Abstract
The purpose of this paper is to discuss the current diagnosis of Eagle’s syndrome (elongated styloid process) and to discuss a new and a much simpler technique for styloidectomy with an intraoral approach which can be used in local anesthesia. Easiness to perform, non-association of any anesthetic complications and avoidance of an extraoral scar dictates that this approach can be practiced much safely in patients with elongated styloid process.
Keywords: Eagle’s syndrome, Styloidectomy, Surgical technique
Introduction
Eagle’s syndrome, also known as elongated styloid process, is a condition that may be the source of craniofacial and cervical pain. It is known to occur when either the total length of the styloid process is longer than 25 mm [1] or when stylohyoid or stylomandibular ligaments [2, 3] are ossified. Its incidence has been reported variably in literature (1.0–84.4 %) [1, 4]. The symptoms related to Eagle’s syndrome can be confused with those attributed to a wide variety of facial neuralgias and/or oral, dental and TMJ diseases but adequate history, proper clinical and radiological examination and sound knowledge of mimicking pathology can help in diagnosing the disease. In this paper, Eagle’s syndrome presenting as pain of dental origin is described and a new simpler intraoral surgical procedure has been discussed to treat the same.
Case Report
Two patients presented with a complaint of discomfort while swallowing and dull pain behind the maxillary arch (left side in both the cases). The pain radiated to the mastoid areas and was lessened on bending the neck to the ipsilateral side. There was associated dysphagia, headache, discomfort on extension of the tongue.
Diagnostic Work Up
The patient’s past medical history was non-contributory and there were no extraoral findings. All the other possible causes of pain that is, odontogenic, oral lesion, dental, neuralgic and muscular, and temporomandibular diseases were ruled out.
The differential diagnosis was based upon the knowledge of the conditions that mimicked the kind of pain, which were orderly excluded to arrive at a conclusive diagnosis. The differential diagnosis included but was not limited to Glossopharyngeal neuralgia, Superior laryngeal neuralgia, Occipital neuralgia, Sphenopalatine neuralgia, Nervus intermedius neuralgia, Cephalalgias migraine, Cervicogenic headache, Oromandibular disorders temporo-mandibular joint disorders, impacted, Unerupted or distorted third molar, Faulty dental prostheses, Sialolithiasis, Tonsillitis, Otitis Mastoiditis, Foreign bodies, Inflammatory and neoplastic processes in the oropharyngeal and esophageal areas and other psychosomatic diseases.
Intra-oral palpation [5] of the pharyngeal area was done using index finger under local anesthesia using 15 % lignocaine spray in pharynx. The palpation of pharyngeal area revealed a pointed bony outgrowth, that was felt below the pharyngeal soft tissues. The tenderness on palpation in both the cases revealed elongated styloid processes which was absent on contralateral side and therefore the diagnosis of Elongated styloid process was made.
The diagnosis was supported on orthopantomogram which was showing elongated styloid process with an “s” shaped bend in the styloid, suggestive of forward course of styloid making it travel towards the pharynx and hence impinging in pharynx and also making it palpable intraorally (Figs. 1, 9).
Fig. 1.

Elongated styloid in OPG with forward bending on left side
Fig. 9.

Elongated styloid in OPG with forward bending on left side
Styloid process is always present, but is not always visible on routine radiograph if normal in length, because it overlies other skeletal structures [6]. CT provided complimentary information to that of plain radiography (Fig. 2).
Fig. 2.

