Abstract
Background and Objectives:
The vertical sleeve gastrectomy is quickly becoming a preferred bariatric operation. There is a dearth of published data about histopathologic changes in the specimens of morbidly obese patients, especially sleeve patients. The aim of this study is to add more data about the characteristics of the resected gastric specimens to the published literature.
Methods:
A prospective database of all patients undergoing laparoscopic sleeve gastrectomies at a single institution was used to gather our data. Patient characteristics such as age, sex, and initial body mass index were examined. The pathology reports of these patients were examined for any histopathologic changes or findings.
Results:
One hundred forty-five patients over a 3-year period had specimens available for review. Ninety-seven of the patients were women. The mean starting body mass index was 47.5 kg/m2 (range, 35–72.8 kg/m2). The mean age at the time of the operation was 43.1 years. A minority of patients, 62 (49.7%), had histopathologic findings in the resected specimens. The main histopathologic findings were acute and chronic gastritis in 4 patients, chronic gastritis in 61, and follicular lymphoid hyperplasia in 11. One leiomyoma and 2 fundic polyps were found. Seventy-three patients had no histopathologic changes.
Conclusion:
A minority of patients had pathologic findings in the resected specimens. This study will help build a dataset regarding the resected stomachs of morbidly obese individuals. These results can help determine what histopathologic findings can be expected after sleeve gastrectomies.
Keywords: Gastric sleeve, Histopathology
INTRODUCTION
The laparoscopic sleeve gastrectomy (LSG) has become a favored procedure in the worldwide fight against the obesity pandemic. The LSG is a restrictive procedure but also has very strong metabolic effects. The restrictive and metabolic effects of the LSG are made possible by the vertical resection of a large portion of the stomach, including the fundus. There seem to be some common methods of performing the operation, and as we move forward as a community of bariatric/metabolic surgeons, the procedure will likely become more standardized, similar to the Roux-en-Y gastric bypass (RNYGB). Meanwhile, it is incumbent on the bariatric/metabolic surgeon to collect data on the LSG so that we can learn as much as possible about it and the long- and short-term effects of the operation. There is a dearth of published data on histopathologic changes in the resected specimens of LSG patients. Unlike the RNYGB, there is a large specimen available for analysis after the LSG. The size of the resected stomach also obviously differs from the size of a preoperative biopsy specimen in bariatric patients.
This is an observational study that is intended to answer the following questions: What are the common histopathologic findings in resected stomach specimens in morbidly obese patients undergoing an LSG? Can information be gained that may be helpful in determining future guidelines for preoperative workup?
METHODS
This is an observational, retrospective study of resected stomach specimens of consecutive patients undergoing an LSG from August 2008 to December 2012. There were 145 individual specimens evaluated by the pathology department. The specimens were obtained after vertical resection of the stomach during an LSG. The resection was sized using a 34-French bougie. The specimens were removed without a specimen extraction bag, directly through the abdominal wall, by enlarging a 15-mm port site. The specimens were sent for permanent section in formalin and grossly examined. Representative section blocks of 2 mm in thickness were fixed in formalin and paraffin and stained with hematoxylin-eosin and were examined by pathologists in the form of permanent slides sliced to 2 μm in thickness. The slides were also stained with Giemsa to check for microorganisms. Any additional pathologic findings were examined with extra slides.
The inclusion criteria were all patients who underwent LSG. All patients had given specific informed consent before surgery for study of any resected specimens and proper disposal of said specimens. Preoperative endoscopy was performed on a selective basis, based on patient symptomatology. The data were deidentified, and an Excel spreadsheet (Microsoft, Redmond, Washington) was created for data management and analysis. Our patient population is from the Texas-Mexico border area and was mostly Hispanic, of Mexican descent.
