Abstract
Aims
To understand how US cancer control plans address alcohol use, an important but frequently overlooked cancer risk factor, and how many US adults are at risk.
Methods
We reviewed alcohol control efforts in 69 comprehensive cancer control plans in US states, tribes and jurisdictions. Using the 2011 Behavioral Risk Factor Surveillance System, we assessed the prevalence of current alcohol use among US adults and the proportion of these drinkers who exceeded guidelines for moderate drinking.
Results
Most comprehensive cancer control plans acknowledged alcohol use as a cancer risk factor but fewer than half included a goal, objective or strategy to address alcohol use. More than half of US adults reported current alcohol use in 2011, and two of three drinkers exceeded moderate drinking guidelines at least once in the past month. Many states that did not address alcohol use in comprehensive cancer control plans also had a high proportion of adults at risk.
Conclusion
Alcohol use is a common cancer risk factor in the USA, but alcohol control strategies are not commonly included in comprehensive cancer control plans. Supporting the implementation of evidence-based strategies to prevent the excessive use of alcohol is one tool the cancer control community can use to reduce the risk of cancer.
INTRODUCTION
Each year in the USA, excessive alcohol use is responsible for ~88,000 premature deaths (Centers for Disease Control and Prevention, 2013). In 2006, excessive alcohol use was estimated to cost the USA about $224 billion in lost productivity, health care expenditures, criminal justice system costs and motor vehicle crashes (Bouchery et al., 2011). Additionally, alcohol use is causally related to several cancers, including cancers of the oral cavity, pharynx, larynx, esophagus, liver, colon, rectum and breast (International Agency for Research on Cancer, 2010; Parkin, 2011). A recent study estimated that 3.2–3.7% (18,200–21,300) cancer deaths in the USA in 2009 can be attributed to alcohol (Nelson et al., 2013). Cancer risk increases with the amount of alcohol consumed for many types of cancer, and even a few drinks a week may be harmful for some cancers (Boffetta and Hashibe, 2006; Parkin, 2011; Pelucchi et al., 2011). Although the potential to prevent cancer by reducing alcohol use is recognized within the public health community (Institute of Medicine, 2003; Frieden et al., 2008), data from the 2003 Health Information National Trends Survey found that only 11% of US adults stated that limiting alcohol intake could prevent cancer (Hawkins et al., 2010).
The 2010 US Dietary Guidelines recommend that those who drink alcohol should do so in moderation, defined as no more than one drink a day for women and no more than two drinks a day for men (U.S. Department of Agriculture and U.S. Department of Health and Human Services, 2010). Several public health organizations have issued guidelines or recommendations to prevent alcohol misuse and promote healthy environments (World Health Organization, 2010; National Prevention Council, 2011; Guide to Community Preventive Services, 2012; Moyer, 2013). One objective of this study was to examine the extent to which alcohol control efforts, in the context of cancer prevention, are being implemented in comprehensive cancer control plans. A second objective was to examine the prevalence of current alcohol use among US adults, categorized by adherence to the 2010 US Dietary Guidelines.
METHODS
Through the National Comprehensive Cancer Control Program (NCCCP), the Centers for Disease Control and Prevention (CDC) funds all 50 states, the District of Columbia, seven tribal governments, and seven territories and jurisdictions to establish coalitions of public and private stakeholders, assess the burden of cancer, determine priorities, and develop and implement cancer plans (Given et al., 2005). One of the grantees, the Federated States of Micronesia, supports four Micronesian states, each of which submits a cancer plan to CDC. So, in total, there are 69 comprehensive cancer control plans. During January–May 2013, we reviewed the most recent comprehensive cancer control plan from each program, including 52 plans posted on the Cancer Control P.L.A.N.E.T. website (http://cancercontrolplanet.cancer.gov/) and 17 plans that were updated but not yet posted on the Cancer Control P.L.A.N.E.T. website. At this time plans spanned 1–10 year periods from 2003 through 2020. In comprehensive cancer control plans, a goal refers to a specific program achievement within a specified time period; an objective refers to efforts undertaken to achieve that goal; and a strategy or tactic refers to specific activities needed to achieve that goal. The keyword ‘alcohol’ was used to search all plans, and content containing the term ‘alcohol’ was abstracted and reviewed. First, the plan was evaluated to determine if alcohol use was included as a cancer risk factor in the background information. Next, plans were classified as to whether alcohol use was addressed as a risk factor in at least one goal, objective or strategy. Then relevant goals, objectives and strategies were classified as pertaining to one or more of the following categories: raising public awareness of cancer risk associated with alcohol use, educating individuals about cancer risk associated with alcohol use; reducing prevalence of excessive alcohol use (categorized as measurable or nonmeasurable); partnering with health care providers; developing collaborations; and other (e.g. preventing initiation among youth). States were mapped into three categories according to whether the comprehensive cancer control plan: (a) did not address alcohol use; (b) addressed alcohol use as background information only; or (c) addressed alcohol use as a goal, objective or strategy.
