Abstract
Background
Although the problem-based learning (PBL) emerged in 1969 and was soon widely applied internationally, the rapid development in China only occurred in the last 10 years. This study aims to compare the effect of PBL and lecture-based learning (LBL) on student course examination results for introductory Chinese undergraduate medical courses.
Methods
Randomized and nonrandomized controlled trial studies on PBL use in Chinese undergraduate medical education were retrieved through PubMed, the Excerpta Medica Database (EMBASE), Chinese National Knowledge Infrastructure (CNKI) and VIP China Science and Technology Journal Database (VIP-CSTJ) with publication dates from 1st January 1966 till 31 August 2014. The pass rate, excellence rate and examination scores of course examination were collected. Methodological quality was evaluated based on the modified Jadad scale. The I-square statistic and Chi-square test of heterogeneity were used to assess the statistical heterogeneity. Overall RRs or SMDs with their 95% CIs were calculated in meta-analysis. Meta-regression and subgroup meta-analyses were also performed based on comparators and other confounding factors. Funnel plots and Egger’s tests were performed to assess degrees of publication bias.
Results
The meta-analysis included 31studies and 4,699 subjects. Fourteen studies were of high quality with modified Jadad scores of 4 to 6, and 17 studies were of low quality with scores of 1 to 3. Relative to the LBL model, the PBL model yielded higher course examination pass rates [RR = 1.09, 95%CI (1.03, 1.17)], excellence rates [RR = 1.66, 95%CI (1.33, 2.06)] and examination scores [SMD = 0.82, 95%CI (0.63, 1.01)]. The meta-regression results show that course type was the significant confounding factor that caused heterogeneity in the examination-score meta-analysis (t = 0.410, P<0.001). The examination score SMD in “laboratory course” subgroup [SMD = 2.01, 95% CI: (1.50, 2.52)] was higher than that in “theory course” subgroup [SMD = 0.72, 95% CI: (0.56, 0.89)].
Conclusions
PBL teaching model application in introductory undergraduate medical courses can increase course examination excellence rates and scores in Chinese medical education system. It is more effective when applied to laboratory courses than to theory-based courses.
Background
The problem-based learning (PBL) teaching model was first developed in 1969, and the approach has since become a popular education model internationally [1,2]. According to World Health Organization data, the PBL teaching model has been used in more than 1,700 medical schools globally, and this number continues to grow [3]. The PBL teaching model was first used in higher medical education settings in China in the 1980s. Due to current shifts in approaches to medical education prevalent in China, this model has been extensively applied as an experimental teaching method in Chinese medical schools. The annual number of published Chinese studies focusing the application of PBL teaching methods has increased exponentially from 14 in 2000 to 474 in 2011.
The PBL teaching model is still controversial [4,5]. Numerous studies have found that in medical education settings, relative to traditional, lecture-based learning (LBL) models, the PBL model presents certain advantages with respect to improving student abilities in inactive learning, two-way communication, clinical thinking, and teamwork [6–9]. A study by Abraham et al. suggested that physiology teaching outcomes could be improved through the use of the PBL teaching model [6]. A study by Mehadizadeh et al. demonstrated that anatomy students that had been instructed via PBL teaching methods not only achieved higher examination scores, but were also highly satisfied with this teaching method [8]. Furthermore, a study by the University of Missouri School of Medicine revealed that overtime, the PBL teaching model may improve the passing rate of the United States Medical Licensing Examination [9]. However, other researchers do not consider the PBL teaching model to be superior to the LBL teaching model with respect to the acquisition of theoretical and fundamental knowledge [10–15].
PBL teaching reforms in China have largely been applied to clinical courses, and these reforms have affected levels of teaching effectiveness in similar ways as they have in other countries [16–18]. However, a systematic, quantitative assessment of the outcomes of PBL teaching model application during learning stages of introductory medical courses has not yet been conducted. For this study, meta-analysis methods were applied to compare the effects of PBL and LBL teaching models on course examination results of introductory undergraduate medical courses in China, thereby providing a scientific basis for evaluating the necessity and feasibility of PBL application in such courses.
Methods
Inclusion and exclusion criteria
For this study, we used the following definition of PBL provided by Kinkade [19]: a curriculum of carefully selected activities that test the learner’s critical knowledge acquisition, problem-solving, self-directed learning, and team-participation capacities. Students work in small groups, generate hypotheses about the given case and learning objectives, work outside of class hours to fulfill learning objectives, and then reconvene and solve the problem.
Studies included in this review met the following inclusion criteria: 1) examination of PBL use as a teaching method for five-year undergraduate medical curricula applied in Chinese medical schools; and 2) use of randomized or nonrandomized controlled trials (RCTs), in which experimental groups were instructed using either the PBL teaching model alone or using the PBL teaching model in combination with the traditional LBL teaching model while control groups were instructed strictly based on the LBL teaching model. Courses for which PBL was applied were introductory medical courses in physiology, biochemistry, pharmacological, anatomy, medical statistics, etc. Course examinations were used to assess study populations, and data on examination results were reported.
We excluded studies that did not include a control group; that examined postgraduate or other non-undergraduate courses; that involved non-introductory postgraduate medical courses in internal medicine, surgery, diagnostics and clinical practice; and that did not cite objective course examination data and republished studies.
Search strategy
To identify relevant studies, we searched for publications using the following databases from the earliest available date through 31 August of 2014: PubMed (1st January 1966), the Excerpta Medica Database (EMBASE) (1st January 1966), the China Knowledge Resource Integrated Database (China National Knowledge Infrastructure, CNKI http://www.cnki.net/, 1st January 1979) and the VIP China Science and Technology Journal Database (VIP-CSTJ, http://oldweb.cqvip.com, 1st January 1979). The search terms “PBL,” “problem-based learning,” “based on problems,” “active learning,” and “learner centered” were used to identify PBL studies, and these were combined with other key terms such as “medical,” “undergraduate,” “Chinese,” and “China.” We also manually searched through the reference lists of retrieved articles to trace potentially relevant papers.
Data extraction and quality assessment
Literature screening was independently performed by two reviewers (L.Z. and X.L.) in accordance with the inclusion and exclusion criteria; the data were then extracted and cross-checked. Data extraction in consistencies were resolved through discussion, and secondary calculations found during data extraction were resolved in consultation with a third reviewer (Y.Z.).The extracted data included general study information(the title, author name, publication year and literature resources); basic study characteristics (the number of experimental and control groups, participant characteristics, course name and type, study type, intervention process, literature quality assessment characteristics; etc.)and outcomes (the number of “excellent,” “pass” and “fail” scores, or experimental and control group examination sores).On a 100-point scale, “excellent” denotes a score of≥80 points, “pass” denotes a score of≥60 points and “fail” denotes a score of<60 points.
Methodological quality assessments of the included studies were independently performed by two researchers using the modified Jadad scale [20]. The scale included eight items: randomization, blinding, withdrawals, dropouts, inclusion/exclusion criteria, adverse effects and statistical analysis (Table 1). The total score for each article ranged from 0 to 8 and was computed by summing the score of each item. Low quality studies wielded scores of 0 to 3, and high quality studies achieved scores of 4 to 8.
Table 1. The modified Jadad scale.
| Eight items | Answer | Score |
|---|---|---|
| Was the study described as randomized? | Yes | +1 |
| No | 0 | |
| Was the method of randomization appropriate? | Yes | +1 |
| No | -1 | |
| Not described | 0 | |
| Was the study described as blinding? a | Yes | +1 |
| No | 0 | |
| Was the method of blinding appropriate? | Yes | +1 |
| No | -1 | |
| Not described | 0 | |
| Was there a description of withdrawals and dropouts? | Yes | +1 |
| No | 0 | |
| Was there a clear description of the inclusion/exclusion criteria? | Yes | +1 |
| No | 0 | |
| Was the method used to assess adverse effects described? | Yes | +1 |
| No | 0 | |
| Was the methods of statistical analysis described? | Yes | +1 |
| No | 0 |
a: double-blind got 1 score, single-blind got 0.5 score.
Statistical methods
The outcome measures of this study were course examination results, which were given two expression forms. The first was a dichotomous outcome (“excellent”, “pass” or “fail” evaluation), and the other was a continuous outcome (i.e., examination scores).
RevMan version 5.3 (Cochrane Collaboration, Copenhagen, Denmark) and the meta-analysis module included in Stata 11.0 (College Station, Texas 77845 USA)were utilized for the meta-analysis. The analytical statistics of relative risk (RR) and standardized mean difference (SMD) at 95% confidence intervals (95% CIs)were used to determine the teaching effectiveness of the PBL model for dichotomous and continuous outcomes, respectively. Before the study results were combined, the I-square statistic and Chi-square test of heterogeneity were used to assess the statistical heterogeneity of the included studies. Values of I2>50% or P<0.10 were considered to exhibit significant heterogeneity across studies. The total RR or SMD score at 95% CI was calculated using a random-effects model when heterogeneous results appeared. Otherwise, a fixed-effects model was used.
