Abstract
Primary hepatic actinomycosis is one of the chronic abscess-forming infections of the liver. Accurate diagnosis is frequently delayed due to its indolent course and nonspecific clinical and radiological manifestations. We report a case of a 57-year-old man presenting with asymptomatic multiple hepatic masses on follow-up abdominal computed tomography performed 1 year after stomach cancer surgery. Although a percutaneous liver biopsy procedure was conducted twice in order to obtain confirmative pathology, only a nonspecific organizing abscess with plasma cell infiltration was revealed, without identification of any organism in the tissue cultures. Ultimately, actinomycosis was diagnosed following the detection of sulfur granules on open surgical biopsied tissue. This case suggests that primary hepatic actinomycosis should be considered as one of the possible causes for enigmatic inflammatory lesions of the liver.
Keywords: Actinomycosis, Multiple liver abscess, Differential diagnosis
INTRODUCTION
Actinomycosis is a chronic suppurative granulomatous infection caused by anaerobic or microaerophilic bacteria, primarily from the genus Actinomyces. It normally colonizes the mouth, gastrointestinal tract, and female genital tract. Any site of body can be affected by actinomycosis, but hepatic involvement is rare. Hepatic actinomycosis is usually secondary to other intraabdominal infections, and primary hepatic actinomycosis only accounts for 5% of all actinomycosis cases.1 A diagnosis of hepatic actinomycosis is frequently missed because of its indolent and slowly progressive characters, and non-specific clinical and radiologic manifestations.
We experienced a case of 57-year-old man with multiple asymptomatic space occupying lesions of liver, which were ultimately found to be primary hepatic actinomycosis. We here report this case along with a review of relevant literature.
Case Report
A 57-year-old man was referred to the department of Internal Medicine for multiple hepatic masses.
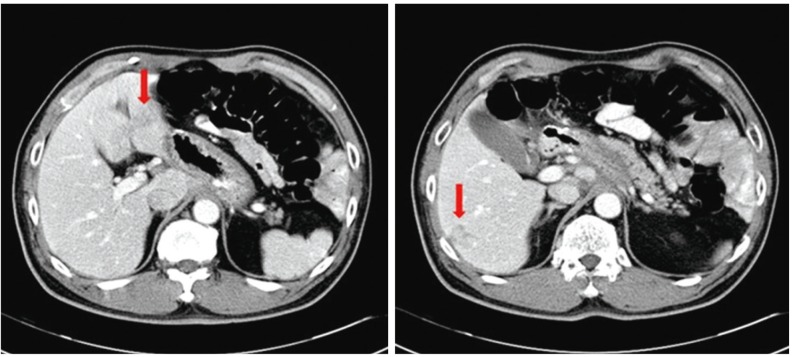
He had undergone distal gastrectomy due to an early gastric cancer. The postoperative check-up 6 months after operation showed no abnormal findings. However, multiple hepatic masses were detected on follow-up computed tomography (CT) at 1 year after operation. They were ill-defined and showed heterogeneous low-attenuation on delayed phase (Fig. 1). He did not complain of any symptom including fever, chilling, abdominal pain or weight loss. He had eaten sliced beef omasum (the 3rd compartment of the stomach in ruminants) 1 month ago. On physical examination, his blood pressure was 121/78 mmHg, pulse rate 80/min, body temperature 36.3℃. He did not appear acutely ill, and presented no abdominal tenderness, palpable organ, or enlarged lymph node. White blood cell (WBC) count was 8,500/mm3 (neutrophil 65.5%, lymphocyte 28.0%, eosinophil 1.5%). Serum aspartate aminotransferase was 18 IU/L, alanine aminotransferase 20 IU/L, and total bilribuin 0.5 mg/dL. His serum alkaline phosphatase and C-reactive protein were elevated to 153 IU/L (40-120 IU/L) and 6.1 mg/dL, respectively. Serologic markers of hepatitis B and C were all negative, while the antibody to toxocara was positive. Considering history of eating omasum and positivity for toxocara antibody, liver biopsy was done and albendazole was prescribed on clinical impression of hepatic toxocariasis. Percutaneous liver biopsy revealed polymorphous inflammatory cells with fibrosis and marked plasma cell infiltration which is consistent with organizing abscess.
Figure 1. Abdominal CT image obtained at 12 months after distal gastrectomy, showing ill-defined hepatic masses with heterogeneous low attenuation on delayed phase.
