depression (HAD)) |
The 2-year change of outcomes was more favorable in the 12 screening and care high schools compared to the no-screening ones: a 0.11 lower increase in BMI (p=0.0303); a 0.04 greater decrease in BMI z-score (p=0.0173); and a 1.71% greater decrease in overweight/obesity prevalence (p=0.0386). Education and environment strategies were not more effective than no strategy intervention. |
| Thivel et al., 2011 |
BMI, body fat |
Aerobic and anaerobic fitness |
Anthropometric measurements, 4 skinfold thickness, 20-m shuttle run test, cycling peak power test |
The intervention did not yield positive anthropometric improvements, but appears effective in terms of aerobic and anaerobic physical fitness in both lean and obese children. | |
| Simon et al., 2008 |
ICAPS (ntervention Centered on Adolescents’ Physical activity and Sedentary behavior) |
BMI |
Changes in body composition, PA, PA attitudes, self-efficacy, cardiovascular risk factors |
Anthropometric measurements, bioelectrical impedance analysis, blood samples, self-reported leisure PA (Modifiable Activity Questionnaire for adolescents), self efficacy (Stanford Adolescent Heart Health Program’s questionnaire), blood sample (plasma glucose, total and high-density lipoproteincholesterol, triacylglycerols and insulin) |
Intervention students had a lower increase in BMI (p=0.01) and age- and gender-adjusted BMI (p<0.02) over time than controls. An interaction with baseline weight status was noted. The intervention had a significant effect throughout the study in initially non-overweight adolescents, corresponding to a lower increase in fat mass index (p<0.001). In initially overweight adolescents, the differences observed across groups at 2 years did not persist over time. At 4 years, 4.2% of the initially non-overweight adolescents were overweight in the intervention schools, 9.8% in the controls (p<0.01). Independent of initial weight status, intervention adolescents had an increase in supervised physical activity (p<0.0001), a decrease of TV/video viewing (p<0.01) and an increase of high-density cholesterol concentrations (p<0.0001) compared with controls. |
| De Coen et al., 2012 |
POP (Prevention of Overweight among Pre-school and schoolchildren) |
BMI z-score |
Eating behavior, physical activity and screen-time. |
Anthropometric measurements, questionnaires |
No significant effects were found on BMI Z-scores for the total sample. However, there was a significant decrease in BMI Z-score of 0·11 in the low-SocioEconomicStatus intervention community compared with the low-SES control community, where the BMI Z-score increased by 0·04 (p= 0·01). No significant intervention effects could be found for eating behaviour, physical activity or screen-time. There were no significant interaction effects of age and gender of the children on the outcome variables |
| Haerens et al., 2006 |
Physical Activity |
Fat intake, fruit, water and soft drink consumption |
Questionnaires (Flemish Physical Activity Questionnaire (FPAQ), questionnaire on food intake), accelerometer |
The intervention showed significant effects on PA in both genders and on fat intake in girls. Parental involvement did not increase intervention effects. In boys, significant 2-year post-baseline intervention effects on levels of PA, but not on eating behaviours, were found. School-related PA increased significantly more in the intervention groups compared with controls (p< 0.05). Accelerometer data revealed a trend for significant lower decreases in low-intensity PA in the intervention groups compared with controls (p< 0.001). Time spent in MVPA remained stable in the intervention group, while it significantly decreased in the controls (p< 0.05). In girls, significant 2-year post-baseline intervention effects were found for both PA and eating behaviours. In girls, the intervention was effective in preventing decreases of low intensity PA. Time spent in low-intensity PA decreased significantly less in the intervention groups compared with the controls (p< 0.05). Decreases in fat intake and percent energy from fat were significantly higher in the intervention groups compared with the controls (p< 0.05). | |
| Haerens et al., 2007 |
PA levels |
Accelerometer, questionnaire |
The intervention with parental support led to an increase in self-reported school-related PA of, on average, 6.4 minutes per day (p≤ .05). Low intensity PA measured with accelerometers decreased with, on average, 36 minutes per day as a result of the intervention with parental support (p≤.05). MVPA measured with accelerometers significantly increased with on average 4 minutes per day in the intervention group with parental support, while it decreased with almost 7 minutes per day in the controls (p ≤ .05, d = .46). | ||
| Kipping et al., 2008 |
Active for Life year 5 |
Hours of screen activities, body mass index, mode of transport to school and teachers' views of the intervention. |
Anthropometric measurements, questionnaires |
Children from intervention schools spent less time on screen-viewing activities after the intervention but these differences were imprecisely estimated: mean difference in minutes spent on screen viewing at the end of the intervention (intervention schools minus control schools) adjusted for baseline levels and clustering within schools was -11.6 (95% CI -42.7 to 19.4) for a week day and was -15.4 (95% CI -57.5 to 26.8) for a Saturday. There was no difference in mean body mass index or the odds of obesity. | |
| Sahota et al., 2001 a |
APPLES (Active Program Promoting Lifestyle Education in Schools) |
BMI, diet, physical activity, and psychological state. |
Anthropometric measurements, 3-day food diary and 24h-recall, questionnaires |
