Abstract
OBJECTIVES
The current study evaluates the incremental value of transluminal attenuation gradient (TAG), TAG with corrected contrast opacification (CCO), and TAG with exclusion of calcified coronary segments (ExC) over coronary computed tomography angiogram (CTA) alone using fractional flow reserve (FFR) as the gold standard.
BACKGROUND
TAG is defined as the contrast opacification gradient along the length of a coronary artery on a coronary CTA. Preliminary data suggest that TAG provides additional functional information. Interpretation of TAG is hampered by multiple heartbeat acquisition algorithms and coronary calcifications. Two correction models have been proposed based on either dephasing of contrast delivery by relating coronary density to corresponding descending aortic opacification (TAG-CCO) or excluding calcified coronary segments (TAG-ExC).
METHODS
Eighty-five patients with intermediate probability of coronary artery disease were prospectively included. All patients underwent step-and-shoot 256-slice coronary CTA. TAG, TAG-CCO, and TAG-ExC analyses were performed followed by invasive coronary angiography in conjunction with FFR measurements of all major coronary branches.
RESULTS
Thirty-four patients (40%) were diagnosed with hemodynamically-significant coronary artery disease (i.e., FFR ≤0.80). On a per-vessel basis (n = 253), 59 lesions (23%) were graded as hemodynamically significant, and the diagnostic accuracy of coronary CTA (diameter stenosis ≥50%) was 95%, 75%, 98%, and 54% for sensitivity, specificity, negative predictive value, and positive predictive value, respectively. TAG and TAG-ExC did not discriminate between vessels with or without hemodynamically significant lesions (−13.5 ± 17.1 HU [Hounsfield units] × 10 mm−1 vs. −11.6 ± 13.3 HU × 10 mm−1, p = 0.36; and 13.1 ± 15.9 HU × 10 mm−1 vs. −11.4 ± 11.7 HU × 10 mm−1, p = 0.77, respectively). TAG-CCO was lower in vessels with a hemodynamically-significant lesion (−0.050 ± 0.051 10 mm−1 vs. −0.036 ± 0.034 10 mm−1, p = 0.03) and TAG-ExC resulted in a slight improvement of the net reclassification index (0.021, p < 0.05).
CONCLUSIONS
TAG did not provide incremental diagnostic value over 256-slice coronary CTA alone in assessing the hemodynamic consequences of a coronary stenosis. Correction for temporal nonuniformity of contrast delivery or exclusion of calcified coronary segments slightly enhanced the results.
Keywords: coronary artery disease, coronary computed tomography angiography, fractional flow reserve
Coronary computed tomography angiography (CTA) is increasingly used as a noninvasive diagnostic imaging tool for detection and exclusion of coronary artery disease (CAD) (1–3). A well-recognized limitation of coronary CTA, similar to the anatomical evaluation during invasive coronary angiography (ICA), is its moderate ability to assess the hemodynamic significance of a given coronary stenosis (4–6). Therefore, functional evaluation of coronary lesions deemed significant by coronary CTA is warranted to avoid excess referral for ICA and to guide revascularization therapy in a judicious manner (6,7). Although computed tomography (CT) stress perfusion and coronary CTA-derived estimation of fractional flow reserve (FFRCT) based on computational fluid dynamics have been developed for this purpose, these methods require additional contrast/radiation exposure or extremely complex off-line analysis, respectively, hampering their implementation in routine clinical practice (8–11). Alternatively, linear regression analysis of the attenuation gradient along the course of a coronary artery has been proposed to evaluate the functional relevance of a coronary lesion. The rationale behind the transluminal attenuation gradient (TAG) is that contrast opacification should fall off more rapidly in the presence of a functionally-significant stenosis (12). Preliminary data, obtained using a 320-row CT, have shown incremental value of TAG over coronary CTA assessment alone (13). However, TAG interpretation is complicated by multiple heartbeat acquisitions (64- to 256-slice CT) resulting in a lack of temporal uniformity. In addition, distortions due to highly calcified coronary plaques may influence results. Two correction models have been proposed based on either dephasing of contrast delivery by relating coronary density to corresponding descending aortic opacification (TAG corrected contrast opacification [CCO]) or excluding nonlinear values provoked by coronary calcifications (TAG excluding calcified coronary segments [ExC]) (14,15). Studies that have evaluated these models are scarce, and the results are conflicting (14–17). The current study aims to explore the diagnostic potential of TAG, including its correction models, obtained with a 256-slice CT scanner. Imaging results were prospectively compared with ICA in conjunction with invasive FFR.
METHODS
Patient population
A total of 91 patients with an intermediate probability of CAD, determined according to the criteria of Diamond and Forrester (18), were prospectively enrolled. Exclusion criteria were previous percutaneous coronary intervention, coronary artery bypass graft surgery, a previous myocardial infarction, atrial fibrillation, second- or third-degree atrioventricular block, impaired renal function, symptomatic asthma, or pregnancy. Electrocardiography and echocardiography confirmed normal global left ventricular systolic function and the absence of previous myocardial infarction or regional wall motion abnormalities in all patients. The protocol consisted of cardiac CT with coronary artery calcium (CAC) score and coronary CTA, followed by ICA in conjunction with FFR measurements of all major coronary branches within 5 days. Coronary CTA was not performed in case of persistent elevated heart rate above 65 beats/min despite pre-treatment with beta-blocking agents (n = 4). Two patients refused ICA after coronary CTA. The study population, therefore, comprised 85 patients. No cardiac events were documented between coronary CTA and ICA in these patients. The study was approved by the ethics committee, and written informed consent was obtained from all patients.
Cardiac CT
Patients underwent CAC scoring and coronary CTA on a 256-slice CT scanner (Philips Brilliance iCT, Philips Healthcare, Best, the Netherlands). A stable low heart rate <65 beats/min was achieved prior to the scanning protocol, either spontaneously or after administration of oral and/or intravenous metoprolol. A standard scanning protocol was applied, with a section collimation of 2 × 128 × 0.625 mm, a gantry rotation time of 270 ms, a tube voltage of 120 kV, and a tube current of 55 to 150 mA (for CAC scoring) or 200 mA (for coronary CTA). All scans were performed with prospective electrocardiogram-gating (Step & Shoot Cardiac, Philips Healthcare) at 75% of the R-R interval. Coronary calcification was defined as a plaque with an area of 1.03 mm2 and a density ≥130 Hounsfield units (HU). The CAC score was calculated according to the method described by Agatston et al. (19). After CAC scoring, coronary CTA was performed immediately after administration of sublingual nitroglycerine. For visualization of the coronary artery lumen, a bolus of 100 ml iobitridol (XenetiX 350, Guerbet, Brussels, Belgium) was injected intravenously (5.7 ml · s−1 ) followed by a 50-ml saline chaser. The scan was triggered, using an automatic bolus-tracking technique with a region of interest placed in the descending thoracic aorta, at a threshold of 150 HU. All CT scans were analyzed on a 3-dimensional workstation (Brilliance, Philips Medical Systems) by an experienced radiologist and cardiologist. The coronary tree was evaluated according to a 16-segment coronary artery model modified from that of the American Heart Association (20); a ≥50% diameter stenosis (DS) was deemed significant. Image quality was determined on a 3-point scale: poor, moderate, or good. The mean radiation effective dose during CAC score and coronary CTA was estimated using the dose-length product multiplied by 0.014 as conversion factor (21).