Next, we estimated the prevalence of alcohol use using the Behavioral Risk Factor Surveillance System (BRFSS), an annual, state-based, random-digit–dialed telephone survey of non-institutionalized US adults aged ≥18 years that collects information on many leading health conditions and health risk behaviors, including alcohol use. In 2011, all 50 states and the District of Columbia (DC) conducted the BRFSS survey by landline and cellular telephones; the median proportion of all BRFSS interviews completed by cellular telephones was ~11% (Centers for Disease Control and Prevention, 2012). In 2011, the median survey response rate was 49.7%, ranging from 33.8–64.1% (http://www.cdc.gov/brfss/technical_infodata/quality.htm). BRFSS data were weighted to adjust for several demographic variables (e.g. education levels, marital status, home ownership and telephone source). These analyses were restricted to adults of legal drinking age (≥21 years). A total of 447,505 respondents were included in this analysis.
We used responses to questions about alcohol use during the past 30 days [i.e. the number of days used, the average number of drinks daily, the prevalence of binge drinking (four or more alcohol drinks per occasion for women and five or more alcoholic drinks per occasion for men) and the largest number of drinks consumed on any one occasion], to calculate the prevalence of current alcohol use and then to categorize alcohol use by adherence to the 2010 US Dietary Guidelines, which state ‘If alcohol is consumed, it should be consumed in moderation—up to one drink per day for women and two drinks per day for men—and only by adults of legal drinking age’ (U.S. Department of Agriculture and U.S. Department of Health and Human Services, 2010, p. 21). Current drinkers were defined as respondents who consumed at least one drink of any alcoholic beverage during the past 30 days. Drinkers adhering to moderate drinking guidelines were defined as women who consumed no more than one alcoholic drink a day during the past 30 days and men who consumed no more than two alcoholic drinks a day during the past 30 days. Exceeding moderate drinking guidelines was defined as current drinkers who reported alcohol use above moderate drinking guidelines, at least once in the past 30 days; this category includes respondents who reported that the largest number of drinks on any occasion was more than the moderate drinking guidelines, those whose average number of drinks was more than the moderate drinking guidelines, and/or those who reported binge drinking. The state-specific age-adjusted prevalence of current drinkers and proportion of current drinkers exceeding moderate drinking guidelines were mapped using tertiles to group states into three categories.
RESULTS
Content addressing alcohol as a cancer risk factor in comprehensive cancer control plans
We reviewed comprehensive cancer control plans from 69 programs. Of these plans, 50 (72%) included alcohol use as a cancer risk factor (Table 1). Thirty-one plans (45%) addressed alcohol use as a cancer risk factor in at least one goal, objective or strategy/tactic.
Table 1.