Vegetable consumption by 24 hour recall was higher in children in the intervention group than the control group (weighted mean difference 0.3 portions/day, 95% confidence interval 0.2 to 0.4), representing a difference equivalent to 50% of baseline consumption. Fruit consumption was lower in obese children in the intervention group (-1.0, -1.8 to -0.2) than those in the control group. The three day diary showed higher consumption of high sugar foods (0.8, 0.1 to 1.6)) among overweight children in the intervention group than the control group. Sedentary behaviour was higher in overweight children in the intervention group (0.3, 0.0 to 0.7). Global self worth was higher in obese children in the intervention group (0.3, 0.3 to 0.6). There was no difference in body mass index, other psychological measures, or dieting behaviour between the groups. | |
| Sahota et al., 2001 b |
APPLES (Active Program Promoting Lifestyle Education in Schools) |
Response rates to questionnaires, teachers' evaluation of training and input, success of school action plans, content of school meals, and children's knowledge of healthy living and self reported behaviour. |
Questionnaire |
All 10 schools participated throughout the study. 76 (89%) of the action points determined by schools in their school action plans were achieved, along with positive changes in school meals. A high level of support for nutrition education and promotion of physical activity was expressed by both teachers and parents. 410 (64%) parents responded to the questionnaire concerning changes they would like to see implemented in school. 19 out of 20 teachers attended the training, and all reported satisfaction with the training, resources, and support. Intervention children showed a higher score for knowledge, attitudes, and self reported behaviour for healthy eating and physical activity. | |
| Butcher et al., 2007 |
Steps/minutes |
Pedometer |
Students in the FB+I group achieved significantly more steps per minute than those in the FB (p= 0.003) and CON (p= 0.0001) groups. | ||
| Hardman et al., 2011 |
Fit 'n' Fun Dude |
Physical Activity |
BMI, waist circunference |
Steps per day, anthropometric measurements |
During the intervention, the full intervention school showed the largest increase in physical activity relative to baseline (p< 0.001). There was a smaller increase in the no-rewards school (p< 0.03), and no significant change in the control. At the end of the taper phase, physical activity in the no-rewards school continued to increase (p< 0.001) but had returned to baseline in the full intervention school. The intervention that used only peer-modelling and pedometer goals produced better effects over time. No effect was found for either intervention on BMI and waist circumference compared with controls. |
| Chatzisarantis & Hagger, 2009 |
Self reported vigorous PA |
Teacher's autonomy support perceived, intention to perform leisure time PA, |
Leisure Time Exercise Questionnaire |
Pupils who were taught by autonomy-supportive teachers reported stronger intentions to exercise during leisure time and participated more frequently in leisure-time physical activities than pupils in the control condition. Autonomous motivation and intentions mediated the effects of the intervention on self-reported physical activity behaviour. | |
| Magnusson et al., 2011 |
Physical Activity |
BMI percentile |
PA was assessed by means of accelerometers and subjectively at the intervention schools via teachers' PA log-books; anthropometric measurements |
There was no difference in PA intensity (minutes of moderate-to-vigorous physical activity - min of MVPA) between the two study groups at baseline, but children in the intervention schools were more physically active at moderate-to-vigorous intensity compared to those in control schools after one year of intervention (p= 0.04). A significantly greater increase of MVPA was showed among the boys in the intervention schools compared to girls (p= .02). No difference in PA was detected between the study groups at the end of the study period after two years of intervention. | |
| Magnusson et al., 2012 |
BMI, skinfolds, waist circumference, percentage lean mass, percentage fat mass |
Relationship between the change in cardiorespiratory fitness over time and the change in body fat. |
Anthropometric measurements, dual energy x-ray scan (DEXA), ergometer bike |
None of the effect sizes of body composition were statistically significant. Children in the intervention group increased their fitness by an average of 0.37 z score units more than the controls (p= 0.18). Boys had higher fitness (p= 0.001) than girls, independent of study group, fitness z score at baseline andBMI. Post hoc analysis showed that the intervention school with the highest fitness z score change was significantly different from two of the lowest control schools (respectively, p< 0.0001 and p= 0.01), but it was also significantly different from the lowest intervention school (p= 0.05). | |
| Sacchetti et al., 2013 |
SAMBA project (Sorveglianza dell'AttivitÀ Motoria nei Bambini) |
Physical abilities |
Physical fitness, BMI |
Sport participation and daily activity habits were assessed by a self-administered questionnaire (PAQ-C). Anthropometric measurements. Physical performance was assessed by means of standardized tests (Sit & Reach test: flexibility; 2 kg medicine-ball forward throw test: upper limbs explosive strength; standing long jump test: lower body and legs explosive strength; 20m running speed test: speed and anaerobic power; forward roll test: self-perception in space and dynamic total body coordination). | The enhanced program of physical education was effective in improving physical abilities of children and determining a decrease (boys: 10%; girls: 12%) in daily sedentary activities (preintervention versus postintervention, p < .05; intervention versus control group, p < .01). The percentages of overweight and obese children did not vary significantly, but the experimental group showed a significantly lower rise in BMI compared to the control group (p < .001). |
| AraÚjo-Soares et al., 2009 |