Transluminal attenuation gradient
TAG was determined on an IntelliSpace Portal workstation (version 5.0.0.20030, Philips). For all major coronary branches on coronary CTA, the luminal centerline was determined. Perpendicular cross-sectional images were constructed, and a circular region of interest of 1.0 mm2 was manually positioned in the luminal center. The mean HU were determined within the region of interest. Measurements were obtained at 5-mm intervals from the coronary ostium to the distal segment (up to a cross-sectional area of 2.0 mm2 as described previously [13]). TAG, expressed in HU × 10 mm−1 , was measured in the 3 major coronary branches matching the arteries interrogated by FFR. Besides standard TAG analysis, 2 correction models were applied: 1) TAG-ExC, excluding excessive calcified coronary segments in order to maintain linearity of the gradient (14,17); and 2) TAG-CCO, corrected for timing-dependent perturbation of coronary contrast delivery associated with multiple heart beat imaging of 256-slice coronary CTA. Each luminal attenuation measurement was normalized to the descending aortic attenuation of the corresponding scanning cycle by dividing the mean coronary HU by the mean aortic HU (13,15,17). TAG-CCO is defined as the gradient of the quotient of the mean coronary HU and mean aortic HU per 10 mm.
ICA and FFR
ICA imaging was performed with a biplane or monoplane cardiovascular x-ray system (Allura Xper FD 10/10, Philips Healthcare) in ≥2 orthogonal directions per evaluated coronary artery segment. Prior to the contrast injection, 0.2 ml of nitroglycerin was administered intracoronarily to induce epicardial coronary vasodilation. Each major coronary artery territory was routinely interrogated by FFR except for occluded or subtotal lesions. The operator refrained from FFR measurements in these tight lesions due to the potential risk of inflicting a coronary dissection by the pressure wire. The FFR was measured using a 0.014-inch sensor-tipped guidewire (Volcano Corporation, Rancho Cordova, California), which was introduced through a 5- or 6-F guiding catheter, calibrated, and advanced into the coronary artery. Adenosine was infused intracoronarily (150 µg) in the right and left coronary artery to induce maximal coronary hyperemia (22). The FFR was calculated as the ratio of the mean distal intracoronary pressure, measured by the pressure wire, to the mean arterial pressure measured by the coronary catheter (23). A stenosis with >90% luminal diameter reduction or with an FFR ≤0.80 was considered hemodynamically significant (6). The coronary tree was divided into a 16-segment coronary artery model modified from the American Heart Association (20). Quantitative coronary angiography was performed on all coronary segments >1.5 mm in diameter (Xcelera, Philips Healthcare). Two experienced interventional cardiologists blinded to the coronary CTA results interpreted all images and FFR signals. TIMI (Thrombolysis In Myocardial Infarction) flow grade was assessed in each major coronary artery.
Statistical analyses
Continuous variables are presented as mean ± SD, whereas categorical variables are expressed as actual numbers. TAG, TAG-ExC, and TAG-CCO were determined as a linear regression coefficient from the coronary ostium to the most distally measured value per 10 mm. There were no corrections performed for the interdependency of the coronary data within 1 patient. Continuous variables of TAG, TAG-ExC, and TAG-CCO between groups were compared with the Mann-Whitney U test because of non-normal distribution. A receiver-operating characteristic curve analysis was used to define optimal cutoff values based on the maximal sum of specificity and sensitivity (Youden index) to obtain the highest discriminatory value for TAG, TAG-ExC, and TAG-CCO. Diagnostic performance of coronary CTA, TAG, TAG-ExC, and TAG-CCO for the diagnosis of obstructive CAD compared with FFR was determined with sensitivity, specificity, negative predictive value, and positive predictive value, including their related 95% confidence intervals, on a per-vessel and -patient basis. Incremental value of TAG, TAG-ExC, and TAG-CCO to coronary CTA was determined with area under the receiver-operating characteristic curve analysis based on a combination of parameters in the logistic regression model and the net reclassification index (24). The relations among the 3 TAG modalities were analyzed using linear regression analysis. Intraobserver and interobserver variability of TAG was determined with the intraclass correlation coefficient using a 2-way random effects model. A p value <0.05 was considered statistically significant. All statistical analyses were performed using SPSS software package (version 20.0, IBM SPSS Statistics, Chicago, Illinois).
RESULTS
Baseline characteristics of the 85 included patients are shown in Table 1.
Table 1.
Baseline Patient Characteristics (n = 85)
| Age, yrs | 57.3 ± 9.7 |
| Male | 51 (60) |
| Body mass index, kg · mm−2 | 27.1 ± 4.1 |
| CAD risk factors | |
| Hypertension | 31 (37) |
| Hypercholesterolemia | 32 (38) |
| Current or history of smoking | 38 (45) |
| Family history of IHD | 39 (46) |
| Diabetes | 13 (16) |
| Medication | |
| Aspirin | 76 (89) |
| ACE inhibitors | 16 (19) |
| Beta-blockers | 54 (64) |
| Statins | 72 (85) |
| Angiotensin-II receptor blockers | 12 (14) |
| Calcium-channel blockers | 31 (25) |
| Long acting nitrates | 10 (12) |
Values are mean ± SD or n (%).
ACE = angiotensin-converting enzyme; CAD = coronary artery disease; IHD = ischemic heart disease.
Coronary CTA
Prior to coronary CTA, 14 patients (16%) received additional oral metoprolol (range 50 to 150 mg), and in 30 patients (35%), metoprolol was administered intravenously (range 5 to 30 mg). Sublingual nitroglycerin was given in 83 patients (98%). All patients were in sinus rhythm with an average heart rate of 57 ± 7 min−1 , coronary CTA characteristics are shown in Table 2. Fifty-two of 85 patients (61%) were diagnosed with obstructive CAD (i.e., >50% DS in ≥1coronary artery) based on coronary CTA results.
Table 2.
Coronary Computed Tomography Angiography
| Characteristics | |
| Heart rate, beats/min | 57 ± 7 |
| Radiation dose, mSv | 4.97 ± 0.89 |
| Image quality | |
| Good | 73 (86) |
| Moderate | 10 (12) |
| Poor | 2(2) |
| Coronary CTA DS ≥50% | |
| Per patient (n = 85) | 52(61) |
| Per vessel (n = 253) | 104 (41) |
| CAC score | 141 (0–818) |
| Age- and sex-corrected percentile, % | 66 ± 37 |
Values are mean ± SD, n (%), or median (interquartile range).
CAC = coronary artery calcium; CTA = computed tomography angiography; DS = diameter stenosis.
Invasive coronary angiography
All procedures and FFR measurements were conducted without any complications. Of the 255 vessels in 85 patients, 2 vessels with an intermediate stenosis were excluded due to the inability to interrogate the artery with FFR owing to tortuosity, resulting in a total of 253 evaluated vessels. FFR measurements were obtained in 230 of these 253 vessels (91%). The operator refrained from FFR interrogation in 19 arteries (8%) due to the presence of a subtotal lesion, and 3 lesions (1%) were chronic total occlusions with collateral circulation from a native donor artery. These 22 (sub)total lesions were considered hemodynamically significant (6). All patent arteries displayed TIMI flow grade 3. In 1 vessel without an apparent lesion, FFR was not obtained for technical reasons. This vessel was allocated to the nonsignificant group. On a per-patient basis, 34 (40%) displayed ≥1 vessel with FFR ≤0.80, whereas on a per-vessel basis, 59 lesions (23%) were hemodynamically significant. Quantitative coronary angiography diameter stenosis per vessel analysis is shown in Table 3.
Table 3.
QCA DS at ICA (n = 253)
| <30% | 137 (54) |
| 30%–49% | 57 (23) |
| 50%–70% | 22 (9) |
| >70% | 37(15) |
Values are n (%).
DS = diameter stenosis; ICA = invasive coronary angiography; QCA = quantitative coronary angiography.
