Abstract
Pseudoaneurysm of internal maxillary artery following trauma is a rare clinical entity. A rapidly growing swelling in the facial region following fracture of the mandibular subcondylar region is an indication of a developing aneurysm. A case of pseudoaneurysm of the internal maxillary artery following condylar fracture of mandible is reported. The case was treated successfully by surgery.
Keywords: Pseudoaneurysm, Internal maxillary artery, Mandibular condylar fracture
Introduction
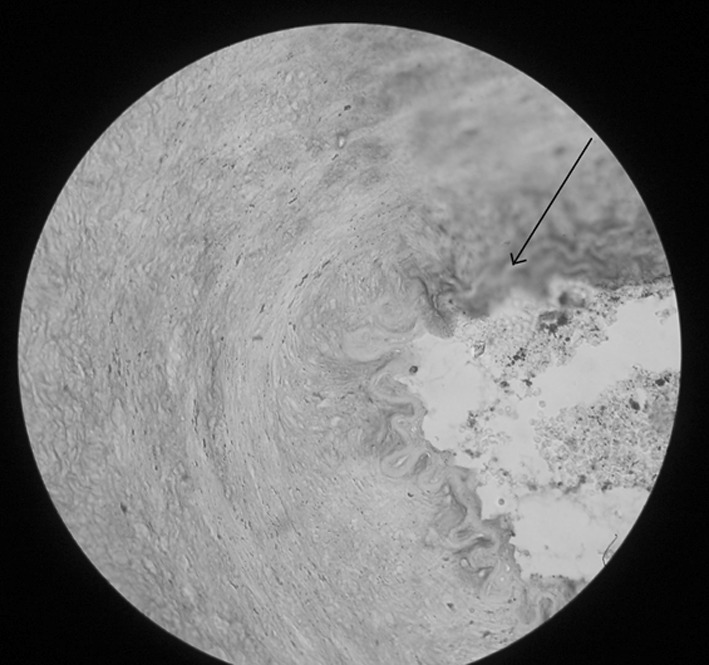
Aneurysm is an irreversible dilatation of an artery. It may involve all the layers of the artery wall (true aneurysm) or only a portion of the wall and surrounding tissue (false or pseudoaneurysm).Traumatic aneurysm is an example of false aneurysm or pseudoaneurysm caused by injuries which rupture the full thickness of the arterial wall leading to extravasation of blood into surrounding tissues, producing a pulsatile haematoma. The compressed perivascular connective tissue forms the sac around this false or pseudoaneurysm [1] (Figs. 1, 2).
Fig. 1.

Perivascular compressed connective tissue of pseudoaneurysm (on eosin and haematoxylin stained histopathological slide) in ×10 magnification
Fig. 2.
Perivascular compressed connective tissue of pseudoaneurysm (on eosin and haematoxylin stained histopathological slide) in ×40 magnification
Internal maxillary artery pseudoaneurysm may be caused as a possible complication of trauma [2–4], infection [5], occurring as a result of maxillofacial surgery, therapeutic or diagnostic arterial wall needle puncture. More rarely, internal maxillary artery pseudoaneurysm may result from post-radiation vasculopathy or tumor invasion [2].
Sporadic cases of false aneurysm following fractures of the facial bones have been reported but are a few in number [6, 7]. Despite the great frequency of mandibular condylar fracture and the proximity of the maxillary artery to the fracture site, the occurance of false aneurysm to this artery is very rare [8].
Most of the aneurysms of the internal maxillary artery occur in its terminal (pterygopalatine) segment, while it is very rare in the first or mandibular segments. It is noteworthy that in this patient, the pseudoaneurysm had arisen out of the first part of the maxillary artery [9].
Case Report
A 23 year old male patient reported to the OPD of Dr. R. Ahmed Dental College & Hospital, Kolkata, with the complaint of swelling and throbbing pain in the right side of face in front of the ear following a fall on the point of the chin a fortnight earlier from the date of presentation. Past medical and dental histories were insignificant.
