Abstract
Background and Aims:
Various adjuvants have been used to prolong the duration of local anaesthetic action after peripheral and regional nerve blocks. We evaluated the effect of dexamethasone on the duration of pain relief in shoulder arthroscopic surgeries performed under interscalene brachial plexus using ropivacaine as local anaesthetic.
Methods:
After Ethical Committee approval and informed consent from patients we performed a prospective, randomised, comparative study on patients scheduled for arthroscopic shoulder surgery under interscalene block (ISB). Patients in ropivacaine group (Group R) received 30 ml of 0.5% ropivacaine plus 2 ml normal saline (n = 50) and dexamethasone-ropivacaine (Group RD) received 0.5% ropivacaine 30 ml plus 8 mg dexamethasone (4 mg/ml) (n = 50). Duration of analgesia, onset of sensory and motor block, success and failure of block, and complications were recorded and compared. Computer software SPSS version-16 (SPSS Inc., Chicago, Illinois, USA) was used for statistical analysis. Chi-square test and Student's t-test were used and P < 0.05 was considered as significant.
Results:
The mean duration of analgesia in Group RD was 1103.72 ± 296.027 min and in Group R it was 551.54 ± 166.92 min (P = 0.0001). Onset of sensory block in Group RD was 12.24 ± 1.88 min and in Group R was 13.48 ± 1.81 min (P = 0.5170). Onset of motor block in Group RD was 16.24 ± 2.04 min and in Group R was 17.76 ± 2.21 min (P = 0.2244). Onset of surgical anaesthesia in Group RD was19.46 ± 1.86 min and in Group R was 20.84 ± 1.71 min (P = 0.0859).
Conclusion:
Dexamethasone significantly prolonged duration of analgesia of ropivacaine during ISB used for arthroscopic surgeries of shoulder. Dexamethasone when mixed with ropivacaine had no effect on the onset of sensory and motor effects of ISB with ropivacaine.
Keywords: Brachial plexus block, dexamethasone, interscalene block, ropivacaine
INTRODUCTION
Interscalene block (ISB) provides excellent anaesthesia and analgesia for shoulder surgery.[1] However, post-operative analgesia is not sufficient to help in early mobilisation. Various additives such as epinephrine[2] and clonidine[3] have been studied to prolong the duration of peripheral nerve blocks however, these agents may have undesirable side effects. Dexamethasone prolongs the effect of peripheral nerve block when added to short-acting local anaesthetics.[4] We have recently started using ropivacaine for single shot ISB for shoulder, which provides excellent intraoperative anaesthesia, but duration of post-operative analgesia is limited. Various studies have shown that dexamethasone is a safe adjunct to ropivacaine;[4,5] therefore, we wanted to evaluate the additive effect of dexamethasone and ropivacaine used in ISB for shoulder surgeries.
The present study was conducted to compare 0.5% ropivacaine and mixture of 0.5% ropivacaine with dexamethasone in ISB used for shoulder arthroscopic surgeries. Primary outcome measure was to evaluate the effect of mixing dexamethasone on duration of analgesia provided by ISB. Secondary outcomes measures were onset time of sensory and motor block, pain scores by visual analogue scale score (VAS), analgesic consumption in 24 h and interscalene brachial block-related complications.
METHODS
This prospective randomised controlled trial was conducted after approval from Hospital Ethics Committee and after obtaining written informed consent from patients. Exclusion criteria were patient refusal, known hypersensitivity to test drugs or contraindications to ISB. Sample size was calculated assuming 20% increase in duration of analgesia after addition of dexamethasone; 50 patients per group were required with α =0.05, 80% power and 95% confidence limit. We required 50 patients in each group(100 total) and considering 10% drop outs (due to change in technique or cancellation on table), 112 patients of either sex between 18 and 70 years and American Society of Anaesthesiologists physical status I and II scheduled for shoulder arthroscopic surgery under ISB were enrolled in study. 112 patients were divided into two groups with 56 patients in each group using computer generated randomisation. One group was Group R (n = 56) where only ropivacaine was used, and another group was Group RD (n = 56) where dexamethasone was mixed with ropivacaine. Sealed opaque envelopes containing group allocation were opened before the blocks were performed.