Meta-regression was used to examine the confounding factors’ effect. Confounding factors included the following: degree major, teaching pattern, course type, PBL group tutor scale, study type and modified Jadad score. We also performed subgroup meta-analyses based on these confounding factors. For the subgroup analysis based on teaching patterns, two subgroups based on whether the PBL teaching model was used independently for the experimental group were used. For one subgroup, the comparator was PBL vs. LBL, and the PBL teaching model was used independently for the experimental group. In the other subgroup, the comparator was PBL+LBL vs. LBL, and both PBL and LBL teaching models were used for the experimental group. We utilized funnel plots and Egger’s tests to assess the degree of publication bias both graphically and statistically. A sensitivity analysis was performed by exchanging the combined model (fixed effects model and random effects model).
Results
Literature search results
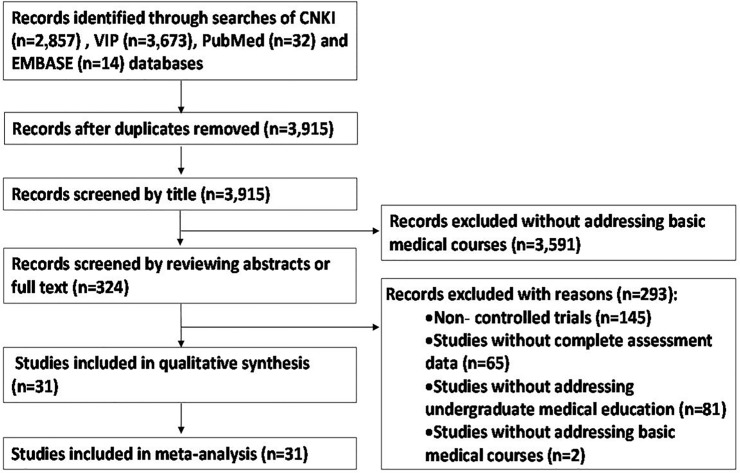
Using the literature search method, a total of 3,915 relevant studies were initially retrieved. After reviewing the titles, abstracts, and full texts of these studies, 3,884 studies were excluded, and 31 studies were used for the qualitative synthesis and meta-analysis [21–51]. The literature screening process and results are depicted in Fig 1.
Fig 1. Literature screening process and results.
General study characteristics
The general characteristics of the included studies are shown in Table 2. The 31 studies cover 14 disciplines, including clinical medicine, integrative Chinese and western medicine, and pharmaceutical science. Of fifteen courses examined, including those in anatomy, biochemistry, physiology, etc., six are laboratory-based[23,26,31,36,42,50], and 25 are theory-based[21,22,24,25,27–30,32–35,37–41,43–49,51]. Ten of the studies are RCT-based[27,28,31,37,39,43,46,49–51], and the other 21 are non-RCT-based[21–26,29,30,32–36,38,40–42,44,45,47,48].Research subjects included in the studies are freshman to junior-year college students. A total of 4,699 students were included in this meta-analysis, including 2,450 students in the experimental group and 2,249 students in the control group.
Table 2. Basic characteristics of the included studies.
| ID | Included study | Study time | Study type | Major | Course name | Course type | Number of cases (E/C) | Pattern(E/C) | Tutor scale inPBL group | Grade of students | Course hour in experimental group (PBL/LBL) | Course hour in control group | Outcome | Modified Jadad score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Ma 2005[21] | 2004 | non-RCT | Preventive medicine Pharmacy | Physiology | Theory course | 54/53 | PBL+LBL/LBL | One tutor in each group | Sophomore | NA/NA | NA | ES | 3 |
| 2 | Zhang 2005[22] | 2003 | non-RCT | Diagnostic imaging | Pharmacology | Theory course | 30/30 | PBL+LBL/LBL | One tutor in all groups | NA | 6/30 | 36 | ES | 3 |
| 3 | Chen R 2006[23] | 2005 | non-RCT | Clinical medicine | Pathophysiology | Laboratory Course | 35/33 | PBL /LBL | One tutor in all groups | Sophomore | 5/- | 5 | PR, ER | 3 |
| 4 | Chen S 2006[24] | 2005 | non-RCT | Clinical medicine | Physiology | Theory course | 174/169 | PBL+LBL/LBL | One tutor in all groups | Sophomore | 8/NA | NA | ES | 2 |
| 5 | Lv 2006[25] | 2005 | non-RCT | Stomatology | Medical physics | Theory course | 58/56 | PBL+LBL/LBL | One tutor in all groups | Freshman | NA/NA | NA | ES | 3 |
| 6 | Cui 2007[26] | 2006 | non-RCT | Clinical medicine | Biochemistry | Laboratory Course | 32/36 | PBL /LBL | One tutor in all groups | Sophomore | NA/- | NA | PR, ER | 3 |
| 7 | Lu 2007[27] | 2005 | RCT | Biomedical engineering | Biochemistry | Theory course | 70/35 | PBL /LBL | One tutor in each group | Sophomore | NA/- | NA | ES | 5 |
| 8 | Qi 2007[28] | 2004–2005 | RCT | Clinical medicine | Histology and embryology | Theory course | 97/100 | PBL /LBL | One tutor in all groups | Freshman | NA/- | NA | ES | 4 |
| 9 | Qin 2007[29] | 2005 | non-RCT | Clinical medicine | Physiology | Theory course | 148/158 | PBL+LBL/LBL | One tutor in all groups | Sophomore | NA/NA | NA | PR, ER | 3 |
| 10 | Liu 2008[30] | 2006 | non-RCT | Anesthesiology, Medical Imaging | Medical advanced mathematics | Theory course | 72/68 | PBL /LBL | One tutor in all groups | Freshman | NA/- | NA | ES | 4 |
| 11 | Wang 2008[31] | 2006 | RCT | Clinical medicine | Medical statistics | Laboratory Course | 36/36 | PBL /LBL | One tutor in all groups | Juniors | NA/- | NA | PR | 5 |
| 12 | Dai 2009[32] | 2008 | non-RCT | Clinical medicine | Pathology | Theory course | 42/40 | PBL/LBL | One tutor in all groups | Juniors | NA/- | NA | ES | 3 |
| 13 | Deng 2009[33] | 2007 | non-RCT | Clinical medicine | Laboratory diagnosis | Theory course | 40/40 | PBL /LBL | One tutor in all groups | NA | NA/- | NA | PR | 3 |
| 14 | Luo 2009[34] | 2006 | non-RCT | Medical Laboratory Science | Biochemistry | Theory course | 56/58 | PBL+LBL/LBL | One tutor in all groups | Sophomore | NA/NA | NA | ES | 3 |
| 15 | Shen 2009[35] | 2006 | non-RCT | Medical English | Pathophysiology | Theory course | 30/29 | PBL /LBL | One tutor in all groups | Sophomore | 3/- | NA | ES | 3 |
| 16 | Xu 2009[36] | 2007 | non-RCT | Clinical medicine | Pathology | Laboratory Course | 49/49 | PBL /LBL | One tutor in all groups | Juniors | NA/- | NA | PR, ER | 3 |
| 17 | Zhou 2009[37] | 2007 | RCT | Clinical medicine | Anatomy | Theory course | 100/100 | PBL+LBL/LBL | One tutor in all groups | Freshman | NA/NA | NA | PR, ER | 3 |
| 18 | Zhang 2010[38] | 2006–2008 | non-RCT | Clinical medicine | Medical statistics | Theory course | 39/39 | PBL+LBL/LBL | One tutor in all groups | Juniors | 8/32 | 40 | PR, ER | 4 |
| 19 | Cui 2011[39] | 2010 | RCT | Pharmacy | Pharmacology | Theory course | 51/48 | PBL+LBL/LBL | One tutor in each group | Juniors | NA/NA | NA | ES | 3 |
| 20 | Huang 2011[40] | 2011 | non-RCT | Chinese medicine | Physiology | Theory course | 68/64 | PBL+LBL/LBL | One tutor in all groups | Sophomore | NA/NA | NA | ES | 4 |
| 21 | Liu 2011[41] | 2010 | non-RCT | Integrative Chinese and western medicine | Biochemistry | Theory course | 91/70 | PBL+LBL/LBL | One tutor in all groups | Sophomore | NA/NA | NA | ES | 4 |
| 22 | Song 2011[42] | 2010 | non-RCT | Integrative Chinese and western medicine | Pharmacology | Laboratory Course | 63/63 | PBL /LBL | One tutor in all groups | Juniors | 10/- | 10 | ES | 4 |
| 23 | Tian 2011[43] | 2009 | RCT | Clinical medicine | Evidence-based medicine | Theory course | 46/50 | PBL /LBL | One tutor in all groups | Juniors | NA/- | NA | ES | 6 |
| 24 | Wu 2011 [44] | 2009 | non-RCT | Integrative Chinese and western medicine | Histology | Theory course | 100/100/100 | PBL/PBL+LBL /LBL | One tutor in all groups | Freshman | NA/- | NA | ES | 3 |
| 25 | Xing 2011[45] | 2009 | non-RCT | Obstetrics and gynecology | Laboratory diagnosis | Theory course | 57/55 | PBL+LBL/LBL | One tutor in all groups | Juniors | NA/NA | NA | ES | 4 |
| 26 | Yang 2012[46] | 2011 | RCT | Clinical medicine | Immunology | Theory course | 256/238 | PBL+LBL/LBL | One tutor in all groups | Sophomore | NA/NA | NA | PR, ER | 5 |
| 27 | Yan 2013[47] | 2011 | non-RCT | Orthopsychiatry | Pathology | Theory course | 57/53 | PBL+LBL/LBL | One tutor in all groups | Juniors | NA /NA | NA | ES | 3 |
| 28 | He 2014[48] | 2012 | non-RCT | Clinical medicine | Biochemistry | Theory course | 92/91 | PBL+LBL/LBL | One tutor in all groups | Sophomore | NA/NA | NA | PR, ER | 3 |
