Keloids are non-malignant mesenchymal tumours which develop in genetically susceptible individuals as a result of various injuries, and they are the result of disorders in the wound healing process [1–5].
The clinical image presents vivid red or even brown tumour-like lesions. Their density is much higher than that of the surrounding skin since they contain mostly collagen fibres. The lesions are clearly visible, and in the peripheral area there are characteristic processes.
The lesions are mostly located in seborrhoeic regions: the chest in the sternum area, back, arms, earlobes and neck.
Keloids tend to occur most frequently in association with some of the genetic diseases of connective tissue like Rubinstein-Taybi syndrome [1–7].
Rubinstein-Taybi syndrome (RSTS, OMIM 180849) is characterized by mental retardation (IQ index is usually between 35 and 50) and physical abnormalities such as broad thumbs and halluces, short stature, microcephaly and facial dysmorphia (beaked nose, hypoplastic maxilla, down-slanting palpebral fissure). Other physical findings may include eye anomalies (ptosis of the eyelids, obstruction of a nasolacrimal duct, refractory problems), congenital heart defects, joint hypermobility and some skin problems such as high susceptibility to keloid formation and hypertrichosis. Patients with RSTS are prone to develop brain tumours (meningioma) and leukaemia before the age of 15 [6, 8, 9].
The birth prevalence of RSTS is 1 in 100 000 to 125 000, and the diagnosis is essentially based on the clinical manifestation; however, evaluation for a microdeletion at chromosome 16p13.3 and mutations in the CREBBP or p300 gene is helpful in diagnosis. The pattern of inheritance is autosomal dominant with variable expression, and most frequently de novo mutations occur [6, 8–10].
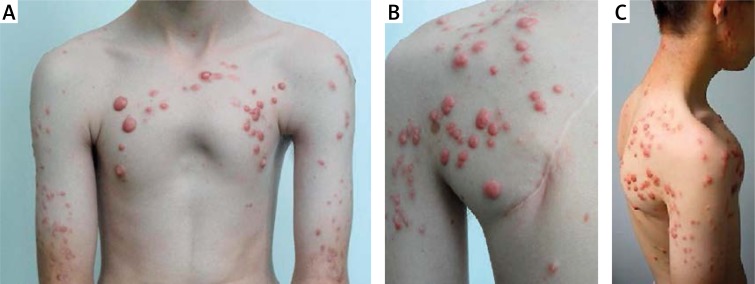
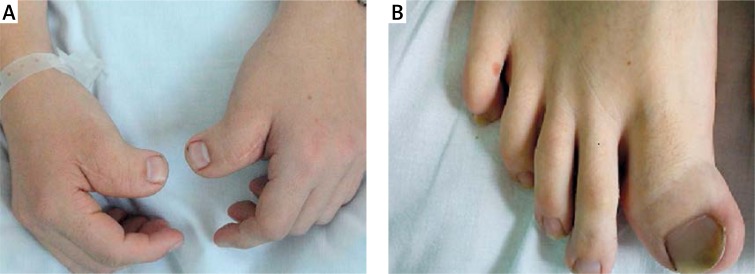
We present a case of a 16-year-old boy hospitalized in our clinic in September 2011 with multiple large keloids on the upper chest, arms, neck, legs and on the earlobe (Figure 1). The first keloids appeared in January 2011 as a complication of a severe form of acne, despite treatment with several oral antibiotics and finally 20 mg/day of isotretinoin until July 2010. The dynamics of the appearance of keloids were exceptional in this case. The susceptibility to keloid formation was extremely strong in our patient, who had more than 100 large, protuberant and disseminated keloids in the typical seborrhoeic regions as well as on the lower limbs. Apart from numerous keloids, the patient presented short stature and low body mass (164 cm/52 kg < 3rd percentile), malformation of the skeletal system (kyphosis, scoliosis, large toes and broad thumbs radially deviated – Figure 2), mild hypertrichosis and subtle facial dysmorphia. The boy had been surgically treated several times for his persistent arterial duct and for bilateral cryptorchidism in early childhood. His mental development and school progress were correct. The parents and siblings of this boy did not present any health problems. There were no complications during the pregnancy period or delivery. The patient has been under the care of genetic counselling since the age of 1 month and under cardiological, orthopaedic, neurological and psychological care. The clinical picture corresponds well with the diagnosis of Rubinstein-Taybi syndrome. The diagnosis was made by genetic counselling in the early childhood of our patient.
