Abstract
Osteomas are rare benign tumours in the bone. We describe a case of giant osteoma involving the lingual side of the ramus and body of mandible that recurred 8 years after its surgical treatment at another hospital. Surgical resection with reconstruction is the treatment of choice for this lesion. The clinicopathological features of osteoma are discussed and Gardner’s syndrome was excluded.
Keywords: Peripheral osteoma, Gardner’s syndrome, Segmental resection, Iliac bone graft, Mandible
Introduction
Osteomas are benign lesions composed of mature compact and/or cancellous bone that grows continuously. The pathogenesis of this tumour is currently unknown [1]. Both hamartomatous and neoplastic factors have been advocated, but no definite conclusion has been reported in any study so far.
Osteomas are of three forms: central, peripheral, or extraosseous. The central form derives from the endosteum and the peripheral form derives from the periosteum, whereas the extraosseous form develops in muscular tissue structures [2].
The most common location of the periosteal osteoma is the skull. However, lesions also occur in the mandible, especially on the lingual aspect of the body, angle and inferior border of the mandible [3].
Histologically, three types of osteoma can be identified: compact (ivory), cancellous (trabecula), and fibrous (spongy) [4].
The purpose of this article is to describe a giant osteoma involving almost half of the mandible with pain and disfigurement and complete removal of lesion by resection was the treatment option since recurrence was seen.
Case Report
A 16 year old female patient was referred to JSS Dental College and Hospital by a private dental practitioner with complaints of swelling and recurrent pain over the left posterior region of the mandible since 1 month and slowly increasing in size (Figs. 1, 2).
Fig. 1.

Pre operative lateral view
Fig. 2.

Pre operative intraoral view
Patient gave history of a swelling 8 years back in the same region where pieces of bones were surgically removed from the lingual side along with extraction of teeth on the same side in another hospital for which there was no record regarding the nature of the surgery performed.
A solitary well defined mixed radiopaque radiolucent lesion around 4 cm × 5 cm was found in the left mandibular ramus and angle region extending superiorly up to coronoid process on a orthopantomograph, mandibular left lateral view showed lingual cortical expansion (Figs. 3, 4).
Fig. 3.

Pre operative orthopantomograph
Fig. 4.

Mandibular left lateral radiograph
On palpation diffuse bony hard solitary swelling over alveolar ridge and external oblique ridge approximately 2 cm × 2 cm was noticed which was non tender on palpation with no signs of any surface mucosal changes. The lower left 2nd and 3rd molars were missing.
A single tender lymph node was palpable on the left submandibular region.
Under local anaesthesia incisional biopsy was done and histopathological study suggested cancellous osteoma.
The results of blood and serum chemistry were within the normal limits. Gardner’s syndrome was excluded in this patient as there were no relevant clinical findings as well as in ultrasound evaluation.
Informed consent was obtained preoperatively and under general anaesthesia the lesion was exposed through a left sided submandibular incision; segmental resection was done distal to left 1st premolar including the coronoid process (Fig. 5).
Fig. 5.
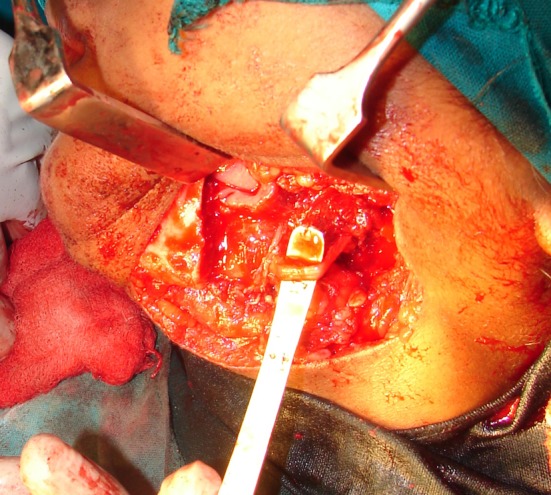
Intraoperative view showing resected surgical site along with preserved lingual nerve
Iliac bone graft was harvested and grafted with the help of long titanium 2.5 mm reconstruction ‘L’ plate (Fig. 6).
Fig. 6.

