Abstract
Osteochondroma or solitary osteocartilagenous exostosis is characterized by cartilage-capped osseous lesion, protruding from the surface of affected bone. It is one of the most common benign bone tumor in axial skeleton and infrequent in maxillofacial skeleton. This paper describes a giant osteochondroma of coronoid process in a 20 year old woman, presented with limited mouth opening (15 mm inter incisal distance) and pain without any facial swelling, asymmetry and TMJ problems. Based on clinical examination, panoramic radiography and computed tomography images a provisional diagnosis of osteoma or osteochondroma of the coronoid process was made. Under general anaesthesia through intra oral approach excision of the bony tumor along with the coronoid process was performed, with recovery of mouth opening up to 40 mm immediately following surgery. The histopathology of excised specimen revealed features suggestive of osteochondroma. After follow up period of 54 months patient is symptom free. Here we are presenting and discussing the complete diagnostic and treatment aspect of this unusually large osteochondroma of coronoid process of mandible.
Keywords: Coronoid process, Osteochondroma, Diagnosis, Treatment
Introduction
Osteochondroma or solitary osteocartilagenous exostosis is one of the most common benign bone tumor in axial skeleton and infrequent in cranio-facial bones. The embryonic development of condyle, coronoid and symphysis from cartilaginous ossification makes this area the most frequent facial site of this type of tumor. Osteochondromas are slow growing tumors that parallel the skeleton growth of the individual. Coronoid process is rare site for osteochondroma. The diagnosis is based on clinical examination, panoramic radiograph, Computed Tomography (CT) images and histopathological features. We report a unique case of giant (large) osteochomdroma of the coronoid process with progressive limited mouth opening (15 mm inter incisal distance) and pain without any facial asymmetry, swelling and TMJ problems.
Case Report
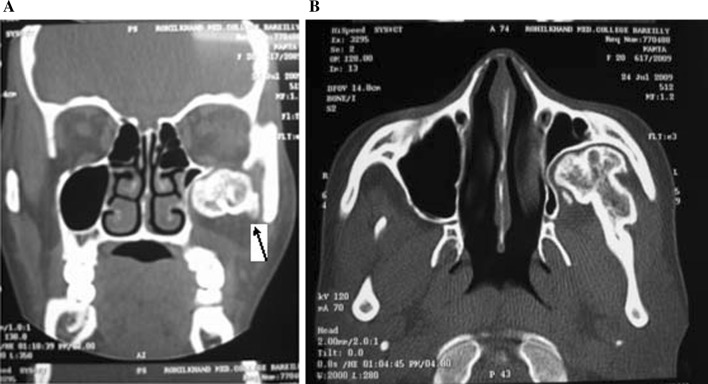
A 20 year old female patient was referred to the Department of Oral and Maxillofacial Surgery with progressive limitation of mouth opening from the last 1 year, with accompanying pain on mouth opening. Physical and extraoral examination did not reveal any relevant signs apart from limited mouth opening, without any facial asymmetry and swelling. The interincisal distance was 15 mm. There was no associated TMJ complaints. Panoramic radiograph revealed a large radiopaque mass as an extension from coronoid process measuring about 4 cm at widest diameter on left side (Fig. 1). Coronal and axial CT scan confirmed a large bony outgrowth arising from the coronoid process, displacing the left maxillary posterior and lateral walls (Fig. 2). The dimensions of the maxillary sinus appear to be reduced on left side in comparision to right side, due to compression from the bony tumor. Based on clinical and radiographic images a provisional diagnosis of osteoma or osteochondroma of the coronoid process was made. Following routine investigations and informed consent the patient was taken under general anesthesia and a surgical procedure was carried through intraoral approach. Incision was made along the anterior border of ramus, following external oblique ridge. The mucoperiosteal flap was raised both medially and laterally. Blunt dissection was performed to strip the temporalis muscle (myotomy) followed by excision of bony tumor along with the coronoid process (coronoidectomy) using fissure bur and chisel (Fig. 3). As there was cleavage present between zygomatic arch and tumor, intraoral retrieval was achieved without much resistance. Mouth opening was recovered up to 40 mm immediately following surgery. The histopathological features of the excised specimen shows the presence of clusters of chondrocytes in the cartilaginous cap, arranged in parallel, oblong, lacunar spaces, similar to those of normal epiphysial cartilage. The deeper layer shows endochondral ossifications and transition to cancellous bone with intertrabecular red or fatty marrow suggesting diagnosis of osteochondroma (Fig. 4). After follow-up period of 54 months the patient was found to be asymptomatic (Fig. 5).
