Abstract
Cytomegalovirus (CMV) is an important pathogen in immunocompromised individuals. The aim of this study was to analyze prevalence and dynamics of CMV infection among patients undergoing chronic hemodialysis. From 2010 to 2012, a total of 162 patients and 160 control subjects were tested for the presence of CMV IgM and IgG antibodies using enzyme-linked immunosorbent assay. IgM/IgG reactive samples were further evaluated for IgG avidity to confirm or rule out recent primary CMV infection. The overall IgG seropositivity was higher in hemodialysis patients compared to controls (90.7% vs. 81.9%; crude odds ratio [OR] =2.02, 95% confidence interval [CI] =1.05–3.89; OR adjusted for age and gender = 2.18, 95% CI = 1.05–4.55). CMV IgG antibody titers were similar in both groups. There was no difference in CMV prevalence between males (87.9%) and females (96.3%). According to age, a progressive increase in seropositivity was observed in both hemodialysis patients and the control group. Three hemodialysis patients (1.9%) developed recurrent CMV infection (positive IgM with high avidity IgG antibodies). In one patient (2.9%), seroconversion was documented during the second year of the follow-up period indicating primary infection. In contrast, in the control group, recent primary CMV infection (positive IgM with low/borderline IgG avidity) was demonstrated in three subjects (1.9%), whereas one (0.6%) developed recurrent infection. On multivariate logistic regression, hemodialysis and older age were significant predictors for CMV seropositivity.
Keywords: Cytomegalovirus, hemodialysis, seroprevalence
Introduction
Cytomegalovirus (CMV) is a ubiquitous virus that infects people throughout the world. The prevalence of antibodies in adults varies in different geographic regions, from 40%-100%, with lower rates in Europe, parts of North America and Australia, and higher rates in Africa and Asia.[1,2,3,4,5] Most infections are acquired by close personal contact with infected individuals. CMV has been detected in many body fluids, including saliva, urine, blood, cervicovaginal secretions, semen and breast milk. In children, the virus is usually transmitted through infected saliva. In adolescents and adults, sexual transmission is an important route. Moreover, CMV can be transmitted by blood transfusion and organ transplantation.[6]
Primary CMV infections are usually asymptomatic in otherwise healthy children and adults. However, the incidence and spectrum of disease in immunocompromised people establish this virus as an important human pathogen.[7,8] Moreover, there are number of reports of severe clinical manifestations of CMV infections in immunocompetent patients.[9,10,11]
It has been well documented that hemodialysis patients have impaired immune response, which may result in higher prevalence rates of viral infections, including CMV.[12,13,14] Infections in these patients may be due to primary infection or, more commonly, by reactivation of latent virus or re-infection with exogenous virus, which may be introduced by blood transfusion or kidney transplant.[6,15]
The aim of this study was to analyze the prevalence and dynamics of CMV infection among patients in end-stage renal disease undergoing chronic hemodialysis.
Materials and Methods
During a 3-year period (2010–2012), serum samples from 162 consecutive patients undergoing chronic hemodialysis were tested for the presence of CMV-specific IgM and IgG antibodies. The control group consisted of 160 patients presenting for routine check-up with no symptoms of acute febrile disease (antenatal screening, couples undergoing medically assisted reproduction, elective preoperative check-up). Patients and controls did not differ significantly in age (P = 0.413). The mean patient age was 53.7 ± 12.4 (range 21-78) years, whereas the mean age of control subjects was 52.5 ± 12.4 (range 26-79) years [Figure 1]. A subset of 34 hemodialysis patients, enrolled in the transplant program, was evaluated during a period of 2 years on the request of the referring physician.
Figure 1.