Bilaterally elongated styloids in CT
Surgery
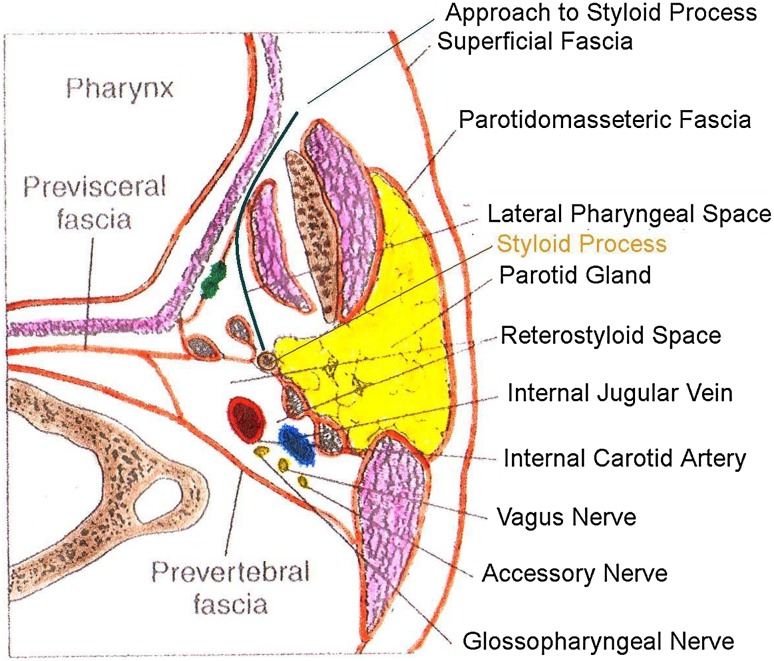
Anatomy (Fig. 3)
Fig. 3.
Approach to styloid
The styloid process is a thin, elongated, cylindrical bony projection that is situated anteromedially to the mastoid process. Its length varies from 2 to 3 cm. Posterior to the styloid is the facial nerve, which emerges from the stylomastoid foramen. Medial to styloid, moving posterior to anterior are the internal jugular vein (with XI, XII, X and IX cranial nerves) and the internal carotid artery. Medial to the tip of the styloid process are the superior constrictor muscle and the pharyngobasilar fascia, which lie adjacent to the tonsillar fossa. Lateral to the tip of the process is the external carotid artery that bifurcates into superficial temporal and maxillary arteries. The stylohyoid ligament extends from the styloid to the lesser cornu of hyoid bone.
Technique
After being diagnosed as cases of Eagle’s syndrome secondary to elongated styloid process, the patients underwent surgical removal of the elongated styloid bone through an intraoral approach.
Preparation
After through investigations, patients were scheduled for surgery under local anesthesia. Premedication was given in the form of Diazepam 10 mg i.m. and Atropine Sulfate i.m. Preoperative prophylactic antibiotics were given in the form of Amoxycilliin 500 mg oral, 1 h before surgery which was then continued as three times a day for 5 days.
Anesthesia
Local anesthesia was given as submucosal infiltration along medial aspect of ascending ramus and vicinity of styloid process after giving intraoral mandibular nerve block using 2 % lignocaine with 1:80000 adrenaline.
Incision
Incision is given along the ascending border of the ramus, cutting through mucosa and submucosa (Figs. 4, 10). Then blunt dissection is done with curved hemostat, thereby dissecting posteriorly, medial to the medial pterygoid muscle and lateral to the superior constrictor muscle (Fig. 3). Styloid apparatus is exposed and incision is given along the periosteum (without disturbing the styloid attachments) to deglov the styloid process (Figs. 5, 11). The naked styloid was grasped between two hemostats and was fractured (Fig. 6). The fractured process was freed and was removed (Figs. 7, 12). The muscles and the mucosa were then closed to attain a perfect closure (Figs. 8, 13).
Fig. 4.

Incision along ascending border of ramus
Fig. 10.
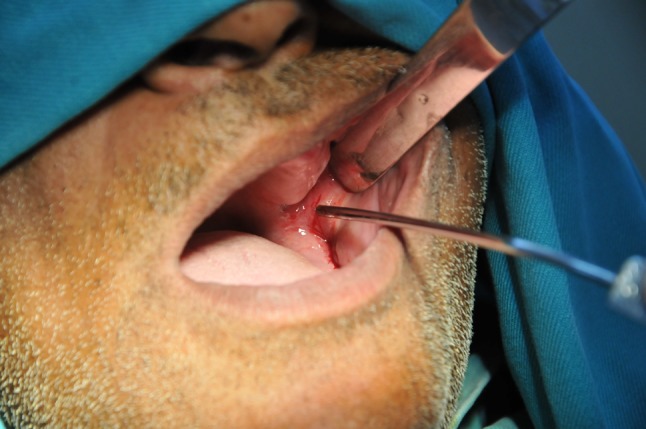
Incision to styloid
Fig. 5.

Styloid process exposed intraorally
Fig. 11.

Styloid process exposed intraorally
Fig. 6.
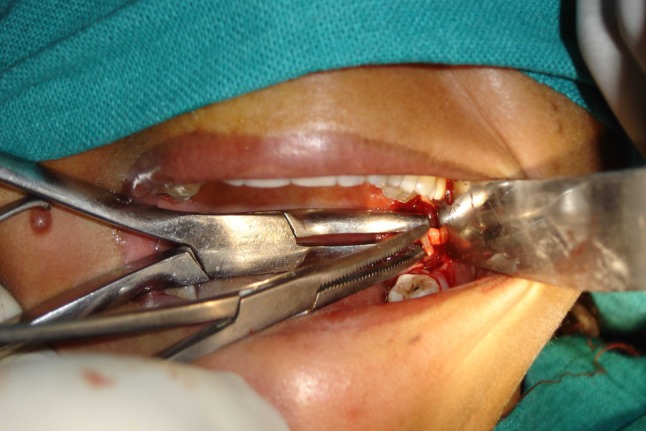
Styloid grasped between hemostats and fractured
Fig. 7.