Moderate to vigorous Physical Activity |
Social Cognitive Theory (SCT), Self-regulation Theory (SRT) and planning variables |
Questionnaires (International Physical Activity Questionnaire, Questionnaires on SCT and SRT) |
At post-test, participants in the intervention group 18 min more PA, adjusted for pre-intervention, age and sex, than those in the control group (p = 0.249). This difference increased to 33 min (p = 0.082) at three months and to 57 min (p = 0.008) at nine-month follow-up. Moreover, the intervention resulted in changes of some of the theoretical target variables, including outcome expectancies and coping planning. However, no evidence was found for the changes in theoretical moderators to mediate the intervention effects on behaviour. | |
| Angelopoulos et al., 2009 |
The CHILDREN study |
BMI, blood pressure |
Moderate to vigorous PA, diet |
Anthropometric measurements, blood pressure measures, questionnaire |
The intervention group increases leisure timpe moderate to vigorous PA, while controls decrease it (p=0.04). IG had higher consumption of fruits (p=0.04) and lower consumption of fats/oils (p=0.02) and sweets/beverages (0.03) compared with the CG. Intervention's effect on BMI (p=0.04) could be explained by the changes in fruit and fats/oils intake whereas the reduction of systolic and diastolic BP (p= 0.016 and p= 0.05) could be explained by the reduction of BMI. |
| Marcus et al., 2009 |
STOPP (School and after school care-based Obesity Prevention Programme) |
BMI, Physical Activity |
Healthy eating habits |
Accelerometer, anthropometric measurements, questionnaire (ChEAT (Children’s Eating Attitude Test). |
The prevalence of overweight and obesity decreased by 3.2% in intervention schools compared with an increase of 2.8% in control schools (p<0.05). The results showed no difference between intervention and controls, after cluster adjustment, in the longitudinal analysis of BMIsds changes. However, a larger proportion of the children who were initially overweight reached normal weight in the intervention group compared with the control group (p=0.017). PA did not differ between intervention and control schools after cluster adjustment. Eating habits at home were found to be healthier among families with children in intervention schools at the end of the intervention. There was no difference between children in intervention and control schools in self-reported eating disorders. |
BMD= Bone Mineral Density; BMI= Body Mass Index; BP= Blood pressure; CG or CON= Control group; EG= Experimental group; IG= Intervention group; MVPA=Moderate to Vigorous Physical Activity; PA= Physical Activity; QoL= Quality of Life; TST= triceps skinfold thickness; VO2 max= maximum volume of oxygen; VPA= Vigorous Physical Activity.
OVERVIEW OF THE MAIN FINDINGS
The great number of studies identified by this search testifies to researchers’ interest in this field.
However, the findings of school-based physical activity interventions are not always positive, resulting in an inconclusive picture. Some differences were identified between interventions that promoted or encouraged physical activity, and those that were effectively based on physical activity.
Multicomponent intervention focused on healthy lifestyle promotion, with a PA component of awareness, knowledge, recommendation, or stimulation, showed mixed results. The Program Si!, performed on preschoolers, showed an increase of children’s knowledge, attitudes and habits on diet, PA and human body, but no improvement in emotions [7]. The EdAl Study found a gender-specific decrease in obesity prevalence and BMI z-score in boys, while in girls there were no changes; moreover, BMI was not statistically different in the intervention group compared with controls. However, PA change showed a positive trend in favor of the intervention group [6]. The FATaintPHAT had no effect on BMI, waist circumference, and sedentary behaviors, and a negative effect on PA, sports participation [12]. The PRALIMAP showed positive effect on BMI and BMI z-scores only for the screening plus care intervention, and no effect of the other intervention strategies (education and environment strategies) [13]. The POP Study showed no significant effect on BMI z-score for the total sample, neither for eating behaviors, PA nor sedentary habits [17]. The intervention carried out by Haerens and colleagues found a significant increase of PA of moderate to vigorous intensity in the intervention group with parental support, and a decrease of fat intake and percent energy from fat [26,27]. The CHILDREN Study found an increase in leisure time moderate to vigorous PA, a reduction both in BMI and in blood pressure, and healthy diet changes in the intervention group [20]. The DOiT intervention failed to reduce BMI and to increase aerobic fitness, but showed a significant decrease in hip circumference and sum of skinfold thickness among girls, and in waist circumference among boys, with similar findings after 20 months [22, 23]. Finally, the APPLES study showed no results on BMI, eating behaviors and psychological outcomes, and even negative findings among obese children in the intervention group, which reduced fruit consumption, and increased sedentary behaviors and high sugar food consumption [31, 32].
Trials focused on multicomponent healthy lifestyle intervention including an actual PA component also showed different results. The JuvenTUM project reached a reduction in waist circumference in the intervention group, more pronounced in overweight/obese children, but failed to show increased PA and physical fitness [11]. The URMEL-ICE intervention showed a non-significant positive trend in decreasing waist circumference and subscapular skinfold thickness, and no effect on BMI [16]. The trial carried out by Araújo-Soares and colleagues found an increase in PA in intervention group that further increased at 3 and 9 months follow-up [21].