Fig. 1.

Panoramic radiograph showing tumour on left coronoid process
Fig. 2.
A Coronal CT (arrow) image showing bony outgrowth from morphologically normal coronoid process. B Axial CT scan showing well defined bony outgrowth from coronoid process with continuity of cortex and medulla with that of tumour and displacing left maxillary posterior and lateral walls
Fig. 3.

Excised specimen
Fig. 4.
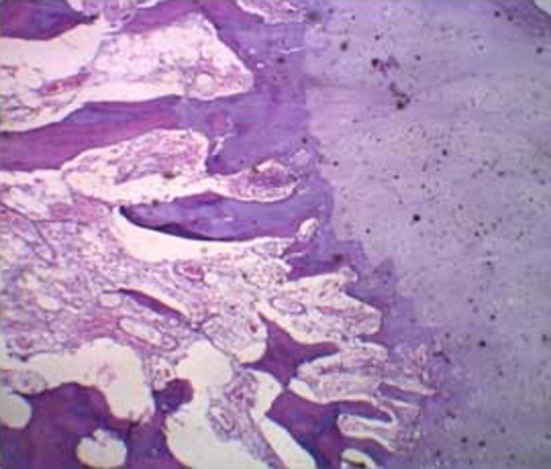
The photomicrograph showing the peripheral cartilaginous portion enclosing chondrocytes in the lacune and the innermost areas of mineralized bone. (Hematoxylin and Eosin ×4 magnification)
Fig. 5.

Post-operative OPG
Discussion
Osteochondroma is one of the most common and slow growing benign tumor arising from cortex of bone and contains a prominent cap of cartilage tissue. It usually occurs in long bones at or near the epiphyseal-metaphyseal junction, the proximal metaphysis of tibia and distal metaphysis of femur are more commonly involved [1]. This was first described by French anatomist Oscer Jacob in 1899. In cranio facial skeleton the tumor has been reported in cranial base, posterior maxillary surface [2], maxillary sinus [3], zygomatic arch [4], body [5], symphysis [6], mandibular condyle and coronoid [7]. In mandible it is most frequently encountered in condyle and coronoid process [7]. The embryonic development of condyle, coronoid and symphysis from cartilaginous ossification makes this area the most frequent facial site of this type of tumor. Osteochondromas are slow growing tumors that parallel the skeletal growth of the individual and usually cease growth after puberty. The origin of tumor is controversial; developmental, neoplastic, reparative and traumatic etiologies have all been suggested. Several theories about the etiology of these tumors have been proposed. In 1981 Virchow postulated the physeal theory [8]. In 1920 Keith proposed defect in the perichondrial ring surrounding the physis as the cause of osteochondroma [9]. Muller’s periosteal theory states exostosis are produced by small nests of cartilage derived from the cambium layer of periosteum [10]. Sicher proposed that continuous activity of tendons inserted in the coronoid stimulate a hyperplastic development of embryonic cells with chondrogenic potential [11]. Lichtenstein theory proposes that periosteum has the potential to develop osteoblasts and chondroblasts [12]. Several osteochondromas located throughout the skeleton are observed in hereditary multiple exostosis conditions (HME) [6], an autosomal dominant disorder with multiple exostosis causing bone deformities and impaired joint mobility that may be complicated by pathological fractures and compression of nerves, vessels and tendons. Osteochondroma associated with Langer giedion syndrome is accompanied by learning difficulties, redundant skin, multiple exostosis, characteristic facial features and cone shaped phalanges [13]. Sarcomatous changes are rare in solitary osteochondroma (1 %) but does occur in approximately 11 % of cases of multiple hereditary osteochondromas [14].