Transluminal attenuation gradient
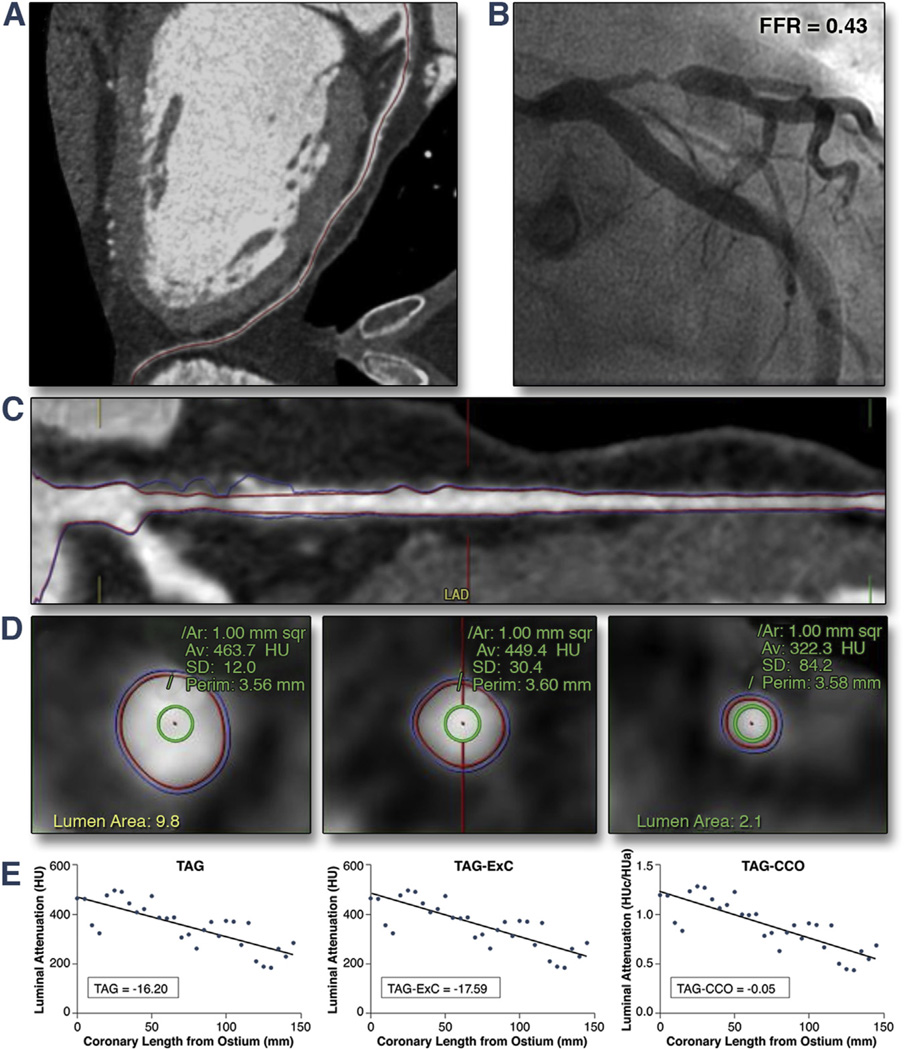
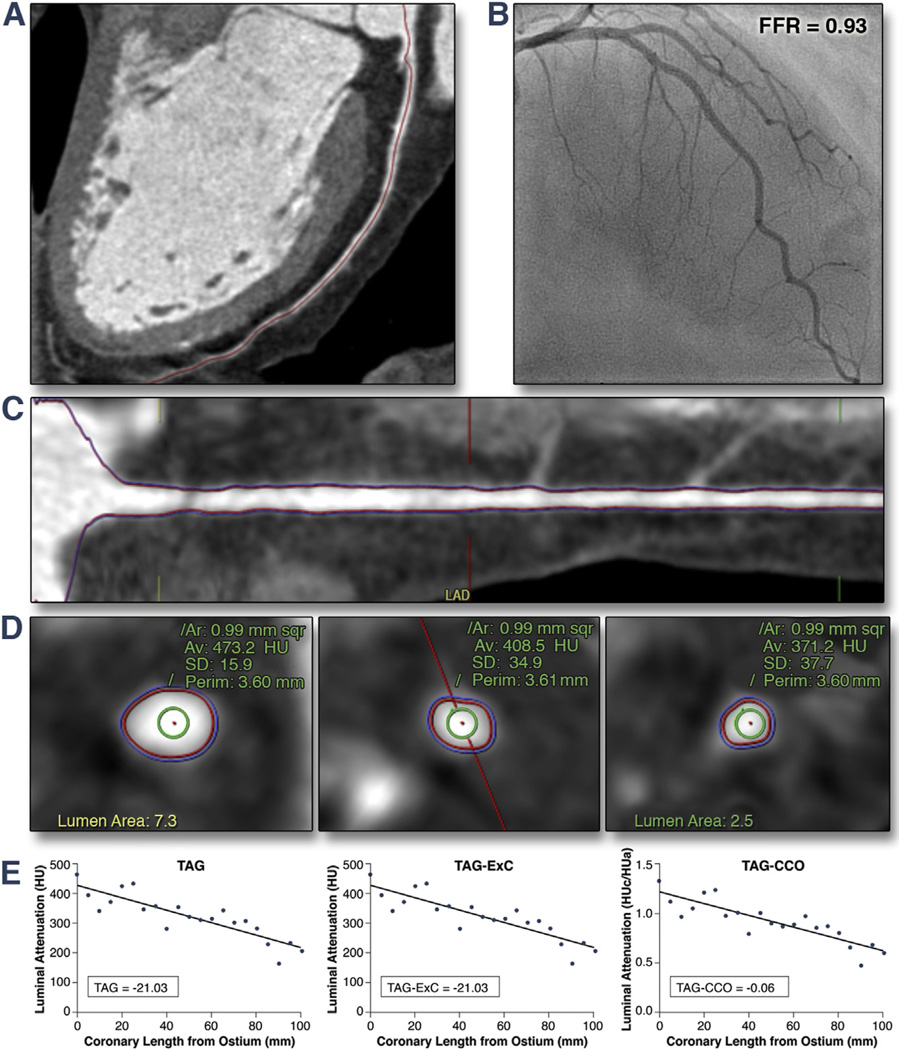
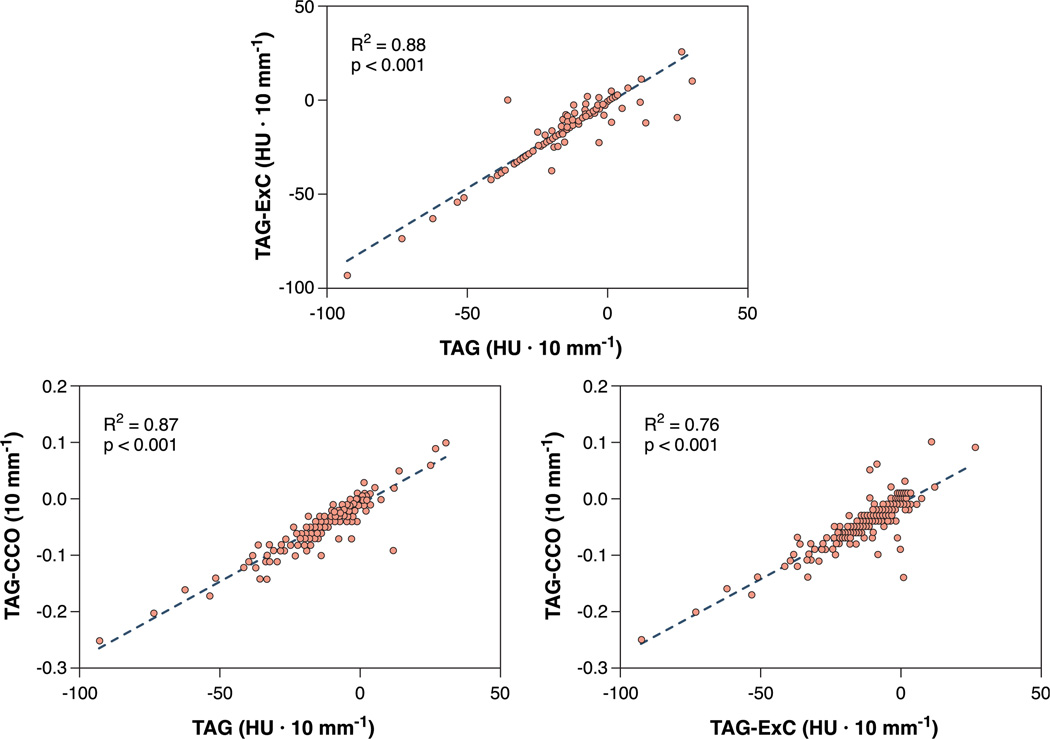
TAG, TAG-ExC, and TAG-CCO were measured in all 253 vessels, regardless of the presence of CAD or image quality (good to moderate in 98%) (Table 2, Figs. 1 and 2). Subgroup analysis was performed in vessels with a coronary CTA-based DS ≥50%. Table 4 lists mean TAG parameters and differentiation between vessels with or without coronary CTA-graded significant lesions. Although all 3 TAG analyses showed on average a slightly lower value for the vessels containing a hemodynamically significant stenosis, statistical significance was only achieved for TAG-CCO (p = 0.03). When subgroup analysis of vessels with a coronary CTA-based DS $50% was performed, TAG-CCO was no longer significant (n = 104, p = 0.07). Figure 3 shows the correlation between different TAG parameters. All correlations were highly significant (p < 0.001).