The HEIA study increased the overall PA levels in the intervention group, more positively among normal-weight participants, with a more pronounced effect among girls and low-activity intervention group; among girls, the intervention also reduced time spent in sedentary activities. Perceived support from teachers mediated the intervention effect on girls and normal-weight children. Weight status appeared to moderate the effect on enjoyment for PA, with reduced enjoyment among overweight participants [8-10]. The AVall trial reached, at the end of the 2 years of intervention, a lower increase of the BMI, and a lower prevalence of overweight/obese children in intervention group [14, 15]. The Ballabeina study, performed on predominantly migrant preschoolers, showed more positive effects on waist circumference reduction on overweight children and on all adiposity outcomes on low-fit children. The whole intervention group showed an increase in aerobic fitness, in motor agility, in body fat percentage and waist circumference, but no effect on BMI [18, 19]. The STOPP trial failed to show neither a significant effect in reducing overweight/obesity prevalence among children in intervention group, nor in increasing PA levels; however, it was efficacious in reducing weight among those who were initially overweight, and producing healthier eating habits in children in intervention schools [24]. The CHILT project showed no effect in reducing the incidence and prevalence of overweigh/obese children; some motor abilities and physical performance improved in intervention group (such as 6-minutes run and lateral jumping), with overweight children performing poorer performances [28-30].
Trials focused on solely PA school-based intervention aimed to enhance moderate to vigorous PA also showed mixed results on both PA levels and metabolic parameters, only partially affected by interventions.
The SAMBA project improved physical abilities of children and decreased sedentary activities; the intervention group also showed a significantly lower rise in BMI compared to the control group [33].
The EDUFIT trial did not positively affect cardio-metabolic parameters except for LDLc, and only in the intervention group that exercised at high intensity; nevertheless, there were improvements in aerobic fitness and flexibility for both intervention intensity levels, and in speed-agility for the high intensity intervention group. Interestingly, participants who complete the program showed a trend of better cognitive and academic performance, and worse levels of adiposity, diastolic tension, handgrip strength and maximal expiratory pressure [34-36].
PA intensity at moderate to vigorous levels after one year of intervention carried out by Magnusson and colleagues was higher in the intervention schools, with a significantly greater increase among the boys, but no difference in PA was detected between intervention and control groups after two years of intervention [40, 41].
The KISS trial failed to show a positive effect on body composition parameters, except for a decrease in z-score of the sum of four skinfolds [44]. Neither physical nor psychological Quality of Life was affected by KISS intervention; moreover, the intervention was not effective in managing Fear of Negative Evaluation, that even increased in overweight children [45,46].
Walther and colleagues showed a significant effect of their intervention on oxygen maximal consumption and increased circulating progenitor cells evaluated by flow cytometry, but neither an effect was found on BMI z-score, nor on high-density lipoprotein cholesterol; likewise, the intervention was not able to affect motor and coordinative performances [51].
Interventions based on moderate, recreational PA did not change BMI status, whereas these studies showed some interesting findings related to other PA outcomes. The ICAPS trial, carried out over 4 years, showed a lower increase in BMI in intervention group, though this effect did not persist in initially overweight adolescents over time. Nevertheless, independently from initial weight status, participants in the intervention group had an increase in supervised physical activity, a decrease in screen viewing and an increase in high-density cholesterol concentrations compared with controls [37].
Similarly, the intervention carried out by Thivel and colleagues did not affect BMI and body fat; nevertheless, it improved aerobic and anaerobic physical fitness in both lean and overweight children [52].
The MOVI program, an after school intervention, did not show an effect on BMI, total cholesterol, triglycerides or blood pressure in either sex, except for an increase in diastolic blood pressure, although boys and girls in the intervention group showed a decrease in triceps skinfold thickness and a positive pattern of blood lipids; moreover, intervention girls showed also a decrease in the percentage of body fat [38]. The MOVI program was also assessed by using a cost-effectiveness analysis, resulting in 269.83 €/year/child versus 844,56 €/year/child of the usual after-school care programs [39].
Two interventions based on feedback (pedometers), without a direct PA intervention, showed similar results, even if differing for duration. In Fit’n’Dude, carried out over 14 weeks, no effect was found on BMI and waist circumference, but it was noted that the largest increase in PA was seen in the “full intervention” school (pedometer and rewards) group, compared with a smaller effect in the no-rewards school and no effect in the control group. Nevertheless, after the end of the taper phase, while physical activity in the no-rewards school continued to increase, it had returned to baseline in the full intervention school [47]. The intervention carried out by Butcher and colleagues, carried out over 5 days, showed a significant increase of daily PA in the intervention group that wore pedometers and had feedback information provided by the researchers compared to control group children who only wore pedometer [49].
The iPlay intervention, focused on physical injuries prevention during PA, showed a higher effect in reducing sport injuries in a low activity group, with a 50% reduction of total injuries; moreover, the number of severe injuries in the intervention group was smaller than that in the controls [48].
The intervention carried out by Chatzisarantis & Hagger, based on Self-determination Theory, showed that teacher’s autonomy supportive educational style determined an increase in students’ leisure-time PA and stronger intention to exercise during leisure time; such effect was mediated by autonomous motivation and intention [50].
DISCUSSION
Among the European school-based Physical Activity interventions retrieved by our search, a small number seemed to reach positive results in terms of decrease in BMI, the universally recognized parameter to define weight status. These programs were quite different from each other [13,15, 16,20,33]. Thus, we were not able to understand if those positive findings were related to PA features (such as exercise intensity and duration, i.e. PA dose), rather than sample’s characteristics (such as sample size, age, sex, economic status), intrinsic characteristics of the interventions (theoretical framework, enjoyment in PA design, methods), or environmental characteristics (school participation, teachers’ motivation, simplicity of PA implementation). Analogous results regarding no effect or, at the best, a small effect of school-based physical activity programs on reducing BMI have been shown by several meta-analysis [53-55].
