Sir,
Acute renal failure is an important cause of morbidity and mortality. Inflammation also plays an important role in the physiopathology of acute renal failure.[1] Neutrophil lymphocyte ratio (NLR) is also an important indicator of systemic inflammation.[2] High NLR has been demonstrated to be related with increased mortality in acute coronary syndrome, cancer, hemodialysis and peritoneal dialysis patients.[3,4] At the same time, increased NLR has also been associated with bad prognosis in some disorders.[5] We evaluated NLR of 26 (18 females and 8 males) patients with community-acquired acute renal failure. Patients with acute or chronic infection, hematologic disease, or malignancy were excluded. All patients had been admitted with a diagnosis of acute renal failure and their renal functions recovered after treatment. As all of them had community-acquired acute renal failure, they had no previous laboratory values before the development of acute renal failure; their laboratory values after recovery of renal functions were obtained.
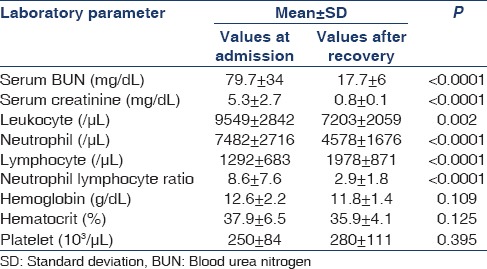
Complete blood count, serum blood urea nitrogen and serum creatinine levels at hospital admission and after recovery of renal functions were recorded. NLR was obtained by dividing neutrophil count to lymphocyte count.
The mean age was 63.3 ± 14 (range, 36–86) years. The laboratory values of patients at hospital admission and after the recovery of acute renal failure are presented in Table 1 . The mean duration of recovery was 7.8 ± 3.8 (3–20) days. While NLR of acute renal failure patients at the time of hospital admission was 8.6, the rate decreased to 2.9 after recovery (P < 0.0001).
Table 1.
Laboratory values of patients at the time of diagnosis and after the recovery of renal functions
We showed that NLR, which is an important indicator of inflammation, was significantly increased in patients with community-acquired acute renal failure. Elevated NLR is a predictor of long-term mortality and bad prognosis; it can also be used in acute inflammatory conditions. The immune system of patients treated in the intensive care unit rapidly responds to systemic inflammation or sepsis. Neutrophilia and lymphocytopenia are related to disease severity. As the clinical condition worsens, neutrophilia and lymphocytopenia become significant and NLR is increased. NLR can be used as a parameter of disease severity in patients treated at the intensive care unit.[2] In our study, NLR was high at the time of acute renal failure diagnosis and decreased when renal function recovered. The mean duration of acute renal failure recovery was 7.8 days. As neutrophils and lymphocytes give more rapid response to the severity of inflammation, NLR can be used for monitoring acute inflammatory conditions. Studies are needed to evaluate the prognostic/diagnostic utility of NLR in monitoring acute inflammatory conditions and acute renal failure.
References
- 1.Akcay A, Nguyen Q, Edelstein CL. Mediators of inflammation in acute kidney injury. Mediators Inflamm. 2009;2009:137072. doi: 10.1155/2009/137072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zahorec R. Ratio of neutrophil to lymphocyte counts--Rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001;102:5–14. [PubMed] [Google Scholar]
- 3.Erdem E, Kaya C, Karataş A, Dilek M, Akpolat T. Neutrophil to lymphocyte ratio in predicting short-term mortality in hemodialysis patients. J Exp Clin Med. 2013;30:129–32. [Google Scholar]
- 4.An X, Mao HP, Wei X, Chen JH, Yang X, Li ZB, et al. Elevated neutrophil to lymphocyte ratio predicts overall and cardiovascular mortality in maintenance peritoneal dialysis patients. Int Urol Nephrol. 2012;44:1521–8. doi: 10.1007/s11255-012-0130-3. [DOI] [PubMed] [Google Scholar]
- 5.Azab B, Jaglall N, Atallah JP, Lamet A, Raja-Surya V, Farah B, et al. Neutrophil-lymphocyte ratio as a predictor of adverse outcomes of acute pancreatitis. Pancreatology. 2011;11:445–52. doi: 10.1159/000331494. [DOI] [PubMed] [Google Scholar]