Intraoperative view showing placement of ‘L’ reconstruction plate with bone graft
The solitary lymph node was dissected and excised for histopathological study.
Patient underwent periodic clinical and radiographic follow-up and has remained free of tumor 3 years after surgery (Figs. 7, 8, 9, 10).
Fig. 7.

Post operative lateral view
Fig. 8.

Post operative front profile view
Fig. 9.

Post operative intraoral view
Fig. 10.

Post operative orthopantomograph
Gross Pathology
The specimen consisted of resected part of mandible about 6 cm × 6 cm × 2 cm with coronoid process. Surface showed bosellated exophytic bony growth measuring 4 × 3 cm (Figs. 11, 12).
Fig. 11.
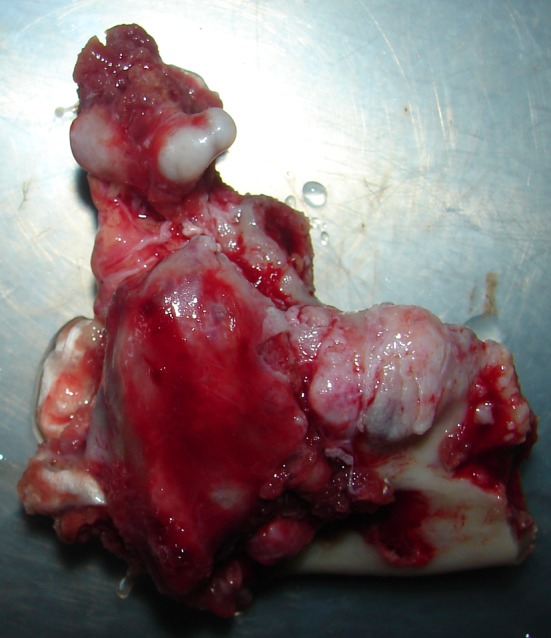
Lingual surface of resected mandible
Fig. 12.