Nevertheless, more interesting findings emerged regarding other metabolic parameters, like waist circumference, skinfold thickness, body fat. Several trials achieved positive results, in particular among those focused on multicomponent interventions with an actual PA component, such as the JuvenTUM [11], the Ballabeina [18, 19], the STOPP [24] and the KISS trials [44], as well as the DOiT [22, 23] and The MOVI program [38]. It could be hypothesized that BMI should not be considered a gold standard to assessed changes in body composition during developmental age, or, alternatively, that it could be necessary for higher doses and longer duration of the interventions to achieve a BMI reduction.
Moreover, school-based PA interventions frequently aimed to increase PA, physical fitness, motor agilities, and/or to decrease sedentary habits. Positive results in these fields were attained by a larger proportion of the selected trials, such as the EdAl [6], the CHILDREN [20], the HEIA [8], the Ballabeina [18 and 19], the SAMBA [33], the EDUFIT [35], the ICAPS [39], the Fit’n’Dude [47], and in those performed by Hearens et al. [26, 27], Araujo-Soares et al. [21], Walther et al. [51], Thivel et al. [52], Butcher et al. [49], and Chatzisarantis & Hagger [50]. Such positive results could be partially explained because in some cases a self-reported assessment of PA was used [20, 21, 37, 50]. A recent meta-analysis showed a small effect size of physical activity interventions on children’s PA when objectively measured (with accelerometers), and this finding has been hypothesized to explain the limited effect of these programs in reducing BMI [56]. As overweight and obesity generally coupled both unhealthy eating habits and sedentary attitudes, such findings of our review seem to address the efforts of the school policy in promoting PA interventions.
Surprisingly, few interventions take into account psychological and cognitive outcomes. Because schools are the place where youths live about one third of their lives, in which they study, learn, build friendship, have social relations, it seems somehow natural that physical activity interventions should include such components. Furthermore, evidence from studies carried out on both children and adults showed effects of exercise beyond improvements in physical fitness and body composition, like mental wellbeing, psychosocial outcomes, behavior, and academic achievement in children [57], and enhancement of auditory and visual attention, and processing speed in older adults without known cognitive impairment [58]. Further school-based physical activity interventions should be focused on these topics.
In European Countries, obesity and overweight affected children and adolescents, with up to 27 percent of 13-year-olds and 33 percent of 11-year-olds in some European countries that are overweight or obese, according to the WHO’s latest report [59]; Greece, Portugal, Ireland, Spain and UK have the highest proportion of overweight 11-year-olds (28 to 33 percent). From 2002 to 2010 the number of European Countries with more than 20 percent of overweight 11-, 13- and 15-year-olds rose from 5 to 11 Countries [5]. Moreover, in 23 out of 36 European Countries, 30 percent of teenagers do not get enough exercise [59].
It is urgently needed a strong response from the policy makers to stop such an epidemic, and schools have the potentiality to play a central role.
CONCLUSION
Physical inactivity, as well as the unhealthy foods, high in fat, sugar and salt, and sweet soft drinks, have caused a rise in children’s and adolescents’ overweight and obesity in the recent decades, and European Countries are markedly affected from this problem. Schools are the ideal places to modify unhealthy habits, particularly those related to sedentary lifestyle. Physical education could be regarded as a potential setting to enhance physical activity, and to promote healthy behaviors.
A number of physical activity programs have been conducted throughout Europe in the past years. The results of these interventions should addressed policy decisions in terms of prevention of obesity in developmental age.
Physical activity interventions need to directly incorporate PA behaviors, implementing the compulsory hours of physical education; moreover, intervention have to result simple, enjoyable and ecological (i.e. it must be performed in a natural setting, with teachers, as well as parents, involved in the intervention), rather to solely increase PA. Healthy information (on nutrition and active behavior) could be added to physical activity, and a multicomponent intervention should be addressed to all pupils, to avoid the stigmatization of those subjects that more need help, like low fit and overweight students.
ACKNOWLEDGEMENTS
Declared none.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.World Health Organization6 Global recommendations on physical activity for health. Available on http: //whqlibdoc.who.int/ publica-tions/2010/9789241599979_eng.pdf [Google Scholar]
- 2.Eime RM, Young JA, Harvey JT, Charity MJ, Payne WR. A systematic review of the psychological and social benefits of participation in sport for children and adolescents informing development of a conceptual model of health through sport. Int J Behav Nutr Phys Act. 2013;10:98. doi: 10.1186/1479-5868-10-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sancassiani F, Pintus E, Holte A , et al. Enhancing youths’ emotional and social skills to promote their wellbeing and positive development a systematic review of universal school-based randomized controlled trials. Clin Pract Epidemiol Mental Health. 2015;11:21–40. doi: 10.2174/1745017901511010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cossu G, Cantone E, Pintus M , et al. Integrating children with psychiatric problems in the classroom. A systematic review. Clin Pract Epidemiol Mental Health. 2015;11:41–57. doi: 10.2174/1745017901511010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO Global Status Report on Non-Communicable Diseases. http: //www.who.int/nmh/publications/ncd_report2010/en/ 2010.