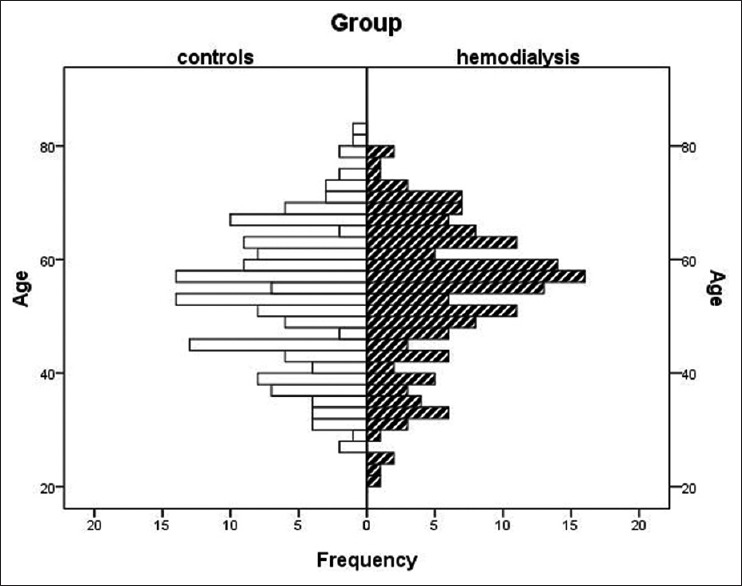
Age distribution of study participants
Anti-CMV IgM and IgG antibodies were detected using a commercial enzyme-linked immunosorbent assay (ELISA) (ETI-Cytok M/ETI-Cytok G; DiaSorin, Saluggia, Italy) and expressed in arbitrary units (AU/ml). Samples with absorbance values greater than or equal to the cut-off value + 10% are considered positive. All IgM/IgG-positive samples were further tested for IgG avidity to confirm or to rule out acute CMV infection. The determination of IgG avidity was carried out with urea as the denaturing agent using a commercial assay (Avidity: Anti-CMV ELISA IgG, Euroimmun, Lübeck, Germany). The IgG avidity index (AI) was calculated and expressed as percentage using the OD values with and without urea treatment and interpreted as follows: AI < 40% = low avidity antibodies indicating recent primary CMV infection; AI 40–60% = borderline avidity; AI > 60% = high avidity antibodies indicating past CMV infection.
Statistical analysis
Groups of categorical variables were compared by Fischer's exact test. Since distributions of numerical variables were not significantly different from normal distribution (Kolmogorov–Smirnov test), t-test for two groups' comparison was used. The strength of association between dependent (IgG positivity) and independent variables was assessed by univariate and multiple logistic regression. The analysis was performed using software package STATA/IC 11.2 for Windows (StataCorp LP, USA).
Results
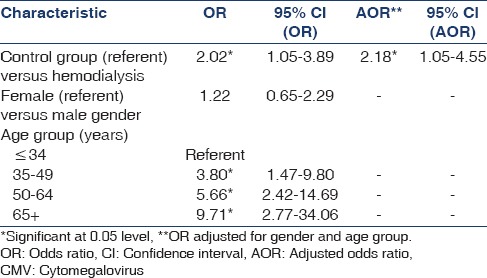
Cytomegalovirus IgG antibodies were detected in 147/90.7% (95% CI = 84.4–94.2) hemodialysis patients and 131/81.9% (95% CI = 75.0–87.5) control subjects [Table 1]. Logistic regression showed that the overall CMV IgG positivity in hemodialysis patients was significantly higher than in controls: Crude OR was 2.02 (95% CI = 1.2–4.35), while OR adjusted for age and gender amounted 2.18 (95% CI = 1.0–4.25) [Table 2]. According to age, a progressive increase in IgG seroprevalence was observed in both hemodialysis patients (73.3%−96.8%) and control group (42.9%−89.3%). Comparing seropositivity between the same age groups, patients on hemodialysis younger than 34 years had almost two times higher prevalence than control subjects (73.3% vs. 42.9%) [Table 1]. Older age group was a significant risk factor for CMV seropositivity [Table 2]. CMV seroprevalence did not differ significantly between males and females (OR = 1.22, 95% CI = 0.65–2.29).
Table 1.
Prevalence of CMV IgG antibodies in hemodialysis patients (n=162) and control group (n=160)
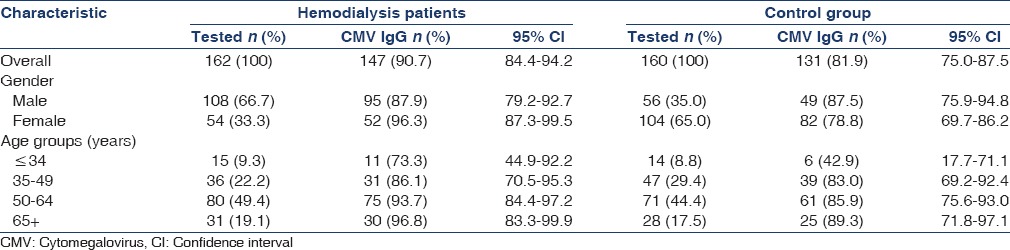
Table 2.