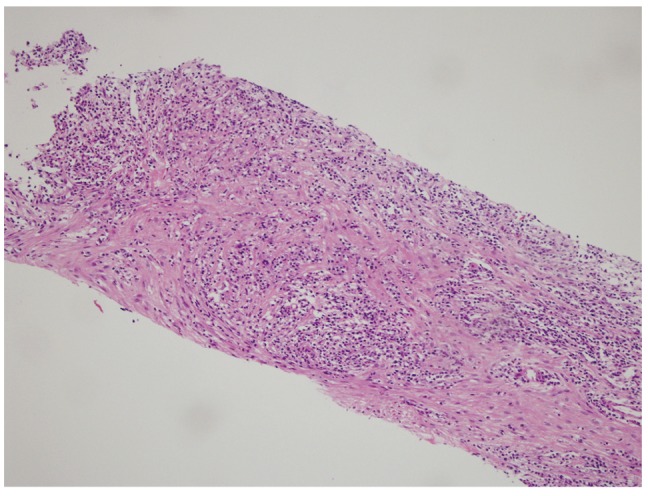
Two months later, he complained of right flank pain. Tenderness with overlying skin redness and warmth was noted on physical examination. Abdominal CT showed the pre-existing multiple hepatic masses increasing in size and extending to the parietal peritoneum. They were heterogeneously low-attenuated with peripheral hyperemic changes on arterial phase, and highly attenuated on delayed phase. Considering inflammatory pseudotumor and malignancy, further evaluations were done. Serum immunoglobulin G (IgG) was elevated to 2580 mg/dL (700-1,600 mg/dL), while immunoglobulin G4 (IgG4) was within normal range. A whole body positron emission tomography-CT showed multiple hypermetabolic hepatic masses (maximum standardized uptake value (SUV) of 14.3) and generalized hypermetabolic lymph nodes (maximum SUV of 5.0). The second percutaneous liver biopsy was done and showed the organizing abscesses, which was the same for the previous one (Fig. 2). The number of IgG4 positive plasma cell was 14/high power field (HPF) and IgG/IgG4 was rated less than 5%. No organisms were identified by gram stain and culture, acid-fast bacilli stain and culture, and fungus culture of the liver tissue. Although IgG4 level was not elevated, systemic corticosteroid was administered on the possible diagnosis of the hepatic inflammatory pseudotumor.
Figure 2. The second percutaneous liver biopsy revealed polymorphous inflammatory cells with fibrosis and marked plasma cell infiltration, which is consistent with an organizing abscess. Hematoxylin and eosin (H&E) stain, ×100.
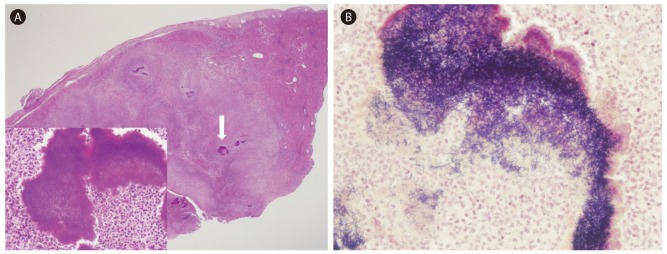
After 2 week of corticosteroid treatment, patient's right flank pain was intensified. WBC was elevated to 17,400/mm3 (neutrophil 87.6%). Multiple hepatic masses became more prominent and invaded into the muscle layer of right abdominal wall on CT (Fig. 3). To find out an unusual infection which might be aggravated during immunosuppressive treatment, the exploratory laparotomy was performed. On the operative finding, several whitish masses were noted on the surface of liver. The surgically biopsied tissue for the lesion showed chronic inflammation with abscess and sulfur granule on hematoxylin and eosin stain. Numerous gram-positive filamentous organisms were noted on gram stain (Fig. 4). The tissue culture did not identify any organisms incubated aerobically and anaerobically up to 2 weeks. The acid-fast bacilli stain was negative and there was no evidence of malignancy. Then, the definite diagnosis was confirmed as hepatic actinomycosis.
Figure 3. Abdominal CT image obtained after 2 weeks of corticosteroid treatment showing enlarged hepatic masses invading the muscle layer of the right abdominal wall.
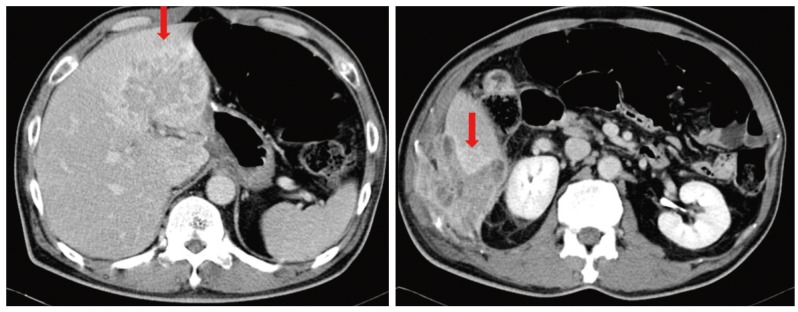
Figure 4. (A) An open surgical biopsy sample showing several sulfur granules in the background of an organizing abscess (H&E, ×40). The indicated sulfur granule is enlarged in the box on the left (H&E stain, ×400). (B) Numerous Gram-positive filamentous organisms can be identified (Gram stain, ×400).
