A cross-sectional survey of hospital pharmacies in New Jersey demonstrates a lack of general consensus regarding hospital pharmacy preparedness for mass casualty scenarios despite individualized institutional protocols for disaster preparedness.
Keywords: Hospital pharmacy, mass casualty, disaster preparedness, pharmacist roles
Abstract
Objectives:
To assess the preparedness of hospital pharmacies in New Jersey to provide pharmaceutical services in mass casualty scenarios.
Methods:
An electronic cross-sectional survey was developed to assess the general knowledge of available resources and attitudes toward the preparedness of the pharmacy department.
Results:
Out of 60 invitations to participate, 18 surveys (30%) were completed. Respondents practiced at community hospitals (12, 66.6%) with no trauma center designation (11, 67.4%) that served more than 500 licensed beds (five, 29.4%). Six respondents (35.3%) indicated that 75,000 to 100,000 patients visited their emergency departments annually. Seventeen sites (94.4%) reported the existence of an institutional disaster preparedness protocol; 10 (55.5%) indicated that there is a specific plan for the pharmacy department. Most respondents (10, 55.5%) were unsure whether their hospitals had an adequate supply of analgesics, rapid sequence intubation agents, vasopressors, antiemetics, respiratory medications, ophthalmics, oral antimicrobials, and chemical-weapon-specific antidotes. Five (27.7%) agreed that the pharmacy disaster plan included processes to ensure care for patients already hospitalized, and four (22.2%) agreed that the quantity of medication was adequate to treat patients and hospital employees if necessary. Medication stock and quantities were determined based on national or international guidelines at three (16.6%) institutions surveyed.
Conclusion:
This survey demonstrates a lack of general consensus regarding hospital pharmacy preparedness for mass casualty scenarios despite individualized institutional protocols for disaster preparedness. Standardized recommendations from government and/or professional pharmacy organizations should be developed to guide the preparation of hospital pharmacy departments for mass casualty scenarios.
INTRODUCTION
The United States faces a broad threat of disasters that can cause damage and destruction.1 These diverse threats include natural disasters (i.e., hurricanes, tornadoes, earthquakes), man-made accidental disasters (i.e., industrial chemical spills), man-made intentional disasters (i.e., acts of terrorism), and technological disasters that may fall under each category (i.e., power grid failure).1 In response to these threats, two overarching presidential directives were issued. Homeland Security Presidential Directive 5 helped establish the National Incident Management System (NIMS). Presidential Policy Directive 8 was issued to prepare the United States for threats with specific objectives as part of the National Preparedness Goal (NPG), which aims to prevent, protect against, mitigate, respond to, and recover from any form of emergency or disaster. The accompanying National Preparedness System (NPS) is designed to achieve this goal.1–3
Hospitals across the country increasingly understand their role in emergency preparedness.2 Due to the diverse needs of respective institutions, individual hospitals are responsible for creating a Hospital Incident Command System (HICS) with a customized response structure.4 Within the HICS, coordinated efforts must encompass various hospital departments, including nursing, medicine, pharmacy, and administration. Each department must be equally prepared with a specific, defined role.5 Pharmacy departments play a critical role in the HICS, ensuring adequate supply and utilization of medications. The American Society of Health-System Pharmacists (ASHP) has provided two statements describing the general role of hospital pharmacists and pharmacy departments in disaster preparedness and counterterrorism, but both are lacking in specifically defining how pharmacists and pharmacy departments should prepare for and participate in such events.6,7 While the available literature provides retrospective descriptions of preparation and response (such as hospital pharmacy response to Hurricane Sandy8), to date, specific resources are not available for planning and for training health system pharmacy personnel in preparation for mass casualty and patient surge events.
To develop such recommendations, it is necessary to understand current practices that hospital pharmacies are undertaking. A survey of New Jersey hospital pharmacy departments was conducted to assess how they are prepared to provide pharmaceutical services in mass casualty scenarios.