Patients were pre-medicated with tablet alprazolam (0.5 mg) and tablet ranitidine (150 mg) per oral, night before surgery and on the day of surgery 2 h before operation. On arrival in operation theatre, intravenous (IV) cannulation was done and normal saline infusion was started at flow rate of 100 mL/h and oxygen was administered at the rate of 2–3 L/min via nasal prongs and multiparameter monitor was connected. Oxygen saturation (SpO2), heart rate (HR), non-invasive blood pressure (NIBP), and continuous electrocardiograph were monitored. Patients were sedated with IV midazolam (0.05 mg/kg) before block was administered. Standard nerve stimulation technique was used for ISB. Initial current was set at 2 mA and contraction (of deltoid muscle/shoulder) at a stimulating current of 0.5 mA (2 Hz, 0.1 ms duration) was considered as evidence of appropriate needle position. If the threshold current needed was higher, the needle was repositioned. Once the desired response was found, the needle was stabilised and drug solution was injected slowly in 5 mL increments with frequent aspiration to avoid intravascular injection. If the threshold current was 0.2 mA or less, if injection pressure was high, or if the patient had a paraesthesia during needle placement or injection, the needle was pulled back slightly because of concern of intraneural placement. In Group R (control group) ISB was performed with 30 mL of 0.5% ropivacaine plus 2 mL of normal saline and in Group RD (dexamethasone group) ISB was performed with 30 mL 0.5% ropivacaine plus 2 mL (4 mg/mL) dexamethasone. Medications were prepared earlier by one of the anaesthesiologists who was not involved in observation and were delivered in similar unidentifiable syringes. All ISB were performed by senior anaesthesiologists who had more than 10 years of experience in ISB. After incremental injection of the designated drug solution, patients were evaluated at 5 min intervals till 30 min for the development of sensory and motor block.
Sensory block was assessed by loss of sensation to pinprick over the deltoid muscle (C5, C6 dermatome) and evaluated using a three-point scale: 2 = normal sensation, 1 = loss of sensation to pinprick, and 0 = loss of sensation to light touch. Motor block was assessed by Modified Bromage Scale (4 = Full power in arm and shoulder muscles, 3 = Reduced power but ability to move arm and shoulder against resistance, 2 = Ability to move arm and shoulder against gravity but inability to move against resistance, 1 = Flicker of movement in arm and shoulder muscles, 0 = No movement in arm and shoulder muscles). The anaesthesiologist who assessed all study parameters was blinded to group allocation and drug used. Overall quality of block was assessed on a three-point scale: 0 = complete failure, 1 = inadequate block, 2 = successful block. At the end of 30 min if there were no signs of motor and sensory block, it was considered failed block and patients were excluded. However, if any patient had incomplete block or complained of discomfort/pain intraoperatively they were managed with supplemental analgesia with IV ketamine (1–1.5 mg/kg) and propofol (1–2 mg/kg) and block was considered as inadequate block.
Intraoperative vital parameters (HR/NIBP/rhythm/SpO2) were monitored every 5 min throughout the study. Each patient was observed for side effects like Horner's syndrome (HS), ipsilateral diaphragmatic paralysis, hoarseness of voice, difficulty in swallowing and complications like pneumothorax, vascular injury (external jugular vein puncture, haematoma formation, intra-arterial injection), epidural or spinal injection, neuropathy/nerve injury.
Pain evaluation was done using VAS (0–10) where 0 = no pain and 10 = unbearable pain. When VAS was >3 or when the patient demanded analgesia, intramuscular diclofenac (1 mg/kg) given. If VAS remained ≥3 or pain control remained unsatisfactory 45 min after diclofenac injection, injection tramadol 1 mg/kg IV was used. Number of total rescue injections (diclofenac + tramadol) given to each patient during first 24 h of the post-operative period, were recorded.
