A 54-year-old man with end-stage heart failure due to hypertrophic cardiomyopathy was admitted because of acute hemodynamic deterioration accompanied by disabling dyspnea and asthenia at rest, in association with fluid overload, poor urinary output, and a contextual increase of neurohormonal activation (brain natriuretic peptide level, 4,168 pg/mL). He was already enrolled for heart transplantation at our center.
Despite continuing inotropic support (with milrinone) and high-dose diuretics, the patient developed evidence of kidney and liver dysfunction and deteriorated to Class II Interagency Registry for Mechanically Assisted Circulatory Support (Intermacs). The heart team considered him a possible candidate for left ventricular assist device (LVAD) implantation as a bridge to transplantation. Preimplantation echocardiographic evaluation revealed severely impaired left ventricular (LV) systolic function with only mild LV dilation (Fig. 1). Right ventricular (RV) evaluation revealed a fractional area change (34%) below the range of normal value (Fig. 2), low tricuspid annular plane systolic excursion (12 mm) (Fig. 3), and a tissue-Doppler peak systolic velocity (8 cm/s) of the tricuspid annulus, again below the range of normal (Fig. 4).
Fig. 1.
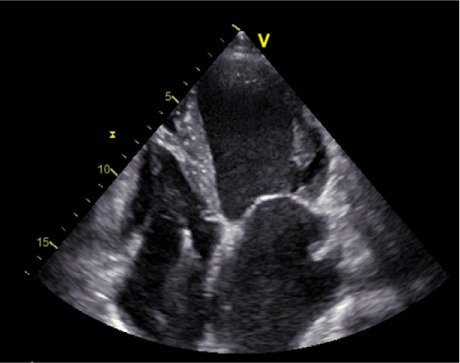
Transthoracic echocardiogram (apical 4-chamber view) shows a mildly dilated left ventricle with markedly reduced systolic function and preserved left ventricular wall thickness. Note also the severe left atrial enlargement.
Real-time motion image is available for Figure 1 (2MB, mp4) .
Fig. 2.
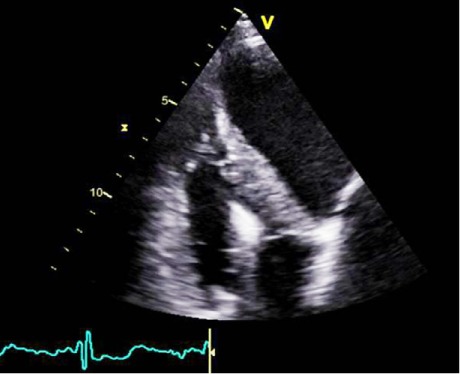
Transthoracic echocardiogram (apical off-axis view), focused on the right ventricle. Note the visually preserved free wall longitudinal function, with reduced fractional area change.
Real-time motion image is available for Figure 2 (2.1MB, mp4) .
Fig. 3.
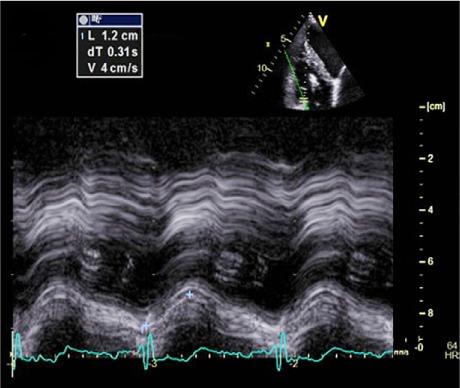
M-mode transthoracic echocardiogram, at the level of the lateral tricuspid annulus, revealed low (12 mm) tricuspid annular plane systolic excursion and low longitudinal right ventricular function.
Fig. 4.
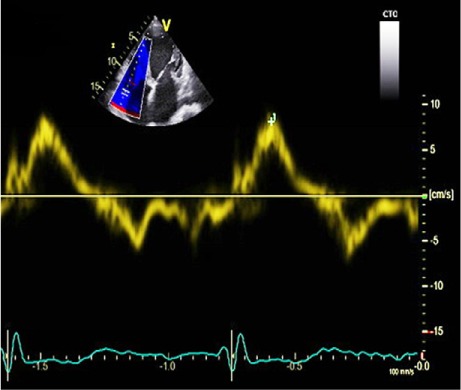
Tissue-Doppler image at the level of the lateral tricuspid annulus reveals a peak systolic velocity of 8 cm/s, indicating relatively low right ventricular longitudinal function.
In contrast, the value for RV free-wall longitudinal strain obtained with use of 2-dimensional speckle-tracking echocardiography and EchoPAC PC software (GE Medical Systems; Horten, Norway) was high (−16%), predicting good RV performance after implantation. The 2-dimensional speckle-tracking echocardiograms (Fig. 5) were obtained through offline analysis of grayscale conventional transthoracic images acquired during breath-hold and with a stable electrocardiogram recording. For each figure, 3 consecutive heart cycles were recorded and averaged. The frame rate was set between 60 and 80 frames.
Fig. 5.