| 29 | Qiu 2014[49] | 2012 | RCT | Clinical medicine | Human developmental genetics | Theory course | 124/126 | PBL/LBL | One tutor in all groups | Sophomore | NA/- | NA | ES | 5 |
| 30 | Yin 2014[50] | 2012 | RCT | Rehabilitation medicine | Anatomy | Laboratory Course | 32/32 | PBL/LBL | One tutor in all groups | Freshman | NA/- | NA | ES | 4 |
| 31 | Zhao 2014[51] | 2009 | RCT | Clinical medicine | Pharmacology | Theory course | 151/130 | PBL+LBL/LBL | One tutor in all groups | Sophomore | NA/NA | NA | PR, ER | 5 |
E/C: E mean experimental group, C mean control group
Pattern: teaching pattern, PBL mean PBL teaching model alone in experimental group, PBL+LBL mean PBL+LBL teaching model in combination in experimental group, LBL mean LBL teaching model in control group
Outcome: PR mean pass rate, ER mean excellent rate, ES mean examination score
NA: Not Applicable
Among the 31 studies that were included in the meta-analysis, experimental groups examined in14 of these studies adopted the complete PBL teaching model [23,26–28,30–33,35,36,42,43,49,50], and experimental groups examined in 16 of the studies adopted the mixed PBL+LBL teaching model [21,22,24,25,29,34,37–41,45–48,51]. One of the studies considered two experimental groups [44], with one applying the complete PBL teaching model while the other applied the mixed PBL+LBL teaching model. The control groups used in all 31studies applied the LBL teaching model. In all of the studies, the PBL teaching model was only applied for one semester. While class schedule data were collected, several studies did not provide information on class hours. Outcome measurements were largely collected toward the end of each class. Assessment tools applied were largely tests designed by the researchers themselves.
Eleven studies disclosed the number of "pass" and “fail" grades collected for final course examinations[23,26,29,31,33,36–38,46,48,51], nine of which also reported the number of “excellent” grades collected[23,26,29,36–38,46,48,51]. In total, 23studies disclosed numerical examination scores for final course examinations[21,22,24,25,27,28,30,32,34,35,38–47,49–51]. Of these 23 studies, three reported on the number of “excellent,” "pass" and “fail" grades collected [38,46,51].
Evaluation of the methodological quality of the included studies
The 31studies examined were evaluated using the modified Jadad scale. From on this assessment, 17studies (54.8%) were assigned scores of 2 or 3[21–26,29,32–37,39,44,47,48], and 14studies (45.2%) were assigned scores of 4, 5 or 6[27,28,30,31,38,40–43,45,46,49–51]. The mean modified Jadad scale score was 3.6, and the standard deviation was 0.9. The modified Jadad scores collected for each study are shown in Table 3.
Table 3. Modified Jadad scores of the included studies.
| ID | Included study | Was the research described as randomized? # | Was the approach of randomization appropriate?* | Was the research described as blinding? # | Was the approach of blinding appropriate? * | Was there a presentation of withdrawals and dropouts? # | Was there a presentation of the inclusion/exclusion criteria? # | Was the approach used to assess adverse effects described? # | Was the approach of statistical analysis described? # | total |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Ma 2005[21] | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 3 |
| 2 | Zhang 2005[22] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 3 |
| 3 | Chen R 2006[23] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 3 |
| 4 | Chen S 2006[24] | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 2 |
| 5 | Lv 2006[25] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 3 |
| 6 | Cui 2007[26] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 3 |
| 7 | Lu 2007[27] | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| 8 | Qi 2007[28] | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
| 9 | Qin 2007[29] | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 3 |
| 10 | Liu 2008[30] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 |
| 11 | Wang 2008[31] | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 5 |
| 12 | Dai 2009[32] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 3 |
| 13 | Deng 2009[33] | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 3 |
| 14 | Luo 2009[34] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 3 |
| 15 | Shen 2009[35] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 3 |
| 16 | Xu 2009[36] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 3 |
| 17 | Zhou 2009[37] | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 3 |
| 18 | Zhang 2010[38] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 |
| 19 | Cui 2011[39] | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 3 |
| 20 | Huang 2011[40] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 |
| 21 | Liu 2011[41] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 |
| 22 | Song 2011[42] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 |
| 23 | Tian 2011[43] | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| 24 | Wu 2011 [44] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 3 |
| 25 | Xing 2011[45] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 |
| 26 | Yang 2012[46] | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| 27 | Yan 2013[47] | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 3 |
| 28 | He 2014[48] | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 3 |
| 29 | Qiu 2014[49] | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| 30 | Yin 2014[50] | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 |
| 31 | Zhao 2014[51] | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
#: “1” means “Yes”, “0” means “No”;
*: “1” means “Yes”, “0” means “Not described”
Meta-analysis results
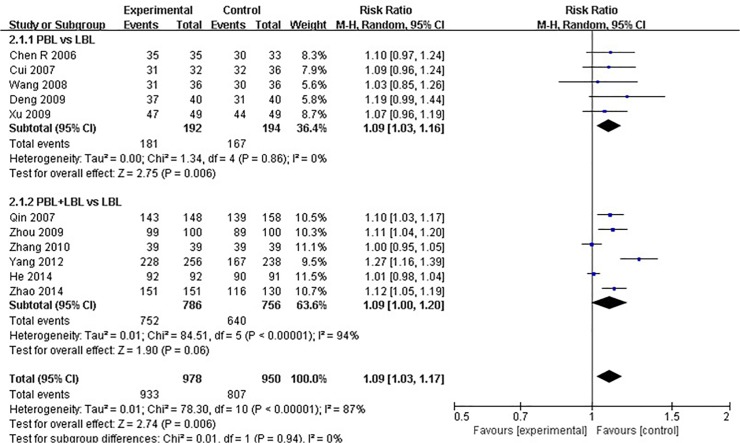
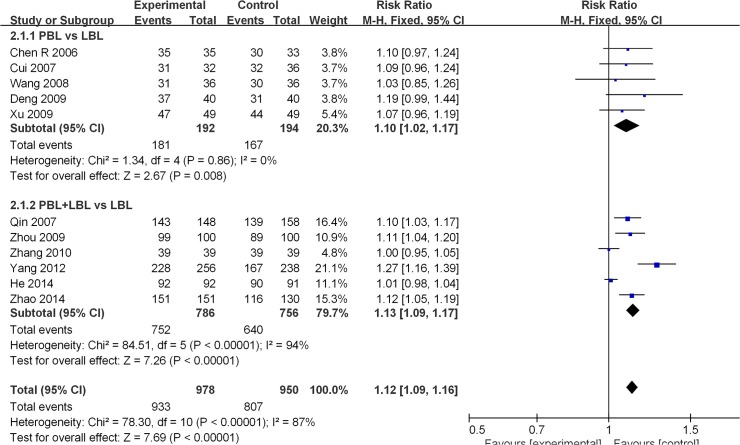
Eleven studies disclosed pass rate data [23,26,29,31,33,36–38,46,48,51]. The average experimental group pass rate was 95.4% [95%CI: (94.1%, 96.7%)], and that of control group was 84.9% [95%CI: (82.6%, 87.2%)] (Table 4). Because a significant degree of heterogeneity was observed across all of the11 studies (I2 = 87%, P<0.001),a random effects model was utilized for the meta-analysis. The analytical results reveal that the experimental group produced higher course examination pass rates than the LBL control group [RR: 1.09, 95% CI: (1.03, 1.17)] (Fig 2). For studies that compared PBL and LBL methods, the average PBL group passing rate was 94.3% [95%CI: (91.0%, 97.6%)], and that of the LBL group was 86.1% [95%CI: (81.2%, 91.0%)] (Table 4). No heterogeneity was observed across these studies (I2 = 0%, P = 0.860), and the analytical results reveal that the PBL model produces higher course examination passing rates than the traditional teaching model [RR: 1.09, 95% CI: (1.03, 1.16)] (Fig 2). Among studies that conducted PBL+LBL vs. LBL comparisons, the average PBL+LBL group passing rate was 95.7% [95%CI: (94.3%, 97.1%)], and that of the LBL group was 82.7%[95%CI: (82.1%, 87.3%)] (Table 4). Due to the presence of heterogeneity across these studies (I2 = 94%, P<0.001), a random effects model was utilized for the meta-analysis. The analytical results reveal that the PBL+LBL model did not produce a significantly higher course examination passing rate than the traditional teaching model [RR: 1.09, 95% CI: (1.00, 1.20)](Fig 2).