RESULTS
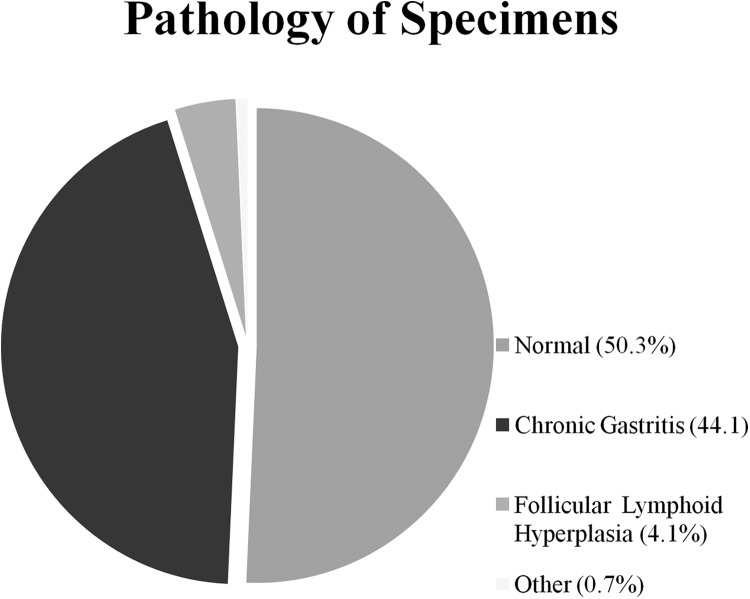
One hundred forty-five patients over a 3-year period had specimens available for review. Ninety-seven of the patients were women. The mean starting body mass index was 47.5 kg/m2 (range, 35–72.8 kg/m2). The mean age at the time of the operation was 43.1 years. A minority of patients, 62 (49.7%), had histopathologic findings in the resected specimen. The main histopathologic findings were acute and chronic gastritis in 4 patients, chronic gastritis in 61, and follicular lymphoid hyperplasia in 11. One leiomyoma and 2 fundic polyps were found. Seventy-three patients had no histopathologic changes (Figure 1).
Figure 1.
Pathology of specimens.
Only 44 specimens underwent Giemsa staining for Helicobacter pylori. Of these, only 8 were positive, for a rate of 18%. We did not start checking for this until late in the series.
DISCUSSION
A majority of patients had no histopathologic changes evident in the resected stomach. The most common finding otherwise was that of chronic gastritis. The second most common change was follicular hyperplasia. There were only 3 patients with polyps. The rate of H. pylori was low, but special staining for microorganisms was not routinely performed early in this series.
Published data on histopathologic specimens obtained from the LSG are lacking. A poster was presented at a meeting of the International Federation for the Surgery of Obesity and Metabolic Disorders–European Chapter in 2012 (Borg et al1), and a report by a group from Kuwait was recently published (Almazeedi et al2). Borg et al found a rate of abnormal pathologic findings of 45%, with a 19% rate of H. pylori infection. Almazeedi et al found a chronic gastritis rate of 74.4%. The H. pylori rate was 7.3%. Our finding of a 44% rate of chronic gastritis is closer to the finding of the English group (Borg et al), as is our H. pylori infection rate of 18%. This leads to other questions, such as why is there a geographical distribution of gastritis, and what is the importance of these findings in any case?
There is also no consensus on the need for preoperative endoscopy or for preoperative endoscopy with a tissue biopsy. Many surgeons support a policy of checking for H. pylori preoperatively, but this is not standardized and can be performed in multiple ways. A serum antigen test, a urease breath test, or a stool antigen test may be used. A tissue biopsy with Giemsa staining is also used. Moreover, the argument can be made that a preoperative determination of the presence of H. pylori may not be necessary because access to the entire remaining stomach remains, in contradistinction to the RNYGB. There is no agreement regarding these issues in the bariatric surgery community.
The information obtained from these specimens has no immediate clinical ramifications as far as changing the postoperative course of LSG patients. However, only by reporting our results can we build enough data to look for patterns of disease and possibly come up with new preoperative algorithms. For example, should all patients undergo endoscopy before an LSG? What is the role of proton pump inhibitors preoperatively? Is preoperative body mass index correlated with any of these histologic findings? By building a body of literature regarding our findings, we can lay the groundwork for analysis and interpretation.
CONCLUSIONS
A minority of patients had pathologic findings in the resected specimens. This study will help build a dataset regarding the resected stomachs of morbidly obese individuals. These results can help determine what histopathologic findings can be expected after sleeve gastrectomies.
References:
- 1. Borg CM, Elkalaaway A, Rotundo M, et al. Laparoscopic sleeve gastrectomy: Routine histological examination of the gastric remnant is highly recommended. Obes Surg. 2012;22:1175. [Google Scholar]
- 2. Almazeedi S, Al-Sabah S, Al-Mulla A, et al. Gastric histopathologies in patients undergoing laparoscopic sleeve gastrectomies. Obes Surg. 2012;23:314–319. [DOI] [PubMed] [Google Scholar]