Abstract
Osteoma is a benign osteogenic slow-growing tumor. Though mandible is involved more often than the maxilla only one other case of osteoma sigmoid notch has been mentioned in the English literature till date. Cosmesis and function are the main reasons that dictate the removal of the osteomas, so we preferred to use an intra oral approach to better prevent the scar and achieve good patient acceptance.
Keywords: Osteoma, Peripheral osteoma, Sigmoid notch, Transoral, Mandible tumors
Introduction
Osteoma is a benign osteogenic tumor characterized by proliferation of compact or cancellous bone with limited growth potential. It can be central, peripheral, or extraskeletal. Central osteomas arise from the endosteum, peripheral osteoma from the periosteum, and extraskeletal soft tissue osteoma within a muscle.
The pathogenesis of osteomas is unclear. They are referred to developmental anomalies, true neoplams, or reactive lesions triggered by trauma, muscle traction, or infection [1–3].
In craniofacial bones peripheral osteoma (PO) occurs most frequently in the paranasal sinuses. Other locations include the orbital wall, temporal bone, ptyregoid processes, and external auditory canal [3, 4]. The literature review suggests that a solitary PO of the jaw bones is quite rare, mandible is involved more often than the maxilla [3, 4]. In mandible most frequent site affected is the posterior body, followed by the condyle, angle, ascending ramus, coronoid process, anterior body, and sigmoid notch [4, 5]. Osteomas can occur at any age with equal incidence in males and females [3, 5]. Peripheral osteomas are usually asymptomatic slow-growing lesions; however, when they reach a large size, they can produce swelling and asymmetry.
Patients with osteomas should be evaluated for Gardner’s syndrome, an automosal dominant disease characterized by gastrointestinal polyps, multiple osteomas, skin and soft tissue tumors, and multiple impacted or supernumerary teeth [1, 5].
Only one case of osteoma of sigmoid notch has been reported in English literature [5, 6]. We report the second case of large peripheral osteoma originating from the sigmoid notch area of the mandible in a16-year-old female.
Case Report
A 16-year-old female was referred to the Department of Oral and Maxillofacial Surgery with a complaint of asymptomatic progressive swelling on the right side of the face just anterior to the lobule of the ear for the past 3 years. She had no history of trauma or medical contributory factors.
Physical examination revealed a well-defined, round, bony hard mass along the area of sigmoid notch of the mandible. The mass was fixed to mandible even during the functional movements of the mandible. Overlying skin and the intraoral mucosa were normal. A solitary round, 3 × 3 cm well-defined radiopaque lesion of mandible at the sigmoid notch was detected with panoramic radiography and computed tomograpy (CT) with 3-dimensional (3D) reconstruction (Figs. 1, 2). The working diagnosis of PO of right sigmoid notch of the mandible was made and planned accordingly. There were no associated features of Gardner`s syndrome.
Fig. 1.
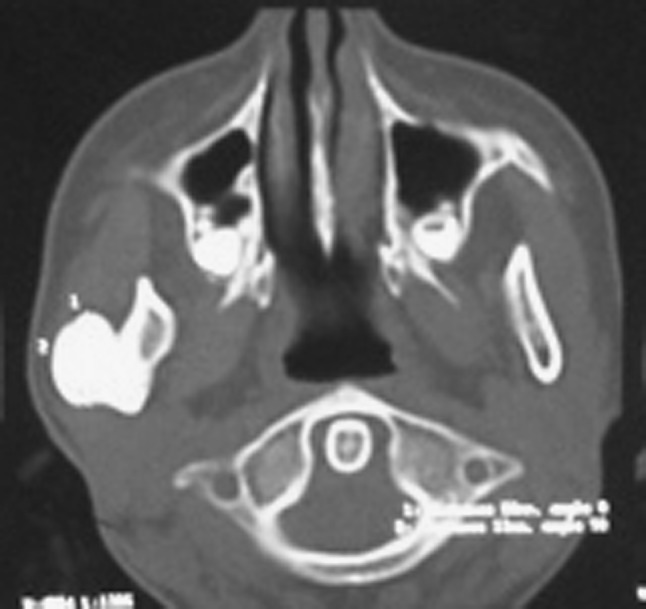
Axial section of the CT scan at the level of sigmoid area
Fig. 2.
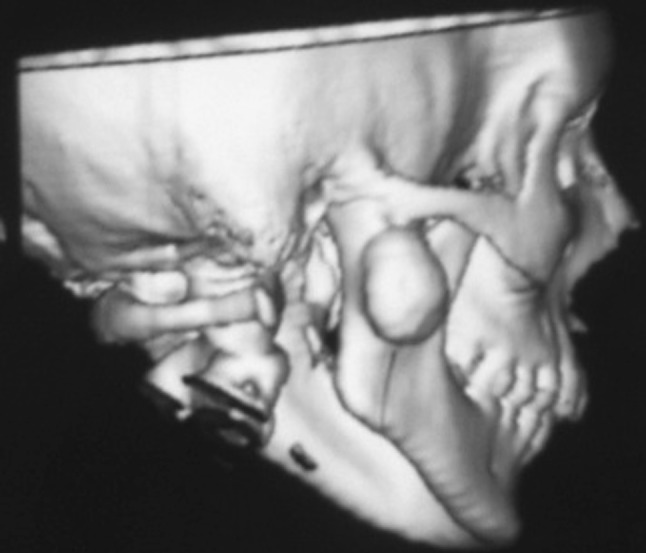
3D CT scan showing the osteoma attached to sigmoid notch
Under general anesthesia after nasal intubation, the mass was approached using an intraoral anterior ramal incision similar to the one used for the sagittal osteotomy of the mandible. The masseter muscle was striped laterally to expose the mass. The lesion was removed using a broad chisel (Fig. 3). Microscopic examination of the specimen confirmed the preoperative diagnosis of PO consisting entirely of dense lameller compact bone (Fig. 4). The follow-up of 2 years showed uneventful healing with normal bone without any signs of recurrence.
