Abstract
Odontoma is a mixed odontogenic hamartoma involving both epithelial and mesenchymal tissues. If left untreated, it can lead to complications in certain conditions. Here is a rare presentation of an extensive complex odontoma in maxillary sinus pushing third molar near the orbital floor causing transient diplopia in upward gaze occasionally and chronic sinusitis. Although odontomata are not uncommon and are familiar to practitioners, but some aggressive cases may cause problematic sequelae. Even postoperative complications may result if oral surgeons are not aware of the potential pitfalls associated with the surgical removal of large maxillary antrum odontomata. This article reports a rare presentation which can be considered unique because when obstruction of sinus drainage is evident, serious complications such as orbital infections, epidural and subdural empyema, meningitis, cerebritis, cavernous sinus thrombosis, brain abscess and death can occur. It also addresses points and pitfalls concerning surgery to remove odontoma.
Keywords: Extensive complex odontoma, Transient diplopia, Chronic sinusitis
Introduction
The term odontoma was first used by Paul Broca in 1867 [1]. Currently odontoma is considered to be a hamartomatous malformation rather than true neoplasm [2]. Odontoma is often associated with impacted teeth or retained deciduous teeth.
Sinusitis of dental origin is a relatively frequent disease and is caused by extension of periapical abscesses to the maxillary sinus or by secondary infections from oro-antral fistulae. Cases of sinusitis and transient diplopia resulting from an odontoma in the maxillary sinus are rare. Here is a rare presentation of complex odontoma in the maxillary sinus pushing 3rd molar near the orbital floor causing transient diplopia in upward gaze occasionally and chronic sinusitis.
The treatment of an odontoma consists of surgical removal. Small odontomata can be removed easily; however, removing larger odontomata may be difficult. To prevent complications, several rules and principles for successful atraumatic removal of large maxillary odontomata must be followed.
Case Presentation
A 20 year old female presented with pain and foul smelling discharge in relation to left posterior teeth in the upper jaw. She also complained of unilateral nasal obstruction, fetid breath, presence of purulent secretion during sinusitis episodes and having double vision in upward direction occasionally since 3 years. Clinically presenting an erupting hard, yellowish-brown mass, a tooth like structure was present in relation to 27 with inflamed gingiva and deep pocket, 26 was Grade II mobile and 28 was absent (Fig. 1).
Fig. 1.

Intraoral view showing a hard yellowish mass associated with the absence of upper left 2nd and 3rd molars
Panoramic radiography revealed a radiopaque lesion measuring 6 cm × 4 cm approximately in the left maxilla extending from alveolar ridge to the maxillary sinus in relation to the 27 region, encircled by a radiolucent band, distal to 26 there was complete bone loss, 28 was impacted in an unusual position near the floor of the orbit. The sinus lining was thickened (Fig. 2).
Fig. 2.

Preoperative panaromic radiograph showing a radiopaque lesion encircled by radiolucent band in the left maxillary sinus, 3rd molar near orbital floor, thickened sinus lining and complete bone loss distal to 2nd molar
Surgical Technique
Antibiotic therapy and topical nasal decongestant was started. After control of infection, a full thickness trapezoid muco-periosteal flap was reflected bucally from the line angle of the second left premolar, extending posteriorly past the area of the first, second and third molars over the tuberosity and upward. Using an electric drill, a thin layer of the bone overlying the odontoma was removed, creating an oval window several millimeters behind the distal root of the second premolar and above the crest of tuberosity, thus exposing the calcified amorphous mass. Extraction of 26 was performed. The mass was removed using a straight elevator, pushing it anteriorly and downward. Removal of impacted 28, and thickened sinus lining curettage was done via intraoral access. Antral packing and nasal antrostomy were performed. The buccal pad of fat graft facilitated primary closure of the surgical wound, minimizing the risk of dehiscence and consequent occurrence of an oral sinus fistula (Fig. 3).
Fig. 3.
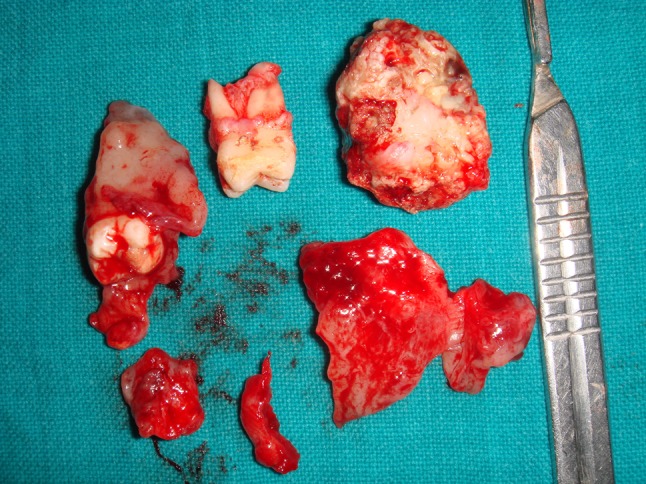
Excised mass of odontoma, 2nd and 3rd molars with sinus lining
Histopathological analysis confirmed complex odontoma.
The postoperative follow-up was satisfactory with the patient developing no oral sinus fistula, showing no signs of maxillary sinusitis and no episode of transient diplopia.
Discussion
The aim of selecting and highlighting this case is that this case appropriately displays limits of an entire spectrum which can clinically manifest under this entity and its management.