Content related to alcohol use in 69 comprehensive cancer control plans 2003–2020
| Content | No. of Plans |
(%) | Example |
|---|---|---|---|
| Plan acknowledges alcohol use as a cancer risk factor | 50 | (72%) | ‘Alcohol consumption directly and indirectly accounts for 3–6% of all cancer deaths. A causal association has been established between alcohol consumption and cancers of the oral cavity, pharynx, larynx, esophagus, liver, colon, rectum, and female breast, and an association is suspected for pancreatic and lung cancers.’ |
| At least one goal, objective or strategy addresses alcohol use as a cancer risk factor (including any of the below) Raise public awareness of cancer risk associated with alcohol use |
31 | (45%) | |
| 19 | (28%) | ‘Support the implementation of a social marketing media campaign to increase public awareness of the link between high risk alcohol consumption and certain cancers.’ |
|
| Educate individuals about cancer risk associated with alcohol use |
10 | (14%) | ‘Promote the education of individuals in alcohol recovery about healthy eating and physical activity.’ |
| Reduce prevalence of excessive alcohol use Measurable |
16 | (23%) | ‘Decrease to 6% the proportion of adults 18 and older who drink more alcohol than the moderate level (adult women one drink per day and adult men two drinks per day) by 2010. Baseline: 8% BRFSS 2003.’ |
| Non-measurable | 7 | (10%) | ‘Discourage consumption of alcoholic beverages in excess of recommended levels.’ |
| Partner with health care providers to promote awareness among their patients |
12 | (17%) | ‘Promote screening and brief interventions for alcohol abuse in physicians’ offices, clinics, schools and emergency rooms.’ |
| Collaborate with other organizations | 12 | (17%) | ‘Collaborate with organizations such as the Department of Motor Vehicles, Department of Transportation, Mothers Against Drunk Driving, high schools and community centers to distribute public health and public safety messages regarding the hazards of excessive alcohol use and cancer risk.’ |
Sixteen plans (23%) incorporated measureable objectives to reduce the proportion of adults who exceed moderate drinking guidelines and/or to reduce the proportion of those who are under the age of 21 years who consume alcohol, and seven additional plans (10%) included non-measurable action steps like ‘reducing alcohol consumption’.
Nineteen plans (28%) included objectives or strategies to raise public awareness about the link between alcohol use and cancer risk. Ten plans (14%) included educational/awareness strategies directed at individuals, such as those in alcohol recovery programs or oral cancer screening programs. Twelve plans (17%) included objectives or strategies to partner with health care providers, including dentists and substance abuse counselors, in educating patients about the link between alcohol use and cancer risk; for example, by providing materials for counseling patients. Twelve programs (17%) planned to collaborate with stakeholders and partners with a shared interest in reducing alcohol misuse, particularly tobacco prevention and control organizations and underage drinking prevention programs.
Prevalence of alcohol use
In 2011, 56% of adults aged ≥21 years reported having at least one alcoholic drink in the past 30 days (Table 2). By level of alcohol use in the past 30 days, 44% of adults did not report current alcohol use and thus adhered to moderate drinking guidelines, 19% of adults were current drinkers and adhered to moderate drinking guidelines and 37% were current drinkers and exceeded moderate drinking guidelines. Men exceeded moderate drinking guidelines more than women. Exceeding moderate drinking guidelines was more common among younger adults, and decreased with age. Exceeding moderate drinking guidelines also was more common among non-Hispanic whites (40%), college graduates (45%) and persons with household incomes ≥$75,000 (49%).