Logistic regression analysis for the risk of CMV IgG seropositivity
Levels of CMV IgG titers in patients and controls are presented in Figure 2. A nonsignificant higher proportion of hemodialysis patients (22.8%) showed a very high IgG titer exceeding the upper cut-off (>10 AU/ml) compared to 16.4% of controls. The proportions of participants with lower CMV titers were similar in both groups (P = 0.219).
Figure 2.
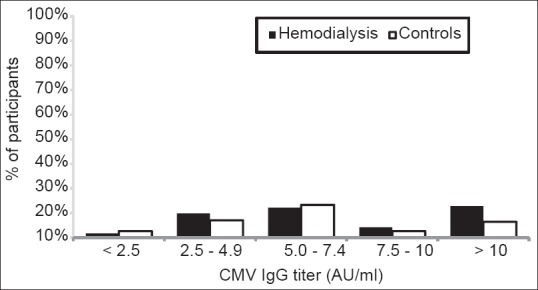
Cytomegalovirus IgG antibody titers in hemodialysis patients and controls
Cytomegalovirus IgM antibodies were detected in three (1.9%) hemodialysis patients and four (2.5%) controls. All three IgM-positive hemodialysis patients showed evidence of recurrent CMV infection (IgG avidity 81%, 83% and 95%, respectively). One initially seronegative hemodialysis patient (0.6%) seroconverted during the second year of the follow-up period. Three participants (1.9%) in the control group developed primary CMV infection. One of them demonstrated low IgG avidity (29%) and two demonstrated borderline IgG avidity (42% and 58%, respectively). One control subject (0.6%) developed recurrent infection (IgG avidity 83%).
Discussion
Cytomegalovirus is one of the most frequently encountered opportunistic viral pathogens in immunocompromised individuals, including hemodialysis patients.[16] There are several published articles on seroprevalence of CMV among hemodialysis patients in Europe in 1990s. The prevalence of CMV antibodies in this population is reported to be 67% in Italy,[17]80% in the Czech Republic,[18] 83% in Germany[19] and 99.3% in Serbia.[20] A study conducted in the Netherlands in 2007 showed a seroprevalence rate of 68.7% among Dutch patients.[12]
In Croatia, there are very few data on the prevalence of CMV infection. The only published study conducted from 2005 to 2009 among childbearing-aged women showed a seropositivity rate of 75.3%.[4] In the Croatian general population, overall CMV seroprevalence is reported to be 63% (78% in adults; unpublished data of the laboratory for virologic serologic diagnostics, Croatian National Institute of Public Health). Results of this study showed a significantly higher CMV seropositivity among hemodialysis patients (90.7%) compared to the healthy control group (81.9%). Studies conducted in Germany[19] and in Turkey[21] showed similar results, while in a Dutch study, the percentage of CMV-seropositive hemodialysis patients was in the range of the reported prevalence in the general population.[12] A higher CMV prevalence in hemodialysis patients could be explained by the acquisition of CMV through repeated blood transfusions or exposure to CMV during hemodialysis procedures. In hyperendemic areas such as Saudi Arabia and Sudan where high percentages of CMV in the population (up to 100%) were reported, the differences among hemodialysis patients and the general population were not observed.[22,23,24]
In this study, no significant difference in CMV IgG antibody titers between hemodialysis patients and controls was documented. In contrast, a study conducted in Thailand showed higher mean antibody titer in patients on hemodialysis compared to healthy controls. However, the overall prevalence in both groups was reported to be 100%.[13]
Our results showed that age was a significant risk factor for CMV seropositivity. A progressive increase in seroprevalence with age was observed in both hemodialysis patients and controls. Age-related increase in the seroprevalence of CMV antibodies has also been shown in some other studies.[12,13,14,15,16,17,18,19,20,21,22,23,24,25]
Females generally had higher CMV seroprevalences than males, although in most studies the differences were small.[2,25,26] This study showed similar results (seroprevalence in women and men was 96.3% and 87.0%, respectively).