Figure 1A–C.
Multiple, large keloids on the chest, arms and earlobe. Scoliosis and kyphosis are also remarkable
Figure 2A–B.
Large toe and broad thumbs radially deviated
For his keloids we applied combined therapy with intralesional steroid injections, 585 nm PDL laser and cryotherapy. We informed the boy and his parents about the need for regular repeats of the therapy, which is essential for obtaining satisfactory results.
In conclusion, our patient presented skeletal malformation, short stature and low body mass, mild hypotrichosis and dysmorphia, cardiac and urinary complications, and an unusual number of large, protuberant keloids that appeared recently in a short period of time. All of these features confirmed the diagnosis of Rubinstein-Taybi syndrome made by genetic counselling.
Finally the authors of this letter would like to state that in the literature there are a few articles about the possible role of isotretinoin in keloid formation [11]. Whether isotretinoin contributed to the development of keloids in this case or it was absolutely independent remains an unresolved issue.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Al-Attar A, Mess S, Thomassen JM, et al. Keloid pathogenesis and treatment. Plast Reconstr Surg J. 2006;117:286–94. doi: 10.1097/01.prs.0000195073.73580.46. [DOI] [PubMed] [Google Scholar]
- 2.O'Sullivan ST, O'Shaughnessy M, O'Connor TPF. Aetiology and management of hypertrophic scars and keloids. Ann R Coll Surg Engl. 1996;78:168–75. [PMC free article] [PubMed] [Google Scholar]
- 3.Slemp EA, Kirschner E. Keloids and scars: a review of keloids and scars, their pathogenesis, risk factors and management. Curr Opin Pediatr. 2006;18:396–402. doi: 10.1097/01.mop.0000236389.41462.ef. [DOI] [PubMed] [Google Scholar]
- 4.Chike-Obi CJ, Cole PD, Brissett AE. Keloids: pathogenesis, clinical features and management. Semin Plast Surg. 2009;23:178–84. doi: 10.1055/s-0029-1224797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zieliński T, Witmanowski H, Lewandowicz E, et al. Hypertrophic scars and keloids. Part II – Prevention and treatment [Polish] Postep Derm Alergol. 2008;25:116–24. [Google Scholar]
- 6.Hennekam RCM, Tilanus M, Hamel BCJ, et al. Deletion at chromosome 16p13.3 as a cause of Rubinstein-Taybi syndrome: clinical aspects. Am J Hum Genet. 1993;52:255–62. [PMC free article] [PubMed] [Google Scholar]
- 7.Kędzia A, Pawlaczyk M, Petriczko E. Hypertrophic scars in a patient with Turner's syndrome treated with recombinant growth hormone. Postep Derm Alergol. 2014;31:117–20. doi: 10.5114/pdia.2014.40917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hennekam RCM. Rubinstein-Taybi syndrome. Eur J Hum Genet. 2006;14:981–5. doi: 10.1038/sj.ejhg.5201594. [DOI] [PubMed] [Google Scholar]
- 9.Tatara Y, Kawakami N, Tsuji T, et al. Rubinstein-Taybi syndrome with scoliosis. Scoliosis. 2011;6:21–7. doi: 10.1186/1748-7161-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harth W, Linse R. Dermatological stigmata in Rubinstein-Taybi syndrome [German] Hautartz. 2001;52:977–9. [PubMed] [Google Scholar]
- 11.Dogan G. Possible isotretinoin-induced keloids in a patient with Behcet's disease. Clin Exp Dermatol. 2006;31:535–7. doi: 10.1111/j.1365-2230.2006.02140.x. [DOI] [PubMed] [Google Scholar]