The diagnosis of osteochondroma of the coronoid process was based on clinical examination, radiographic appearance, CT scan images and microscopic analysis. The distinctive signs of coronoid osteochondroma are slow growing lesion with progressive limitation of mouth opening, pain, extraoral swelling and facial deformity.In case of limited mouth opening due to coronoid process, the patient projects complaint in that region, more in TMJ [15]. In our case there was no extaroral swelling and facial deformity due to medial growth of tumour from the coronoid process.
The panoramic radiograph of osteochondroma of the coronoid process usually shows a sessile or pedunculated globular bony outgrowth from the margins with the normal outline of coronoid being maintained. However, radiographic appearance of osteochondroma can usually be pathognomic. The radiograph of osteochondroma shows mixed density due to cartilage components and calcification phenomenon coexisting in the lesion. When cartilage component is more the radiographic appearance is of low density image, when most of the cartilage component ossify the density of the lesion is increased [16].
Osteochondroma must be differentiated from hyperplasia. Radiographically, osteochondroma appears as a globular projection extending from the margins of the coronoid with normal outline of the coronoid being maintained. Hyperplasia is manifested radiographically as an enlarged coronoid process. In addition to panoramic view, Water’s view radiograph is useful to show coronoid tumor and its relation to the wall of maxillary sinus and zygoma [17].
As complement to clinical examination, panoramic radiograph, CT images play a decisive role in diagnosing the exact site, size, and shape of the tumor, relationship to adjacent structures, differential diagnosis and treatment planning. CT scan shows well defined bony outgrowth, with continuity of cortex and medulla of the parent bone with that of the tumor a diagnostic feature of osteochondroma [18]. Although CT is not best imaging modality for evaluation of non calcified cartilage caps, calcified cartilage demonstrates high accuracy on CT. Osteochondroma must be distinguished from hyperplasia. CT images play important role in differentiating osteochondroma of the coronoid process from hyperplasia. Osteochondroma is seen as growth arising from the morphologically normal coronoid while, hyperplasia is seen as enlargement of coronoid process.
Histologically the diagnosis of osteochondroma includes condrocytes of cartilaginous cap arranged in clusters parallel to lacunar spaces. Differential diagnosis of osteochondroma includes osteoma, benign osteoblastoma, chondroma, chondroblastoma and bony hyperplasia.
The treatment of osteochondroma of the coronoid process was temporalis muscle myotomy and coronoidectomy. In contrast to mandibular condylar osteochondroma that does require reconstruction. Recurrence of osteochondroma of coronoid and malignant transformation are extremely rare [19].
The surgical approach for removal of tumor from coronoid process can be either extra oral coronal approach or intra oral approach. The intra oral approach has an advantage of direct access to the lesion without facial nerve injury. If the tumor of the coronoid process is trapped in zygomatic arch the coronal approach is used for tumor resection which has advantage of better access and visualization.
Conclusion
The diagnosis of osteochondroma should be based not only on plain radiography and microscopic analysis but special emphasis on CT scan should be given to make the diagnosis much more reliable. The osteochondroma of the coronoid process may arise medially or laterally from the tip of the coronoid process and may have diverse shapes on radiographs. However, in our case the lesion was huge and was present on the medial aspect of the coronoid process with a plane of cleavage between zygomatic arch and the tumor, retrieval of tumor intraoraly was achieved with minimal to nil resistance.
Acknowledgments
Conflict of interest
We hereby declare that there is no conflict of interest and our study is not funded by any source or agency.
