Abstract
Ludwig’s angina is a potentially life threatening disease that can arise from odontogenic infections if they are not attended well in advance. Its incidence in pregnancy is rare, but has been reported. Pregnancy is associated with complex physiological changes in the body which can make small dental infections assume grave proportions if not treated appropriately. This article presents a case of a 24 year old, 32 week pregnant lady who reported with swelling around the jaws and neck, difficulty in breathing and swallowing since 2 days. She had to be taken up for pre-term delivery to avoid damage to foetus. Subsequently she underwent multiple debridement of the cellulitis affecting the deep neck spaces and superior mediastinum. Surgical debridement and intravenous antibiotics along with adequate hydration improved the health of the patient before she was discharged.
Introduction
Wilhelm Frederick von Ludwig described an infection through the posterior border of the mylohyoid muscle to the sub maxillary, sublingual, and sub mental spaces that together form the submandibular space which starts in either the sub maxillary or the sublingual spaces and then disseminates to entire submandibular space; it begins as a cellulitis, then turns into fasciitis, and finally becomes a true abscess [1]. The aetiology for most cases is associated with a preceding odontogenic infection, peritonsillar abscess, mandibular fracture, or other facial trauma. The treatment of patients with Ludwig’s angina is directed in three ways: airway safety, antibiotic treatment, and surgical drainage. Metabolic control and fluid replacement are important adjuncts. Pregnancy is associated with significant psychological and physiological changes in the body with high incidence of poor oral hygiene, dental caries, and subsequent infection. Pregnant women are at higher risk of tooth decay for several reasons, including increased acidity in the oral cavity, sugary dietary cravings, and limited attention to oral health [2]. Dental caries or unattended oral infection can assume grave proportions during pregnancy due to an upheaval of the physiological system and severe septic complications and an increased risk of adverse foetal outcomes has been reported [3]. Fortunately the incidence of these severe maxillofacial infections during pregnancy is low; however a couple of cases of Ludwig’s angina during pregnancy have been reported in the literature [4]. Although many elective procedures may be delayed until the baby has been delivered, several circumstances exist in which care cannot be postponed, including those involving trauma, acute infections of the head and neck, erupting or impacted teeth that are causing problems, and benign and malignant tumors [5]. Because of a fear of injuring either the mother or unborn child, some practitioners may withhold care or medications from their patients, inadvertently causing harm. An understanding of the patient’s physiologic changes, the effects of chronic infection, and the risks or benefits of medications is necessary to adequately advise a patient [6]. We present a case of Ludwig’s angina along with deep neck space infection in a young pregnant lady who had to deliver prematurely to avoid fatal complications to the foetus. The lady was treated by multiple surgical debridement’s under general anaesthesia and appropriate antibiotics and medical support before she was discharged.
Case Report
A 24 year old, 32 week pregnant lady reported to emergency triage with difficulty in breathing and swallowing since 2 days and a swelling around the jaws and neck since 1 week. Oral and maxillofacial surgery consultation was sought in view of suspected Ludwig’s angina because of a large swelling over the neck and jaws, and gasping for breath (Fig. 1). After obtaining consultation with Department of Obstetrics and Gynaecology regarding the status of the foetus and the administration of the antibiotics, the patient was immediately started with empirical antibiotics and salbutamol nebulisation. An emergency surgery was planned for incision and decompression under general anaesthesia to relieve the pressure on the airway and an effective awake fibre optic intubation was carried out followed by ultrasonography to assess the status of foetus which revealed foetal bradycardia and thus a decision was made to deliver the child primarily to avoid any permanent damage to the foetus. A lower segment caesarean section was carried out to deliver the baby who was then transferred to the neonatal intensive care unit for further management. Following safe delivery, Ludwig’s angina was attended wherein offending deeply carious right lower first molar and right upper second molar were extracted, and bilateral extra oral sub mandibular and sub mental incisions were placed to release the contents of the cellulitis over the jaws and neck. The collections obtained were sent for culture and sensitivity. The antibiotic regimen started preoperatively included intravenous amoxicillin-clavulanate combination 1.2 g three times daily, metronidazole 500 mg three times daily and gentamicin 80 mg twice daily along with anti-inflammatory medications and adequate hydration.
Fig. 1.