Among immunosuppressed individuals, reactivation of latent CMV infection seems to be more frequent than that experienced by the general population.[7,20] Reactivation of CMV in hemodialysis patients may be caused by the uremia-associated immunodeficiency in these patients.[12] In this study, the prevalence of active CMV infection (detection of IgM antibodies) was similar among hemodialysis patients and control group (1.9% vs. 2.5%). Recurrent CMV infection was documented in all hemodialysis IgM-positive patients (two of them reported recurrent infection during the second year), compared to one control subject. None of them reported symptoms of CMV infection. Infection was not confirmed by nucleic acid testing since PCR is not routinely performed in asymptomatic patients. In three participants from the control group, low/borderline avidity was demonstrated indicating recent primary CMV infection. In addition, primary infection was confirmed by seroconversion in one initially seronegative hemodialysis patient during the second year of follow-up period.
Conclusion
The results of this study indicate that being on hemodialysis and older age are significant risk factors affecting CMV seropositivity. A high proportion of hemodialysis patients (90.7%) are seropositive to CMV. Since primary CMV infection remains a concern due to its potential for severe disease in immunocompromised individuals, identification of seronegative individuals is important in preventing this disease.
Acknowledgment
This research was supported by the Ministry of Science, Education, and Sports of the Republic of Croatia, Grant No 005-0053443-3447 (to GMG). The authors thank Ljiljana Milasincic, Snjezana Artl and Jelena Loncar for technical assistance.
Footnotes
Source of Support: This research was supported by the Ministry of Science, Education, and Sports of the Republic of Croatia, Grant No 005-0053443-3447 (to GMG)
Conflict of Interest: None declared.
References
- 1.Enders G, Daiminger A, Lindemann L, Knotek F, Bäder U, Exler S, et al. Cytomegalovirus (CMV) seroprevalence in pregnant women, bone marrow donors and adolescents in Germany, 1996-2010. Med Microbiol Immunol. 2012;201:303–9. doi: 10.1007/s00430-012-0232-7. [DOI] [PubMed] [Google Scholar]
- 2.Cannon MJ, Schmid DS, Hyde TB. Review of cytomegalovirus seroprevalence and demographic characteristics associated with infection. Rev Med Virol. 2010;20:202–13. doi: 10.1002/rmv.655. [DOI] [PubMed] [Google Scholar]
- 3.Lopo S, Vinagre E, Palminha P, Paixao MT, Nogueira P, Freitas MG. Seroprevalence to cytomegalovirus in the Portuguese population, 2002-2003. Euro Surveill. 2011;16:pii:19896. [PubMed] [Google Scholar]
- 4.Vilibic-Cavlek T, Ljubin-Sternak S, Ban M, Kolaric B, Sviben M, Mlinaric-Galinovic G. Seroprevalence of TORCH infections in women of childbearing age in Croatia. J Matern Fetal Neonatal Med. 2011;24:280–3. doi: 10.3109/14767058.2010.485233. [DOI] [PubMed] [Google Scholar]
- 5.Adjei AA, Armah HB, Gbagbo F, Boamah I, Adu-Gyamfi C, Asare I. Seroprevalence of HHV-8, CMV, and EBV among the general population in Ghana, West Africa. BMC Infect Dis. 2008;8:111. doi: 10.1186/1471-2334-8-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hodinka RL. Human cytomegalovirus. In: Versalovic J, Carroll KC, Funke G, Jorgensen JH, Landry ML, Warnick DW, editors. Manual of Clinical Microbiology. 10th ed. Washington, DC: ASM Press; 2011. pp. 1558–74. [Google Scholar]
- 7.Kamar N, Mengelle C, Esposito L, Guitard J, Mehrenberger M, Lavayssière L, et al. Predictive factors for cytomegalovirus reactivation in cytomegalovirus-seropositive kidney-transplant patients. J Med Virol. 2008;80:1012–7. doi: 10.1002/jmv.21176. [DOI] [PubMed] [Google Scholar]
- 8.Cheng JW, Chen YC, Tian YC, Fang JT, Yang CW. Coinfection of cytomegalovirus and miliary tuberculosis in a post-renal transplant recipient. J Nephrol. 2007;20:114–8. [PubMed] [Google Scholar]