On examination there was a swelling in right preauricular region, around 4 cm in transverse dimension and 6 cm in longitudinal one (Figs. 3, 4). On palpation, swelling was resilient, pulsatile and slightly tender. There was a systolic bruit on auscultation.
Fig. 3.
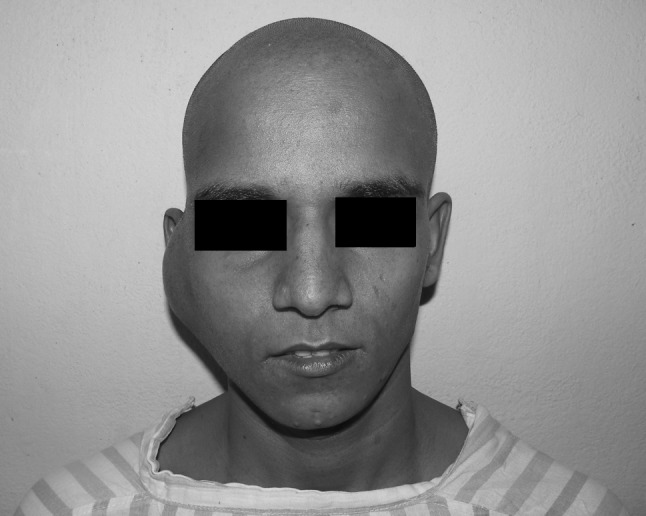
Preauricular swelling in frontal view
Fig. 4.

Preauricular swelling in profile view
Mouth opening was restricted (interincisal opening less than 20 mm) (Fig. 5).
Fig. 5.
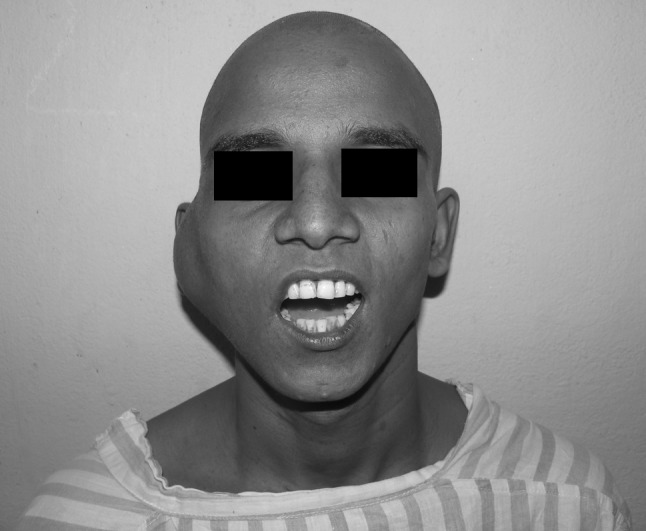
Preoperative mouth opening
Aspiration with wide bore needle yielded rapid filling up of bright red blood in the syringe.
A CT scan revealed a hyperdense lesion in right preauricular region. The lesion emerged at the posterior border of the mandible (Figs. 6, 7).
Fig. 6, 7.
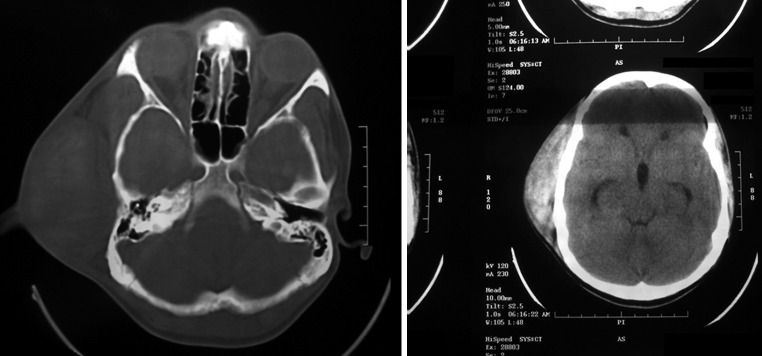
A hyperdense lesion of 6 × 4 cm on axial section, CT scan
Fig. 8.
