Drug overdose death rates have increased steadily in the United States since 1979. In 2008, a total of 36,450 drug overdose deaths (i.e., unintentional, intentional [suicide or homicide], or undetermined intent) were reported, with prescription opioid analgesics (e.g., oxycodone, hydrocodone, and methadone), cocaine, and heroin the drugs most commonly involved (1). Since the mid-1990s, community-based programs have offered opioid overdose prevention services to persons who use drugs, their families and friends, and service providers. Since 1996, an increasing number of these programs have provided the opioid antagonist naloxone hydrochloride, the treatment of choice to reverse the potentially fatal respiratory depression caused by overdose of heroin and other opioids (2). Naloxone has no effect on non-opioid overdoses (e.g., cocaine, benzodiazepines, or alcohol) (3). In October 2010, the Harm Reduction Coalition, a national advocacy and capacity-building organization, surveyed 50 programs known to distribute naloxone in the United States, to collect data on local program locations, naloxone distribution, and overdose reversals. This report summarizes the findings for the 48 programs that completed the survey and the 188 local programs represented by the responses. Since the first opioid overdose prevention program began distributing naloxone in 1996, the respondent programs reported training and distributing naloxone to 53,032 persons and receiving reports of 10,171 overdose reversals. Providing opioid overdose education and naloxone to persons who use drugs and to persons who might be present at an opioid overdose can help reduce opioid overdose mortality, a rapidly growing public health concern.
Overdose is common among persons who use opioids, including heroin users. In a 2002–2004 study of 329 drug users, 82% said they had used heroin, 64.6% had witnessed a drug overdose, and 34.6% had experienced an unintentional drug overdose (4). In 1996, community-based programs began offering naloxone and other opioid overdose prevention services to persons who use drugs, their families and friends, and service providers (e.g., health-care providers, homeless shelters, and substance abuse treatment programs). These services include education regarding overdose risk factors, recognition of signs of opioid overdose, appropriate responses to an overdose, and administration of naloxone.
To identify local program locations and assess the extent of naloxone distribution, in October 2010 the Harm Reduction Coalition e-mailed an online survey to staff members at the 50 programs then known to distribute naloxone. Follow-up e-mails and telephone calls were used to encourage participation, clarify responses, and obtain information on local, community-based programs. The survey included questions about the year the program began distributing naloxone, the number of persons trained in overdose prevention and naloxone administration, the number of overdose reversals reported, and whether the totals were estimates or based on program data. The survey also asked questions regarding the naloxone formulations currently distributed, any recent difficulties in obtaining naloxone, and the program’s experience with naloxone distribution.
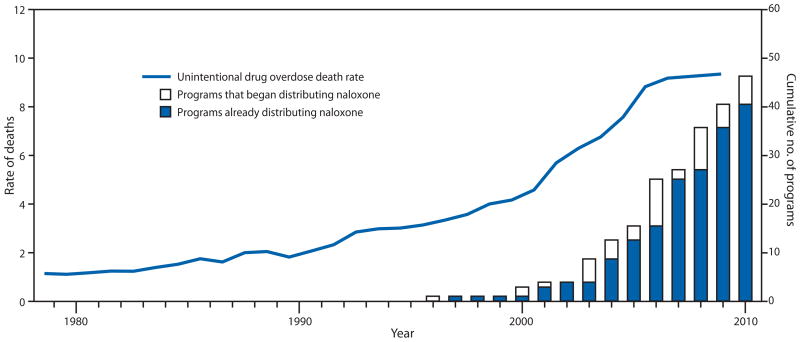
Staff members at 48 (96%) of the 50 programs completed the online survey. Since the first program began distributing naloxone in 1996, through June 2010, the 48 responding programs reported providing training and distributing naloxone to an estimated 53,032 persons (program range: zero to 16,220; median: 102.5; mean: 1,104.8).* From the first naloxone distribution in 1996 through June 2010, the programs received reports of 10,171 overdose reversals using naloxone (range: zero to 2,385; median: 32; mean: 211.9).† During a recent 12-month period, respondents distributed an estimated 38,860 naloxone vials (Table).§ Using data from the survey, the number of programs beginning naloxone distribution each year during 1996–2010 was compared with the annual crude rates of unintentional drug overdose deaths per 100,000 population from 1979 to 2008 (Figure 1) (1).
TABLE.