Table 2.
Prevalence of alcohol use and level of alcohol use [adhering to or exceeding 2010 U.S. Dietary Guidelines for moderate drinking (≤1 drink per day for women or ≤2 drinks per day for men)] among adults age ≥21 years, by socio-demographic characteristics, Behavioral Risk Factor Surveillance System, United States, 2011
| Current drinkers | Proportion of adults who were current drinkers and adhered to moderate drinking guidelines |
Proportion of adults who were current drinkers and exceeded moderate drinking guidelines |
Proportion of current drinkers who exceeded moderate drinking guidelines |
|
|---|---|---|---|---|
| Characteristic | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) |
| Overall | 55.8 (55.5–56.1) | 18.5 (18.2–18.7) | 37.3 (37.0–37.6) | 66.8 (66.4–67.2) |
| Sex | ||||
| Male | 62.6 (62.2–63.1) | 21.9 (21.5–22.3) | 40.7 (40.3–1.2) | 65.0 (64.5–65.6) |
| Female | 49.5 (49.1–9.8) | 15.2 (15.0–15.5) | 34.1 (33.7–34.4) | 68.9 (68.3–69.4) |
| Age group (years) | ||||
| 21–25 | 69.5 (68.2–70.7) | 12.5 (11.6–13.4) | 56.7 (55.3–58.0) | 81.6 (80.3–82.8) |
| 26–34 | 63.6 (62.7–64.4) | 15.0 (14.4–15.6) | 48.4 (47.6–49.3) | 76.2 (75.3–77.2) |
| 35–54 | 58.6 (58.1–59.1) | 18.5 (18.1–18.9) | 40.0 (39.6–40.5) | 68.3 (67.7–68.9) |
| 55+ | 45.4 (45.1–5.8) | 21.6 (21.3–21.9) | 23.8 (23.5–24.1) | 52.3 (51.8–52.9) |
| Race and ethnicity | ||||
| White, non-Hispanic | 58.9 (58.6–59.2) | 19.2 (18.9–19.4) | 39.7 (39.4–0.0) | 67.4 (67.0–67.8) |
| Black, non-Hispanic | 49.1 (48.0–50.1) | 17.7 (16.9–18.6) | 31.1 (30.1–32.1) | 63.4 (61.8–64.9) |
| Hispanic | 49.3 (48.1–50.4) | 14.6 (13.9–15.4) | 34.5 (33.4–35.6) | 70.0 (68.5–71.5) |
| Other, non-Hispanic | 49.2 (47.8–50.6) | 20.1 (19.0–21.2) | 29.1 (27.9–30.4) | 59.1 (57.2–61.1) |
| Education level | ||||
| <high school diploma | 35.8 (34.8–36.9) | 10.8 (10.2–11.5) | 24.9 (24.0–25.9) | 69.5 (67.9–71.2) |
| High school diploma | 49.6 (49.1–50.2) | 16.0 (15.6–16.4) | 33.4 (32.9–34.0) | 67.3 (66.5–68.1) |
| Some college | 58.9 (58.4–59.5) | 19.1 (18.7–19.6) | 39.8 (39.3–40.4) | 67.6 (66.9–68.3) |
| College graduate | 69.0 (68.5–69.4) | 24.1 (23.7–24.5) | 44.8 (44.3–45.3) | 65.0 (64.4–65.5) |
| Annual household income | ||||
| <$25,000 | 42.3 (41.7–43.0) | 13.3 (12.8–13.7) | 29.0 (28.4–29.6) | 68.5 (67.5–69.4) |
| $25,000–$49,999 | 54.2 (53.6–54.8) | 18.1 (17.7–18.6) | 36.0 (35.4–36.6) | 66.5 (65.6–67.3) |
| $50,000–$74,999 | 62.6 (61.9–63.4) | 21.5 (20.8–22.1) | 41.2 (40.4–41.9) | 65.7 (64.8–66.6) |
| >$75,000 | 72.7 (72.2–73.2) | 23.5 (23.0–23.9) | 49.3 (48.7–49.8) | 67.7 (67.1–68.3) |
CI, confidence interval.
Among current drinkers, 67% reported exceeding moderate drinking guidelines at least once in the past 30 days (Table 2). When examined by socio-demographic characteristics, consistently about two-thirds of current drinkers exceeded moderate drinking guidelines, except for persons aged 55 years and older (52%) and persons from racial groups other than white or black (59%). While current drinking was lower among women than men, the proportion of drinkers exceeding moderate drinking guidelines was higher among women than men.
State-specific prevalence of alcohol use and comprehensive cancer control plans
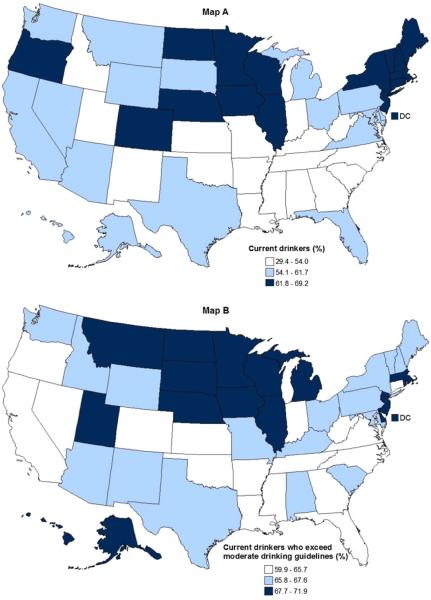
By state, the prevalence of current drinking ranged from 29 to 69% (Fig. 1, Map A). Among current drinkers the proportion exceeding moderate drinking guidelines ranged from 60 to 72% by state and generally was highest among states in the upper Midwest and lowest among states in the South (Fig. 1, Map B). Even among states with low prevalence of alcohol use, such as Utah, most current drinkers exceeded moderate drinking guidelines.