METHODS
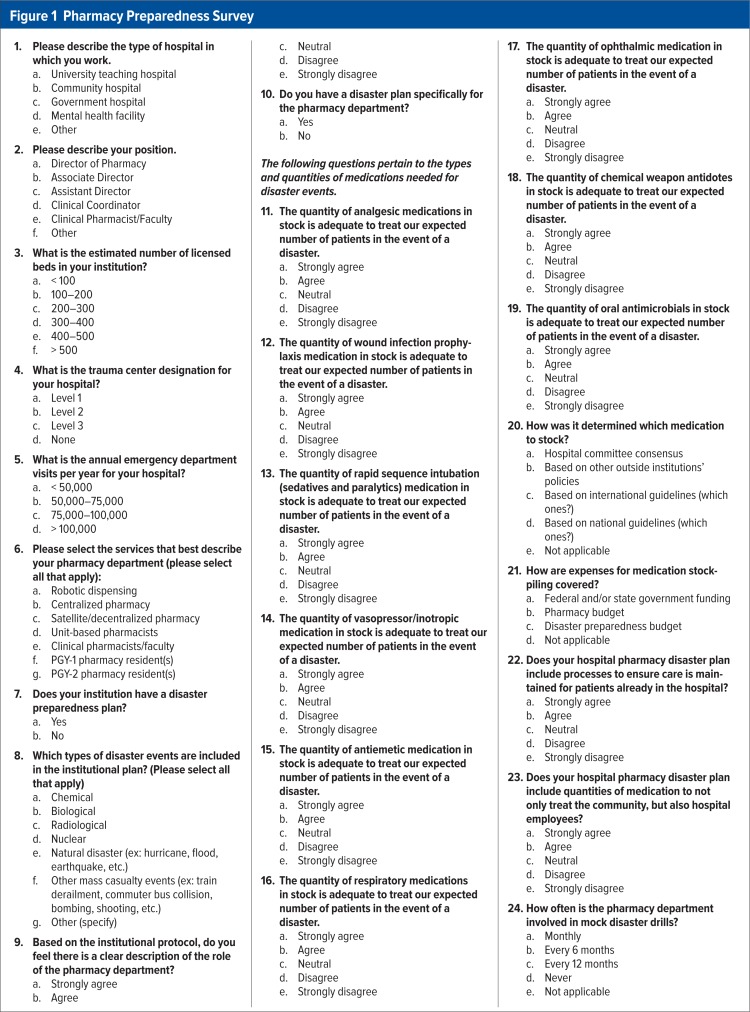
This study and the survey tool were approved by the institutional review board at Rutgers University. An electronic cross-sectional survey developed via SurveyMonkey (www.surveymonkey.com) was distributed to hospital pharmacy directors or representatives in New Jersey. The survey consisted of questions assessing the general knowledge of available resources, attitudes toward the preparedness of the pharmacy department, and expectations of government and national pharmacy organization recommendations to guide pharmacy preparedness. The survey tool consisted of 12 questions formatted under the Likert scale (allowing five responses ranging from “strongly disagree” to “strongly agree”) and 12 multiple-choice questions (Figure 1).
Figure 1.
Pharmacy Preparedness Survey
Pharmacy departments at all identifiable acute-care hospitals in New Jersey were eligible. The contact email for each pharmacy director or representative was accessed through each hospital’s website as listed on the New Jersey Hospital Association website (www.njha.com). The survey remained open for two months, from June 1 through August 1, 2013. Data were collected and analyzed using descriptive statistics.
RESULTS
Sixty invitations to participate were distributed; 18 surveys (30%) were returned. However, not all questions were answered on all 18 of these surveys, so the number of answers to each question serves as the denominator for that response.
Most respondents practiced at community hospitals (12, 66.6%), followed by university teaching hospitals (four, 22.2%), with the remainder designating themselves as “other” (two, 11.1%). The majority of institutions were not trauma centers (11, 64.7%), while two (11.8%) were designated Level I trauma centers, three (17.7%) were Level II trauma centers, and one (5.9%) was a Level III trauma center (Table 1).
Table 1.
Demographics of Respondents (N = 17)
| Number of Licensed Beds | n | % |
| Less than 100 | 1 | 5.9 |
| 100 to 200 | 2 | 11.8 |
| 200 to 300 | 4 | 23.5 |
| 300 to 400 | 4 | 23.5 |
| 400 to 500 | 1 | 5.9 |
| Greater than 500 | 5 | 29.4 |
| Annual Number of Visits to the Emergency Department | n | % |
| Less than 50,000 | 5 | 29.4 |
| 50,000 to 75,000 | 3 | 17.7 |
| 75,000 to 100,000 | 6 | 35.3 |
| Greater than 100,000 | 3 | 17.7 |
| Trauma Center Designation | n | % |
| Level I | 2 | 11.8 |
| Level II | 3 | 17.7 |
| Level III | 1 | 5.9 |
| None | 11 | 64.7 |
| Provision of Pharmacy Services | n | % |
| Robotic dispensing | 5 | 29.4 |
| Centralized pharmacy | 16 | 94.1 |
| Clinical pharmacists/faculty | 13 | 76.5 |
| Unit-based pharmacists | 6 | 35.3 |
| Decentralized pharmacy satellites | 6 | 35.3 |
| PGY-1 general residents | 8 | 47.1 |
| PGY-2 specialty residents | 2 | 11.8 |
Among these institutions, the estimated numbers of licensed beds and annual emergency department visits varied widely. A centralized pharmacy department structure was common among surveyed institutions (16 of 17, 94.1%), as was the presence of clinical pharmacists/faculty (13 of 17, 76.5%) (Table 1).