The data were analysed statistically by using statistical software SPSS version-16® (SPSS Inc., Chicago, Illinois, USA). All continuous data were expressed as mean and standard deviation and compared using independent sample t-test. All descriptive variables were compared using Chi-square-test. The level of significance was set at P < 0.05, and 95% confidence intervals were calculated for the main outcome measures.
RESULTS
Totally 112 patients were enrolled in the study. Two patients were removed from RD Group due to change in the surgical plan. General anaesthesia was administered in two patients in each group due to failed block and they were excluded from the analysis. Two patients in Group RD and 4 in Group R had inadequate block and they were also excluded. A total of 100 patients were included in statistical analysis (Group R n = 50, Group RD n = 50) [Figure 1].
Figure 1.
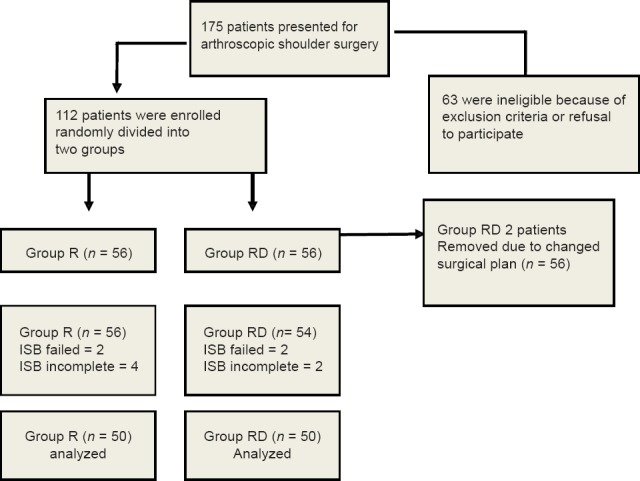
Consort diagram
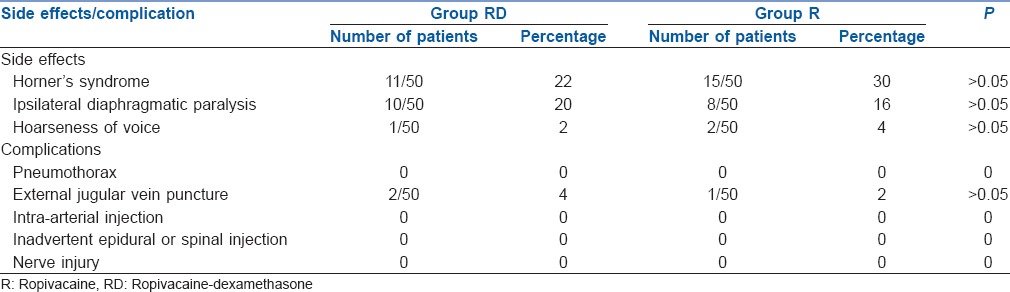
Patients in both groups were comparable in age, sex (male/female) ratio, weight and height [Table 1]. Onset of sensory block, motor block and onset of surgical anaesthesia were early in Group RD compared with Group R [statistically not significant (Table 2)]. The duration of analgesia was significantly prolonged in the Group RD 1103.72 ± 296.027 min compared to Group R 551.54 ± 166.92 min (P = 0.0001) [Table 2]. VAS scores in the first 4 h were comparable (P > 0.05). VAS scores were significantly higher in the Group R at the end of 8 h, 12 h, 16 h, 20 h and 24 h (P < 0.05). Patients in Group RD showed excellent pain control up to 24 h. and had significantly lower VAS scores (2.5–3.3) compared to Group R (4.2-5.06) (P < 0.05) [Figure 2]. Rescue analgesic consumption was significantly lower in the Group RD (1.22 ± 0.47 analgesic injections) in comparison to Group R (1.9 ± 0.73), (P < 0.001) in the first 24 h post-operatively [Figure 3]. The incidence of side-effects was low and comparable between the groups [Table 3]. HS was observed in 11/50 (22%) in Group RD and 15/50 (30%) in Group R (P > 0.05). Ipsilateral diaphragmatic paresis was seen in (10/50) (20%) in Group RD and (8/50) (16%) in Group R (P > 0.05). Hoarseness of voice due to recurrent laryngeal nerve block was seen in 1/50 (2%) in Group RD and in 2/50 (4%) in Group R (P > 0.05). No major complications like pneumothorax, epidural or spinal injection, intra-arterial injection, any neurological sequale (persistent numbness, paraesthesia or weakness of operative limb) were reported. Two patients (2/50) in Group RD and 1 (1/50) in Group R had external jugular vein puncture, which was managed with external compression and did not require any intervention [Table 3].