Fig. 1.
Age-adjusted prevalence of current alcohol use and proportion of current drinkers who exceeded 2010 U.S. Dietary Guidelines for moderate drinking (≤1 drink a day among women or ≤2 drinks a day among men) among adults aged ≥21 years, by state, Behavioral Risk Factor Surveillance System, United States, 2011. Map A depicts the prevalence of current alcohol use and Map B depicts the proportion of current drinkers who exceeded moderate drinking guidelines.
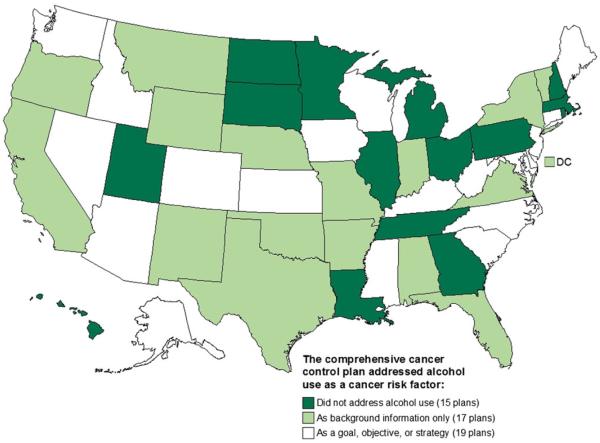
Of states with the lowest proportion of drinkers exceeding moderate drinking guidelines (Fig. 1, Map B), seven states included addressing alcohol use as a cancer risk factor in at least one goal, objective or strategy, seven included alcohol use only as background information, and three did not mention alcohol at all in the comprehensive cancer control plan (Fig. 2). In comparison, of states with the highest proportion of drinkers exceeding moderate drinking guidelines (Fig. 1, Map B), nine states did not mention alcohol at all in the comprehensive cancer control plan, three included alcohol use only as background information, and five included addressing alcohol use as a cancer risk factor in at least one goal, objective or strategy (Fig. 2). Of the fifteen states that did not mention alcohol at all in the comprehensive cancer control plan (Fig. 2), nine had the highest proportion of drinkers exceeding moderate drinking guidelines (Fig. 1, Map B).
Fig. 2.
Content related to alcohol use in state comprehensive cancer control plans 2003–2020. Map depicts whether the state comprehensive cancer control plan addressed alcohol use as a cancer risk factor in at least one goal, objective or strategy; as background information only; or not at all.
DISCUSSION
Alcohol use is an important, but frequently overlooked, risk factor for cancer. We report, for the first time, that while most US comprehensive cancer control plans acknowledged that alcohol use was a cause of cancer, fewer than half included an objective, goal or strategy to address alcohol as a cancer risk factor. We show that in 2011 more than half of US adults reported current alcohol use, and two of three drinkers exceeded moderate drinking guidelines at least once in the past month, thereby increasing their risk of health problems, including cancer. Many states that did not address alcohol use in comprehensive cancer control plans were among the states with the highest prevalence of current drinking and the highest prevalence of drinkers who exceeded moderate drinking guidelines.
Studies of alcohol use prevalence often examine binge drinking, defined as consuming four or more alcohol drinks per occasion for women and five or more alcoholic drinks per occasion for men (Kanny et al., 2013). In contrast, our study examines alcohol use in regards to adherence to the 2010 US Dietary Guidelines, which recommend that if alcohol is consumed, it should be consumed in moderation, defined as up to one drink per day for women and up to two drinks per day for men, in adults of legal drinking age (U.S. Department of Agriculture and U.S. Department of Health and Human Services, 2010). These guidelines are based on evidence of harm associated with alcohol consumed in excess of moderation. Promoting adherence to these guidelines may also help to reduce excessive drinking, including binge drinking. Our study demonstrates that most legal-aged drinkers in the USA exceed moderate drinking guidelines at least once a month. This is concerning because evidence suggests that cancer risk increases with number of drinks and that the risk of several cancers (oral, pharynx, esophagus and breast) is increased even at low doses (≤1 drink/day) (Boffetta and Hashibe, 2006; Parkin, 2011; Pelucchi et al., 2011). A recent study reported an 84% increased risk for alcohol-related cancer deaths among men who drank >14 drinks per week and women who drank >7 drinks per week (Schoenborn et al., 2014). The American Cancer Society (Kushi et al., 2012) and the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) (World Cancer Research Fund/American Institute for Cancer Research, 2007) each have produced reports on guidelines for nutrition, food, and physical activity and also recommend that if alcohol is consumed, it should be consumed in moderation. The WCRF/AICR Panel further recommends that to prevent cancer, consumption of alcoholic drinks should be avoided (World Cancer Research Fund/American Institute for Cancer Research, 2007).