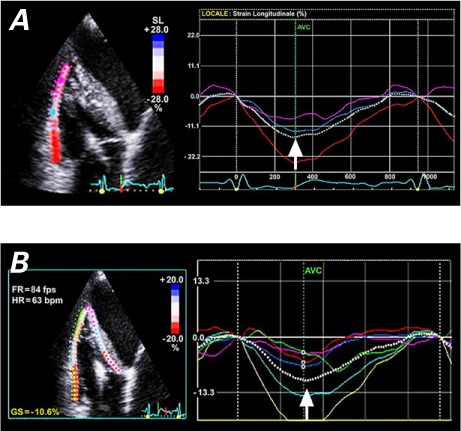
Two-dimensional speckle-tracking echocardiography (transthoracic apical off-axis view) was used to measure A) right ventricular free wall longitudinal strain (RVFWLS) and B) right ventricular global longitudinal strain (RVGLS). In A), the manual tracing of the RV free wall endocardial border (left) delineates a region of interest including the basal, mid, and apical segments. The RVFWLS curve (right, dashed white line) shows excellent global longitudinal performance, with a peak value of −16% (arrow). The highest values are seen in the basal segment (red line), intermediate values in mid-wall segment (blue line), and lower values in the apical segment (violet line). Longitudinal function progressively decreases from the basal to the apical segment of RV free wall. In B), the manual tracing of the RV endocardial border (left) delineates a region of interest including 6 segments: the basal, mid, and apical segments of the RV free wall, and the basal, mid, and apical segments of the ventricular septum. The average peak value of the RVGLS curve (right, dashed white line) is −11% (arrow). A gradient of longitudinal function decreasing from the RV free wall to the interventricular septum and from base to apex is evident.
The patient successfully underwent LVAD implantation during a short hospital stay.
Comment
Mechanical circulatory support is a relatively new successful option for patients with end-stage heart failure. According to the most recent Intermacs report,1 the one-year survival rates for patients with LVADs are approaching those for patients who have undergone heart transplantation, which has encouraged the technical improvement of devices and refined the accuracy of candidate selection. Right ventricular failure that requires biventricular assistance or inotropic support for longer than 2 weeks has been a major cause of postimplantation morbidity and death.2 For this reason, the accurate evaluation of RV performance—with the aid of new echocardiographic markers of prognosis—becomes necessary in selecting appropriate patients for LVAD implantation.3
Two-dimensional speckle-tracking echocardiography of the RV is a relatively new technique. Because its improved signal-to-noise ratio overcomes most Doppler limits, it is not influenced by angle-dependency and tethering effect.4 Together with the use of traditional echocardiographic results and clinical variables, this new technique greatly strengthens the prognostic marking of candidates for LVAD implantation.5,6
For example, RVFWLS can have an additional role in the decision-making for a subset of patients—such as those affected by end-stage hypertrophic cardiomyopathy—in whom the opportunity to implant a mechanical circulatory support device is even more challenging. Our case shows how comprehensive RV evaluation (including RVFWLS) can be used for correct prognostic stratification of candidates for LVAD implantation, when traditional echocardiographic results, considered alone, do not clearly indicate freedom from RV failure after LVAD implantation.
Supplementary Material
Footnotes
Section Editor: Raymond F. Stainback, MD, Department of Adult Cardiology, Texas Heart Institute, 6624 Fannin St., Suite 2480, Houston, TX 77030
From: Cardiology Unit (Drs. Carerj and Todaro), Department of Clinical and Experimental Medicine, University of Messina, 98125 Messina, Italy; Mediterranean Institute for Transplantation and High Specialization Therapies (Drs. Clemenza, Pilato, and Romano), 90133 Palermo, Italy; and Aurora Cardiovascular Services (Dr. Khandheria), Aurora Sinai/Aurora St. Luke's Medical Centers, University of Wisconsin School of Medicine and Public Health, Milwaukee, Wisconsin 53215
References
- 1.Kirklin JK, Naftel DC, Pagani FD, Kormos RL, Stevenson LW, Blume ED et al. Sixth INTERMACS annual report: a 10,000-patient database. J Heart Lung Transplant. 2014;33(6):555–64. doi: 10.1016/j.healun.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 2.John R, Lee S, Eckman P, Liao K. Right ventricular failure--a continuing problem in patients with left ventricular assist device support. J Cardiovasc Transl Res. 2010;3(6):604–11. doi: 10.1007/s12265-010-9216-4. [DOI] [PubMed] [Google Scholar]
- 3.Raina A, Seetha Rammohan HR, Gertz ZM, Rame JE, Woo YJ, Kirkpatrick JN. Postoperative right ventricular failure after left ventricular assist device placement is predicted by preoperative echocardiographic structural, hemodynamic, and functional parameters. J Card Fail. 2013;19(1):16–24. doi: 10.1016/j.cardfail.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23(7):685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Grant AD, Smedira NG, Starling RC, Marwick TH. Independent and incremental role of quantitative right ventricular evaluation for the prediction of right ventricular failure after left ventricular assist device implantation. J Am Coll Cardiol. 2012;60(6):521–8. doi: 10.1016/j.jacc.2012.02.073. [DOI] [PubMed] [Google Scholar]
- 6.Cameli M, Lisi M, Righini FM, Focardi M, Lunghetti S, Bernazzali S et al. Speckle tracking echocardiography as a new technique to evaluate right ventricular function in patients with left ventricular assist device therapy. J Heart Lung Transplant. 2013;32(4):424–30. doi: 10.1016/j.healun.2012.12.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