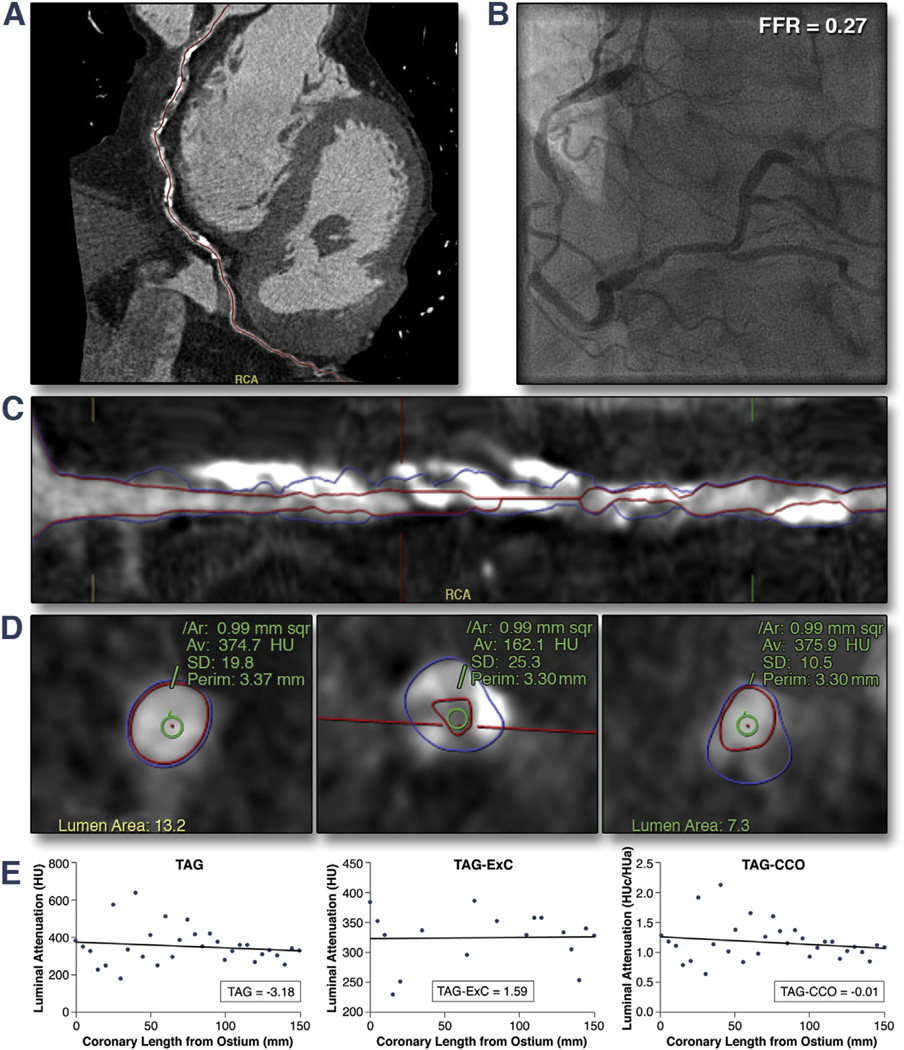
Figure 1. Example of TAG Analysis of a LAD With a Hemodynamically-Significant Stenosis.
Coronary computed tomography angiography (CTA) (A and C) and cross-sectional images with the region of interest indicated by the green circle (D), invasive coronary angiography with FFR (B), and results of 3 transluminal attenuation gradient (TAG) analyses (E). Note the decrease of contrast density along the coronary artery, which is compatible with the presence of an obstructive lesion in the left anterior descending coronary artery (LAD) with a noncalcified hemodynamically-significant stenosis (fractional flow reserve [FFR] = 0.43). CCO = corrected contrast opacification; ExC = excluding calcified coronary segments; HU = Hounsfield units; HUa = aortic Hounsfield units; HUc = coronary Hounsfield units.
Figure 2. Example of TAG Analysis of a LAD Without Stenosis.
Coronary CTA (A and C) and cross-sectional images with the region of interest indicated by the green circle (D), invasive coronary angiography with FFR (B), and TAG analyses (E) of a normal left anterior descending coronary artery without stenosis (FFR = 0.93). Note that TAG values are in the same order of magnitude as the patient with an ischemic lesion as depicted in Figure 1. Abbreviations as in Figure 1.
Table 4.
TAG Analyses on a Per-Vessel Basis and Subgroup Analysis for Coronary CTA Significant (DS ≥50%) Vessels
| Average | FFR >0.80 | FFR ≤0.80 | Between FFR Groups, p Value* |
|
|---|---|---|---|---|
| All vessels | 253 | 194 | 59 | |
| TAG, HU × 10 mm−1 | −11.6 ± 13.3 | −11.1 ± 11.8 | −13.5 ± 17.1 | 0.36 |
| TAG-ExC, HU × 10 mm−1 | −11.8 ± 12.8 | −11.4 ± 11.7 | −13.1 ± 15.9 | 0.77 |
| TAG-CCO, 10 mm−1 | −0.039 ± 0.039 | −0.036 ± 0.034 | −0.050 ± 0.051 | 0.03 |
| Coronary CTA DS ≥50% | 104 | 48 | 56 | |
| TAG, HU × 10 mm−1 | −11.3 ± 15.3 | −9.0 ±12.3 | −13.3 ± 17.3 | 0.17 |
| TAG-ExC, HU × 10 mm−1 | −11.6 ± 14.2 | −10.1 ± 11.7 | −12.9 ± 16.0 | 0.36 |
| TAG-CCO, 10 mm−1 | −0.042 ± 0.045 | −0.034 ± 0.037 | −0.049 ± 0.051 | 0.07 |
Values are n or mean ± SD.
The p values are determined using the Mann-Whitney U test.
CCO = corrected contrast opacification; ExC = excluding calcified coronary segments; FFR = fractional flow reserve; HU = Hounsfield units; TAG = transluminal attenuation gradient; other abbreviations as in Table 2.