Because binge drinkers are included, by definition, among drinkers who exceed moderate drinking guidelines, states identified in this study as having high prevalence of exceeding moderate drinking guidelines also tended to have high prevalence of binge drinking (Kanny et al., 2013). The prevention of excessive alcohol use, including binge drinking, has been identified by the US National Prevention Strategy as one of seven prevention priorities (National Prevention Council, 2011). Several evidence-based strategies and interventions to reduce alcohol misuse and its related harms have been issued by the US Preventive Services Task Force (Moyer, 2013), the National Prevention Council (National Prevention Council, 2011), the Community Preventive Services Task Force (Guide to Community Preventive Services, 2012) and the World Health Organization (World Health Organization, 2010). These include individual-level interventions such as screening for excessive alcohol use and behavioral counseling to reduce misuse as well as population-level strategies such as decreasing availability of alcohol and creating environments that empower young people not to drink or use other drugs. The Community Guide recommends seven population-level interventions: limiting alcohol outlet density; holding alcohol retailers liable for harms related to the sale of alcoholic beverages to minors and intoxicated patrons (dram shop liability); maintaining existing limits on the days when alcohol is sold; maintaining existing limits on the hours when alcohol is sold; increasing the price of alcohol; avoiding further privatization of alcohol sales in states with government-operated or contracted liquor stores; and electronic screening and brief intervention (Guide to Community Preventive Services, 2012). A recent study found that states with strong population-level alcohol control strategies tended to have lower adult binge drinking prevalence (Naimi et al., 2014).
State health departments have access to state-level data on alcohol use from the BRFSS and on cancer incidence from cancer registries supported through the CDC’s National Program of Cancer Registries or the National Cancer Institute’s SEER program. These data can be used to examine the need for alcohol control strategies within the state’s comprehensive cancer control plans. In our study, almost a third of comprehensive cancer control programs included strategies to raise public awareness of the link between alcohol use and cancer. If people are more aware of the carcinogenic effects of alcohol, they may be more likely to limit their alcohol intake (Hawkins et al., 2010). Strategies that emphasize individual counseling and education may have more impact when combined with strategies that emphasize public policies and change the context in which health decisions are made (Frieden et al., 2008; Frieden, 2010). However, only a few comprehensive cancer control plans included population-level interventions; for example, two state comprehensive cancer control plans included the Community Guide’s recommendation for increasing the price of alcoholic beverages as a strategy to prevent excessive alcohol use.
Our study shows that already >70% of comprehensive cancer control plans recognize the link between alcohol use and cancer. Through efforts to prevent alcohol-related cancers, the cancer control community could emerge as a leader in reducing excessive alcohol use. For example, authors of reports on risk factors for breast cancer have noted the importance of focusing on alcohol use for reducing the risk of breast cancer (Clarke et al., 2006; Colditz and Bohlke, 2014). To reduce cancer risk factors such as tobacco use, physical inactivity and obesity, which increase the risks of multiple chronic diseases, the cancer control community often partners with prevention programs for heart disease and diabetes (Frieden and Berwick, 2011; Jain, 2013). Programs to address alcohol use as a cancer risk factor may benefit from working with non-traditional cancer control partners, such as substance abuse prevention programs.
This study has several limitations. First, the category ‘exceeding moderate drinking guidelines’ groups people who drink above moderate drinking guidelines occasionally with people who do so habitually. Second, BRFSS data are self-reported. Among adults, alcohol use generally and excessive drinking in particular, are underreported in surveys because of recall bias and social desirability bias (Stockwell et al., 2004). A recent study using BRFSS data found that self-reports identified only 22–32% of presumed alcohol use in states, based on alcohol sales (Nelson et al., 2010). Third, BRFSS does not collect information from persons living in institutional settings (e.g. rehabilitation centers, college campuses and military bases); therefore, BRFSS data might not be representative of these populations. Fourth, the content analysis of comprehensive cancer control plans was based on keyword search, and did not include analysis using qualitative software. Finally, content from the comprehensive cancer control plans may not have been implemented.