- 6.Tarro L, Llauradó E, Albaladejo R , et al. A primary-school-based study to reduce the prevalence of childhood obesity--the EdAl (Educació en Alimentació) study a randomized controlled trial. Trials. 2014;15:58. doi: 10.1186/1745-6215-15-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peñalvo JL, Sotos-Prieto M, Santos-Beneit G, Pocock S, Redondo J, Fuster V. The Program SI! intervention for enhancing a healthy lifestyle in preschoolers first results from a cluster randomized trial. BMC Public Health. 2013;13:1208. doi: 10.1186/1471-2458-13-1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grydeland M, Bergh IH, Bjelland M , et al. Intervention effects on physical activity the HEIA study - a cluster randomized controlled trial. Int J Behav Nutr Phys Act. 2013;10:17. doi: 10.1186/1479-5868-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bergh IH, Bjelland M, Grydeland M , et al. Mid-way and post-intervention effects on potential determinants of physical activity and sedentary behavior, results of the HEIA study - a multi-component school-based randomized trial. Int J Behav Nutr Phys Act. 2012;9:63. doi: 10.1186/1479-5868-9-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bergh IH, van Stralen MM, Grydeland M , et al. Exploring mediators of accelerometer assessed physical activity in young adolescents in the Health In Adolescents Study - a group randomized controlled trial. BMC Public Health. 2012;12:814. doi: 10.1186/1471-2458-12-814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siegrist M, Lammel C, Haller B, Christle J, Halle M. Effects of a physical education program on physical activity, fitness, and health in children the JuvenTUM project. Scand J Med Sci Sports. 2013;23(3):323–30. doi: 10.1111/j.1600-0838.2011.01387.x. [DOI] [PubMed] [Google Scholar]
- 12.Ezendam NP, Brug J, Oenema A. Evaluation of the Web-based computer-tailored FATaintPHAT intervention to promote energy balance among adolescents results from a school cluster randomized trial. Arch Pediatr Adolesc Med. 2012;166(3):248–55. doi: 10.1001/archpediatrics.2011.204. [DOI] [PubMed] [Google Scholar]
- 13.Bonsergent E, Agrinier N, Thilly N , et al. Overweight and obesity prevention for adolescents a cluster randomized controlled trial in a school setting. Am J Prev Med. 2013;44(1):30–9. doi: 10.1016/j.amepre.2012.09.055. [DOI] [PubMed] [Google Scholar]
- 14.Llargues E, Franco R, Recasens A , et al. Assessment of a school-based intervention in eating habits and physical activity in school children the AVall study. J Epidemiol Community Health. 2011;65(10):896–901. doi: 10.1136/jech.2009.102319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Llargués E, Recasens A, Franco R , et al. Medium-term evaluation of an educational intervention on dietary and physical exercise habits in schoolchildren the Avall 2 study. Endocrinol Nutr. 2012;59(5):288–95. doi: 10.1016/j.endonu.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Brandstetter S, Klenk J, Berg S , et al. Overweight prevention implemented by primary school teachers a randomised controlled trial. Obes Facts. 2012;5(1):1–11. doi: 10.1159/000336255. [DOI] [PubMed] [Google Scholar]
- 17.De Coen V, De Bourdeaudhuij I, Vereecken C , et al. Effects of a 2-year healthy eating and physical activity intervention for 3-6-year-olds in communities of high and low socio-economic status the POP (Prevention of Overweight among Pre-school and school children) project. Public Health Nutr. 2012;15(9):1737–45. doi: 10.1017/S1368980012000687. [DOI] [PubMed] [Google Scholar]
- 18.Niederer I, Bürgi F, Ebenegger V , et al. Effects of a lifestyle intervention on adiposity and fitness in overweight or low fit preschoolers (Ballabeina). Obesity (Silver Spring). 2013;21(3):E287–93. doi: 10.1002/oby.20119. [DOI] [PubMed] [Google Scholar]
- 19.Puder JJ, Marques-Vidal P, Schindler C , et al. Effect of multidimensional lifestyle intervention on fitness and adiposity in predominantly migrant preschool children (Ballabeina): cluster randomised controlled trial. BMJ. 2011;343:d6195. doi: 10.1136/bmj.d6195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Angelopoulos PD, Milionis HJ, Grammatikaki E, Moschonis G, Manios Y. Changes in BMI and blood pressure after a school based intervention the CHILDREN study. Eur J Public Health. 2009;19(3):319–25. doi: 10.1093/eurpub/ckp004. [DOI] [PubMed] [Google Scholar]
- 21.Araújo-Soares V, McIntyre T, MacLennan G, Sniehotta FF. Development and exploratory cluster-randomised opportunistic trial of a theory-based intervention to enhance physical activity among adolescents. Psychol Health. 2009;24(7):805–22. doi: 10.1080/08870440802040707. [DOI] [PubMed] [Google Scholar]