References
- 1.Mirra JM. Bone tumors: clinical, radiographic and pathologic correlations. Philadelphia: Lea & Febiger; 1989. pp. 1626–1660. [Google Scholar]
- 2.Brady FA, Sapp JP, Christensen RE. Extracondylar osteochondromas of the jaws. Oral Surg Oral Med Oral Pathol. 1978;46:658–668. doi: 10.1016/0030-4220(78)90462-0. [DOI] [PubMed] [Google Scholar]
- 3.Traub DJ, Marco WP, Eisenberg E, Barrows G. Osteochondroma of the maxillary sinus: report of a case. J Oral Maxillofac Surg. 1990;48:752–755. doi: 10.1016/0278-2391(90)90066-B. [DOI] [PubMed] [Google Scholar]
- 4.Pool JW, Tilson HB, Thornton WE, Steed DL. Osteochondroma of the zygomatic arch: report of a case. J Oral Surg. 1979;37:673–675. [PubMed] [Google Scholar]
- 5.Miyawaki T, Kobayashi M, Takeishi M, Uchida M, Kurihara K. Osteochondroma of the mandibular body. Plast Reconstr Surg. 2000;105:1426–1428. doi: 10.1097/00006534-200004040-00023. [DOI] [PubMed] [Google Scholar]
- 6.Tanaka E, Lida S, Tsuji H, Kogo M, Morita M. Solitary osteochondroma of the mandibular symphysis. Int J Oral Maxillofac Surg. 2004;33:625–626. doi: 10.1016/j.ijom.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 7.Kerscher A, Piette E, Tideman H, Wu PC. Osteochondroma of coronoid process of the mandible. Oral Surg Oral Med Oral Pathol. 1993;75:559–564. doi: 10.1016/0030-4220(93)90224-R. [DOI] [PubMed] [Google Scholar]
- 8.Virchow R. Ueber multiple exostosen. mit Vorlegung von Praparaten Berl Klin Wochenschr. 1891;28:1082–1085. [Google Scholar]
- 9.Keith A. Studies on the anatomical changes which accompany certain growth disorders of the human body. J Anat. 1920;54:101–110. [PMC free article] [PubMed] [Google Scholar]
- 10.Muller E. Uber hereditare multiple cartilaginare Exostosen und Ecchondrosen. Beitr Pathol Anat. 1913;57:232–313. [Google Scholar]
- 11.Weinmann JP, Sicher H. Bone and bones: fundamentals of bone biology. St. Louis: CV Mosby; 1995. pp. 88–126. [Google Scholar]
- 12.Litchtenstein L. Bone tumors. St Louis: CV Mosby; 1977. pp. 17–29. [Google Scholar]
- 13.Morioka D, Suse T, Shimizu Y, Ohkubo F, Hosaka Y. Langer giedion syndrome associated with submucous cleft palate. Plast Reconstr Surg. 1999;103:1458–1463. doi: 10.1097/00006534-199904020-00015. [DOI] [PubMed] [Google Scholar]
- 14.Jaffe HL. Tumors and tumerous conditions of the bones and joints. Philadelphia: Lea & Febiger; 1961. p. 150. [Google Scholar]
- 15.Villanueva J, Gonzalez A, Cornejo M, Nunez C, Encina S. Osteochondroma of the coronoid process. Med Oral Pathol Oral Cir Bucal. 2006;11:E289–E291. [PubMed] [Google Scholar]
- 16.Zhang J, Wang H, Li X, Li W, Wu H, Miao J, Yuan X. Osteochondromas of the mandibular condyle: variance in radiographic appearance on panoramic radiographs. Dentomaxillofac Radiol. 2008;37:154–160. doi: 10.1259/dmfr/19168643. [DOI] [PubMed] [Google Scholar]
- 17.Hernandez-Alfaro F, Escudero O, Marco V. Joint formation between an osteochondroma of the coronoid process and the zygomatic arch (Jacob disease): report of case and review of the literature. J Oral Maxillofac Surg. 2000;58:227–232. doi: 10.1016/S0278-2391(00)90345-8. [DOI] [PubMed] [Google Scholar]
- 18.Avinash KR, Rajagopal KV, Ramakrishnaiah RH, Carnello S, Mahmood NS. Computed tomographic features of mandibular osteochondroma. Dentomaxillofac Radiol. 2007;36:434–436. doi: 10.1259/dmfr/54329867. [DOI] [PubMed] [Google Scholar]
- 19.Emekli U, Aslan A, Onel D, Çizmeci O, Demiryont M. Osteochondroma of the coronoid process (Jacob’s disease) J Oral Maxillofac surg. 2002;60:1354–1356. doi: 10.1053/joms.2002.35742. [DOI] [PubMed] [Google Scholar]