- 9.Jain M, Duggal S, Chugh TD. Cytomegalovirus infection in non-immunosuppressed critically ill patients. J Infect Dev Ctries. 2011;5:571–9. doi: 10.3855/jidc.1487. [DOI] [PubMed] [Google Scholar]
- 10.Orasch C, Conen A. Severe primary cytomegalovirus infection in the immunocompetent adult patient: A case series. Scand J Infect Dis. 2012;44:987–91. doi: 10.3109/00365548.2012.697637. [DOI] [PubMed] [Google Scholar]
- 11.Doan TT, Phung TT, Pham HV, Pham SH, Nguyen LT. Effect of ganciclovir for the treatment of severe cytomegalovirus-associated pneumonia in children without a specific immunocompromised state. BMC Infect Dis. 2013;13:424. doi: 10.1186/1471-2334-13-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Betjes MG, Litjens NH, Zietse R. Seropositivity for cytomegalovirus in patients with end-stage renal disease is strongly associated with atherosclerotic disease. Nephrol Dial Transplant. 2007;22:3298–303. doi: 10.1093/ndt/gfm348. [DOI] [PubMed] [Google Scholar]
- 13.Kao TW, Hsu WA, Chen HS, Chen WY. A two year follow-up study of common virus infections in hemodialysis patients in Taiwan. Artif Organs. 2002;26:879–83. doi: 10.1046/j.1525-1594.2002.07053.x. [DOI] [PubMed] [Google Scholar]
- 14.Jha V. Post-transplant infections: An ounce of prevention. Indian J Nephrol. 2010;20:171–8. doi: 10.4103/0971-4065.73431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cordero E, Casasola C, Ecarma R, Danguilan R. Cytomegalovirus disease in kidney transplant recipients: Incidence, clinical profile, and risk factors. Transplant Proc. 2012;44:694–700. doi: 10.1016/j.transproceed.2011.11.053. [DOI] [PubMed] [Google Scholar]
- 16.Cavdar C, Celtik A, Saglam F, Sifil A, Atila K, Celik A, et al. Cytomegalovirus disease in renal transplant recipients: A single-center experience. Ren Fail. 2008;30:503–6. doi: 10.1080/08860220802064705. [DOI] [PubMed] [Google Scholar]
- 17.Spisni C, Stingone A, Di Vito R, Rondinella I, D'Amario C, Tucci E, et al. Serum epidemiological trial on the prevalence of the anti-cytomegalovirus antibodies in patients under substitutive treatment with hemodialysis and CAPD. Nephron. 1992;61:373–4. doi: 10.1159/000186950. [DOI] [PubMed] [Google Scholar]
- 18.Korcáková L, Kaslík J, Svobodová J, Kaslíková J, Bláha J, Sedlácková E, et al. CMV infection in patients with chronic renal failure and in those following transplantation. Czech Med. 1988;11:131–6. [PubMed] [Google Scholar]
- 19.Sibrowski W, Kühnl P, Kalmar G, Albert S, Böhm BO, Doerr HW. Cytomegalovirus diagnosis in blood donors and risk patients. Beitr Infusionsther. 1990;26:37–9. [PubMed] [Google Scholar]
- 20.Trkulic M, Jovanovic D, Ostojic G, Kovacevic Z, Taseski J. Cytomegalovirus infection in patients with kidney diseases. Vojnosanit Pregl. 2000;57:63–7. [PubMed] [Google Scholar]
- 21.Ocak S, Duran N, Eskiocak AF. Seroprevalence of cytomegalovirus antibodies in hemodialysis patients. Turk J Med Sci. 2006;36:155–8. [Google Scholar]
- 22.Ashraf SJ, Arya SC, Parande CM. Viral hepatitis markers in patients on haemodialysis in a hyperendemic area. J Med Virol. 1986;19:41–6. doi: 10.1002/jmv.1890190107. [DOI] [PubMed] [Google Scholar]
- 23.Enan KA, El-Hussein AM, El Eragi A, Elkhider IM. Sero-reactivity to human cytomegalovirus in a cohort of Sudanese renal transplant patients. Khartoum Med J. 2009;2:197–9. [Google Scholar]
- 24.Al-Alousy BM, Abdul-Razak SH, Al-Ajeeli KS, Al-Jashamy KA. Anti-HCMV IgG positivity rate among renal transplant recipients in Baghdad. Saudi J Kidney Dis Transpl. 2011;22:1269–74. [PubMed] [Google Scholar]
- 25.Ikram H. Cytomegalovirus infections in hemodialysis centers. Clin Nephrol. 1981;15:1–4. [PubMed] [Google Scholar]
- 26.Sepehrvand N, Khameneh ZR, Eslamloo HR. Survey the seroprevalence of CMV among hemodialysis patients in Urmia, Iran. Saudi J Kidney Dis Transpl. 2010;21:363–7. [PubMed] [Google Scholar]