Fractured styloid delivered intraorally
Fig. 12.
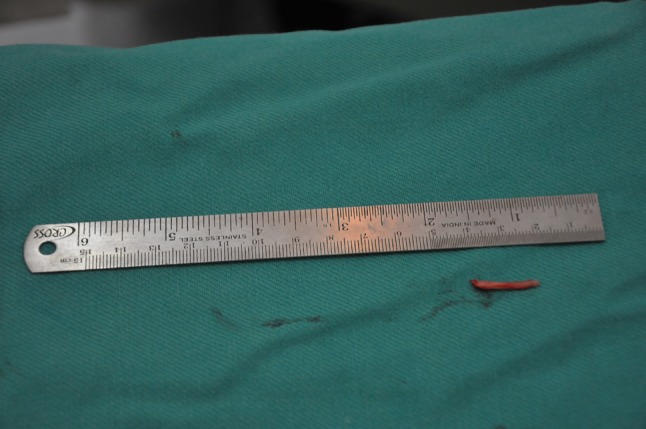
Styloid fractured and delivered
Fig. 8.

Closure done
Fig. 13.

Closure done
Postoperative Care and Follow Up
Patients were given postoperative analgesics (Ibuprofen 400 mg TDS for 3 days) and were discharged after 6 h with appropriate postoperative instructions. Sutures were removed on the seventh postoperative day and regular follow ups were done.
Results
Surgery was uneventful, and follow ups revealed that the patients had remained symptom free after surgery.
Discussion
Eagle’s syndrome is an aggregate of symptoms that includes recurrent throat pain, foreign body sensation, dysphagia, and/or facial pain as a direct result of an elongated styloid process or calcified stylohyoid ligament. Although approximately 4 % of the population is thought to have an elongated styloid process, only a small percentage (between 4 and 10.3 %) of this group is thought to actually be symptomatic [7].Radiographic studies have shown that a normal styloid process is generally less than one inch (about 2.5 cm) in length [8]. The thickness of a normal styloid process varies between 2 and 5 mm [6]. Elongated styloid processes or one with bent course in a forward direction can elicit oropharyngeal pain not pertaining to impacted or unerupted third molars or dental caries or any other cause.
Careful palpation of the tonsillar fossa which elicits the patient’s pain and a panoramic radiography examination which can show a correct picture of the elongated styloid process confirms the diagnosis.
Treatment for Eagle’s Syndrome include nonsurgical treatments comprising of reassurance, nonsteroidal anti-inflammatory medications, and injections of steroid [2, 9] and local anesthetics (1 % lidocaine or novocaine) at the hyoid bone’s inferior cornu or into the inferior tonsillar fossa which is the most common non-surgical treatment. Its effectiveness has not been substantiated [10].
Among surgical treatments, transpharyngeal [11] manipulation with manual fracturing of the elongated styloid process has been described as an office procedure performed under local anesthesia of the transpharyngeal area [12]. This treatment is associated with poor outcome due to stylalgia [13]. Hemorrhage of major vessels cannot be managed appropriately when using this approach [14, 15]. In addition, the glossopharyngeal nerve may be damaged [16]. Also, it has been heavily criticized because of the increased risk of deep space neck infection and poor visualization of the surgical field (must be performed through the mouth).
Another surgical treatment advocated is the extraoral [17] approach which can be criticized because of its prolonged duration, morbidity and involvement of adjacent anatomical structures. Two reported surgical complications are internal carotid thrombosis [19] and subcutaneous cervical emphysema [18]. Nevertheless, some authors [14, 15], advocate the extraoral approach in cases where the styloid process has to be completely removed to improve access to other structures. This approach also improves visualization in case of hemorrhage and the risk of deep cervical infection is reduced.
Although both procedures are effective in removing an elongated styloid process, but none of the two is free from complications.
Our technique differs from the intraoral transpharyngeal approach in that, dissection is kept lateral to superior constrictor, so there is no need of tonsillectomy and dissection becomes less time consuming. This technique not only benefits the patient of not having an extraoral scar, but also in being simpler.
It is important to note here that in the OPG (Figs. 1, 9), the styloid process is not reaching the angle of the mandible (Figs. 10, 11). It is because of a sharp bend in the middle of the styloid process which caused tip to be located more anteriorly causing impingement on the lateral pharyngeal wall (which lies in front of the styloid tip) and hence discomfort and pain to the patient. Further, the osteotomy in our case, is not done at the stump (base), thereby showing the length to be 3 cm in the picture (Figs. 7, 12).