- 22.Singh AS, Chin A Paw MJ, Brug J, van Mechelen W. Short-term effects of school-based weight gain prevention among adolescents. Arch Pediatr Adolesc Med. 2007;161(6):565–71. doi: 10.1001/archpedi.161.6.565. [DOI] [PubMed] [Google Scholar]
- 23.Singh AS, Chin A Paw MJ, Brug J, van Mechelen W. Dutch obesity intervention in teenagers effectiveness of a school-based program on body composition and behavior. Arch Pediatr Adolesc Med. 2009;163(4):309–17. doi: 10.1001/archpediatrics.2009.2. [DOI] [PubMed] [Google Scholar]
- 24.Marcus C, Nyberg G, Nordenfelt A, Karpmyr M, Kowalski J, Ekelund U. A 4-year, cluster-randomized, controlled childhood obesity prevention study STOPP. Int J Obes. 2009;33(4):408–17. doi: 10.1038/ijo.2009.38. [DOI] [PubMed] [Google Scholar]
- 25.Kipping RR, Payne C, Lawlor DA. Randomised controlled trial adapting US school obesity prevention to England. Arch Dis Child. 2008;93(6):469–73. doi: 10.1136/adc.2007.116970. [DOI] [PubMed] [Google Scholar]
- 26.Haerens L, Deforche B, Maes L, Cardon G, Stevens V, De Bourdeaudhuij I. Evaluation of a 2-year physical activity and healthy eating intervention in middle school children. Health Educ Res. 2006;21(6):911–21. doi: 10.1093/her/cyl115. [DOI] [PubMed] [Google Scholar]
- 27.Haerens L, De Bourdeaudhuij I, Maes L, Cardon G, Deforche B. School-based randomized controlled trial of a physical activity intervention among adolescents. J Adolesc Health. 2007;40(3):258–65. doi: 10.1016/j.jadohealth.2006.09.028. [DOI] [PubMed] [Google Scholar]
- 28.Graf C, Koch B, Kretschmann-Kandel E , et al. Correlation between BMI, leisure habits and motor abilities in childhood (CHILT-project). Int J Obes Relat Metab Disord. 2004;28(1):22–6. doi: 10.1038/sj.ijo.0802428. [DOI] [PubMed] [Google Scholar]
- 29.Graf C, Koch B, Falkowski G , et al. Effects of a school-based intervention on BMI and motor abilities in childhood. J Sports Sci Med. 2005;4(3):291–9. [PMC free article] [PubMed] [Google Scholar]
- 30.Graf C, Koch B, Falkowski G , et al. School-based prevention effects on obesity and physical performance after 4 years. J Sports Sci. 2008;26(10):987–94. doi: 10.1080/02640410801930176. [DOI] [PubMed] [Google Scholar]
- 31.Sahota P, Rudolf MC, Dixey R, Hill AJ, Barth JH, Cade J. Randomised controlled trial of primary school based intervention to reduce risk factors for obesity. BMJ. 2001;323(7320):1029–32. doi: 10.1136/bmj.323.7320.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sahota P, Rudolf MC, Dixey R, Hill AJ, Barth JH, Cade J. Evaluation of implementation and effect of primary school based intervention to reduce risk factors for obesity. BMJ. 2001;323(7320):1027–9. doi: 10.1136/bmj.323.7320.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sacchetti R, Ceciliani A, Garulli A, Dallolio L, Beltrami P, Leoni E. Effects of a 2-year school-based intervention of enhanced physical education in the primary school. J Sch Health. 2013;83(9):639–46. doi: 10.1111/josh.12076. [DOI] [PubMed] [Google Scholar]
- 34.Ardoy DN, Fernández-Rodríguez JM, Chillón P , et al. Physical fitness enhancement through education, EDUFIT study background, design, methodology and dropout analysis. Rev Esp Salud Publica. 2010;84(2):151–68. doi: 10.1590/s1135-57272010000200004. [DOI] [PubMed] [Google Scholar]
- 35.Ardoy DN, Fernández-Rodríguez JM, Ruiz Jr , et al. Improving physical fitness in adolescents through a school-based intervention the EDUFIT study. Rev Esp Cardiol. 2011;64(6):484–91. doi: 10.1016/j.recesp.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 36.Ardoy DN, Artero EG, Ruiz Jr , et al. Effects on adolescents' lipid profile of a fitness-enhancing intervention in the school setting; the EDUFIT study. Nutr Hosp. 2013;28(1):119–26. doi: 10.3305/nh.2013.28.1.6146. [DOI] [PubMed] [Google Scholar]
- 37.Simon C, Schweitzer B, Oujaa M , et al. Successful overweight prevention in adolescents by increasing physical activity a 4-year randomized controlled intervention. Int J Obes (Lond). 2008;32(10):1489–98. doi: 10.1038/ijo.2008.99. [DOI] [PubMed] [Google Scholar]
- 38.Martínez VV, Salcedo AF, Franquelo GR , et al. Assessment of an after-school physical activity program to prevent obesity among 9- to 10-year-old children a cluster randomized trial. Int J Obes (Lond). 2008;32(1):12–22. doi: 10.1038/sj.ijo.0803738. [DOI] [PubMed] [Google Scholar]
- 39.Moya MP, Sánchez LM, López BJ , et al. Cost-effectiveness of an intervention to reduce overweight and obesity in 9-10-year-olds. The Cuenca study. Gac Sanit. 2011;25(3):198–204. doi: 10.1016/j.gaceta.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 40.Magnusson KT, Sigurgeirsson I, Sveinsson T, Johannsson E. Assessment of a two-year school-based physical activity intervention among 7-9-year-old children. Int J Behav Nutr Phys Act. 2011;20, 8:138. doi: 10.1186/1479-5868-8-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Magnusson KT, Hrafnkelsson H, Sigurgeirsson I, Johannsson E, Sveinsson T. Limited effects of a 2-year school-based physical activity intervention on body composition and cardiorespiratory fitness in 7-year-old children. Health Educ Res. 2012;27(3):484–94. doi: 10.1093/her/cys049. [DOI] [PubMed] [Google Scholar]