Table 1.
Demographic variables of ropivacaine group and ropivacaine-dexamethasone group
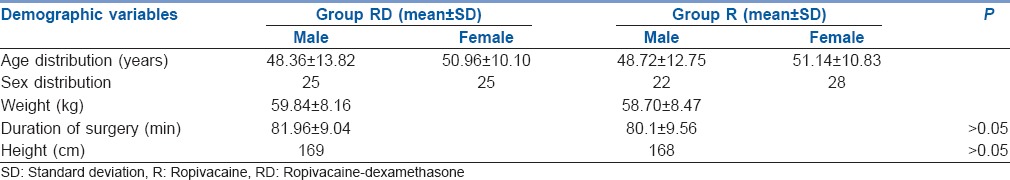
Table 2.
Onset of sensory block, motor block, surgical anaesthesia and duration of analgesia

Figure 2.
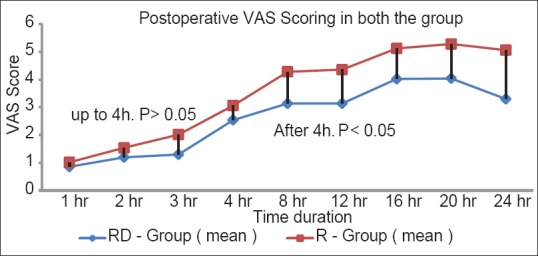
Comparative post-operative visual analogue scale scores
Figure 3.
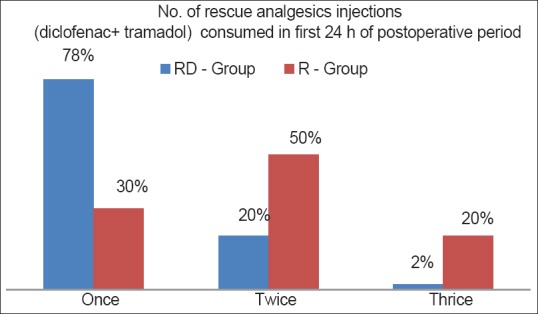
Number of rescue analgesics used in 24 h
Table 3.
Incidence of side effects and complication between the two groups
DISCUSSION
The present study demonstrated that dexamethasone significantly prolonged the duration of analgesia of ropivacaine in interscalene brachial plexus block. This finding was generally consistent with previous studies.[4,5,6,7] We observed 2.0-fold prolongation of analgesia in RD Group in comparison to Group R almost similar to Cummings et al.[5] who observed a 1.9-fold increase in the duration of ISB when dexamethasone was mixed with local anaesthetic. Dar et al.[6] noticed significant early onset of sensory and motor block when dexamethasone was mixed with ropivacaine and they postulated a synergism between ropivacaine and dexamethasone for this effect.[7] In a clinical situation, this difference could be dependent on local anaesthetic used during block. For example, early onset was observed when lignocaine[8] or mixture of lignocaine-bupivacaine was used[9,10] and no effect when mepivacaine was used.[11]
Steroid adjuvants have been found to prolong the block duration when used in regional blocks.[12,13] However, its mechanism of action is not clearly understood. Corticosteroids may have a local effect on the nerve,[7] or they may act by their anti-inflammatory effects[14] ; they may alter the function of potassium channels in the excitable cells via glucocorticoid receptors.[15]
We observed that mean VAS score and rescue analgesic consumption was significantly less when dexamethasone was mixed with ropivacaine. A recent systematic review has shown that dexamethasone significantly reduces the VAS score and analgesic consumption when used along with local anaesthetic however, the duration of significant relief is variable.[16]
Minor complications like HS were observed in 11/50 (22%) in Group RD and 15/50 (30%) in Group R (P > 0.05). Islam et al.[10] have reported 33.3% incidence of HS with mixture of lignocaine and bupivacaine and Desmet et al.[17] observed 20.5% HS in patients who received ropivacaine only and 23.5% patients who received ropivacaine and dexamethasone mixture in ISB. It has been observed that diaphragmatic paresis is an inevitable consequence of ISB when providing anaesthesia sufficient for shoulder surgery.[18] The low rate of occurrence in our study may be due to two reasons; firstly we used only 30 mL instead of large volumes reported in earlier reports, and secondly, we observed our patients clinically and did not use ultrasound for assessment.[18] We observed ipsilateral diaphragmatic paresis in (10/50, 20%) in Group RD and (8/50, 16%) in Group R; however, no patient complained of breathing difficulty. The involvement of ipsilateral phrenic nerve during ISB is frequently associated with a significant reduction in lung volumes which is well tolerated in most healthy patients.