Figure 3. Scatter Plot Showing the Relations Among TAG, TAG-CCO, and TAG-ExC.
Correlations of TAG, TAG-CCO, and TAG-ExC were highly significant (p < 0.001 for all correlations). Abbreviations as in Figure 1.
Diagnostic accuracy of coronary CTA diameter stenosis and TAG
Table 5 summarizes the diagnostic accuracy of CT parameters. A DS ≥50% was used as a cutoff value for coronary CTA, whereas optimal thresholds for TAG, TAG-ExC, and TAG-CCO were derived from receiver-operating characteristic curve analyses. Diagnostic accuracy of coronary CTA was distinctly superior to any TAG modality. The area under the curve at receiver-operating characteristic analyses for TAG, TAG-ExC, and TAG-CCO did not significantly differ from the line of identity (p > 0.05 for all).
Table 5.
Diagnostic Accuracy (95% CI) of Coronary CTA, TAG, TAG-ExC, and TAG-CCO for Predicting FFR <0.80 on a Per-Patient and -Vessel Basis (Both for All and Coronary CTA-Positive Vessels Only)
| Coronary CTA | TAG, HU × 10 mm−1 |
TAG-ExC, HU × 10 mm−1 |
TAG-CCO, 10 mm−1 |
|
|---|---|---|---|---|
| Per-vessel basis (n = 253) | DS ≥50% | ≤−7.51 | ≤−7.36 | ≤−0.035 |
| Sensitivity, % | 95 (86–99) | 69 (56–81) | 64 (51–76) | 63 (49–75) |
| Specificity, % | 75 (69–81) | 44 (37–52) | 44 (37–51) | 54 (46–61) |
| NPV, % | 98 (94–100) | 83 (74–90) | 80 (71–87) | 83 (75–89) |
| PPV, % | 54 (44–64) | 27 (21–35) | 26 (19–34) | 29 (22–38) |
| Per-patient basis (n = 85) | DS≥50% | ≤−7.51 | ≤−7.36 | ≤−0.035 |
| Sensitivity, % | 100 (100) | 91 (76–98) | 91 (76–98) | 91 (76–98) |
| Specificity, % | 65 (50–78) | 16 (7–29) | 14 (6–26) | 20 (10–33) |
| NPV, % | 100 (100) | 73 (39–94) | 70 (35–93) | 77 (46–95) |
| PPV, % | 65 (50–78) | 42 (31–54) | 41 (30–53) | 43 (31–55) |
| Coronary CTA significant vessels (n = 104) | ≤−7.51 | ≤−3.29 | ≤−0.025 | |
| Sensitivity, % | NA | 70 (56–81) | 84 (72–92) | 77 (64–87) |
| Specificity, % | NA | 52 (37–67) | 33 (20–48) | 44 (30–59) |
| NPV, % | NA | 60 (43–74) | 64 (43–82) | 62 (44–78) |
| PPV, % | NA | 62 (50–75) | 59 (48–70) | 61 (49–73) |
Incremental value of TAG in addition to coronary CTA DS for predicting FFR ≤0.80
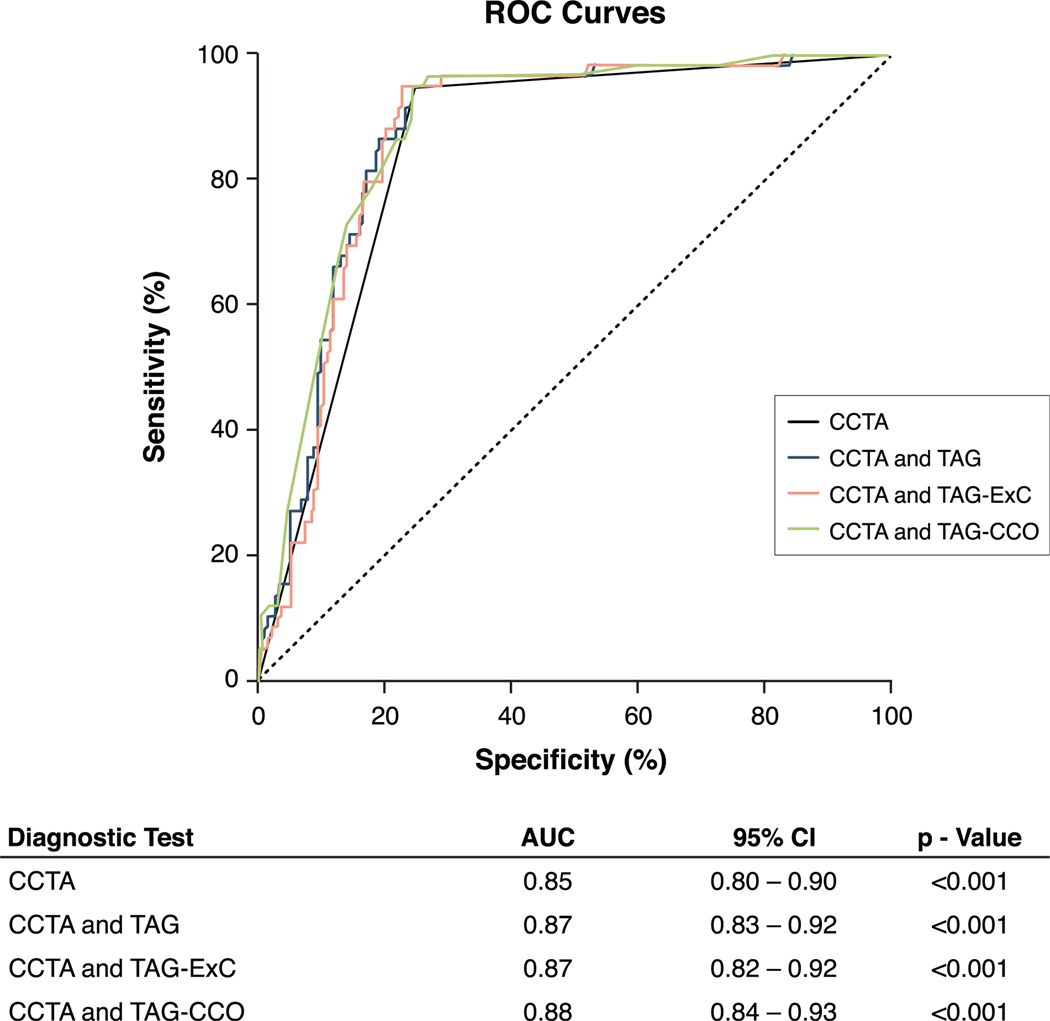
Figure 4 illustrates the incremental value of the TAG parameters to the diagnostic value of coronary CTA DS alone. None of the added TAG parameters raised the area under the curve of coronary CTA DS analysis. Table 6 lists the diagnostic accuracy of coronary CTA in conjunction with each of the TAG modalities and net reclassification indexes. Although differences were minute, TAG-ExC had a significant impact on coronary CTA alone and resulted in 4 correct reclassifications (1.6%) from false positive to true negative (net reclassification improvement index = 0.021, p = 0.046). Net reclassification indexes were not significant for TAG and TAG-CCO.
Figure 4. Diagnostic Performance of Coronary CTA Alone and With TAG, TAG-ExC, and TAG-CCO.
Receiver-operating characteristic (ROC) curve analysis with corresponding area under the curve (AUC) and 95% confidence interval (CI) displaying the diagnostic performance of coronary CTA, coronary CTA and TAG, coronary CTA and TAG-ExC, and coronary CTA and TAG-CCO for the detection of hemodynamically-significant coronary artery disease as indicated by FFR. Abbreviations as in Figure 1.
Table 6.