Buccal surface of resected mandible
Microscopic Pathology
The mass showed lamellar bone with interspersed adipose tissue and marrow elements and an impression of a cancellous osteoma was given.
The excised lymph node showed fibrocollagenous tissue suggestive of reactive lymph node hyperplasia.
Discussion
Osteomas of the maxillofacial region are often detected on routine examination except in cases where lesion is sufficiently large to cause disfigurement and or functional discomfort to the patient.
Peripheral osteomas of the maxillofacial region affects mainly the frontal bone, mandible and the paranasal sinus [4].
Cases affecting the mandible have predilection to affect the angle and condylar region followed by the molar region of the mandibular body and the ascending ramus [5–8].
The clinical, radiological and histological features of the present case support the diagnosis of peripheral cancellous osteoma of posterior lingual mandible [8].
Peripheral osteomas almost certainly arise from the periosteum and as they grow they exhibit either a pedunculated or sessile bases that are continuous with the underlying cortical bones.
Studies suggest that peripheral osteoma can be completely cured by surgical intervention, and there is no recurrence. Compact bone is made up the outer zone, covering an intermediate area of cancellous bone and showing increased osteoblastic activity. Centrally, there is a loose fibrous stroma with more vessels, plump osteoblasts, and a few trabeculae of immature bone. This zonation suggests that growth commences centrally with increasing maturation of bone toward the external surface, and it may also explain why partial excision leaving only a peripheral residuum does not usually lead to recurrence [4, 9].
Contrary to the above study our patient showed clinical recurrence following earlier complete or incomplete surgical removal of the growth.
A diagnosis of osteomas raises the possibility of Gardner’s syndrome, a condition represented by the triad of colorectal polyposis with very high propensity for malignant transformation, skeletal abnormality that include multiple osteomas of the skull and facial skeleton, and multiple supernumerary teeth [6].
Patients with Gardener’s syndrome may also present with symptoms of rectal bleeding, diarrhea and abdominal pains which was not seen in our patient.
In terms of differential diagnosis, peripheral osteomas of the jaws should be distinguished from other bony exostoses of jaws like Tori. Osteoblastoma and osteoid osteomas may present as lingual or buccal bony expansions and should be distinguished from peripheral osteomas [6].
Radiographic features of an osteoma generally show a round or oval well circumscribed radiopaque mass with a broad base [10].
In summary, although osteomas of the jaws remain a rare entity, very large lesions as in the case presented have the potential to interfere with normal function such as mouth opening, swallowing, and speech and may cause facial disfigurement and pain.
Mandibular osteoma, suspected to have Gardener’s syndrome, should be further evaluated to rule out colorectal carcinoma [11].
Malignant transformation of peripheral osteoma has not been reported in literature.
Recurrence of peripheral osteomas after surgical excision is extremely rare due to the histological zonation and increasing maturation of bone toward the external surface that is seen in these lesions [4, 9].
Conflict of interest
The author declare that there are no conflicts of interest concerning this article.
Contributor Information
Sujeeth Kumar Shetty, Email: shettymaxfax@gmail.com.
Lakshith Biddappa, Email: bidz85maxfax@gmail.com.
References
- 1.Kerckhaera A, et al. A giant osteoma of the mandible: case report. J Cranio-Maxillofac Surg. 2005;33:282–285. doi: 10.1016/j.jcms.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Bodner L, Gatot A, Sion-Vardy N, et al. Peripheral osteoma of the mandibular ascending ramus. J Oral Maxillofac Surg. 1998;56:1446. doi: 10.1016/S0278-2391(98)90414-1. [DOI] [PubMed] [Google Scholar]
- 3.Oyarbide NL, Castell EV. Osteomas of the craniofacial region. Review of 106 cases. J Oral Pathol Med. 2008;37:38–42. doi: 10.1111/j.1600-0714.2007.00590.x. [DOI] [PubMed] [Google Scholar]
- 4.Del Vecchio A, Agrestini C, Salucci P, Manicone AM, Della Rocca C. Osteomas and exostoses of the facial structures: a morphological study and the etiopathogenetic considerations. Minerva Stomatol. 1993;42:533–540. [PubMed] [Google Scholar]
- 5.Longo F, Califano L, De Maria G, Ciccarelli R. Solitary osteoma of the mandibular ramus: report of a case. J Oral Maxillofac Surg. 2001;59:698–700. doi: 10.1053/joms.2001.23408. [DOI] [PubMed] [Google Scholar]
- 6.Sayan NB, Ucok C, Karasu HA, Gunhan O. Peripheral osteoma of the oral and maxillofacial region: a study of 35 new cases. J Oral Maxillofac Surg. 2002;60:1299–1301. doi: 10.1053/joms.2002.35727. [DOI] [PubMed] [Google Scholar]
- 7.Schneider LC, Dolinsky HB, Grodjesk JE. Solitary peripheral osteoma of the jaws: report of a case and review of the literature. J Oral Surg. 1980;38:452–455. [PubMed] [Google Scholar]
- 8.Ogbureke KUE, et al. Huge peripheral osteoma of the mandible: a case report and review of the literature. Pathol Res Pract. 2007;203(3):185–188. doi: 10.1016/j.prp.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 9.Selva Dinesh, WhiteVA ConnellJO, Rootman J. Primary bone tumors of the orbit. Surv Ophthalmol. 2004;49:328–342. doi: 10.1016/j.survophthal.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 10.Oner AY, Pocan S. Gardner’s syndrome: a case report. Br Dent J. 2007;2006(200):666–667. doi: 10.1038/sj.bdj.4813719. [DOI] [PubMed] [Google Scholar]
- 11.Woldenberg Y, Nash M, Bodner L. Peripheral osteoma of the maxillofacial region. Diagnosis and management: a study of 14 cases. Med Oral Pathol Oral Cir Bucal. 2005;10(Suppl2):E139–E142. [PubMed] [Google Scholar]