Photograph of the patient at the emergency triage showing large swelling over the jaws and neck bilaterally
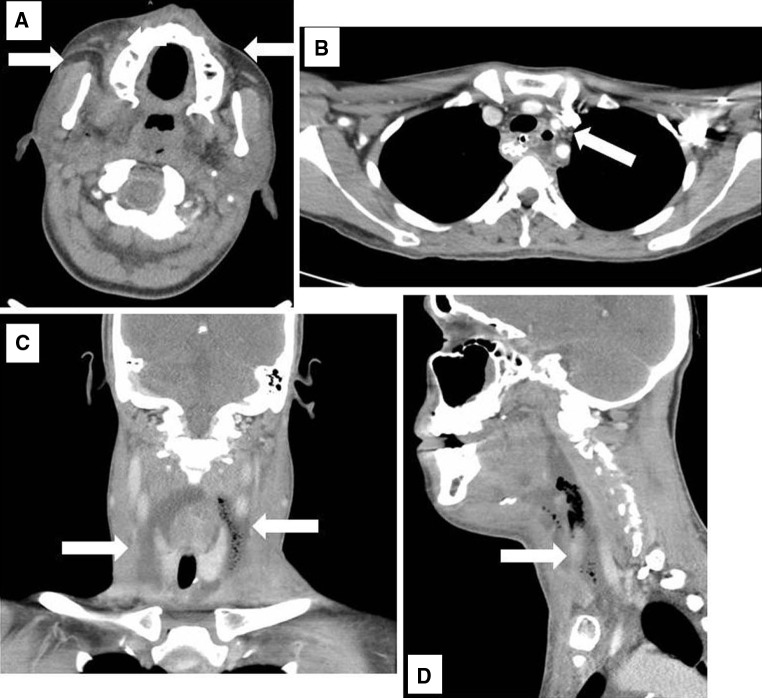
Three days, post-operatively, patient’s condition did not improve satisfactorily with complaints of soreness in throat and difficulty in swallowing and speech. Since the patient had delivered, it was decided to conduct a computed tomography scan with contrast to look for any source of redundant infection. The scan revealed large collections of pus like radiolucencies in the lateral pharyngeal and retropharyngeal spaces bilaterally with small collections in the superior mediastinum along the aortic arch (Fig. 2). A second surgery was planned for debridement under general anaesthesia with assistance from eye, nose and throat specialist and cardiovascular and thoracic surgery specialists. Careful dissection via sub mandibular and sub mental incisions produced drainage of about 150 ml of pus bilaterally (Fig. 3). The superior mediastinum was approached through small supra clavicular incisions on each side of the neck with minimal drainage from both the sites. Rubber corrugated drains were placed at all the incision sites and patency was maintained. The culture and sensitivity report showed evidence of activity with piperacillin and tazobactam antibiotic combination; hence the antibiotic regimen was changed to the sensitive group of antibiotics. Following the second surgery and change in antibiotics the patient started showing significant improvement with relief in symptoms namely, hoarseness of voice and difficulty in swallowing. The drains were removed after the secretions had decreased and the incision sites were closed primarily in layers. The patient had a total stay of about 21 days in the hospital when she was discharged. Subsequent follow up visits were uneventful for the patient.
Fig. 2.
a Computed tomographic scans of the face showing collections in the buccal and submandibular regions. b Scan images of the mediastinum showing collections close to the arch of aorta. c Scan images of the neck showing collections in the lateral pharyngeal spaces. d Scan images of the neck showing collections in the retropharyngeal spaces
Fig. 3.
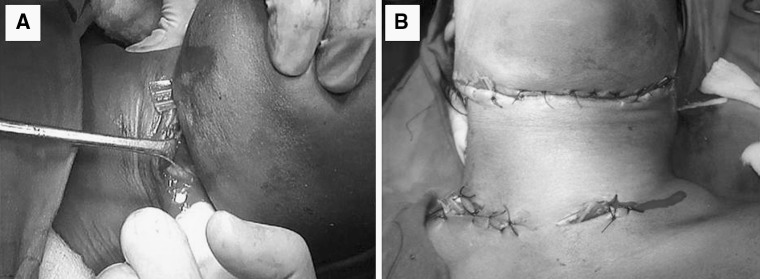
a Copius amount of pus being drained by finger dissection in the neck region. b Incisions placed at the supra clavicular regions bilaterally to drain the collections from superior mediastinum
Discussion
Ludwig angina was first described by WF von Ludwig in 1836, as a rapidly progressive deep gangrenous cellulitis of the soft tissues of the neck and floor of the mouth involving the submandibular and sublingual spaces. Ludwig’s angina usually presents in patients with poor dental hygiene, which accounts for approximately 75–95 % of cases. The clinical presentation consists of malaise, dysphagia, bilateral cervical swelling, neck tenderness, dysphonia, elevation and swelling of the tongue, pain in the floor of the mouth, sore throat, restricted neck movement, and stridor suggestive of impending airway obstruction. The usual cause of Ludwig’s angina is a mixture of aerobic and anaerobic bacteria including predominately normal oral flora. In 1939, Grodinsky proposed the following criteria to diagnose Ludwig angina: the process occurs bilaterally in more than one space; produces gangrenous, serosanguinous, putrid infiltration with little or no pus; involves connective tissue, fascia, muscle, and rarely involves glandular structures; and spreads by continuity not by lymphatics or hematogenously. Pregnancy is associated with complex changes, where oral cavity undergoes enormous alterations many of which are seriously damaging in nature. Every gestational woman should be encouraged to seek medical and dental care during her pregnancy, as failure to treat developing problems affects the health of both the mother and the unborn child. Education of dental care professionals by gaining a basic understanding of the physiologic changes of pregnancy, use of medications or illicit drugs or substances during gestation, and their influence in the delivery of dental care should be mandatory [7]. Dental decay and abscesses in the oral and maxillofacial region may release various exotoxins, cytolytic enzymes, as well as gram-positive and gram-negative bacteria exhibiting their deleterious effects on the entire physiological system [8]. Ascertaining an early diagnosis at the Emergency Department, and involvement of anaesthesia, obstetrics, and, ear, nose and throat specialist services is