Incremental Diagnostic Value (95% CI) of TAG in Addition to Coronary CTA for Predicting FFR ≤0.80 on a Per-Vessel Basis (n = 253)
| Coronary CTA + TAG |
Coronary CTA + TAG-ExC |
Coronary CTA + TAG-CCO |
|
|---|---|---|---|
| Sensitivity, % | 95 (86–99) | 95 (86–99) | 95 (86–99) |
| Specificity, % | 76 (69–82) | 77 (71–83) | 76 (69–82) |
| NPV, % | 98 (94–100) | 98 (94–100) | 98 (94–100) |
| PPV, % | 54 (44–64) | 56 (46–66) | 54 (44–64) |
| NRI | 0.005 | 0.021 | 0.005 |
| p value NRI | 0.32 | 0.046 | 0.32 |
Impact of plaque composition on TAG
Figure 5 displays an example of a patient with heavily calcified coronary plaques, potentially hampering reliable TAG analysis. Subgroup analysis according to the presence and severity of plaque calcification is summarized in Table 7 (calcified vs. noncalcified or partially calcified), with additional subgroup analyses for coronary CTA-positive and -negative vessels. Eighty-six of 253 vessels were defined as calcified, whereas 167 vessels were defined as noncalcified or partially calcified. There was no significant difference of TAG, TAG-ExC, or TAG-CCO between vessels with severely calcified plaques and no or partially calcified plaques.
Figure 5. Example of TAG Analysis of a Highly-Calcified RCA.
Coronary CTA (A and C) and cross-sectional images with the region of interest indicated by the green circle (D), invasive coronary angiography with FFR (B), and TAG analyses (E) of a highly calcified right coronary artery (RCA) with a hemodynamically significant stenosis (FFR = 0.27). Note that TAG analyses were comparable and omission of calcified segments did not alter the results. In this patient, TAG did not show a decline in contrast density along the artery despite a severely compromised hyperemic distal pressure. Abbreviations as Figure 1.
Table 7.
Influence of Plaque Composition on TAG
| Coronary CTA Plaque Composition All (n = 253) |
TAG, HU × 10 mm−1 |
TAG-ExC, HU × 10 mm−1 |
TAG-CCO, 10 mm−1 |
|---|---|---|---|
| Calcified (n = 86) | −10.8 ± 14.6 | −10.9 ± 13.0 | −0.040 ± 0.043 |
| Noncalcified/partially calcified (n = 167) | −12.1 ± 12.6 | −12.2 ± 12.7 | −0.039 ± 0.037 |
| p value* | 0.68 | 0.40 | 0.44 |
| Coronary CTA DS ≥50% (n = 104) | −11.4 ± 15.3 | −11.6 ± 14.2 | −0.042 ± 0.046 |
| Calcified (n = 52) | −10.7 ± 17.6 | −11.0 ± 15.5 | −0.042 ± 0.051 |
| Noncalcified/partially calcified (n = 52) | −12.0 ± 12.7 | −12.3 ± 12.9 | −0.042 ± 0.039 |
| p value* | 0.70 | 0.43 | 0.76 |
| Coronary CTA DS ≤50% (n = 149) | −11.8 ± 11.7 | −11.9 ± 11.7 | −0.038 ± 0.034 |
| Calcified (n = 34) | −10.9 ± 8.0 | −10.9 ± 8.0 | −0.037 ± 0.025 |
| Noncalcified/partially calcified (n = 115) | −12.1 ± 12.6 | −12.2 ± 12.6 | −0.038 ± 0.036 |
| p value* | 0.95 | 0.87 | 0.64 |
Intraobserver and interobserver variability for TAG
TAG measurements were stable and reproducible within and between observers in 25 randomly selected vessels. Corresponding intraclass correlation coefficients for single measures were 0.91 (p < 0.001) and 0.85 (p < 0.001) for intraobserver and interobserver variability, respectively.
DISCUSSION
The current study was conducted to evaluate the potential of TAG to assess the hemodynamic consequences of coronary stenoses diagnosed by coronary CTA. The results demonstrate that TAG does not evidently improve the diagnostic accuracy over 256-slice coronary CTA alone to diagnose hemodynamically-significant lesions by ICA/FFR. Exclusion of calcified coronary plaques or correction for arterial phase-dependent contrast density levels between heartbeats during image acquisition did influence TAG results; however, it did not enhance its diagnostic performance on a clinically-relevant basis.
Coronary CTA
Using a DS threshold of 50%, coronary CTA displayed an excellent sensitivity and negative predictive value on a per-vessel and -patient basis, whereas specificity and positive predictive value were moderate at best to diagnose functional CAD. Although numerous studies have evaluated the diagnostic accuracy of coronary CTA (1–3,25), this is one of the few investigations that have systematically used FFR as a reference technique in a prospective manner (9,26). In line with these studies, 35% of patients with a significant angiographic stenosis at coronary CTA did not exhibit functional CAD when evaluated with invasive FFR, whereas not a single patient with a negative coronary CTA displayed functional CAD on ICA. These data confirm the widely regarded notion that coronary CTA can accurately rule out CAD but requires additional functional testing in case of an equivocal or abnormal result.
Transluminal attenuation gradient
In an effort to retrieve functional information from a routine coronary CTA, TAG has been suggested as a method to evaluate the hemodynamic consequences of a coronary lesion and to enhance the diagnostic performance of coronary CTA alone (13,14). The current data, however, did not reveal any differences in TAG values between FFR-positive and -negative lesions. On average, linear regression analysis of the contrast density along a functionally significant coronary stenosis did display a decline of 13.5 ± HU × 10 mm−1 , yet, a physiological density drop in nearly the same order of magnitude was observed in vessels that were not functionally affected (11.1 ± 11.8 HU × 10 mm−1). Such a fall in contrast density along the length of a non-obstructed coronary has previously been documented by the work of Steigner et al. (27), although an exacerbated decline of TAG was observed in patients with a single significant lesion in the left anterior descending coronary artery. As in the current study, reproducibility of measurements was proven to be high and relatively independent of heart rate, body mass index, or cardiac phase. The relatively steep diminution of contrast density distal to a coronary lesion has been linked to a reduction in basal coronary flow (28). To validate this concept, using a 64-slice device, Choi et al. (14) retrospectively selected 126 patients with a chronic total coronary occlusion in ≥1 vessel. The investigators observed a gradual decline in TAG with decreasing TIMI flow rate as observed during ICA, although a large overlap between groups existed. In general, however, such angiographic findings are infrequent in a prospective patient population without a prior cardiac history and an intermediate likelihood for CAD for whom coronary CTA is considered to be most appropriate (29). Thus, such a study design may be suitable to act as a proof of principle, but it yields results that are not applicable to a clinically-relevant cohort of patients. Indeed, in the current study population, only 3 chronic total occlusions with collateral flow were visualized during ICA, and all of the patent arteries displayed TIMI flow grade 3. Subsequently, 2 64-row CT studies have compared TAG with FFR, and similar to the present study, they used an FFR cutoff of 0.80 as a reference standard. Yoon et al. (17) selected 53 patients and, on exclusion of nonevaluable segments, identified 82 arteries of which 32 had a positive FFR. Although statistically significant, the area under the curve for TAG was only 0.63 with an optimal cutoff value of –6.5 HU × 10 mm−1 . In another study, Choi et al. (16) retrospectively selected 65 patients with a positive coronary CTA with matching ICA and FFR measurements where appropriate. In line with Yoon et al. (17), diagnostic accuracy of TAG was moderate at best with an area under the curve of 0.70 and an optimal threshold of –6.5 HU × 10 mm−1 . Nonetheless, there was some incremental value of TAG over coronary CTA alone. These studies, however, were retrospective in nature, biased in patient selection, and excluded nondiagnostic segments. The current study is the first prospective 256-row CT study with an intention to evaluate all segments, irrespective of imaging quality or lesion characteristics. Comparable with the aforementioned studies, optimal TAG cutoff was –7.51 HU × 10 mm−1 , yet the area under the curve did not appreciably diverge from the line of identity. Moreover, TAG did not add incremental value to the diagnostic accuracy of coronary CTA alone. It therefore appears that the previously demonstrated limited value of TAG as observed in retrospective analysis is no longer present in a prospective study design.