Fig. 3.

Excised osteoma
Fig. 4.

H&E section of the lesion showing dense compact bone
Discussion
Osteomas are benign tumors that mainly affect the craniofacial bones. Their real prevalence is unknown; however, Sondergaard et al. [7] reported that the prevalence of osteoma in the normal population is about 4 %. PO of the jaw bones is quite rare. These lesions are more frequent in the mandible than the maxilla.
The exact etiology and pathogenesis of peripheral osteoma is unknown. Neoplastic and reactive causes have been suggested as possible etiologic factors. Kaplan et al. [1, 3] suggested reactive etiology probably associated to trauma. Also, some authors have reported that the muscle traction plays a pivotal role in the development of peripheral osteomas as many of the lesions are located on the lower border of the mandible and area of muscular attachments [5]. However, in the case described in this article, there being no history of previous trauma or infection, we have no information as to the possible cause.
Clinically, a peripheral osteoma appears as a unilateral and well-circumscribed mass ranging from 10 to 40 mm in diameter [3, 5]. They are usually asymptomatic unlike an painful osteoid osteoma and can be discovered in routine clinical and radiographic examination. Sometimes, depending on the location and size of the lesion, it may cause swelling, facial asymmetry, and functional impairment.
Radiographs or computed tomography are used for imaging; however, as demonstrated in this case, the CT is the best imaging modality for determining the exact location and real extension of the lesion. Peripheral osteomas, in most cases, are easy to recognize, on radiological imaging, a peripheral osteoma of the mandible is a classically well-circumscribed, round or oval, mushroom- like radiopaque mass with distinct borders [2, 5, 6]. The lesion may be sessile and attached to the cortical plates with a broad base or pedunculated with a narrow contact area between the lesion and the compact bone. In our case, the lesion consisted of dense, uniformly opaque compact bone with a broad base demonstrated on CT.
Peripheral osteoma should be differentiated from exostoses, osteoblastoma, and osteoid osteoma, late-stage central ossifying fibroma, or complex odontoma. Exostoses are bony excrescences that usually stop growing after puberty [5, 8]. The central ossifying fibromas have a well-defined border, and a thin, radiolucent line separating it from the surrounding bone with a sclerotic border [8]. Osteoblastomas and osteoid osteomas are more frequently painful and grow more rapidly than peripheral osteomas [4]. A complex odontoma presents as a well-defined highly dense radiopacity situated in bone. It is also surrounded by a narrow radiolucent rim [8].
Removal of an asymptomatic peripheral osteoma is not generally necessary. Surgical intervention is indicated only if it becomes large enough to cause facial asymmetry and functional impairment [2, 5]. Surgical excision is usually simple in peripheral osteomas. Transoral approach for excision of the lesion is always preferable whenever feasible just for the obvious reasons of cosmesis.
Contributor Information
Santhosh Rao, Phone: +91-9981525599, Email: santhoshagastya@gmail.com.
Sruthi Rao, Email: jshru23@gmail.com.
D. S. R. Pramod, Email: pramoddsr@gmail.com
References
- 1.Kaplan I, Calderon S, Buchner A. Peripheral osteoma of the mandible: a study of 10 new cases and analysis of the literature. J Oral Maxillofac Surg. 1994;52:467–470. doi: 10.1016/0278-2391(94)90342-5. [DOI] [PubMed] [Google Scholar]
- 2.Larrea-Oyarbide N, Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C. Osteomas of the craniofacial region. Review of 106 cases. J Oral Pathol Med. 2008;37:38–42. doi: 10.1111/j.1600-0714.2007.00590.x. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan I, Nicolaou Z, Hatuel D, Calderon S. Solitary central osteoma of the jaws: a diagnostic dilemma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e22–e29. doi: 10.1016/j.tripleo.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 4.Sayan NB, Üçok C, Karasu HA, Günhan Ö. Peripheral osteoma of the oral and maxillofacial region: a study of 35 new cases. J Oral Maxillofac Surg. 2002;60:1299–1301. doi: 10.1053/joms.2002.35727. [DOI] [PubMed] [Google Scholar]
- 5.Johann AC, de Freitas JB, de Aguiar MC, de Araujo NS, Mesquita RA. Peripheral osteoma of the mandible: case report and review of the literature. J Craniomaxillofac Surg. 2005;33:276–281. doi: 10.1016/j.jcms.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Bessho K, Murakami K, Iizuka T, Ono T. Osteoma in mandibular condyle. Int J Oral Maxillofac Surg. 1987;16:372–375. doi: 10.1016/S0901-5027(87)80162-5. [DOI] [PubMed] [Google Scholar]
- 7.Sondergaard JO, Svendsen LB, Hegnhoj JO, Witt N. Mandibular osteomas in ulcerative colitis. Scand J Gastroenterol. 1986;21:1089–1090. doi: 10.3109/00365528608996426. [DOI] [PubMed] [Google Scholar]
- 8.Richardson PE, Arendt DM, Fidler JE, Webber CM. Radiopaque mass in the submandibular region. J Oral Maxillofac Surg. 1999;57:709–713. doi: 10.1016/S0278-2391(99)90439-1. [DOI] [PubMed] [Google Scholar]