Number of opioid overdose programs/local programs, naloxone vials provided in a recent 12-month period, program participants overall, and overdose reversals, by program size — United States, 1996–2010
| Program size (by no. of vials of naloxone provided during a recent 12-month period) | No. of program respondents | No. of local programs | No. of naloxone vials provided to participants during a recent 12-month period*
|
No. of program participants from beginning of program through June 2010†
|
Reported opioid overdose reversals from beginning of program through June 2010§
|
|||
|---|---|---|---|---|---|---|---|---|
| No. | (%) | No. | (%) | No. | (%) | |||
| Small <100 | 24 | 24 | 754 | (1.9) | 1,646 | (3.1) | 371 | (3.6) |
| Medium 101–1,000 | 18 | 18 | 5,294 | (13.6) | 13,214 | (24.9) | 3,241 | (31.9) |
| Large 1,001–10,000 | 4 | 74 | 9,792 | (25.3) | 26,213 | (49.4) | 5,648 | (55.5) |
| Very large >10,000 | 2 | 72 | 23,020 | (59.2) | 11,959 | (22.6) | 1,091 | (10.7) |
| Total | 48 | 188 | 38,860 | (100.0) | 53,032 | (100.0) | 10,171 | (100.0) |
Units of naloxone (including number of vials or intranasal doses and refills) distributed to participants during 2009 or July 2009–June 2010. Estimated by 21 program respondents (2,524 units, 6.5% of total) and based on program data for 27 respondents (36,336 units, 93.5%).
Number of participants to whom naloxone was distributed from the start of program through June 2010. Estimated by 29 respondents (14,066 participants, 26.5% of total) and based on program data for 19 respondents (38,966 participants, 73.5%).
Number of opioid overdose reversals reported using the naloxone provided by the program from the start of the program through June 2010. Estimated by 26 respondents (2,582 reversals, 25.4% of total) and based on program data for 22 respondents (7,589 reversals, 74.6%).
FIGURE 1.
Annual crude rates* of unintentional drug overdose deaths and number of overdose prevention programs distributing naloxone — United States, 1979–2010
*Per 100,000 population.
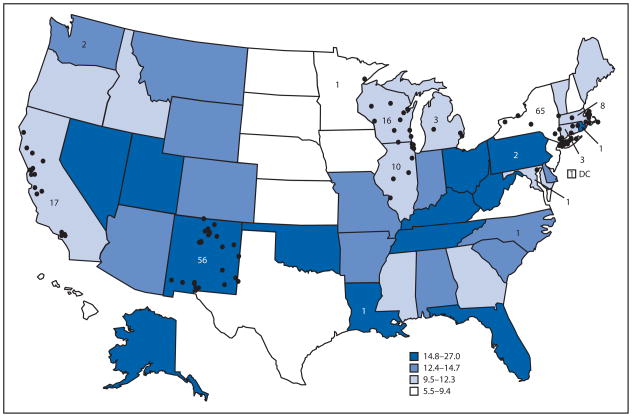
The 48 responding programs were located in 15 states and the District of Columbia. Four responding programs provided consolidated data for multiple local, community-based programs. Three state health departments, in New York, New Mexico, and Massachusetts, provided data for 129 local programs (65, 56, and eight, respectively); a nongovernmental organization in Wisconsin provided data on a statewide operation with 16 local programs. In all, the 48 responding programs provided data for 188 local opioid overdose prevention programs that distributed naloxone (Figure 2). Nineteen (76.0%) of the 25 states with 2008 drug overdose death rates higher than the median and nine (69.2%) of the 13 states in the highest quartile (1) did not have a community-based opioid overdose prevention program that distributed naloxone (Figure 2).
FIGURE 2.
Number (N = 188) and location* of local drug overdose prevention programs providing naloxone in 2010 and age-adjusted rates† of drug overdose deaths§ in 2008 — United States
* Not shown in states with fewer than three local programs.
†Per 100,000 population.
§Source: National Vital Statistics System. Available at http://www.cdc.gov/nchs/nvss.htm. Includes intentional, unintentional, and undetermined.
For a recent 12-month period, the 48 responding programs reported distributing 38,860 naloxone vials, including refills (range: zero to 12,070; median: 97; mean: 809.6).¶ Overdose prevention programs were characterized as small, medium, large, or very large, based on the number of naloxone vials distributed during that period. The six responding programs in the large and very large categories distributed 32,812 (84.4%) of the naloxone vials (Table).