vital for materno-fetal wellbeing. Careful evaluation of the airway and prompt antimicrobial therapy with surgical decompression may represent a plausible alternative in pregnant patients [9]. Fibre optic intubation using topical anaesthesia is the first choice for airway control in adult patients with deep neck infections including Ludwig’s angina [10]. The objectives for management are avoidance of teratogenic drugs, avoidance of intrauterine foetal hypoxia and acidosis, prevention of spontaneous abortion early in pregnancy, and prevention of premature labour later in pregnancy [11]. The decision of pre mature delivery in this case was made because of weak foetal tracing probably due to foetal hypoxia and bradycardia. Though pre mature delivery is not without complications like foeto-maternal morbidity and mortality, it has been reported to improve the maternal ventilation status along with improved hemodynamic changes due to release of the pressure over the vena cava. Once the airway is secured and anaesthesia is achieved the next most important step should be to evacuate the contents of cellulitis resulting in decompression and release of pressure over the airway and other vital structures in the neck. It is believed that the improvement of local perfusion, the decrease of hydrostatic pressure, and the introduction of superficial mucosal flora are factors that help to decrease the spread of the invading pathogens [12]. Of course the role of antibiotics and other medical support cannot be overemphasized here. The guidelines laid down by food and drug authority should always be borne in mind while selecting the medications used for pregnant and lactating mothers.
To conclude, care of the gravid patient may seem daunting, but use of resources helps focus the key issues of care.
Acknowledgments
The authors would like to acknowledge the support received from Professor Ramkumar, Professor and Head, Department of Anaesthesia, and the faculty and residents of the Department of Oral And Maxillofacial Surgery for their timely intervention.
Disclosure
The authors do not have any financial disclosures to be made for this manuscript currently or within 5 years.
References
- 1.Shockley D, Williams W. Ludwig’s angina: a review of current airway management. Arch Otolaryngol Head Neck Surg. 1999;125(5):600–604. doi: 10.1001/archotol.125.5.600. [DOI] [PubMed] [Google Scholar]
- 2.Hey-Hadavi JH. Women’s oral health issues: sex differences and clinical implications. Women’s Health Prim Care. 2002;5(3):189–199. [Google Scholar]
- 3.Mazze RI, Kallen B. Reproductive outcome after anaesthesia and operation during pregnancy: a registry study of 5405 cases. Am J Obstet Gynecol. 1989;161:1178–1185. doi: 10.1016/0002-9378(89)90659-5. [DOI] [PubMed] [Google Scholar]
- 4.Niederhauser A, Kirkwood D, Magann EF, Mullin PM. Morrison JC Ludwig’s angina in pregnancy. J Matern Fetal Neonatal Med. 2006;19(2):119–120. doi: 10.1080/14767050500439368. [DOI] [PubMed] [Google Scholar]
- 5.Ueeck BA, Assael LA. Perioperative management of the female and gravid patient. Oral Maxillofac Surg Clin N Am. 2006;18:195–202. doi: 10.1016/j.coms.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Dellinger TM. Livingston HM pregnancy: physiologic changes and considerations for dental patients. Dent Clin N Am. 2006;50:677–697. doi: 10.1016/j.cden.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Livingston HM, Dellinger TM, Holder R. Considerations in the management of the pregnant patient. Spec Care Dentist. 1998;18(5):183–188. doi: 10.1111/j.1754-4505.1998.tb01737.x. [DOI] [PubMed] [Google Scholar]
- 8.Topazian RG, Goldberg MH, Hupp JR. Oral and maxillofacial infections. 4. Philadelphia: W.B. Saunders; 2002. pp. 30–42. [Google Scholar]
- 9.Soltero R, Mercado-Alvarado J. Successful conservative management of Ludwig’s angina in advanced pregnancy. Bol Asoc Med P R. 2009;101(3):42–43. [PubMed] [Google Scholar]
- 10.Ovassapian A, Tuncbilek M, Weitzel EK, Joshi CW. Airway management in adult patients with deep neck infections: a case series and review of the literature. Anesth Analg. 2005;100:585–589. doi: 10.1213/01.ANE.0000141526.32741.CF. [DOI] [PubMed] [Google Scholar]
- 11.Rosen MA. Management of anaesthesia for the pregnant surgical patient. Anaesthesiology. 1999;91(4):1159–1163. doi: 10.1097/00000542-199910000-00033. [DOI] [PubMed] [Google Scholar]
- 12.Scott A, Stiernberg N, Driscoll . Deep neck space infections; Bailey head & neck surgery–otolaryngology. Philadelphia: Lippincott-Raven Chap; 1998. pp. 819–835. [Google Scholar]