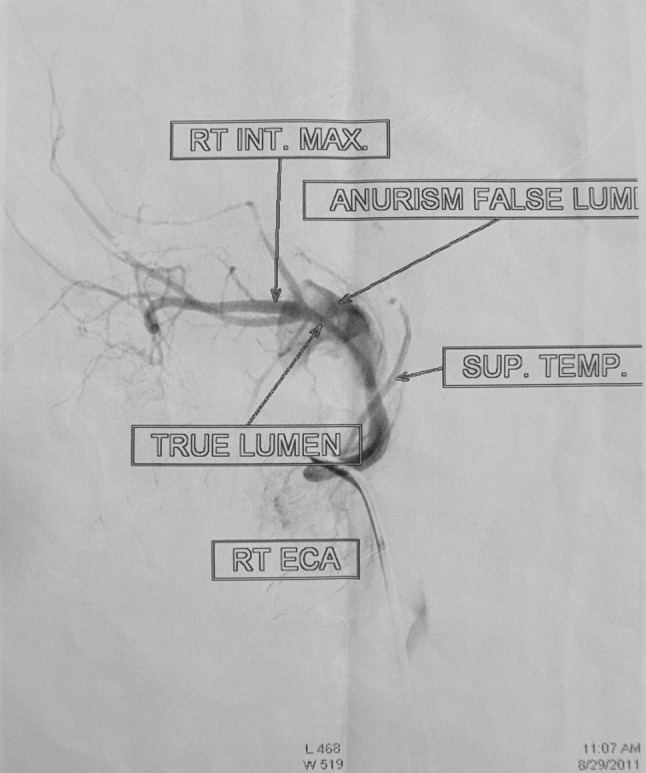
Ballooning of the first part of the internal maxillary artery in carotid angiogram
A carotid angiogram revealed ballooning of internal maxillary artery in its first part. No other feeding vessel or collateral vessels were detectable (Fig. 8).
A treatment plan was chalked out comprising of surgical excision of the aneurysmal sac following external carotid artery ligation.
An extended submandibular incision was made extending from anterior border of right sternocleidomastoid to submental region. The incision was deepened through skin, subcutaneous tissue and platysma. After a sharp dissection through superficial layer of the deep cervical fascia anterior border of sternocleidomastoid was exposed, which was retracted posteriorly. Following this, the posterior belly of diagastric and stylohyoid muscle were exposed and retracted superiorly. The bifurcation of the common carotid artery was exposed. The external carotid artery (ECA) was identified by its various branches in the neck and was ligated above the lingual artery (Fig. 9).
Fig. 9.
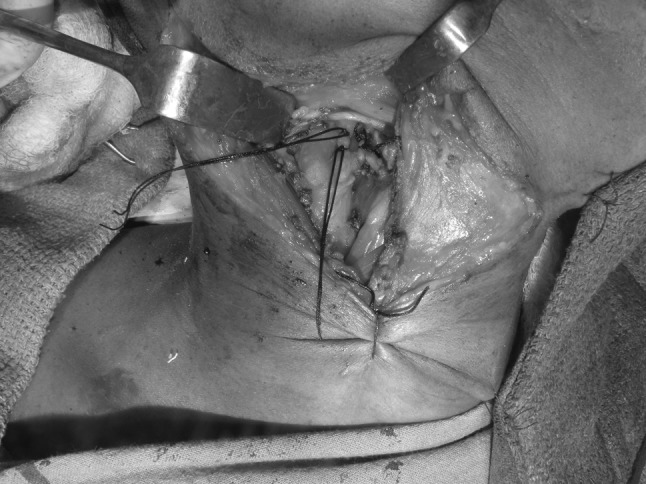
Double ligation of external carotid artery above its superior thyroid artery branch after retraction of sternocleidomastoid muscle and posterior belly of diagastric muscle
Following ligation of ECA, whole lateral surface of ramus and condyle was exposed by further dissection. The aneurysmal sac was seen lying over the lateral surface of ramus and condyle extending into the superficial lobe of the parotid gland.