Table 4. The average pass rate and average excellent rate of experimental group and control group.
| PBL pattern | Average Pass rate (95%CI) | Average Excellent rate (95%CI) |
|---|---|---|
| PBL vs. LBL | ||
| Experimental group | 94.3% (91.0%-97.6%) | 59.5% (50.5%-68.3%) |
| Control group | 86.1% (81.2%-91.0%) | 30.5%(22.2%-38.8%) |
| PBL+LBL vs. LBL | ||
| Experimental group | 95.7% (94.3%-97.1%) | 50.4% (46.9%-53.9%) |
| Control group | 84.7% (82.1%-87.3%) | 31.2% (27.9%-34.5%) |
| Total | ||
| Experimental group | 95.4% (94.1%-96.7%) | 51.6% (48.3%-54.9%) |
| Control group | 84.9% (82.6%-87.2%) | 31.1% (28.0%-34.2%) |
Fig 2. Forest plot of PBL experimental group and LBL control group course pass rates (random effects model).
Events: “pass” events, M-H: Mantel-Haenszel, PBL:PBL teaching model independently applied to the experimental group, PBL+LBL: PBL+LBL teaching models applied to the experimental group, LBL: LBL teaching model applied to the control group.
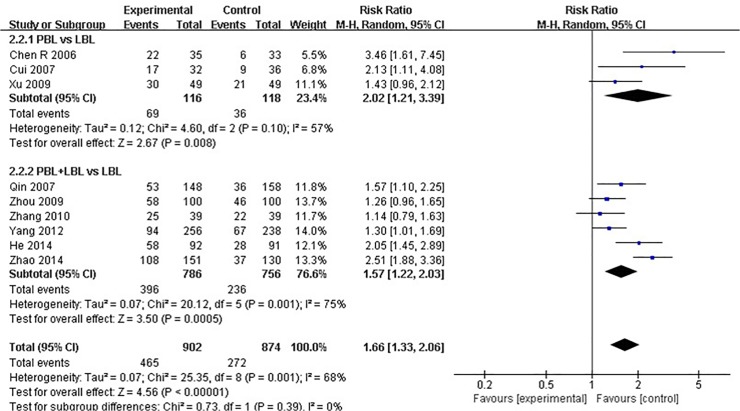
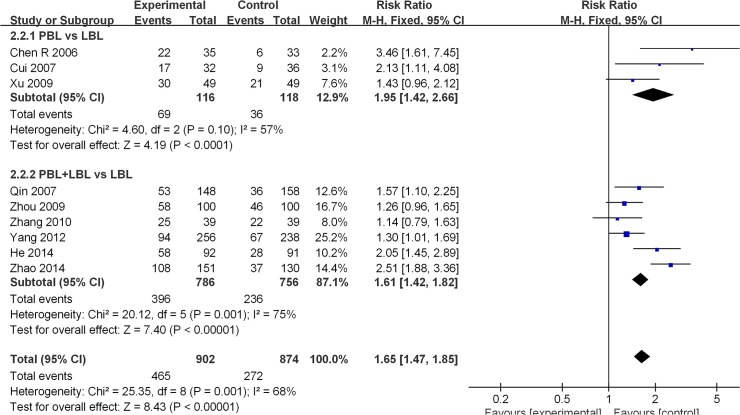
Nine of the included studies [23,26,29,36–38,46,48,51] reported course examination excellence rates (≥80 score). The average experimental group pass rate was 51.6% [95%CI: (48.3%, 54.9%)], and that of the control group was 31.1% [95%CI: (28.0%, 34.2%)] (Table 4). A moderate degree of heterogeneity was observed across all nine studies (I2 = 68%, P = 0.001). A random effects model was utilized for the meta-analysis, and the analytical results reveal that the experimental group produced a significantly higher course examination excellence rate than the LBL control group [RR: 1.66, 95% CI: (1.33, 2.06)] (Fig 3).Among studies that conducted PBL vs. LBL comparisons, the average PBL group excellence rate was 59.5% [95%CI: (50.5%, 68.3%)], and that of the LBL group was 30.5% [95%CI: (22.2%, 38.8%)] (Table 4). A moderate degree of heterogeneity was detected across these studies (I2 = 57%, P = 0.10), and random effects model results reveal that the PBL model generated higher course examination excellence rates than the traditional teaching model [RR: 2.02, 95% CI: (1.21, 3.39)] (Fig 3). Among studies that conducted PBL+LBL vs. LBL comparisons, the average PBL+LBL group excellence rate was 50.4% [95%CI: (46.9%, 53.9%)], and that of the LBL group was 31.2% [95%CI: (27.9%, 34.5%)] (Table 4). A moderate degree of heterogeneity was also observed (I2 = 75%, P = 0.001), and the analytical results reveal that the PBL+LBL model produces higher course examination excellence rates than the traditional teaching model [RR: 1.57 95% CI: (1.22, 2.03)] (Fig 3).
Fig 3. Forest plot of PBL experimental group and LBL control group course excellence rates (random effects model).
Events: “excellence” events, M-H: Mantel-Haenszel, PBL: PBL teaching model independently applied to the experimental group, PBL+LBL: PBL+LBL teaching models applied to the experimental group, LBL: LBL teaching model applied to the control group.
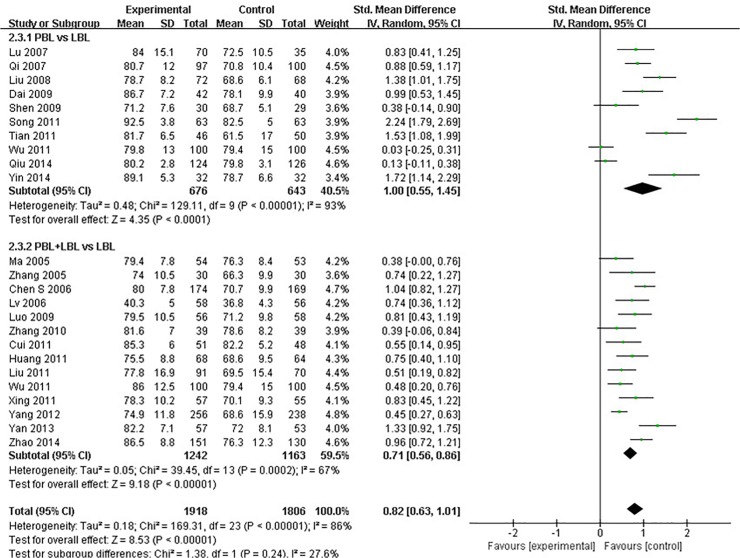
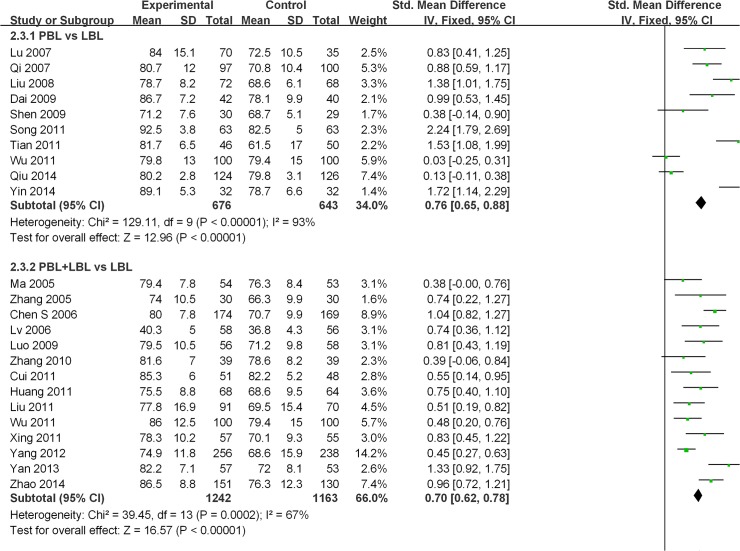
Twenty-three of the studies examined [21,22,24,25,27,28,30,32,34,35,38–47,49–51] reported course examination scores. A high degree of heterogeneity was observed across all of these studies (I2 = 86%, P<0.001), and a random effects model was utilized for the meta-analysis. The analytical results reveal that the experimental group produced significantly higher examination scores than the LBL control group [SMD: 0.82, 95% CI: (0.63, 1.01)] (Fig 4).Among studies that conducted PBL vs. LBL comparisons, a high degree of heterogeneity was found (I2 = 93%, P<0.001). A random effects model was used for the meta-analysis, and the analytical results reveal that PBL methods produce significantly higher course examination scores than traditional teaching methods [SMD: 1.00, 95% CI: (0.55, 1.45)] (Fig 4). Among studies that conducted PBL+LBL vs. LBL comparisons, a moderate degree of heterogeneity was observed (I2 = 67%, P<0.001).Random-effects model results reveal that PBL+LBL methods produce significantly higher course examination scores than traditional teaching methods [SMD: 0.71, 95% CI: (0.56, 0.86)] (Fig 4).