Intravenous penicillin G for a week and ceftriaxone for 5 weeks was administered and then changed to oral amoxicillin for 11 weeks. After 2 months of treatment, the size of hepatic masses was decreased on the abdominal CT and the clinical symptoms were improved.
DISCUSSION
For several decades, primary hepatic actinomycosis has been reported in several literatures. The diagnosis was rather easily made by percutaneous liver biopsy and further surgical procedures were not needed in most of the cases. In Korea, all of the reported cases were confirmed as primary hepatic actinomycosis after one percutaneous biopsy.2,3,4,5,6 However, in our case, the patient was ultimately diagnosed after surgery following two uninformative percutaneous biopsies. The possible explanations for delayed diagnosis are the insufficient incubation period and the lack of the appropriate anaerobic media. Because neither white blood cells nor bacteria were seen on initial gram stain which was done in the microbiology laboratory, the biopsy specimen was incubated only 2 days for culture. In addition, the surfur granules, which virtually guarantee the diagnosis of actinomycosis,6 were relatively scarce on our specimen so would have been hardly detected. Furthermore, as our patient was asymptomatic and the space occupying lesions of the liver were found on routine check-up after cancer surgery, to suspect infectious diseases were far more difficult.
Actinomycosis is a chronic granulomatous infection caused by anaerobic or microaerophillic bacteria from the genus Actinomyces. This infection has a tendency to form draining sinuses, which discharge a conglomeration of Actinomyces filaments solidified with elements of tissue exudate, so called surfur granules.
The most important step in the pathogenesis of this organism is a disruption of mucosal integrity.7 For example, poor oral hygiene, long-standing intrauterine device, peptic ulcer, gastrointestinal infection, and recent abdominal surgery are recognized as predisposing factors.8 It also applies to our patient because he underwent laparoscopic distal gastrectomy 12 months prior to the detection of hepatic actinomycosis.
The proportion of actinomycosis which involves abdomen is about 20% of reported cases.9 Of them, hepatic infection is present in 15% of the patients, which comprises 5% of all actinomycosis cases.1
Clinical manifestations are generally non-specific and indolent, with fever, weight loss or abdominal pain. Laboratory data have frequently associated leukoaytosis (75%) with a left shift, anemia, elevated alkaline phosphatase levels (83.3%) with actinomycosis.10
elevated alkaline phosphatase levels (83.3%) with actinomycosis.10 Imaging findings are non-specific and often mimic other diseases such as neoplasm (either primary or metastatic). Kanellopoulou et al reported in their review of 57 cases of hepatic actinomycosis that the disease manifested as a single abscess/mass in two-thirds of the cases, and as multiple hepatic lesions in the remaining onethird.11
Microbiologic and pathologic studies are essential for a diagnosis of actinomycosis. The ultimate diagnosis is established by growth of the organism in the appropriate media. However, such bacterial confirmation is accomplished in less than 50% of cases because of the overgrowth of associated bacteria, lack of the proper media, insufficient incubation period, improper specimen gathering and transportation techniques or prior antibiotic therapy.6,12 Lacking absolute bacterial identification, the most helpful diagnostic finding is the detection of sulfur granules. However, when only small quantities of tissues are available, sulfur granules can be easily missed and only inflammation or fibrosis may be identified.
For the reasons stated above, the diagnosis of actinomycosis is frequently delayed. In the past, when actinomycosis was much more common, it was referred to as "the most misdiagnosed disease" and it still remains a diagnostic challenge despite technological advances.13 Therefore, it would be prudent to be suspicious that this rare infection may be present under conditions where cell culture reveals only "inflammation", "abscess" or "fibrosis". Furthermore, obtaining sufficient amounts of specimen through repeated cultures and even surgical biopsy should be considered to increase the yield of microbiologic and pathologic diagnosis, as evidenced by our case.
Recently, 16S ribosomal ribonucleic acid gene sequence analysis has been used as a powerful tool for identifying Actinomyces. This method allows for more rapid and accurate identification of actinomycosis possible12 and thus may be useful when actinomycotic chronic inflammation is clinically suspected but no microorganisms are identified in conventional cultures.
Despite the delay in diagnosis, prognosis is favorable because many antibiotics are available to which Actinomyces strains are susceptible. The mortality rate associated with actinomycosis has been reported as 7.6%.1,10,12,14 However, because of the tendency to recur, the antibiotic treatment must incorporate high doses and prolonged duration. A long-term follow-up is also needed for monitoring of the treatment response and for early detection of any recurrence. The duration of treatment should be individualized by disease location, severity, and changes in follow-up imaging results. In general, 10-20 million units of intravenous penicillin for 2 to 6 weeks, followed by oral therapy with penicillin or amoxicillin for 6 to 12 months, is recommended.