Sales and Cavalcanti [3] mentioned odontomata may cause a series of disorders and sequelae, such as problems related to their interference with the process of tooth eruption, ectopic eruption, displacement and malformation of adjacent teeth, diastema, anodontia, and growth pressure exerted by the odontoma may cause pain, devitalization, and tooth and bone resorption. In the present case, the patient presented sequelae, including the absence of the permanent posterior teeth important for occlusion, as well as significant bone loss.
Lee and Park [4] mentioned that odontomata preferentially involve the posterior portion of the jaws and might be associated with an unerupted or missing tooth and are of several millimeters to 3–4 cm in diameter. The present case can be considered rare because of its large size (approximately 6 cm in diameter), in addition to its atypical location, occupying the posterior region of the maxillary antrum and the cause of pushing 3rd molar near the orbital floor.
In a metaanalysis of the epidemiology and clinical manifestations of 3065 odontomata by Sanchez et al. [5] odontomata in the maxillary sinus may cause pain, facial asymmetry and chronic congestion of the sinus. Along with same clinical features, an additional symptom of transient diplopia was observed in the present case in which the odontoma caused marked discomfort to the patient due to the communication between the maxillary sinus and oral cavity caused by exposure of the tumor. Transient diplopia with sinus infection may be the result of significant swelling in the sinus cavity.
Lee and Park [4] mentioned that the radiopaque image of complex odontomata in the maxillary sinus can be confused with various lesions such as cementoblastomas, osteomas, ossifying fibromas, and osteoblastomas, as well as of other odontogenic tumors such as calcifying epithelial odontogenic tumors and ameloblastic fibro-odontomas. In the present case the lesion had well-defined borders and a radiolucent halo around the radiopaque mass which is a characteristic finding.
Korpi et al. [6] managed odontomata situated in close proximity to maxillary sinus by the Le Fort I osteotomy via down fracture. As it is a cumbersome procedure the present case was managed by traditional conventional approach through the lateral walls of the maxillary sinus. The postoperative healing was predictable.
Points for Concern of Management
Compound odontomas are relatively simple to treat, similar to removing impacted teeth. However, it may be difficult to access large complex odontomata in the posterior maxilla like the one in the present case. General anesthesia or IV sedation may be required in such cases, as extensive retraction of the lip and cheek often is necessary. A bite block should not be used to open the mouth; as the mouth opens, the coronoid process of the mandible comes forward adjacent to the maxillary tuberosity. Maximum opening of the mouth will restrict access to the posterior maxilla. Instead, a large triangular mucoperiosteal flap with posterior extension, a trapezoidal flap should be employed to deglove the maxillary tuberosity and enhance vision.
Dental or operatory lamps are difficult to focus in this area, so a fiberoptic head lamp is recommended. When attempting to reflect full-thickness flaps in this area, the periosteium should not perforated, as the buccal fat pad may be herniated through the flap into the operating field, hampering visualization and complicating surgery. An electric drill should be used in these situations, as the blast of air from tip of an air drill or turbine may lead to tissue emphysema.
It is prudent to preserve the bony crest of the maxillary tuberosity. To do so, the bone is removed from above by creating a buccal window (cut out maxillary bone) several millimeters smaller than the diameter of the odontoma, through which the tumour can be removed. To ensure bone formation and prevent postoperative pocket formation, 1.0–2.0 mm of bone should be left distal to the remaining tooth anterior to the lesion.
Conclusion
The present case can be considered unique because when obstruction of sinus drainage is evident, one should be completely aware of serious complications such as orbital infections, epidural and subdural empyema, meningitis, cerebritis, cavernous sinus thrombosis, brain abscess and death can occur. It also addresses points and pitfalls concerning surgery to remove odontoma.
Acknowledgments
We are thankful to Mr. Sham Lal Gupta Chief Eng. Retd. for his invaluable support.
Conflict of interest
None.
References
- 1.Howard RD. The unerupted incisor. A study of the post operative eruptive history of incisors delayed in their eruption by supernumerary teeth. Dent Pract Dent Rec. 1967;17:332–341. [PubMed] [Google Scholar]
- 2.Budnick SD. Compound and complex odontoma. Oral Surg Oral Med Oral Pathol. 1976;42:501–505. doi: 10.1016/0030-4220(76)90297-8. [DOI] [PubMed] [Google Scholar]
- 3.Sales MA, Cavalcanti MG. Complex odontoma associated with dentigerous cyst in maxillary sinus: case report and computed tomography features. Dentomaxillofac Radiol. 2009;38:48–52. doi: 10.1259/dmfr/95388644. [DOI] [PubMed] [Google Scholar]
- 4.Lee CH, Park GJ. Complex and compound odontomas are clinico-pathological entities. Basic Appl Pathol. 2008;1(1):30–33. doi: 10.1111/j.1755-9294.2008.00008.x. [DOI] [Google Scholar]
- 5.Sanchez OH, Berrocal MIL, González JMM. Metaanalysis of the epidemiology and clinical manifestations of odontomas. Med Oral Patol Oral Cir Bucal. 2008;13(11):E730–E734. [PubMed] [Google Scholar]
- 6.Korpi JT, Kainulainen VT, Sandor GKB, Oikarinen KS. Removal of large complex odontoma using Le Fort I osteotomy. J Oral Maxillofac Surg. 2009;67:2018–2021. doi: 10.1016/j.joms.2009.04.105. [DOI] [PubMed] [Google Scholar]