[19] Reported incidence of hoarseness of voice during ISB is variable and the reported highest incidence is 48%.[17] In our study, hoarseness of voice due to recurrent laryngeal nerve block was seen in 1/50 (2%) in Group RD and in 2/50 (4%) in Group R. Similar incidence is being commonly reported.[10,20] The incidence of serious vascular puncture (arterial puncture and haematoma formation) is rare during ISB. The reported incidence of arterial puncture and haematoma formation in one cadaveric study was <1.0%.[21] In our study, two patients (2/50) in Group RD and 1 (1/50) in Group R had external jugular vein puncture managed with external compression and did not require any intervention.
CONCLUSION
Dexamethasone (8 mg) significantly prolonged the duration of analgesia when used with 0.5% ropivacaine during ISB for arthroscopic surgery of shoulder. Dexamethasone also improved the quality of pain relief in the first 24 h post-operatively. Onset of sensory and motor block was not affected by dexamethasone. No patient had any serious complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Fredrickson MJ, Krishnan S, Chen CY. Postoperative analgesia for shoulder surgery: A critical appraisal and review of current techniques. Anaesthesia. 2010;65:608–24. doi: 10.1111/j.1365-2044.2009.06231.x. [DOI] [PubMed] [Google Scholar]
- 2.Chawda PM, Sharma G. A clinical study comparing epinephrine 200μg or clonidine 90μg as adjuvants to local anaesthetic agent in brachial plexus block via supraclavicular approach. J Anaesthesiol Clin Pharmacol. 2010;26:523–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Kohli S, Kaur M, Sahoo S, Vajifdar H, Kohli P. Brachial plexus block: Comparison of two different doses of clonidine added to bupivacaine. J Anaesthesiol Clin Pharmacol. 2013;29:491–5. doi: 10.4103/0970-9185.119147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Movafegh A, Razazian M, Hajimaohamadi F, Meysamie A. Dexamethasone added to lidocaine prolongs axillary brachial plexus blockade. Anesth Analg. 2006;102:263–7. doi: 10.1213/01.ane.0000189055.06729.0a. [DOI] [PubMed] [Google Scholar]
- 5.Cummings KC, 3rd, Napierkowski DE, Parra-Sanchez I, Kurz A, Dalton JE, Brems JJ, et al. Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine. Br J Anaesth. 2011;107:446–53. doi: 10.1093/bja/aer159. [DOI] [PubMed] [Google Scholar]
- 6.Dar FA, Najar MR, Jan N. Effect of addition of dexamethasone to ropivacaine in Supraclavicular brachial plexus block. Indian J Pain. 2013;27:165–9. [Google Scholar]
- 7.Dräger C, Benziger D, Gao F, Berde CB. Prolonged intercostal nerve blockade in sheep using controlled-release of bupivacaine and dexamethasone from polymer microspheres. Anesthesiology. 1998;89:969–79. doi: 10.1097/00000542-199810000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Biradar PA, Kaimar P, Gopalakrishna K. Effect of dexamethasone added to lidocaine in supraclavicular brachial plexus block: A prospective, randomised, double-blind study. Indian J Anaesth. 2013;57:180–4. doi: 10.4103/0019-5049.111850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shrestha BR, Maharjan SK, Tabedar S. Supraclavicular brachial plexus block with and without dexamethasone - A comparative study. Kathmandu Univ Med J (KUMJ) 2003;1:158–60. [PubMed] [Google Scholar]