Correction temporal nonuniformity of contrast delivery and for coronary calcification
A limitation of the current and the aforementioned studies is that images were obtained using CT equipment that requires multiple heartbeats to cover the entire heart. During post-processing, these images of successive beats are stitched together. Consequently, different segments of the artery from proximal to distal lack temporal uniformity of contrast opacification. To resolve this issue, Chow et al. (15) proposed CCO, whereby intracoronary contrast density is divided by the density level of the descending aorta in the same axial plain. CCO is then defined as the quotient of this value obtained proximal and distal of a coronary lesion. Chow et al. (15) performed a proof-of-concept study using a 64-slice CT in 52 patients selected on the basis of an abnormal coronary CTA. CCO was significantly lower in arteries with impaired resting flow (TIMI flow grade <3 at ICA), but they could not distinguish significantly stenosed from nonsignificantly stenosed vessels in case of TIMI flow grade 3. Choi et al. (16) were subsequently unable to establish an enhanced diagnostic accuracy of CCO over conventional TAG, both of which added no surplus value to coronary CTA. In an effort to optimize results, in the current study, CCO was calculated using linear regression of CCO values along the coronary as employed with TAG (TAG-CCO). Although TAG-CCO was lower in arteries with a positive FFR (–0.036 ± 0.034 × 10 mm−1 vs. –0.050 ± 0.051 × 10 mm−1 , p = 0.03), there was a large overlap between FFR groups, and TAG-CCO did not increase diagnostic accuracy of coronary CTA alone. To circumvent the issue of temporal uniformity, Wong et al. (13) recently used TAG with a single-beat acquisition of a 320-row CT system in a retrospective cohort of patients. They reported a potential incremental value of TAG; clearly, more TAG studies on such devices that acquire the entire heart volume within a single beat are warranted.
It has been suggested that omission of heavily-calcified segments that disrupt the linear regression analysis on which TAG is based may improve results (14). Therefore, TAG analysis excluding these calcified segments was additionally performed. This analysis, however, did not alter the results. In fact, and as depicted in Figure 3, TAG correlated highly with both TAG-ExC and TAG-CCO, and these parameters appeared to be interchangeable. Finally, given the high sensitivity and negative predictive value of coronary CTA, TAG may only be useful in obstructive vessels to enhance the low specificity and positive predictive value. Some of the aforementioned retrospective studies may, in fact, have more accurately identified the obstructive-vessel patients who might benefit from this approach. Subgroup analysis in CT-based abnormal arteries in the current study, however, did not alter the results, and TAG remained unable to discriminate hemodynamically-significant from non–flow-limiting stenoses.
From a theoretical point of view, these observations are not entirely unanticipated. A fall in contrast opacification beyond a stenosis reflects impaired resting flow (27), whereas multiple studies have clearly demonstrated that resting flow remains stable until the point of subtotal coronary occlusion (30–32). Therefore, TAG appears to be most suitable to detect subtotal occlusions with TIMI flow rates <3 or total occlusions with a collateral circulation.
Study limitations
It must be acknowledged that comparison between the current and previous studies on the value of TAG is hampered by differences in scan technology and acquisition. Most studies have used 64-row devices with helical acquisition mode, whereas the current study has used step-and-shoot 256-slice CT. Moreover, initiation of the CT acquisition was triggered by bolus tracking of the descending aorta, whereas previous studies were based on acquisition timing after test bolus tracking. These factors may result in discrepancies of coronary contrast concentrations, which may affect the TAG results. Furthermore, signal magnitude is dependent on tube voltage and milliamperes. Different scan settings between studies may have been influencing factors.
The sample size of the current study was relatively small and, therefore, did not provide definite evidence of the limited additional value of TAG over coronary CTA. Larger studies are needed to provide more insight into this matter. The use of 320-slice or high-pitch dual-source CT equipment will also be pivotal in these studies, overcoming the shortcomings of temporal nonuniformity of contrast delivery by single-beat acquisitions.
With respect to missing FFR values, some assumptions were made. A stenosis of >90% was considered hemodynamically significant, although no FFR was provided. The operator refrained from FFR measurements due to a potential risk of causing pressure wire–related complications. Anatomical lesion severity is known for its inability to provide accurate functional information; however, Tonino et al. (6) showed FFR to be ≤0.80 in 96% of all lesions with a severity of 91% to 99%.
Intracoronary adenosine administration was used in the current study protocol to achieve vasodilation during FFR measurements, whereas intravenous administration of 140 µg/kg/min is generally considered the reference standard (33). Although the utilized dosage of 150 µg intracoronary agrees well with intravenous administration (22), some studies have reported more potent vasodilation with higher doses ranging from 300 to 600 µg that, therefore, may have yielded different results (34,35).
CONCLUSIONS
In the current prospective cohort of patients with an intermediate likelihood for CAD, TAG did not provide incremental diagnostic value over 256-slice coronary CTA alone in assessing the hemodynamic consequences of a coronary stenosis. Correction for temporal nonuniformity of contrast delivery or exclusion of calcified coronary segments slightly enhanced the results, although the clinical impact of these parameters appears to be limited.
Acknowledgments
Dr. Nieman has received research support from Bayer HealthCare, Siemens Medical Solutions, and Abbott Vascular; and speaking fees from Toshiba Medical Systems. Dr. Leipsic has received consulting fees from Heartflow and GE Healthcare. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose. Paolo Raggi, MD, served as Guest Editor for this paper.