Fig 4. Forest plot of PBL experimental group and LBL control group course examination scores (random effects model).
IV: inverse variance, PBL: PBL teaching model independently applied to the experimental group, PBL+LBL: PBL+LBL teaching models applied to the experimental group, LBL: LBL teaching model applied to the control group.
A meta-regression was performed because a relatively high degree of heterogeneity between the included studies was found. The following confounding factors that were considered: degree major, teaching pattern, course type, PBL group tutor scale, study type and modified Jadad score. Among the three outcomes, we discovered that course type is the significant confounding factor that causes examination-score meta-regression heterogeneity (t = 0.410, P<0.001) (Table 5).To further examine heterogeneity from confounding factors, we performed a subgroup meta-analysis based on the following factors: degree major, course type, PBL group tutor scale, study type and modified Jadad score. For most of the subgroups, heterogeneity has not been eliminated. However, for the “laboratory course” subgroup, we did not detect heterogeneity through our meta-analysis of pass rates (I2 = 0%, P = 0.950).As well, heterogeneity was not identified through our meta-analysis of “laboratory course” subgroup examination scores (I2 = 49%, P = 0.160)or of the substantial heterogeneity group(I2 = 18%, P = 0.300). The subgroup examination-score meta-analysis also revealed that the difference in SMD levels between the “theory course”[SMD: 0.72, 95% CI: (0.56, 0.89)] and “laboratory course” subgroups [SMD: 2.01, 95% CI: (1.50, 2.52)]is statistically significance (P<0.001).The examination score SMD value between experimental and control groups for the “laboratory course” subgroup was found to be higher than that of the “theory course” subgroup (Table 6).
Table 5. Meta-regression of the effects of confounding factors on pass rate, excellent rate and examination score.
| Outcome | Factor | Coefficient (95%CI) | std. error | t | P |
|---|---|---|---|---|---|
| Pass Rate | |||||
| Major | - | - | - | - | |
| Pattern | 0.014(-0.103–0.132) | 0.051 | 0.280 | 0.787 | |
| Course type | -0.033(-0.156–0.089) | 0.053 | -0.620 | 0.550 | |
| Tutor scale in PBL group | - | - | - | ||
| Study type | -0.069(-0.162–0.025) | 0.041 | -1.690 | 0.129 | |
| Modified Jadad score | 0.037(-0.015–0.09) | 0.023 | 1.630 | 0.142 | |
| Excellent Rate | |||||
| Major | - | - | - | - | |
| Pattern | -0.231(-0.865–0.403) | 0.268 | -0.860 | 0.417 | |
| Course type | 0.231(-0.403–0.865) | 0.268 | 0.860 | 0.417 | |
| Tutor scale in PBL group | - | - | - | ||
| Study type | 0.069(-0.508–0.647) | 0.244 | 0.280 | 0.785 | |
| Modified Jadad score | -0.005(-0.331–0.322) | 0.138 | -0.030 | 0.974 | |
| Examination Score | |||||
| Major | 0.042(-0.203–0.288) | 0.119 | 0.360 | 0.724 | |
| Pattern | -0.272(-0.706–0.163) | 0.210 | -1.300 | 0.209 | |
| Course type | 1.291(0.637–1.944) | 0.315 | 4.100 | 0.000 | |
| Tutor scale in PBL group | 0.273(-0.391–0.937) | 0.320 | 0.850 | 0.402 | |
| Study type | -0.04(-0.508–0.429) | 0.226 | -0.180 | 0.862 | |
| Modified Jadad score | 0.081(-0.154–0.316) | 0.113 | 0.710 | 0.483 | |
Table 6. Subgroup meta-analyses based on confounding factors.
| Pass Rate | Excellent Rate | Examination Score | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of studies | Sample size(T/C) | Number of events (T/C) | Weight(%) | I2(%) | P of heterogeneity | RR(95% CI) | P of effect | Number of studies | Sample size (T/C) | Number of events (T/C) | Weight(%) | I2(%) | P of heterogeneity | RR(95% CI) | P of effect | Number of studies | Sample size(T/C) | Weight(%) | I2(%) | P of heterogeneity | SMD(95% CI) | P of effect | |
| Major | |||||||||||||||||||||||
| Clinical medicine | 11 | 978/950 | 933/807 | 100 | 87 | <0.001 | 1.09 (1.03–1.17) | 0.006 | 9 | 902/874 | 465/272 | 100 | 68 | 0.001 | 1.66 (1.33–2.06) | <0.001 | 8 | 929/892 | 34.8 | 88 | <0.001 | 0.78 (0.49–1.07) | <0.001 |
| Integrative Chinese and western medicine | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | 4 | 354/333 | 17.3 | 96 | <0.001 | 0.80 (0.03–1.56) | 0.040 | ||
| Others | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | 12 | 635/581 | 47.9 | 68 | <0.001 | 0.86 (0.65–1.07) | <0.001 | ||
| Pattern | |||||||||||||||||||||||
| PBL vs LBL | 5 | 192/194 | 181/167 | 36.4 | 0 | 0.860 | 1.09 (1.03–1.16) | 0.006 | 3 | 116/118 | 69/36 | 23.4 | 57 | 0.100 | 2.02 (1.21–3.39) | 0.008 | 10 | 676/643 | 40.5 | 93 | <0.001 | 1.00 (0.55–1.45) | <0.001 |
| PBL+LBL vs LBL | 6 | 786/756 | 752/640 | 63.6 | 94 | <0.001 | 1.09 (1.00–1.20) | 0.060 | 6 | 786/756 | 396/236 | 76.6 | 75 | 0.001 | 1.57 (1.22–2.03) | <0.001 | 14 | 1242/1163 | 59.5 | 67 | <0.001 | 0.71 (0.56–0.86) | <0.001 |
| Course type | |||||||||||||||||||||||
| Theory course | 7 | 826/796 | 789/671 | 69.4 | 93 | <0.001 | 1.10 (1.01–1.21 | 0.030 | 6 | 786/756 | 396/236 | 76.6 | 75 | 0.001 | 1.57(1.22–2.03) | <0.001 | 22 | 1823/1711 | 92.7 | 81 | <0.001 | 0.72 (0.56–0.89) | <0.001 |
| Laboratory course | 4 | 152/154 | 144/136 | 30.6 | 0 | 0.950 | 1.08 (1.01–1.15) | 0.020 | 3 | 116/118 | 69/36 | 23.4 | 57 | 0.100 | 2.02 (1.21–3.39) | 0.008 | 2 | 95/95 | 7.3 | 49 | 0.160 | 2.01 (1.50–2.52)* | <0.001 |
| Tutor scale in PBL group | |||||||||||||||||||||||
| One tutor in each group | 0 | - | - | - | - | - | 0 | - | - | - | - | - | 3 | 175/136 | 12.2 | 18 | 0.300 | 0.57 (0.32–0.83) | <0.001 | ||||
| One tutor in all groups | 11 | 978/950 | 933/807 | 100 | 87 | <0.001 | 1.09 (1.03–1.17) | 0.006 | 9 | 902/874 | 465/272 | 100 | 68 | 0.001 | 1.66 (1.33–2.06) | <0.001 | 21 | 1743/1670 | 87.8 | 88 | <0.001 | 0.85 (0.65–1.06) | <0.001 |
| Study Type | |||||||||||||||||||||||
| RCT | 4 | 543/504 | 509/402 | 36 | 66 | 0.030 | 1.14 (1.06–1.24) | <0.001 | 3 | 507/468 | 260/150 | 41 | 86 | <0.001 | 1.60 (1.04–2.45) | 0.030 | 8 | 827/759 | 33.9 | 88 | <0.001 | 0.84 (0.52–1.16) | <0.001 |
| Non-RCT | 7 | 435/446 | 424/405 | 64 | 75 | <0.001 | 1.06 (1.00–1.12) | 0.050 | 6 | 395/406 | 205/122 | 59 | 53 | 0.060 | 1.69 (1.30–2.19) | <0.001 | 16 | 1091/1047 | 66.1 | 86 | <0.001 | 0.81 (0.56–1.05) | <0.001 |
| Modified Jadad score | |||||||||||||||||||||||
| <4 | 7 | 496/507 | 484/455 | 63.2 | 74 | <0.001 | 1.08 (1.02–1.15) | 0.010 | 6 | 456/467 | 238/146 | 61 | 51 | <0.001 | 1.69 (1.33–2.15) | <0.001 | 11 | 752/736 | 45.4 | 80 | <0.001 | 0.67 (0.43–0.92) | <0.001 |
| ≥4 | 4 | 482/443 | 449/352 | 36.8 | 93 | <0.001 | 1.10 (0.95–1.29) | 0.210 | 3 | 446/407 | 227/126 | 39 | 87 | <0.001 | 1.56 (0.96–2.52) | 0.070 | 13 | 1166/1070 | 5406 | 90 | <0.001 | 0.94 (0.66–1.23) | <0.001 |
| Total | 11 | 978/950 | 933/807 | 100 | 87 | <0.001 | 1.09 (1.03–1.17) | 0.006 | 9 | 902/874 | 465/272 | 100 | 68 | 0.001 | 1.66 (1.33–2.06) | <0.001 | 24 | 1918/1806 | 100 | 86 | <0.001 | 0.82 (0.63–1.01) | <0.001 |
*: The Examination Score SMD of “Laboratory course” subgroup is higher than “theory course” subgroup, P<0.001.