- 10.Islam SM, Hossain MH, Maruf AA. Effect of addition of dexamethasone to local Anaesthetics in supraclavicular Brachial plexus block. JAFMC Bangladesh. 2011;7:11–4. [Google Scholar]
- 11.Parrington SJ, O'Donnell D, Chan VW, Brown-Shreves D, Subramanyam R, Qu M, et al. Dexamethasone added to mepivacaine prolongs the duration of analgesia after supraclavicular brachial plexus blockade. Reg Anesth Pain Med. 2010;35:422–6. doi: 10.1097/AAP.0b013e3181e85eb9. [DOI] [PubMed] [Google Scholar]
- 12.Stan T, Goodman EJ, Bravo-Fernandez C, Holbrook CR. Adding methylprednisolone to local anesthetic increases the duration of axillary block. Reg Anesth Pain Med. 2004;29:380–1. doi: 10.1016/j.rapm.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Golwala MP, Swadia VN, Dhimar AA, Sridhar NV. Pain relief by dexamethasone as an adjuvant to local anaesthetics in supraclavicular brachial plexus block. J Anaesthesiol Clin Pharmacol. 2009;25:285–8. [Google Scholar]
- 14.Ahlgren SC, Wang JF, Levine JD. C-fiber mechanical stimulus-response functions are different in inflammatory versus neuropathic hyperalgesia in the rat. Neuroscience. 1997;76:285–90. doi: 10.1016/s0306-4522(96)00290-4. [DOI] [PubMed] [Google Scholar]
- 15.Attardi B, Takimoto K, Gealy R, Severns C, Levitan ES. Glucocorticoid induced up-regulation of a pituitary K+channel mRNA in vitro and in vivo. Receptors Channels. 1993;1:287–93. [PubMed] [Google Scholar]
- 16.Noss C, MacKenzie L, Kostash M. Dexamethasone a promising adjuvant in brachial plexus anesthesia. A systematic review? J Anesth Clin Res. 2014;5:421. [Google Scholar]
- 17.Desmet M, Braems H, Reynvoet M, Plasschaert S, Van Cauwelaert J, Pottel H, et al. I.V. and perineural dexamethasone are equivalent in increasing the analgesic duration of a single-shot interscalene block with ropivacaine for shoulder surgery: A prospective, randomized, placebo-controlled study. Br J Anaesth. 2013;111:445–52. doi: 10.1093/bja/aet109. [DOI] [PubMed] [Google Scholar]
- 18.Urmey WF, Talts KH, Sharrock NE. One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg. 1991;72:498–503. doi: 10.1213/00000539-199104000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Hortense A, Perez MV, Amaral JL, Oshiro AC, Rossetti HB. Interscalene brachial plexus block. Effects on pulmonary function. Rev Bras Anestesiol. 2010;60:130–7, 74. doi: 10.1016/s0034-7094(10)70017-9. [DOI] [PubMed] [Google Scholar]
- 20.Casati A, Fanelli G, Aldegheri G, Berti M, Colnaghi E, Cedrati V, et al. Interscalene brachial plexus anaesthesia with 0.5%, 0.75% or 1% ropivacaine: A double-blind comparison with 2% mepivacaine. Br J Anaesth. 1999;83:872–5. doi: 10.1093/bja/83.6.872. [DOI] [PubMed] [Google Scholar]
- 21.Alemanno F, Capozzoli G, Egarter-Vigl E, Gottin L, Alberto B. The middle interscalene block: Cadaver study and clinical assessment. Reg Anesth Pain Med. 2006;31:563–8. doi: 10.1016/j.rapm.2006.05.015. [DOI] [PubMed] [Google Scholar]