ABBREVIATIONS AND ACRONYMS
- CAC
coronary artery calcium
- CAD
coronary artery disease
- CCO
corrected contrast opacification
- CTA
computed tomography angiography
- DS
diameter stenosis
- ExC
excluding calcified coronary segments
- FFR
fractional flow reserve
- HU
Hounsfield units
- ICA
invasive coronary angiography
- TAG
transluminal attenuation gradient
- TIMI
Thrombolysis In Myocardial Infarction
REFERENCES
- 1.Arbab-Zadeh A, Miller JM, Rochitte CE, et al. Diagnostic accuracy of computed tomography coronary angiography according to pre-test probability of coronary artery disease and severity of coronary arterial calcification: the CORE-64 (Coronary Artery Evaluation Using 64-Row Multidetector Computed Tomography Angiography) International Multicenter Study. J Am Coll Cardiol. 2012;59:379–387. doi: 10.1016/j.jacc.2011.06.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52:1724–1732. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 3.Meijboom WB, Meijs MF, Schuijf JD, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol. 2008;52:2135–2144. doi: 10.1016/j.jacc.2008.08.058. [DOI] [PubMed] [Google Scholar]
- 4.Danad I, Raijmakers PG, Harms HJ, et al. Effect of cardiac hybrid 15O-water PET/CT imaging on downstream referral for invasive coronary angiography and revascularization rate. Eur Heart J Cardiovasc Imaging. 2014;15:170–179. doi: 10.1093/ehjci/jet125. [DOI] [PubMed] [Google Scholar]
- 5.Schuijf JD, Wijns W, Jukema JW, et al. Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol. 2006;48:2508–2514. doi: 10.1016/j.jacc.2006.05.080. [DOI] [PubMed] [Google Scholar]
- 6.Tonino PA, Fearon WF, De Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816–2821. doi: 10.1016/j.jacc.2009.11.096. [DOI] [PubMed] [Google Scholar]
- 7.Shreibati JB, Baker LC, Hlatky MA. Association of coronary CT angiography or stress testing with subsequent utilization and spending among Medicare beneficiaries. JAMA. 2011;306:2128–2136. doi: 10.1001/jama.2011.1652. [DOI] [PubMed] [Google Scholar]
- 8.Becker A, Becker C. CT imaging of myocardial perfusion: possibilities and perspectives. J Nucl Cardiol. 2013;20:289–296. doi: 10.1007/s12350-013-9681-7. [DOI] [PubMed] [Google Scholar]
- 9.Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms: results from the prospective multi-center DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol. 2011;58:1989–1997. doi: 10.1016/j.jacc.2011.06.066. [DOI] [PubMed] [Google Scholar]
- 10.Min JK, Koo BK, Erglis A, et al. Usefulness of noninvasive fractional flow reserve computed from coronary computed tomographic angiograms for intermediate stenoses confirmed by quantitative coronary angiography. Am J Cardiol. 2012;110:971–976. doi: 10.1016/j.amjcard.2012.05.033. [DOI] [PubMed] [Google Scholar]
- 11.Bamberg F, Becker A, Schwarz F, et al. Detection of hemodynamically significant coronary artery stenosis: incremental diagnostic value of dynamic CT-based myocardial perfusion imaging. Radiology. 2011;260:689–698. doi: 10.1148/radiol.11110638. [DOI] [PubMed] [Google Scholar]
- 12.Einstein AJ. TAG-is it it? Improving coronary computed tomography angiography with the isotemporal transluminal contrast attenuation gradient. J Am Coll Cardiol. 2013;61:1280–1282. doi: 10.1016/j.jacc.2012.12.027. [DOI] [PubMed] [Google Scholar]
- 13.Wong DT, Ko BS, Cameron JD, et al. Transluminal attenuation gradient in coronary computed tomography angiography is a novel noninvasive approach to the identification of functionally significant coronary artery stenosis: a comparison with fractional flow reserve. J Am Coll Cardiol. 2013;61:1271–1279. doi: 10.1016/j.jacc.2012.12.029. [DOI] [PubMed] [Google Scholar]
- 14.Choi JH, Min JK, Labounty TM, et al. Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. J Am Coll Cardiol Img. 2011;4:1149–1157. doi: 10.1016/j.jcmg.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Chow BJ, Kass M, Gagné O, et al. Can differences in corrected coronary opacification measured with computed tomography predict resting coronary artery flow? J Am Coll Cardiol. 2011;57:1280–1288. doi: 10.1016/j.jacc.2010.09.072. [DOI] [PubMed] [Google Scholar]
- 16.Choi JH, Koo BK, Yoon YE, et al. Diagnostic performance of intracoronary gradient-based methods by coronary computed tomography angiography for the evaluation of physiologically significant coronary artery stenoses: a validation study with fractional flow reserve. Eur Heart J Cardiovasc Imaging. 2012;13:1001–1007. doi: 10.1093/ehjci/jes130. [DOI] [PubMed] [Google Scholar]
- 17.Yoon YE, Choi JH, Kim JH, et al. Noninvasive diagnosis of ischemia-causing coronary stenosis using CT angiography: diagnostic value of transluminal attenuation gradient and fractional flow reserve computed from coronary CT angiography compared to invasively measured fractional flow reserve. J Am Coll Cardiol Img. 2012;5:1088–1096. doi: 10.1016/j.jcmg.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 18.Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med. 1979;300:1350–1358. doi: 10.1056/NEJM197906143002402. [DOI] [PubMed] [Google Scholar]
- 19.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 20.Austen WG, Edwards JE, Frye RL, et al. A reporting system on patients evaluated for coronary artery disease: report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975;51(Suppl 4):5–40. doi: 10.1161/01.cir.51.4.5. [DOI] [PubMed] [Google Scholar]
- 21.Hausleiter J, Meyer T, Hermann F, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301:500–507. doi: 10.1001/jama.2009.54. [DOI] [PubMed] [Google Scholar]
- 22.Casella G, Leibig M, Schiele TM, et al. Are high doses of intracoronary adenosine an alternative to standard intravenous adenosine for the assessment of fractional flow reserve? Am Heart J. 2004;148:590–595. doi: 10.1016/j.ahj.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 23.Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996;334:1703–1708. doi: 10.1056/NEJM199606273342604. [DOI] [PubMed] [Google Scholar]
- 24.Pencina MJ, D’Agostino RB, Sr, D’Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–172. doi: 10.1002/sim.2929. [DOI] [PubMed] [Google Scholar]
- 25.Danad I, Raijmakers PG, Knaapen P. Diagnosing coronary artery disease with hybrid PET/CT: it takes two to tango. J Nucl Cardiol. 2013;20:874–890. doi: 10.1007/s12350-013-9753-8. [DOI] [PubMed] [Google Scholar]
- 26.Meijboom WB, Van Mieghem CA, van Pelt N, et al. Comprehensive assessment of coronary artery stenoses: computed tomography coronary angiography versus conventional coronary angiography and correlation with fractional flow reserve in patients with stable angina. J Am Coll Cardiol. 2008;52:636–643. doi: 10.1016/j.jacc.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 27.Steigner ML, Mitsouras D, Whitmore AG, et al. Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging. 2010;3:179–186. doi: 10.1161/CIRCIMAGING.109.854307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lackner K, Bovenschulte H, Stützer H, Just T, Al-Hassani H, Krug B. In vitro measurements of flow using multislice computed tomography (MSCT) Int J Cardiovasc Imaging. 2011;27:795–804. doi: 10.1007/s10554-010-9728-7. [DOI] [PubMed] [Google Scholar]
- 29.Taylor AJ, Cerqueira M, Hodgson JM, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J AmColl Cardiol. 2010;56:1864–1894. doi: 10.1016/j.jacc.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 30.Uren NG, Melin JA, De Bruyne B, Wijns W, Baudhuin T, Camici PG. Relation between myocardial blood flow and the severity of coronary-artery stenosis. N Engl J Med. 1994;330:1782–1788. doi: 10.1056/NEJM199406233302503. [DOI] [PubMed] [Google Scholar]
- 31.Di Carli M, Czernin J, Hoh CK, et al. Relation among stenosis severity, myocardial blood flow, and flow reserve in patients with coronary artery disease. Circulation. 1995;91:1944–1951. doi: 10.1161/01.cir.91.7.1944. [DOI] [PubMed] [Google Scholar]
- 32.Gould KL, Lipscomb K. Effects of coronary stenoses on coronary flow reserve and resistance. Am J Cardiol. 1974;34:48–55. doi: 10.1016/0002-9149(74)90092-7. [DOI] [PubMed] [Google Scholar]
- 33.Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–224. doi: 10.1056/NEJMoa0807611. [DOI] [PubMed] [Google Scholar]
- 34.Leone AM, Porto I, De Caterina AR, et al. Maximal hyperemia in the assessment of fractional flow reserve: intracoronary adenosine versus intracoronary sodium nitroprusside versus intravenous adenosine: the NASCI (Nitroprussiato versus Adenosina nelle Stenosi Coronariche Intermedie) study. J Am Coll Cardiol Intv. 2012;5:402–408. doi: 10.1016/j.jcin.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 35.López-Palop R, Carrillo P, Frutos A, et al. Comparison of effectiveness of high-dose intracoronary adenosine versus intravenous administration on the assessment of fractional flow reserve in patients with coronary heart disease. Am J Cardiol. 2013;111:1277–1283. doi: 10.1016/j.amjcard.2013.01.270. [DOI] [PubMed] [Google Scholar]