Twenty-one (43.7%) responding programs reported problems obtaining naloxone in the “past few months” before the survey. The most frequently reported reasons for difficulties obtaining naloxone were the cost of naloxone relative to available funding and the inability of suppliers to fill orders.**
Editorial Note
The findings in this report suggest that distribution of naloxone and training in its administration might have prevented numerous deaths from opioid overdoses. Syringe exchange and harm reduction programs for injection-drug users were early adopters of opioid overdose prevention interventions, including providing naloxone (5,6). More noninjection opioid users might be reached by opioid overdose prevention training and (where feasible) provision of naloxone in jails and prisons, substance abuse treatment programs, parent support groups, and physician offices (Maya Doe-Simkins, MPH, Boston Medical Center, personal communication, 2011). Reaching users of prescription opioid analgesics is important because a large proportion of drug overdose deaths have been associated with these drugs (1,7).
Widespread concern about the substantial increases in opioid drug overdose deaths has prompted adoption of various other prevention measures, including 1) education of patients, clinicians, pharmacists, and emergency department staff members; 2) issuing opioid prescribing guidelines; 3) prescription drug monitoring programs; 4) legal and administrative efforts to reduce illegal prescribing; 5) prescription drug take-back programs; and 6) improved access to substance abuse treatment (8,9). Programs such as Project Lazarus and Operation OpioidSAFE in North Carolina include clinicians prescribing naloxone to patients receiving opioid analgesic prescriptions who meet criteria for higher overdose risk (8) (Anthony Dragovich, MD, Womack Army Medical Center, Fort Bragg, North Carolina, personal communication, 2011).
In the United States, naloxone is provided to participants in different ways, including through onsite medical professionals and the use of standing orders. Recognizing the potential value of providing naloxone to laypersons, some states (e.g., California, Illinois, New Mexico, New York, and Washington) have passed laws and changed regulations to provide limited liability for prescribers who work with programs providing naloxone to laypersons. In addition, Washington, Connecticut, New Mexico, and New York have enacted Good Samaritan laws providing protection from arrest in an effort to encourage bystanders at a drug overdose to call 911 and use naloxone when available (9). Because of high overdose mortality among persons who use drugs, the Global Fund to Fight AIDS, Tuberculosis, and Malaria recommends naloxone distribution as a component of comprehensive services for drug users (10).
In this analysis, the majority (76.0%) of the 25 states with 2008 age-adjusted drug overdose death rates higher than the median did not have a community-based opioid overdose prevention program that distributed naloxone. High death rates provide one measure of the extent of drug overdoses; however, the number of deaths also should be considered. For example, in 2008, West Virginia had the highest drug overdose death rate (25.8) in the United States, and Texas (8.6) had one of the lowest. However, the West Virginia rate was based on 459 deaths, whereas the Texas rate was based on 2,053 deaths. States might consider both death rates and number of deaths in their intervention planning.
The findings in this report are subject to at least three limitations. First, other naloxone distribution programs might exist that were unknown to the Harm Reduction Coalition. Second, all data are based on unconfirmed self-reports from the 48 responding programs. Finally, the numbers of persons trained in naloxone administration and the number of overdose reversals involving naloxone likely were underreported because of incomplete data collection and unreported overdose reversals. However, because not all untreated opioid overdoses are fatal, some of the persons with reported overdose reversals likely would have survived without naloxone administration (2).
In this report, nearly half (43.7%) of the responding opioid overdose programs reported problems obtaining naloxone related to cost and the supply chain. Price increases of some formulations of naloxone appear to restrict current program activities and the possibility of new programs. Economic pressures on state and local budgets could decrease funding of opioid overdose prevention activities (Daniel Bigg, Chicago Recovery Alliance, personal communication, 2011). To address the substantial increases in opioid-related drug overdose deaths, public health agencies could consider comprehensive measures that include teaching laypersons how to respond to overdoses and administer naloxone to those in need.
What is already known on this topic?
From 1990 to 2008, drug overdose death rates increased threefold in the United States, and the number of annual deaths increased to 36,450. Opioids (including prescription opioid medications and heroin) are major causes of drug overdose deaths. Naloxone is the standard of care for treatment of potentially fatal respiratory depression caused by opioid overdose.
What is added by this report?
In October 2010, at least 188 local opioid overdose prevention programs that distributed naloxone existed. During 1996–2010, these programs in 15 states and the District of Columbia reported training and providing naloxone to 53,032 persons, resulting in 10,171 drug overdose reversals using naloxone. However, many states with high drug overdose death rates have no opioid overdose prevention programs that distribute naloxone.
What are the implications for public health practice?