There are no established guidelines for surgical intervention. Combined medical and surgical approaches have shown a similar mortality rate with antibiotics monotherapy.10,14 However, surgery alone appears to be inappropriate for the treatment of this disease. 11 Hence, treatments for actinomycosis should be based on antibiotics, and in case of refractory diseases, surgery can be considered as an adjunctive therapy.
In conclusion, making a diagnosis of primary hepatic actinomycosis is difficult because it is rare and progresses slowly. Actinomycosis also mimics a variety of other disorders in terms of clinical manifestations and radiologic findings. Hence, when space-occupying lesions of the liver are identified, efforts should be made to enable a microbiologic and pathologic diagnosis as early as possible to detect unusual microorganisms and to exclude malignancy.
Abbreviations
- CT
computed tomography
- WBC
white blood cell
- Ig
immunoglobulin
- SUV
standardized uptake value
- HPF
high-power field
- H&E
hematoxylin and eosin
Footnotes
Conflicts of Interest: The authors declare that they have no competing interests.
References
- 1.Wong JJ, Kinney TB, Miller FJ, Rivera-Sanfeliz G. Hepatic actinomycotic abscesses: diagnosis and management. AJR Am J Roentgenol. 2006;186:174–176. doi: 10.2214/AJR.04.1691. [DOI] [PubMed] [Google Scholar]
- 2.Ryu JC, Lim CY, Yang ES, Lee JH, Kim KY, Cha SJ, et al. A case of primary hepatic actinomycosis. Korean J Gastroenterol. 1992;24:388–393. [Google Scholar]
- 3.Park SJ, Lee CG, Kim SE, Kim JH, Lee KH, Kim KY, et al. A Case of Liver Abscess Associated with Duodenal Perforation by a Toothpick. Korean J Gastrointest Endosc. 2008;36:390–394. [Google Scholar]
- 4.Kim JU, Park HJ, Song YG, Ji SW, Lee SI, Park CI. A case of primary hepatic actinomycosis coinfected with alpha-streptococcus. Korean J Med. 2002;63:596–599. [Google Scholar]
- 5.Ha CW, Koh JS, Cho KJ, Jang JJ. A case of hepatic actinomycosis disgnosed by fine needle aspiration cytology. Korean J Cytopathol. 1992;3:100–103. [Google Scholar]
- 6.Lee JD, Kim PG, Jo HM, Park DH. A case of primary hepatic actinomycosis. J Korean Med Sci. 1993;8:385–389. doi: 10.3346/jkms.1993.8.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brook I. Actinomycosis: diagnosis and management. South Med J. 2008;101:1019–1023. doi: 10.1097/SMJ.0b013e3181864c1f. [DOI] [PubMed] [Google Scholar]
- 8.Miyamoto MI, Fang FC. Pyogenic liver abscess involving Actinomyces: case report and review. Clin Infect Dis. 1993;16:303–309. doi: 10.1093/clind/16.2.303. [DOI] [PubMed] [Google Scholar]
- 9.Bennhoff DF. Actinomycosis: diagnostic and therapeutic considerations and a review of 32 cases. Laryngoscope. 1984;94:1198–1217. doi: 10.1288/00005537-198409000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Sharma M, Briski LE, Khatib R. Hepatic actinomycosis: an overview of salient features and outcome of therapy. Scand J Infect Dis. 2002;34:386–391. doi: 10.1080/00365540110080304. [DOI] [PubMed] [Google Scholar]
- 11.Kanellopoulou T, Alexopoulou A, Tanouli MI, Tiniakos D, Giannopoulos D, Koskinas J, et al. Primary hepatic actinomycosis. Am J Med Sci. 2010;339:362–365. doi: 10.1097/MAJ.0b013e3181cbf47c. [DOI] [PubMed] [Google Scholar]
- 12.Hansen JM, Fjeldsøe-Nielsen H, Sulim S, Kemp M, Christensen JJ. Actinomyces species: A danish survey on human infections and microbiological characteristics. Open Microbiol J. 2009;3:113–120. doi: 10.2174/1874285800903010113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Acevedo F, Baudrand R, Letelier LM, Gaete P. Actinomycosis: a great pretender. Case reports of unusual presentations and a review of the literature. Int J Infect Dis. 2008;12:358–362. doi: 10.1016/j.ijid.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 14.Lai AT, Lam CM, Ng KK, Yeung C, Ho WL, Poon LT, et al. Hepatic actinomycosis presenting as a liver tumour: case report and literature review. Asian J Surg. 2004;27:345–347. doi: 10.1016/S1015-9584(09)60066-X. [DOI] [PubMed] [Google Scholar]