To expose the deeper part of aneurysmal sac in total a vertical ramus access osteotomy was done and the proximal fragment was swung out laterally (Fig. 10).
Fig. 10.

Swung out proximal part of osteotomised ramus exposing the deep extension of the aneurismal sac
Once the sac was completely exposed it was dissected out carefully using a combination of sharp and blunt dissection (Fig. 11). Brisk haemorrhage which started during the manoeuvre was controlled by vascular clamps. A sharp fracture fragment was removed from medial part of the ramus (which, possibly, had caused the puncture of the arterial wall leading to the formation of the pseudoaneurysm).
Fig. 11.

Dissected aneurismal sac
The osteotomised segments were fixed with a mini plate and screws.
A vacuum drain was placed and wound closed in layers (Fig. 12).
Fig. 12.

Incision closed in layers with vacuum drain in place
Post-operative period was uneventful. A motor weakness was noted in the distribution of the temporal and zygomatic branches of the facial nerve.
Interventional physiotherapy by galvanic stimulation was used to facilitate nerve function recovery. Facial nerve deficit improved considerably (Figs. 13–15).
Fig. 13, 14.
Post op recovery in motor deficit of temporal and zygomatic branches of facial nerve at 3 months post op
Fig. 15.
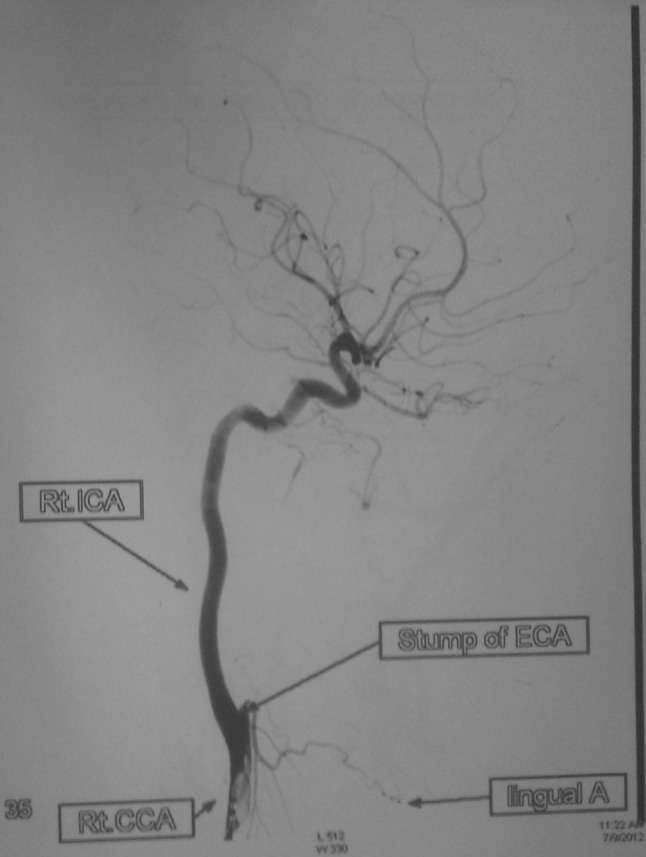
Post-op carotid angiogram showing ligated stump of external carotid artery above the level of lingual artery
Discussion
Pseudoaneurysm is a rare clinical entity. Undiagnosed and untreated it carries the risk of life threatening haemorrhage and exsanguination following rupture.
Presence of pulsatile swelling with an audible systolic bruit with a history of trauma should arouse the suspicion of traumatic pseudoaneurysm and demands further investigations [10]. CT scan and MRI are useful aids in diagnosis.USG and Colour Doppler are also helpful diagnostic tools. But angiography remains the gold standard [10] and most important diagnostic procedure with invaluable aid to the treatment planning. Angiography will confirm the disposition and delineation of the aneurysm with its feeding vessel [11]. Angiography may be combined with CT scan or MRI.
After establishing the diagnosis, there are two treatment modalities to choose from—(1) Endovascular therapy and (2) Surgical management [12].