All 18 respondents indicated that an institutional disaster preparedness protocol existed at their facility, with only one (6.25%) strongly agreeing that there was a clear description of the role of the pharmacy department. Additionally, 10 (55.5%) indicated that there was a specific plan for the pharmacy department. Most respondents (10, 55.5%) were unsure about the adequacy of their hospital’s quantity of analgesic medication, rapid sequence intubation agents, vasopressors, antiemetics, respiratory medications, ophthalmic medications, oral antimicrobials, and chemical-weapon-specific antidotes (Table 2). Five (27.7%) agreed that the pharmacy disaster plan included processes to ensure care for patients already hospitalized, and four (22.2%) agreed that the quantity of medication was adequate to treat both patients and hospital employees. Three respondents (16.6%) indicated that medication stock and quantities were determined based on national or international guidelines. Of the eight respondents reporting how medication-stockpiling expenses were paid, five (62.5%) reported that the pharmacy department budget accounted for medication stockpiling for disaster preparedness, while two institutions (25%) used federal and/or state government funding. Of the eight respondents reporting the frequency of disaster drills at their institutions, four (50%) conducted drills every six months, three (37.5%) conducted drills annually, and one (12.5%) had never conducted a drill.
Table 2.
Distribution of Responses When Asked if Stock of the Following Categories of Medications Is Adequate to Treat the Expected Number of Patients in the Event of a Disaster for Hospital Pharmacies With a Specific Preparedness Plan in Place (n = 8)
| Medication Categories | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
|---|---|---|---|---|---|
| Analgesics | 0 (0%) | 0 (0%) | 1 (12.5%) | 6 (75%) | 1 (12.5%) |
| Medications for rapid sequence intubation | 0 (0%) | 1 (12.5%) | 1 (12.5%) | 5 (62.5%) | 1 (12.5%) |
| Vasopressors/inotropes | 0 (0%) | 0 (0%) | 2 (25%) | 4 (50%) | 2 (25%) |
| Antiemetics | 0 (0%) | 0 (0%) | 1 (12.5%) | 4 (50%) | 3 (37.5%) |
| Respiratory medications | 0 (0%) | 0 (0%) | 0 (0%) | 6 (75%) | 2 (25%) |
| Ophthalmic medications | 1 (12.5%) | 1 (12.5%) | 3 (37.5%) | 3 (37.5%) | 0 (0%) |
| Chemical weapon antidotes | 1 (12.5%) | 1 (12.5%) | 0 (0%) | 5 (62.5%) | 1 (12.5%) |
| Oral antimicrobials | 1 (12.5%) | 1 (12.5%) | 0 (0%) | 4 (50%) | 2 (25%) |
DISCUSSION
Under the directives of NIMS, customized HICSs exist to provide a framework for hospitals to prevent, protect against, mitigate, respond to, and recover from any form of emergency or disaster. Within health systems, pharmacy departments and personnel play a critical role in any HICS model. While the needs of each health care organization vary, there are consistent functions across all hospital pharmacy departments that can aid in planning and preparing for disasters and responding when they occur.
Pharmacists possess critically important skills that can be applied in disaster response settings. Within the various sub-specialties of pharmacy, clinicians can put those skills to use in response to biological events (infectious disease pharmacists), radiological and nuclear events (hematology/oncology pharmacists), and chemical events (emergency medicine and critical-care pharmacists); general-practice pharmacists are capable of counseling patients or administering vaccinations. To effectively use these skills to benefit the response, clear roles and responsibilities must be defined to optimize effort.9 Pincock and colleagues described the potential role for pharmacists in emergency preparedness, but echoed the need for standardized definitions of the role and training necessary for each pharmacist taking on this reponsibility.10
In this survey, all respondents indicated that an institution-specific disaster plan existed, but only one institution indicated that there was specific delineation and description of the role and responsibility of the pharmacy department in mass-casualty events. Approximately half of the respondents indicated that a specific pharmacy plan exists in their HICS. The wide variation in disaster preparedness across institutions was further demonstrated in the consistent uncertainty about the types and quantities of medications stocked for a disaster, the intended population for treatment, and the resources available to guide decision-making.