In literature, haemorrhage of major blood vessels [14, 15] and possible risk of glossopharyngeal nerve damage has limited the use of intraoral approach but with our technique, by careful dissection and restraining to the anterior compartment of the lateral pharyngeal space which houses no vital structures (vital structures are a part of reterostyloid space—Fig. 3), these complications can be avoided (Fig. 13).
References
- 1.Eagle W. Elongated styloid process. Arch Otolaryngol. 1958;67:172–176. doi: 10.1001/archotol.1958.00730010178007. [DOI] [PubMed] [Google Scholar]
- 2.Eagle WW. Elongated styloid process: report of 2 cases. Arch Otolaryngol. 1937;25:584. doi: 10.1001/archotol.1937.00650010656008. [DOI] [PubMed] [Google Scholar]
- 3.Eagle WW. Elongated styloid process. Arch Otolaryngol. 1948;47:630. doi: 10.1001/archotol.1948.00690030654006. [DOI] [PubMed] [Google Scholar]
- 4.Eagle W. The symptoms, diagnosis and treatment of the elongated styloid process. Am Surg. 1962;28:1–5. [PubMed] [Google Scholar]
- 5.Ying-lin Z, et al. Styloid process syndrome: length and palpation of the styloid process. Chin Med J. 1987;100:56–57. [PubMed] [Google Scholar]
- 6.Lentini A, et al. Gli aspetti clinici e radiologici delle anomalie dell’apparato stilo-joideo. Radiol Med. 1975;61:337–364. [Google Scholar]
- 7.Eagle WW. Elongated styloid process: symptoms and treatment. Arch Otolaryngol. 1958;64:172. doi: 10.1001/archotol.1958.00730010178007. [DOI] [PubMed] [Google Scholar]
- 8.Correl R, Jensen J, Taylor J, Rhyne R. Mineralization of the stylohyoid–stylomandibular ligament complex: a radio-graphic incidence study. Oral Surg Oral Med Oral Pathol. 1979;48:286–291. doi: 10.1016/0030-4220(79)90025-2. [DOI] [PubMed] [Google Scholar]
- 9.Jan A. Stylohyoid syndrome (letter) JPMA. 1989;39:23. [PubMed] [Google Scholar]
- 10.Montalbetti L, Ferrandi D, Pergami P, Savoldi F. Elongated styloid process and Eagle’s syndrome. Cephalalgia. 1995;15:80–93. doi: 10.1046/j.1468-2982.1995.015002080.x. [DOI] [PubMed] [Google Scholar]
- 11.Birke W. Therapy of the styloid syndrome. Stomatol Der DDR. 1979;26:441–444. [PubMed] [Google Scholar]
- 12.Marano P, Fenster G, Gosselin C. Eagle’s syndrome necessitating bilateral styloid amputation. Oral Surg. 1972;33:874–878. doi: 10.1016/0030-4220(72)90175-2. [DOI] [PubMed] [Google Scholar]
- 13.Monsour P, Young W, Barnes P. Styloid–stylohyoid syndrome: a clinical update. Aust Dent J. 1985;30:341–345. doi: 10.1111/j.1834-7819.1985.tb02527.x. [DOI] [PubMed] [Google Scholar]
- 14.Chase D, et al. Eagle’s syndrome: a comparison of intraoral versus extraoral surgical approaches. Oral Surg Oral Med Oral Pathol. 1986;62:625–629. doi: 10.1016/0030-4220(86)90253-7. [DOI] [PubMed] [Google Scholar]
- 15.Yoshimura Y, Oka M. Does Eagle’s syndrome always require operative intervention for treatment? Two case reports. Cranio. 1989;7:235–238. doi: 10.1080/08869634.1989.11678290. [DOI] [PubMed] [Google Scholar]
- 16.Watkins A. Elongated styloid process and its treatment. Med J Aust. 1966;2:448–449. doi: 10.5694/j.1326-5377.1966.tb73712.x. [DOI] [PubMed] [Google Scholar]
- 17.Loeser L, Caldwell E. Elongated styloid process: a cause of glossopharyngeal neuralgia. Arch Otolaryngol. 1942;36:198–202. doi: 10.1001/archotol.1942.03760020034003. [DOI] [Google Scholar]
- 18.Riediger D, Ehrenfeld M. Pathogenesis and clinical manifestation of the styloid syndromeé. Dtsch Zahnaerztl Z. 1989;44:968–970. [PubMed] [Google Scholar]
- 19.Strauss M, Zohar YLN. Elongated styloid process syndrome: intraoral versus external approach for styloid surgery. Laryngoscope. 1985;95:976–979. [PubMed] [Google Scholar]