Endovascular therapy is the primary treatment modality in many centres. The use of transcatheter intervention has improved access to surgically inaccessible vessels and has reduced the need for GA and surgery and associated morbidity and mortality [13]. The added benefit of performing endovascular therapy during angiography has increased its use in trauma patients and as well as an adjunct prior to definitive surgical management.
Transcatheter interventions can be categorised into embolisation, stents and stent grafts.
Embolisation therapy involves the use of agents to occlude vessel lumen. There are numerous embolising agents used like gelfoam, isobutylcyanoacrylate, balloons, coils (made of dacron or nylon fibres) [11]. In order to decide which embolization material is most advantageous for a given patient, certain key points are to be considered.
If the vessel to be embolised is large, then larger embolic agents (gelfoam, coils) are most useful. Deciding on temporary versus permanent occlusion will dictate the use of gelfoam versus coils. In cases where temporary occlusion is desired, gelfoam pledgets or slurry may be used. In cases when permanent occlusion is desired, coils may be the most appropriate embolic material to use. Coils when placed in vessel lumen elicit a thrombogenic response by causing thrombus formation on the dacron or nylon fibres of the coil.
Stents are a second form of transcatheter or endovascular intervention that is commonly used in trauma patients. Numerous sizes and types of stents are utilized for many different clinical applications; viz., covered and bare stents. Stents and stent grafts have the advantage that they maintain the patency of vessel lumen [14, 15]. However the presence of extensive collateral between vessels of the right side and left side of the face and various anastamosis between internal and external carotid arteries, the embolisation or surgical ligation of external carotid artery does not cause any significant compromise of blood supply to the peripheral tissues.
Covered stents, also called stent grafts, have a benefit when used in cases involving pseudoaneurysms. The disruption of the vessel wall is covered by stent grafts. Thus the injured vessel may be salvaged, maintaining blood flow through the lumen of the vessel.
Stents can also be used in conjunction with coils in the treatment of pseudoaneurysms. Following placement of the stent across the neck of a pseudoaneurysm, coils may be placed through the struts of the stent to pack the pseudoaneurysm. The stent act to reinforce the vessel wall across the aneurysm, decreasing the chance of rupture such that coils may be packed more tightly.
Endovascular therapy though a very attractive and modern approach, is not without certain disadvantages.
Endovascular therapy requires skilled and experienced interventional radiologist to perform the procedure. The various collaterals between branches of external and internal carotid artery may result in embolus being propelled into branches of internal carotid artery with dangerous sequels [16, 17].
The aneurysm wall may get punctured during transcatheterisation causing brisk haemorrhage. Moreover embolisation with coils may not occlude the large aneurysmal sac completely.
Surgical management remains the gold standard of treatment, especially for large aneurysm and when noninvasive approach fails. In this particular case, the size of the aneurysm, the need for the evacuation of the infected contents of the sac dictated the exigency of surgical treatment in the form of excision of the aneurysmal sac following external carotid ligation.
Conclusion
Treatment planning of traumatic aneurysm of internal maxillary artery thus needs proper decision-making through a team work involving surgical specialists and interventional radiologists.
A carefully planned and executed access osteotomy will delineate the aneurysmal sac in its entirety. One should also look for a bony spicule at the base of the condylar fracture.
