Abstract
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors of the gastrointestinal tract. They can arise from any part of the tract as well as the omentum, mesentery or retroperitoneum. In this study, we present a case of a GIST originating from an extraordinary site, the pancreas. Evaluation of 30-year-old man with complaints of abdominal distension revealed a cystic, distal pancreatic lesion 13 cm in diameter. There were no intra-abdominal or distant organ metastases. The patient was operated with a diagnosis of cystic pancreas tumor, distal pancreatectomy and splenectomy was performed. The lesion was diagnosed as gastrointestinal stromal tumor upon histopathological examination. He was discharged on the sixth postoperative day without any complications and is being followed up for 21 months without systemic or local recurrence. Extragastrointestinal GISTs are reported rarely. To our knowledge, only one pancreatic GIST has been reported previously in the English literature.
Keywords: Gastrointestinal stromal tumour, extragastrointestinal, pancreas
INTRODUCTION
Gastrointestinal stromal tumors (GIST) are the most common tumors of mesenchymal tissue origin in the gastrointestinal tract (GI) (1, 2). It can be seen anywhere throughout the GI tract from the oesophagus to the rectum, but the most common location is the stomach and jejunum (1, 2). Due to mutations of some tyrosine kinase receptors like C-kit and platelet derived growth factor receptor alpha oncogene (PDGFRA), it arises from Cajal cells that provide connection between the myenteric layer and the muscular layer in the GI tract (3–6). Tumors originating from omentum, mesentery, or retroperitoneum, with similar clinical and pathological findings have been described, and these stromal tumors not originitanig from the digestive system are classified as extra-gastrointestinal stromal tumors (EGIST) (7–9). Rare cases of EGIST arising from the gall bladder, abdominal wall, perivesical area, pharynx, posterior mediastinum, liver and pancreas have also been reported (9, 10). In this case report, we present a GIST that did not arise from the gastrointestinal tract (extragastrointestinal), but the pancreas.
CASE PRESENTATION
A thirty-year-old male patient was seen to have a 13 cm mass lesion in the distal pancreas on abdominal ultrasonography performed in another center during evaluation of his abdominal distention. A thoraco-abdominal computed tomography (CT) scan revealed a cystic mass that was 13 cm in size, originating from the distal pancreas, located behind the stomach without any evidence of gastric invasion and containing areas of necrosis and septa (Figure 1). Neither intra-abdominal spread nor distant metastases were observed. Tumor markers including Carbonic antigen (CA) 19-9, carcinoembryonic antigen (CEA) and neuron-specific enolase (NSE) were normal. Considering factors including the patient’s young age, normal levels of tumor markers and the tumors being well defined despite reaching large sizes, without local invasion or systemic spread, it was thought that this lesion was not a classic adenocarcinoma, but a more benign tumor (solid pseudopapillary tumor, neuroendocrine tumor, mass caused by inflammation of the pancreas, etc.). He underwent surgery with a diagnosis of cystic pancreatic tumor. During surgery, a mass that is derived from the tail of the pancreas with no invasion to the retroperitoneal area or adjacent organs was detected. The tumor did not have any attachments to the gastrointestinal tract. The mass was removed by distal pancreatectomy and splenectomy. Histopathological examination of the mass showed a c-kit -positive gastrointestinal stromal tumor with high mitotic index (Figure 2). Histopathological examination did not show any GIS elements. The patient was discharged on the 6th postoperative day without any problems. He is still under follow up for 21 months without any incidents.
Figure 1.

CT image showing a cystic mass that is 13cm in size, originating from the distal pancreas, located behind the stomach without any evidence of gastric invasion and containing areas of necrosis and septa
Figure 2.
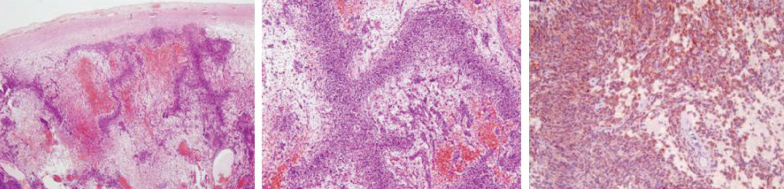
Cells within the neoplastic area containing necrosis and hemorrhage foci and C-kit positivity
DISCUSSION
GISTs are the most common tumors of mesenchymal tissue origin in the gastrointestinal tract, and although it is reported that they can arise outside the digestive system in 5–10%, its true frequency is considered to be even less (7, 9, 10). The origin of EGIST cases located in the omentum, mesentery or retroperitoneum is still controversial. GIST arises from Cajal cells, i.e. are referred to as Cajal cell tumors. However, Cajal cells are not present in the extra-GI areas. Agaimi et al. (9) reported in their series that the rate of EGIST is lower than expected (1.5%) and that some of these tumors are actually masses protruding out of the gastrointestinal canal and eventually lost its communication to the tract due to trauma or during surgery (8–10). Goh et al. (10), in a series of 8 EGIST cases reported that 6 patients had a relation with the GI tract (2 muscular, 4 serosal communication) have reported. In patients with EGIST localized to the liver, the origin is thought to be metastases from unnoticed origin or previous surgical interventions performed for other reasons (9, 11). There are publications reporting GIST cases originating from mesenchymal cells possessing the phenotype of interstitial Cajal cells, outside the GI tract (7, 8). Cajal cells in the pancreas have also been reported (12). The case presented here, did not have a history of previous abdominal surgery. During surgery, the mass was not found to be communicating with the GI tract and no palpable mass was detected in the GI tract. After the pathology report as GIST, an upper and lower gastrointestinal endoscopy were performed, and no additional pathology was detected.