To address the high rates of opioid drug overdose deaths, public health agencies could, as part of a comprehensive prevention program, implement community-based opioid drug overdose prevention programs, including training and providing naloxone to potential overdose witnesses, and systematically assess the impact of these programs.
Acknowledgments
Participating opioid overdose programs. Naloxone Overdose Prevention Education Working Group.
Footnotes
The number of participants to whom naloxone was distributed was estimated by 29 responding programs (26.5% of total) and based on program data for 19 respondents (73.5%).
The number of opioid overdose reversals was estimated by 26 responding programs (25.4% of total) and based on program data for 22 respondents (74.6%).
The number of vials distributed to participants during 2009 or July 2009–June 2010 was estimated by 21 program respondents (6.5% of total) and based on program data for 27 respondents (93.5%).
Responding programs provide naloxone for injection in multidose (10 mL) and single-dose (1 mL) vials with concentrations of 0.4 mg/mL. Vials that are adapted for intranasal use (using a mucosal atomization device) are single-dose 2 mL vials with concentration of 1 mg/mL. Typically, respondents provide 1 multidose or 2 single-dose vials in an overdose rescue kit. Forty-two (87.5%) of 48 reported providing only injectable naloxone (63.0% of total vials), four (8.3%) provided only intranasal naloxone (33.1%), and four (8.3%) provided both injectable and intranasal naloxone (3.9%).
The two most commonly reported reasons for difficulties obtaining naloxone were the cost of naloxone relative to available funding (seven responding programs) and inability of suppliers to fill orders (13 respondents). Four respondents reported interruptions because they did not have a qualified medical provider to either order naloxone from suppliers or prescribe naloxone to users. Five reported two of the three reasons for interruptions.
Contributor Information
Eliza Wheeler, Drug Overdose Prevention and Education (DOPE) Project, Harm Reduction Coalition, Oakland.
Peter J. Davidson, Univ of California, San Diego, California.
T. Stephen Jones, T. Stephen Jones Public Health Consulting, Florence.
Kevin S. Irwin, Tufts Univ, Medford, Massachusetts.
References
- 1.CDC. WONDER [Database] Atlanta, GA: US Department of Health and Human Services, CDC; 2012. [Accessed February 13, 2012]. Available at http://wonder.cdc.gov. [Google Scholar]
- 2.Hardman JG, Limbird LE, editors. Goodman and Gilman’s the pharmacologic basis of therapeutics. 11. New York, NY: McGraw-Hill; 2006. pp. 576–8. [Google Scholar]
- 3.Wermeling DP. Opioid harm reduction strategies: focus on expanded access to intranasal naloxone [Editorial] Pharmacotherapy. 2010;30:627–31. doi: 10.1592/phco.30.7.627. [DOI] [PubMed] [Google Scholar]
- 4.Lagu T, Anderson BJ, Stein M. Overdoses among friends: drug users are willing to administer naloxone to others. J Subst Abuse Treat. 2006;30:129–33. doi: 10.1016/j.jsat.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Doe-Simkins M, Walley AY, Epstein A, Moyer P. Saved by the nose: bystander-administered intranasal naloxone hydrochloride for opioid overdose. Am J Public Health. 2009;99:788–91. doi: 10.2105/AJPH.2008.146647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Enteen L, Bauer J, McLean R, et al. Overdose prevention and naloxone prescription for opioid users in San Francisco. J Urban Health. 2010;8:931–41. doi: 10.1007/s11524-010-9495-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young AM, Havens JR, Leukefeld CG. Route of administration for illicit prescription opioids: a comparison of rural and urban drug users. Harm Reduct J. 2010;7:24. doi: 10.1186/1477-7517-7-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Albert S, Brason FW, Sanford CK, Dasgupta N, Graham J, Lovette B. Project Lazarus: community-based overdose prevention in rural North Carolina. Pain Med. 2011;12(Suppl 2):S77–85. doi: 10.1111/j.1526-4637.2011.01128.x. [DOI] [PubMed] [Google Scholar]
- 9.Burris S, Beletsky L, Castagna C, Coyle C, Crowe C, McLaughlin J. Stopping an invisible epidemic: legal issues in the provision of naloxone to prevent opioid overdose. Drexel L Rev. 2009;1:273–340. [Google Scholar]
- 10.The Global Fund to Fight AIDS, Tuberculosis and Malaria. [Accessed on February 13, 2012];Harm reduction for people who use drugs: information note. 2011 Jun; Available at http://www.theglobalfund.org/documents/rounds/11/r11_harmreduction_infonote_en.