Publication bias
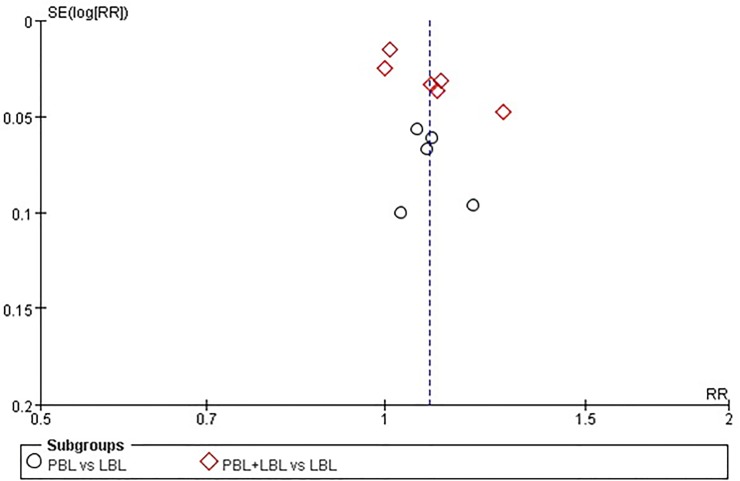
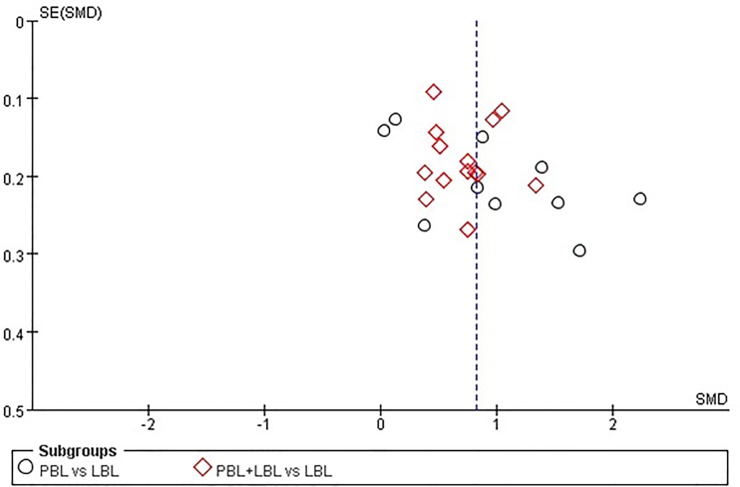
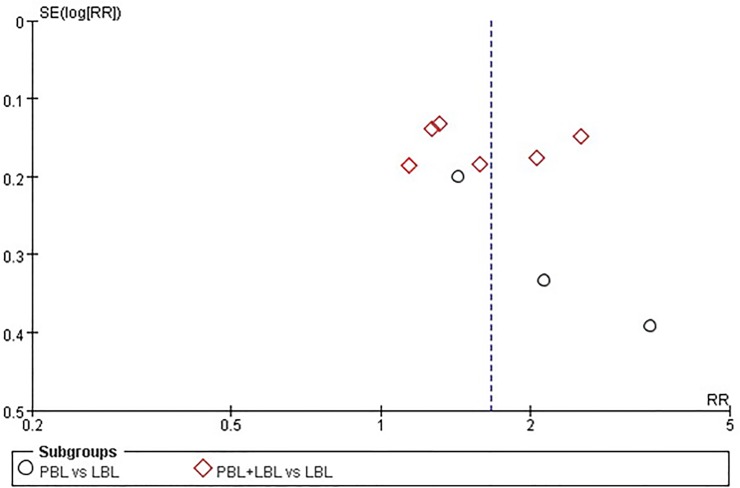
The pass rate, excellence rate and examination score funnel plots do not reveal a significant degree of publication bias between the included studies (Figs 5–7). However, publication bias Egger’s test results reveal a minor degree of publication bias among pass rate (t = 2.310, P = 0.050) and examination score (t = 2.130, P = 0.045) results (Table 7).
Fig 5. Funnel plot of the meta-analysis of PBL experimental group and LBL control group course pass rates.
Fig 7. Funnel plot of the meta-analysis of PBL experimental group and LBL control group course examination score.
Table 7. Egger’s test of pass rate, excellent rate and examination score for publication bias.
| Outcome | Number of studies | coefficient of bias (95%CI) | std. error | t | P |
|---|---|---|---|---|---|
| Pass Rate | 11 | 2.123(0.004–4.243) | 0.919 | 2.310 | 0.050 |
| Excellent Rate | 9 | 2.307(-2.406–7.019) | 1.993 | 1.160 | 0.285 |
| Examination Score | 24 | 3.700(0.093–7.307) | 1.739 | 2.130 | 0.045 |
Fig 6. Funnel plot of the meta-analysis of PBL experimental group and LBL control group course excellence rates.
Sensitivity analysis
A sensitivity analysis was performed by changing the combined model from a random effects model to a fixed effects model. The results of the fixed effects model were consistent with those of the random effects model (Figs 8–10).
Fig 8. Forest plot of PBL experimental group and LBL control group course excellence rates (fixed effects model).
Events: “excellence” events, M-H: Mantel-Haenszel, PBL: PBL teaching model independently applied to the experimental group, PBL+LBL: PBL+LBL teaching models applied to the experimental group, LBL: LBL teaching model applied to the control group.
Fig 10. Forest plot of PBL experimental group and LBL control group course examination scores (fixed effects model).
IV: inverse variance, PBL: PBL teaching model independently applied to the experimental group, PBL+LBL: PBL+LBL teaching models applied to the experimental group, LBL: LBL teaching model applied to the control group.
Fig 9. Forest plot of PBL experimental group and LBL control group course excellence rates (fixed effects model).
Events: “excellence” events, M-H: Mantel-Haenszel, PBL: PBL teaching model independently applied to the experimental group, PBL+LBL: PBL+LBL teaching models applied to the experimental group, LBL: LBL teaching model applied to the control group.
Discussion
Since its first application in Canada in the late 1960s, PBL has been widely adopted innumerous universities internationally. As in China, education systems in various regions and countries differ considerably from those of the U.S. Furthermore, cultural differences influence the effectiveness of PBL methods [52]. Therefore, the target population must be limited to Chinese students of the Chinese education system in order to examine the potential effectiveness of the PBL teaching model in China. Our research method will serve as a valuable reference for researchers based in countries of differing cultural backgrounds who wish to evaluate the effectiveness of the PBL teaching model. Our research conclusions will promote PBL teaching model application in countries of differing cultural characteristics.