This survey highlighted areas for improvement with the delineation of roles and responsibilities of hospital pharmacy departments and their personnel, but important limitations must be disclosed. While this survey attempted to describe the preparedness of all acute-care hospitals in New Jersey, the study survey tool was not validated (although no such validated survey tool exists). While the response rate of 30% does not represent the entire population, we feel that the survey sample, including two of the three Level I trauma centers in New Jersey, reflects institutions that will likely face the greatest impact during a disaster response. However, outcomes may vary based on the needs established in planning with local emergency management agencies or in coordination with other local hospitals to share medication caches. State and regional preparedness and responses are variable and are also important for a hospital to consider and accommodate. Communication and planning with state and local organizations are keys to a hospital knowing what outside resources are available and what these organizations expect of the hospital in disaster scenarios.
Finally, the sample size may not reflect emergency preparedness in all hospitals across the United States, including geographical areas that are accustomed to responding to natural disasters such as hurricanes, tornadoes, and earthquakes. A subsequent study should be conducted nationally with a validated survey tool to further identify areas of needed improvement and future guideline recommendations. Similarly, national pharmacy organizations should seek out professional colleagues around the globe to identify best practices for pharmacists in areas with frequent natural, accidental, or intentional disasters. Institutional pharmacy departments that address the identified areas for improvement in emergency preparedness plans will require important information, including:
Guidance on the types of medications to stock for various scenarios
The availability of these agents, especially as it relates to formulary management and ongoing drug shortages
The anticipated number of patients potentially affected in different scenarios
The duration of treatment needs under various circumstances
CONCLUSION
This survey demonstrates that despite individualized institutional protocols for disaster preparedness, there is a lack of general consensus regarding hospital pharmacy preparedness for mass-casualty scenarios. Standardized recommendations from government and/or professional pharmacy organizations should be developed to guide the preparation of hospital pharmacy departments for mass-casualty scenarios.
Footnotes
Disclosure: The authors report that they have no commercial or financial relationships in regard to this article.
REFERENCES
- 1.Department of Homeland Security Presidential Policy Directive 8: National Preparedness. Mar 30, 2011. Available at: www.dhs.gov/presidential-policy-directive-8-national-preparedness. Accessed August 10, 2013.
- 2.Federal Emergency Management Agency. National Incident Management System Available at: http://www.fema.gov/national-incident-management-system. Accessed August 10, 2013.
- 3.Department of Homeland Security National Preparedness Goal. Available at: http://www.fema.gov/national-preparedness-goal. Accessed August 10, 2013.
- 4.California Emergency Medical Services Authority Hospital Incident Command System Guidebook. Aug, 2006. Available at http://www.emsa.ca.gov/Media/Default/Word/Guidebook_Glossary.pdf. Accessed August 29, 2013.
- 5.Macintyre AG, Christopher GW, Eitzen E, Jr, et al. Weapons of mass destruction events with contaminated casualties: effective planning for health care facilities. JAMA. 2000;283(2):242–249. doi: 10.1001/jama.283.2.242. [DOI] [PubMed] [Google Scholar]
- 6.American Society of Health-System Pharmacists ASHP statement on the role of health-system pharmacists in emergency preparedness. Am J Health-Syst Pharm. 2003;60(19):1993–1995. doi: 10.1093/ajhp/60.19.1993. [DOI] [PubMed] [Google Scholar]
- 7.American Society of Health-System Pharmacists ASHP statement on the role of health-system pharmacists in counterterrorism. Am J Health-Syst Pharm. 2002;59(3):282–283. doi: 10.1093/ajhp/59.3.282. [DOI] [PubMed] [Google Scholar]
- 8.Traynor K. New Jersey hospitals come through during Hurricane Sandy. Am J Health-Syst Pharm. 2012;69(24):2120, 2122. doi: 10.2146/news120084. [DOI] [PubMed] [Google Scholar]
- 9.Buckingham M. The One Thing You Need to Know About Great Managing, Great Leading and Sustained Individual Success. New York, New York: Free Press; 2005. pp. 150–151. [Google Scholar]
- 10.Pincock LL, Montello MJ, Tarosky MJ, et al. Pharmacist readiness roles for emergency preparedness. Am J Health-Syst Pharm. 2011;68(7):620–623. doi: 10.2146/ajhp090659. [DOI] [PubMed] [Google Scholar]