Surgery is the most effective treatment method in gastrointestinal stromal tumors. As in GISTs, it is thought that disease-free and overall survival in EGIST is determined by mitotic activity and cellularity (7, 8). Additionally, larger lesions (>5 cm) are reported to be at high risk of early recurrence (8, 13). In these patients, there is not any alternative chemotherapy regimen to kit inhibitor chemotherapeutics (8, 13). In our patient, the mitotic activity was high and the mass was 13 cm in diameter. However, since surgical margins after resection was detected as tumor-free and the use of adjuvant therapy with kit inhibitors is still controversial in patients with clear surgical margins, adjuvant treatment was not planned for our patient. He is being followed-up without any problems for the last 21 months.
CONCLUSION
Extra-gastrointestinal stromal tumors, especially of pancreatic origin, are very rare and therefore it only emerges as case reports, not being able to explain its biological behavior. The results of long-term follow-up of these cases and the determination of its biological properties will enable us to have more information.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Study concept and design - K.R.S., A.E.; Acquisition of data - K.R.S., M.G.; Analysis and interpretation of data - K.R.S., M.K.; Preparation of the manuscript - K.R.S., M.K.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Miettinen M, Sobin LH, Sarlomo-Rikala M. Immunhistochemical spectrum of GISTs at different sites and their differential diagnosis with a special reference to CD 117 (KIT) Mod Pathol. 2000;13:1134–42. doi: 10.1038/modpathol.3880210. http://dx.doi.org/10.1038/modpathol.3880210. [DOI] [PubMed] [Google Scholar]
- 2.Miettinen M, Lasota J. Gastrointestinal stromal tumors-definition, clinical, histological, immunohistochemical and molecular genetic features and differential diagnosis. Virchows Arch. 2001;438:1–12. doi: 10.1007/s004280000338. http://dx.doi.org/10.1007/s004280000338. [DOI] [PubMed] [Google Scholar]
- 3.Walsh NM, Bodurtha A. Auerbach’s myenteric plexus. A possible site of origin for gastrointestinal stromal tumors in von Recklinghausen’s neurofibromatosis. Arch Pathol Lab Med. 1990;114:522–5. [PubMed] [Google Scholar]
- 4.Rumessen JJ, Thuneberg L. Interstitial cells of Cajal in human small intestine. Ultrastructural identification and organization between the main smooth muscle layers. Gastroenterolog. 1991;100:1417–31. [PubMed] [Google Scholar]
- 5.Hirota S, Ohashi A, Nishida T, Isozaki K, Kinoshita K, Shinomura Y, et al. Gain-of-function mutations of platelet-derived growth factor receptor alpha gene in gastrointestinal stromal tumors. Gastroenterology. 2003;125:660–7. doi: 10.1016/s0016-5085(03)01046-1. http://dx.doi.org/10.1016/S0016-5085(03)01046-1. [DOI] [PubMed] [Google Scholar]
- 6.Medeiros F, Corless CL, Duensing A, Hornick JL, Oliveira AM, Heinrich MC, et al. KIT-negative gastrointestinal stromal tumors: proof of concept and therapeutic implications. Am J Surg Pathol. 2004;28:889–94. doi: 10.1097/00000478-200407000-00007. http://dx.doi.org/10.1097/00000478-200407000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Reith JD, Goldblum JR, Lyles RH, Weiss SW. Extragastrointestinal (soft tissue) stromal tumors: an analysis of 48 cases with emphasis on histologic predictors of outcome. Mod Pathol. 2000;13:577–85. doi: 10.1038/modpathol.3880099. http://dx.doi.org/10.1038/modpathol.3880099. [DOI] [PubMed] [Google Scholar]
- 8.Kobayashi T, Teruya M, Shimizu S, Nishio Y, Ito A, Kobayashi K, et al. Giant extragastrointestinal stromal tumor. Am J Surg. 2004;188:191–2. doi: 10.1016/j.amjsurg.2004.03.006. http://dx.doi.org/10.1016/j.amjsurg.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Agaimy A, Pelz AF, Wieacker P, Roessner A, Wünsch PH, Schneider-Stock R. Gastrointestinal stromal tumors of the vermiform appendix: clinicopathologic, immunohistochemical, and molecular study of 2 cases with literature review. Hum Pathol. 2008;39:1252–7. doi: 10.1016/j.humpath.2007.12.016. http://dx.doi.org/10.1016/j.humpath.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 10.Goh BK, Chow PK, Kesavan SM, Yap WM, Chung YF, Wong WK. A single-institution experience with eight CD117-positive primary extragastro-intestinal stromal tumors: critical appraisal and a comparison with their gastrointestinal counterparts. J Gastrointest Surg. 2009;13:1094–8. doi: 10.1007/s11605-009-0828-4. http://dx.doi.org/10.1007/s11605-009-0828-4. [DOI] [PubMed] [Google Scholar]
- 11.Hu X, Forster J, Damjanov I. Primary malignant gastrointestinal stromal tumor of the liver. Arch Pathol Lab Med. 2003;127:1606–8. doi: 10.5858/2003-127-1606-PMGSTO. [DOI] [PubMed] [Google Scholar]
- 12.Popescu LM, Hinescu ME, Ionescu N, Ciontea SM, Cretoiu D, Ardelean C. Interstitial cells of Cajal in pancreas. J Cell Mol Med. 2005;9:169–90. doi: 10.1111/j.1582-4934.2005.tb00347.x. http://dx.doi.org/10.1111/j.1582-4934.2005.tb00505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Langer C, Gunawan B, Schüler P, Huber W, Füzesi L, Becker H. Prognostic factors influencing surgical management and outcome of gastrointestinal stromal tumours. Br J Surg. 2003;90:332–9. doi: 10.1002/bjs.4046. http://dx.doi.org/10.1002/bjs.4046. [DOI] [PubMed] [Google Scholar]