- 42.Meyer U, Romann M, Zahner L , et al. Effect of a general school-based physical activity intervention on bone mineral content and density a cluster-randomized controlled trial. Bone. 2011;48(4):792–7. doi: 10.1016/j.bone.2010.11.018. [DOI] [PubMed] [Google Scholar]
- 43.Meyer U, Ernst D, Zahner L , et al. 3-Year follow-up results of bone mineral content and density after a school-based physical activity randomized intervention trial. Bone. 2013;55(1):16–22. doi: 10.1016/j.bone.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 44.Kriemler S, Zahner L, Schindler C , et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren cluster randomised controlled trial. BMJ. 2010;340:c785. doi: 10.1136/bmj.c785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hartmann T, Zahner L, Pühse U, Puder JJ, Kriemler S. Effects of a school-based physical activity program on physical and psychosocial quality of life in elementary school children a cluster-randomized trial. Pediatr Exerc Sci. 2010;22(4):511–22. doi: 10.1123/pes.22.4.511. [DOI] [PubMed] [Google Scholar]
- 46.Hartmann T, Zahner L, Pühse U, Schneider S, Puder JJ, Kriemler S. Physical activity, bodyweight, health and fear of negative evaluation in primary school children. Scand J Med Sci Sports. 2010;20(1):e27–34. doi: 10.1111/j.1600-0838.2009.00888.x. [DOI] [PubMed] [Google Scholar]
- 47.Hardman CA, Horne PJ, Fergus Lowe C. Effects of rewards, peer-modelling and pedometer targets on children's physical activity a school-based intervention study. Psychol Health. 2011;26(1):3–21. doi: 10.1080/08870440903318119. [DOI] [PubMed] [Google Scholar]
- 48.Collard DC, Verhagen EA, Chinapaw MJ, Knol DL, van Mechelen W. Effectiveness of a school-based physical activity injury prevention program a cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2010;164(2):145–50. doi: 10.1001/archpediatrics.2009.256. [DOI] [PubMed] [Google Scholar]
- 49.Butcher Z, Fairclough S, Stratton G, Richardson D. The effect of feedback and information on children's pedometer step counts at school. Pediatr Exerc Sci. 2007;19(1):29–38. doi: 10.1123/pes.19.1.29. [DOI] [PubMed] [Google Scholar]
- 50.Chatzisarantis NL, Hagger MS. Effects of an intervention based on self-determination theory on self-reported leisure-time physical activity participation. Psychol Health. 2009;24(1):29–48. doi: 10.1080/08870440701809533. [DOI] [PubMed] [Google Scholar]
- 51.Walther C, Gaede L, Adams V , et al. Effect of increased exercise in school children on physical fitness and endothelial progenitor cells a prospective randomized trial. Circulation. 2009;120(22):2251–9. doi: 10.1161/CIRCULATIONAHA.109.865808. [DOI] [PubMed] [Google Scholar]
- 52.Thivel D, Isacco L, Lazaar N , et al. Effect of a 6-month school-based physical activity program on body composition and physical fitness in lean and obese schoolchildren. Eur J Pediatr. 2011;170(11):1435–43. doi: 10.1007/s00431-011-1466-x. [DOI] [PubMed] [Google Scholar]
- 53.Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev. 2013;2:CD007651. doi: 10.1002/14651858.CD007651.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lavelle HV, Mckay DF, Pell JP. Systematic review and meta-analysis of school-based interventions to reduce body mass index. J Public Health (Oxf). 2012;34(3):360–9. doi: 10.1093/pubmed/fdr116. [DOI] [PubMed] [Google Scholar]
- 55.Dobbins M, De Corby K, Robeson P, Husson H, Tirilis D. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6-18. Cochrane Database Syst Rev. 2009;(1):CD007651. doi: 10.1002/14651858.CD007651. [DOI] [PubMed] [Google Scholar]
- 56.Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54). BMJ. 2012;345:e5888. doi: 10.1136/bmj.e5888. [DOI] [PubMed] [Google Scholar]
- 57.Lees C, Hopkins J. Effect of aerobic exercise on cognition, academic achievement, and psychosocial function in children a systematic review of randomized control trials. Prev Chronic Dis. 2013;10:E174. doi: 10.5888/pcd10.130010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Angevaren M, Aufdemkampe G, Verhaar HJ, Aleman A, Vanhees L. Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev. 2008;(2):CD005381. doi: 10.1002/14651858.CD005381.pub2. [DOI] [PubMed] [Google Scholar]
- 59.OECD Health at a Glance Europe 2012. http: //ec.europa.eu/ health/reports/european/health_glance_2012_en.htm. 2012.