The results of our meta-analysis indicate that the PBL teaching model can yield significantly positive results relative to the LBL teaching model, particularly in excellence rates and examination scores, which is inconsistent with the previous finding that PBL students either perform no differently or slightly worse than students in conventional on measures of knowledge such as basic sciences examinations [53–55]. Considering the differences in higher medical education between China and the West [56], we speculate that the results may be due to the following reasons. In the PBL teaching model, students play a major role in the process of teaching, and teachers facilitate the student learning and support that learning through experimentation, clinical cases, and seminars. The PBL teaching model is rather different from the traditional LBL teaching model in which students often passively accept their teachers’ knowledge. Chinese students have accepted the LBL teaching model for more than 10 years, starting with their primary education, and the PBL teaching model is a novelty that has greatly stimulated students’ interest in learning. [56] Most Chinese medical universities prefer using uniform textbooks for all students, which is quite different from the United States and other Western countries where no uniform textbooks or standard formats of lectures for medical universities exist. [56] In our study, students in the PBL group used the same textbook as students in the LBL group, and they appeared to be better at active learning, which led them to earn more positive examination results. Conversely, the use of the PBL teaching method in Chinese medical higher education is still in its infancy, and the evaluation of the effectiveness of the PBL teaching method is still relatively unsophisticated, particularly for basic medical education. Both teachers and students emphasize course exams [56]; Chinese students’ keen pursuit of positive test scores helps them excel on exams.
The “course type” subgroup analysis shows that the PBL teaching model is more effective when applied in laboratory class settings than in theory-based class settings. Generally speaking, laboratory class exams focus more on execution and analytical skills [23,26,31,36,42,50,53]. The PBL teaching model can inspire students to engage in proactive learning and thinking initiatives, facilitating a stronger grasp of experimental processes and logic. Consequently, students may acquire a deeper understanding of experiments that they conduct, thus enabling them to produce higher quality experimental reports [23]. Therefore, the PBL teaching model would be best applied for laboratory course examinations. On the other hand, while theory courses in several schools also utilize the PBL teaching model, due to limitations on teaching conditions, students are divided into groups but are remain in one classroom, and the number of students in a single classroom can exceed 100 [24,29,37,44,46,49,51]. In contrast, laboratory courses are typically conducted in small groups, which is more suitable for PBL teaching model adoption [23, 26,31,36,42,50,57]. Hence, the advantages of the PBL teaching model relative to the LBL teaching model are more evident when considering laboratory courses.
A number of researchers believe that utilizing a combination of PBL and LBL teaching models for introductory medical courses may improve teaching effectiveness because while the PBL teaching model boosts student initiative and improves proactive learning abilities, the LBL teaching model improves student comprehension of structural knowledge systems and student tendencies to review material after class [44][45]. Our results show that while applying PBL and LBL teaching models in combination can increase excellence rates and examination scores relative to applications of the LBL teaching model alone, there is no evidence that the former approach is more effective than the latter. A detailed review of the studies examined shows that all 17 courses that adopt both PBL and LBL teaching models are theory courses [21,22,24,25,29,34,37–41,44–48,51]. Due to limitations on teaching conditions, teachers can only apply PBL teaching methods when teaching certain modules, and thus the LBL teaching model is still used for remaining classes. As a result, less than half of the lessons conducted over an entire course apply PBL teaching methods. Of the courses that adopt the PBL teaching model exclusively[23,26–28,30–33,35,36,42–44,49,50], 40% (6/15) are laboratory courses[23,26,31,36,42,50]. As mentioned above, laboratory courses may be more suitable for PBL teaching model adoption. Therefore, applying a combination of PBL and LBL teaching models did not result in superior teaching effectiveness relative to the exclusive application of PBL teaching methods.
Study limitations
Because our study only focuses on undergraduate Chinese medicine higher education, the conclusions may be most applicable to circumstances in China and Asia. Furthermore, this study only evaluated test results—objective outcomes—and it did not assess student attitudes about the PBL and LBL models because these subjective outcomes were not “objectively” measured in the original studies. We also decided to omit a description of subjective outcomes and include only objective outcomes.
The overall quality of the included studies was not high. The mean modified Jadad score for the included studies was only 3.6, and 54.8% of the studies showed modified Jadad scores of less than 4. This study on the effectiveness of the PBL teaching model was also not completely randomized or conducted through double-blind trials. Among the 10 studies on RCT, only two described processes used for randomization sequence generation. These issues may have resulted in low modified Jadad scores and information bias. Higher quality studies on RCT must be examined to better assess the effect of PBL teaching methods.
The three indicators analyzed in this meta-analysis all exhibited marked degrees of heterogeneity. The high heterogeneity may be attributable to the variations in PBL implementation procedures, varying degrees of difficulty in examinations and varying levels of teaching quality among the included studies. Although meta-regression and subgroup meta-analyses were performed, much of the heterogeneity in the subgroup was not eliminated. Heterogeneity among PBL methods is a challenge inherent of all PBL research [13]. Understandings of PBL differ considerably between researchers [58] (e.g., PBL and LBL teaching model teaching hours, course examination methods, etc.). Unfortunately, most of the studies examined did not include detailed information on these factors. Therefore, a random-effect model was applied as the meta-regression model in this study. The heterogeneity maybe affected the reliability of the conclusions of this meta-analysis to some extent.
This study also presents a slight degree of publication bias. Though we conducted a search for literature through the PubMed and EMBASE databases, no non-Chinese studies listed on these databases meet the inclusion criteria. We did not perform a grey literature search, which may have generated information on publication bias. The fixed-effect and random-effect model analysis results of the sensitivity analysis are consistent. This indicates that the analysis results of this research are robust and reliable to a certain degree.
Conclusions
PBL teaching model application in introductory undergraduate medical courses can increase course examination excellence rates and scores in Chinese medical education system,. The PBL teaching model is more effective when applied in laboratory course settings than when applied in theory-based course settings.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by Natural Science Foundation of China (No. 81202286), Research Projects of Teaching Reform of Postgraduate Education in Chongqing, China (No. yjg123101) and Research Projects of Teaching Reform of Higher Education in Chongqing, China (No. 133118). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Jones RW. Problem-based learning: description, advantages, disadvantages, scenarios and facilitation. Anaesth Intensive Care. 2006;34:485–488. [DOI] [PubMed] [Google Scholar]
- 2. McParland M, Noble LM, Livingston G. The effectiveness of problem-based learning compared with traditional teaching in undergraduate psychiatry. Med Educ. 2004;38:859–867. [DOI] [PubMed] [Google Scholar]
- 3. Liu Y, Fan X. On PBL teaching model in Chinese medical education. Journal of Liaoning Medical University (Social Science Edition). 2007;5:33–35. [Google Scholar]
- 4. Farrow R, Norman G. The effectiveness of PBL: the debate continues. Is meta-analysis helpful? Med Educ.2003; 37:1131–1132. [DOI] [PubMed] [Google Scholar]
- 5. Schmidt HG, Cohen-Schotanus J, Arends LR. Impact of problem-based, active learning on graduation rates for 10 generations of Dutch medical students. Med Educ. 2009;43:211–218. 10.1111/j.1365-2923.2008.03287.x [DOI] [PubMed] [Google Scholar]
- 6. Abraham RR, Vinod P, Kamath MG, Asha K, Ramnarayan K. Learning approaches of undergraduate medical students to physiology in a non-PBL and partially PBL-oriented curriculum. Adv Physiol Educ. 2008;32:35–37. 10.1152/advan.00063.2007 [DOI] [PubMed] [Google Scholar]