References
- 1.Rich NM, Spencer FC. Vascular trauma. Philadelphia: WB Saunders Co; 1978. pp. 233–259. [Google Scholar]
- 2.Schwartz HC, Kendrick RW. False aneurysm of maxillary artery. An unusual complication of closed facial trauma. Arch Otolaryngology. 1983;109:616–618. doi: 10.1001/archotol.1983.00800230052012. [DOI] [PubMed] [Google Scholar]
- 3.D’Orta JA, Shatney CH. Post traumatic pseudoaneurysm of the internal maxillary artery. J Trauma. 1982;22:161–164. doi: 10.1097/00005373-198202000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Rogers SN, Patel M, Berne JC. Nixon TE—Traumatic aneurysm of the maxillary artery; the role of interventional radiology. J Oral Maxillofac Surg. 1995;24:336–339. doi: 10.1016/S0901-5027(05)80485-0. [DOI] [PubMed] [Google Scholar]
- 5.Lanigan DT, Hey JH, West RA. Major vascular complications of orthognathic surgery: false aneurysm and arteriovenous fistulas following orthognathic surgery. J Oral Maxillofacial Surg. 1991;49:571–577. doi: 10.1016/0278-2391(91)90337-L. [DOI] [PubMed] [Google Scholar]
- 6.Chaloupke JC, Putman CM, Ci Tardi MJ, Ross DA, Sasaki CT. Endovascular therapy for the carotid blowout syndrome in head and neck surgical patients: diagnostic and managerial considerations. AJNR Am J Neuroradiol. 1996;17:843–852. [PMC free article] [PubMed] [Google Scholar]
- 7.Cameron HS, Laird JJ, Carroll SE. False aneurysms, complicating closed fractures. J Trauma. 1972;12:67–74. doi: 10.1097/00005373-197201000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Gerbino G, Roccia F, Grosso M, Regge D. Pseudoaneurysm of the internal maxillary artery and Frey syndrome after blunt facial trauma. J Oral Maxillofac Surg. 1997;55:1485–1490. doi: 10.1016/S0278-2391(97)90657-1. [DOI] [PubMed] [Google Scholar]
- 9.Luo CB, Teng MM, Chang FC, Chang CY. Role of CT and endovascular embolization in managing pseudoaneurysms of the internal maxillary artery. J Chin Med Assoc. 2006;69:310–316. doi: 10.1016/S1726-4901(09)70264-3. [DOI] [PubMed] [Google Scholar]
- 10.Karanth SK, Jagannathan M, Mahesh SG, Devale M. Internal maxillary artery pseudoaneurysm in a case of mandibular fracture. Indian J Plast Surg. 2007;40:51–53. doi: 10.4103/0970-0358.32664. [DOI] [Google Scholar]
- 11.Kawano K, Mizuki H, Mori H, Yanagisawa S (2001) Mandibular Arteriovenous malformation treated by transvenous coil embolisation: a long term follow up with special reference to bone regeneration. J Oral Maxillofac Surg 59:326–330 [DOI] [PubMed]
- 12.Kuehne JP, Weaver FA, Papanicolaou G, Yellin AE. Penetrating trauma of the internal carotid artery. Arch Surg. 1996;131:942–947. doi: 10.1001/archsurg.1996.01430210040008. [DOI] [PubMed] [Google Scholar]
- 13.Chandler JP, Sekhar LN. Intravascular stents and cerebrovascular disease. Crit Rev Neurosurg. 1997;7:315–323. doi: 10.1007/s003290050041. [DOI] [Google Scholar]
- 14.Rogers SN, Patel M, Beirne JC, Nixon TE. Traumatic aneurysm of maxillary artery: the role of interventional radiology. Int J Oral Maxillofac Surg. 1995;24:336–339. doi: 10.1016/S0901-5027(05)80485-0. [DOI] [PubMed] [Google Scholar]
- 15.Hong JT, Lee SW, Lha YK, Son BC, Sung JH, Kim IS, et al. Traumatic pseudoaneurysm of the superficial temporal artery treated by endovascular coil embolization. Surg Neurol. 2006;66:86–88. doi: 10.1016/j.surneu.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 16.Tsumoto T, Natakakita K, Hayashi S, Terada T. Bone defect associated with middle meningeal arteriovenous fistula treated by embolization- case report. Neuro Med Chir. 2001;41:42–47. doi: 10.2176/nmc.41.42. [DOI] [PubMed] [Google Scholar]
- 17.Satoh T, Sakurai M, Yamamoto Y, Asari S. Spontaneous closure of a traumatic middle meningeal arteriovenous fistula. Neuroradiology. 1983;25:105–109. doi: 10.1007/BF00333301. [DOI] [PubMed] [Google Scholar]