- 7. Chou FH, Chin CC. Experience of problem-based learning in nursing education at Kaohsiung Medical University. Kaohsiung J Med Sci. 2009;25:258–263. 10.1016/S1607-551X(09)70071-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mahdizadeh M, Kermanian F, Iravani S, Markazi Moghaddam N, Shayan S. Comparing lecture and problem-based learning methods in teaching limb anatomy to first year medical students. Iran J Med Educ.2008; 2:379–388. [Google Scholar]
- 9. Enarson C. Cariaga-LoL: Influence of curriculum type on student performance in the United States Medical Licensing Examination Step 1 and Step 2 exams: problem-based learning vs. lecture-based curriculum. Med Educ. 2001;35:1050–1055. [DOI] [PubMed] [Google Scholar]
- 10. Vernon DT, Blake RL. Does problem-based learning work? A meta-analysis of evaluative research. Acad Med. 1993;68:550–563. [DOI] [PubMed] [Google Scholar]
- 11. Iputo JE, Kwizera E. Problem-based learning improves the academic performance of medical students in South Africa. Med Educ. 2005;39:388–393. [DOI] [PubMed] [Google Scholar]
- 12. Schmidt HG, Cohen-Schotanus J, Arends LR. Impact of problem-based, active learning on graduation rates for 10 generations of Dutch medical students. Med Educ. 2009;43:211–218. 10.1111/j.1365-2923.2008.03287.x [DOI] [PubMed] [Google Scholar]
- 13. Gerald CK, Hoon EK, Mee LW, David K. The effects of problem-based learning during medical school on physician competency: a systematic review. CMAJ. 2008;178:34–41. 10.1503/cmaj.070565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Antepohl W, Herzig S. Problem-based learning versus lecture-based learning in a course of basic pharmacology: A controlled, randomised study. Med Educ. 1999;33:106–113. [DOI] [PubMed] [Google Scholar]
- 15. Tavakol M, Dennick R, Tavakol S. A descriptive study of medical educators’ views of problem-based learning. BMC Med Educ.2009; 4:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guo WC, Xu LX, Gao YC, Feng WJ. Meta-analysis of study on problem-based learning and lecture-based learning applied in clinical clerkship. Journal of Baotou Medical College.2009; 25:90–92. [Google Scholar]
- 17. Zha GY, Pan LP, Zhang JL. Meta-analysis of effectiveness of PBL teaching on stomatology in China. China Higher Medical Education. 2012;1:110–113. [Google Scholar]
- 18. Wang ZY. Meta-analysis of learning effect of PBL teaching on medical students. China Higher Medical Education. 2001;5:80–82. [Google Scholar]
- 19. Kinkade S. A snapshot of the status of problem-based learning in US medical schools, 2003–04. Acad Med. 2005;80:300–301. [DOI] [PubMed] [Google Scholar]
- 20. Oremus M, Wolfson C, Perrault A, Demers L, Momoli F, et al. Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer’s disease drug trials. Dement Geriatr Cogn Disord. 2001;12:232–236 [DOI] [PubMed] [Google Scholar]
- 21. Ma SF, Guan SD. An experimental study on PBL combined LBL applied to physiology teaching. Researches in Medical Education.2005; 4:155–157. [Google Scholar]
- 22. Zhang HF, Zhou LW, Shen C. Application of problem-based learning in pharmacology teaching. Northwest Medical Education. 2005;13:415–416. [Google Scholar]
- 23. Chen R, Zou P. Application and effect evaluation of PBL teaching on pathophysiology experiment courses. Journal of Shanxi Medical University (Preclinical Medical Education Edition). 2006;8:633–634. [Google Scholar]
- 24. Chen SG, Peng LJ. Application of PBL teaching method on physiology teaching. Journal of Xiangnan University (Medical Sciences). 2006;8:71–72. [Google Scholar]
- 25. Lv L, Zhang ZH, Li YZ, Zhao RH, Fan YY. Application of PBL combined LBL on physics teaching. China Higher Medical Education. 2006;10:65–68. [Google Scholar]
- 26. Cui BQ, Li CM, He ZY, Lin YZ. Application of PBL teaching method on biochemistry experiment courses. China Higher Medical Education. 2007;1:7–8. [Google Scholar]
- 27. Lu XM, Wang YT, Yu Y. Primary application of PBL teaching method on biochemistry teaching. China Journal of Modern Medicine. 2007;13:2430–2432. [Google Scholar]
- 28. Qi YF, Pei LX. Comparative study of PBL teaching model on histology and embryology. Journal of Heze Medical College. 2007;19:95–96. [Google Scholar]
- 29. Qin W, Pan GS, Chen YS, Liu AD, Xiao Z. Application of problem-based teaching method on physiology. Modern Medicine & Health. 2007;10:23 [Google Scholar]
- 30. Liu T, Meng XY. Application of PBL teaching method on medical advanced mathematics teaching. Journal of Mathematical Medicine. 2008;21:636–637. [Google Scholar]
- 31. Wang PY, Xie SY. Application of problem-based learning in experimental teaching of medical statistics for medical undergraduates. Researches in Medical Education. 2008;7:932–634. [Google Scholar]
- 32. Dai XW. Application of PBL teaching method on pathology teaching. Modern Journal of Integrated Traditional Chinese and Western Medicine. 2009;18:4459–4460. [Google Scholar]
- 33. Deng AM, Zhu P, Zhou Y, Chen SX. Application of PBL teaching mode in laboratory diagnosis teaching. Researches in Medical Education. 2009;8:1127–1129. [Google Scholar]
- 34. Luo XJ, Mo XR. The application of PBL model in teaching of clinical biochemistry. Researches in Medical Education. 2009;8:74–75. [Google Scholar]
- 35. Shen W, Sui L, Zhang LY, Cheng Y. Application of PBL based on clinical case discussion on pathophysiology teaching. Journal of Shanxi Medical University (Preclinical Medical Education Edition). 2009;11:270–271. [Google Scholar]
- 36. Xu AF, Guo JL. Study and practice of problem-based learning (PBL) teaching method in experimental teaching of pathology. China Higher Medical Education. 2009;2:114–115. [Google Scholar]
- 37. Zhou B, Wen M, Li HW, Yu ZJ, He YH, et al. Application of the problem-based learning methods in anatomy education. Research in Medical Education. 2009;8:7–8. [Google Scholar]
- 38. Zhang YQ, Wang WC, Liu L, Wu YZ, Yi D. The preliminary study of problem-based learning teaching reform on medical statistics. Research in Medical Education. 2010;9:1697–1699. [Google Scholar]
- 39. Cui GZ, Zhong PR, He X, Zhang SZ. Application of PBL teaching method on pharmacology teaching. National Medical Frontiers of China.201; 6:90–91. [Google Scholar]
- 40. Huang XP, Deng BX, Zeng H, Tang B, Yan XX. Application of problem-based learning (PBL) in physiology teaching. Chinese Medicine Modern Distance Education of China. 2011;9:53–54. [Google Scholar]
- 41. Liu XC, Wang HL, Qi XD, Wang SY, Sun XJ, et al. Exploration of PBL teaching model application on biochemistry teaching. China Modern Medicine.2011;18:128–131. [Google Scholar]
- 42. Song XL. Exploration of PBL teaching method on experimental teaching of pharmacology. Chinese Medicine Modern Distance Education of China. 2011;9:82–83. [Google Scholar]
- 43. Tian JH, Liu AP, Shen XP, Yang KH. Evaluation on effectiveness of PBL in evidence-based medicine teaching. Chinese Journal of Evidence-Based Medicine. 2011;11:39–43. [Google Scholar]
- 44. Wu YS, Peng GJ, Yin SG. Application of PBL and LBL teaching methods on histology teaching. Guide of China Medicine. 2011;9:333–334. [Google Scholar]
- 45. Xing Y, Yang XJ, Cheng JH, Qu Y. Exploratory application of combination of LBL and PBL on experimental diagnostics teaching. Journal of Qiqihar University of Medicine. 2011;49:83–88. [Google Scholar]
- 46. Yang J, Fu N, Deng Q, Zhou Z, Zhan S. Application of LBL combined with PBL in the teaching of medical immunology. China Higher Medical Education. 2012;12:104–106. [Google Scholar]
- 47. Yan C, Wei H. Application of PBL in traditional pathology education. Health Vocational Education. 2013;31:112–113. [Google Scholar]
- 48. He Z, Li L, Xu X, Dai H, Song G. Exploration and Application of New Mode of Teaching Practice in Biochemistry Teaching. Guangdong Chemical Industry. 2014;41:189–190 [Google Scholar]
- 49. Qiu GR, Liu H, Li CY, Li XM, Zhao YY. Application of PBL teaching methods on integrated curriculum of Human developmental genetics. Education Teaching Forum. 2014;15:81–83 [Google Scholar]
- 50. Yin G, Zhong GM, Zhang ZZ, Yan GM, Wang LH, et al. Research and practice of PBL teaching method on Human anatomy laboratory teaching. Journal of Educational Institute of Lilin Province. 2014;30:38–39 [Google Scholar]
- 51. Zhao W, Lan X, Zhu K, Gong Y. Effect analysis of pharmacology PBL teaching. China Medical Herald. 2014;11:135–139 [Google Scholar]
- 52. Frambach JM, Driessen EW, Chan LC, van der Vleuten CP. Rethinking the globalisationof problem-based learning: how culture challenges self-directed learning. Med Educ.2012; 46:738–747. 10.1111/j.1365-2923.2012.04290.x [DOI] [PubMed] [Google Scholar]
- 53. Dochy F, Segers M. Bossche van den P, Gijbels D. Effects of problem-based learning: a meta-analysis. Learning and Instruction. 2003;13:533–68. [Google Scholar]
- 54. Albanese MA, Mitchell S. Problem-based learning: a review of literature on its outcomes and implementation issues. Acad Med. 1993;68:52–81 [DOI] [PubMed] [Google Scholar]
- 55. Norman GR, Schmidt HG. Effectiveness of problem-based learning curricula: theory, practice and paper darts. Med Educ.2000;34:721–728. [DOI] [PubMed] [Google Scholar]
- 56. Ren X, Yin J, Wang B, Roy Schwarz M. A descriptive analysis of medical education in China. Med Teach.2008; 30:667–72 10.1080/01421590802155100 [DOI] [PubMed] [Google Scholar]
- 57. Wu J. Mutation-based learning to improve student autonomy and scientific inquiry skills in a large genetics laboratory course. CBE Life Sci Educ. 2013;12:460–470. 10.1187/cbe.12-09-0168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Maudsley G. Do we all mean the same thing by “problem-based learning”? A review of the concepts and a formulation of the ground rules. Acad Med. 1999;74:178–85. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.