Of known cancer risk factors, alcohol use is one of the most prevalent among US adults. Some, but not all, comprehensive cancer control plans included strategies to address alcohol use. Promoting awareness of the cancer risk associated with alcohol use and supporting widespread implementation of evidence-based strategies to prevent excessive alcohol use, such as those included in the Community Guide, are tools the cancer control community can use to reduce the risk of cancer.
Acknowledgments
Funding — This work was supported by the Division of Cancer Prevention and Control at the National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention.
Footnotes
Conflict of interest statement. No financial disclosures were reported by the authors of this paper. The authors declare that they have no conflict of interest. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- Boffetta P, Hashibe M. Alcohol and cancer. Lancet Oncol. 2006;7:149–56. doi: 10.1016/S1470-2045(06)70577-0. [DOI] [PubMed] [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, et al. Economic costs of excessive alcohol consumption in the U.S., 2006. Am J Prev Med. 2011;41:516–24. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Methodologic changes in the Behavioral Risk Factor Surveillance System in 2011 and potential effects on prevalence estimates. MMWR Morb Mortal Wkly Rep. 2012;61:410–3. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Alcohol-related Disease Impact (ARDI) Application. CDC; Atlanta, GA: 2013. http://apps.nccd.cdc.gov/DACH_ARDI/Default.aspx (24 September 2014, date last accessed) [Google Scholar]
- Clarke C, Purdie D, Glaser S. Population attributable risk of breast cancer in white women associated with immediately modifiable risk factors. BMC Cancer. 2006;6:170. doi: 10.1186/1471-2407-6-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colditz GA, Bohlke K. Priorities for the primary prevention of breast cancer. CA Cancer J Clin. 2014 doi: 10.3322/caac.21225. doi:10.3322/caac.21225. [DOI] [PubMed] [Google Scholar]
- Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100:590–5. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frieden TR, Berwick DM. The ‘Million Hearts’ initiative— preventing heart attacks and strokes. N Engl J Med. 2011;365:e27. doi: 10.1056/NEJMp1110421. [DOI] [PubMed] [Google Scholar]
- Frieden TR, Myers JE, Krauskopf MS, et al. A public health approach to winning the war against cancer. Oncologist. 2008;13:1306–13. doi: 10.1634/theoncologist.2008-0157. [DOI] [PubMed] [Google Scholar]
- Given L, Black B, Lowry G, et al. Collaborating to conquer cancer: a comprehensive approach to cancer control. Cancer Causes Control. 2005;16:3–14. doi: 10.1007/s10552-005-0499-8. [DOI] [PubMed] [Google Scholar]
- Guide to Community Preventive Services Preventing Excessive Alcohol Consumption. 2012 http://www.thecommunityguide.org/alcohol/index.html (24 September 2014, date last accessed)
- Hawkins NA, Berkowitz Z, Peipins LA. What does the public know about preventing cancer? Results from the Health Information National Trends Survey (HINTS) Health Educ Behav. 2010;37:490–503. doi: 10.1177/1090198106296770. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . Fulfilling the Potential for Cancer Prevention and Early Detection. The National Academies Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- International Agency for Research on Cancer . IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Volume 96: Alcohol Consumption and Ethyl Carbamate. International Agency for Research on Cancer; Lyon, France: 2010. [PMC free article] [PubMed] [Google Scholar]
- Jain SH. Advancing the science and practice of diabetes prevention: an introduction to the supplement. Am J Prev Med. 2013;44:S297–8. doi: 10.1016/j.amepre.2013.02.001. [DOI] [PubMed] [Google Scholar]
- Kanny D, Liu Y, Brewer RD, et al. Binge drinking—United States, 2011. MMWR Surveill Summ. 2013;62:77–80. [PubMed] [Google Scholar]
- Kushi LH, Doyle C, McCullough M, et al. American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012;62:30–67. doi: 10.3322/caac.20140. [DOI] [PubMed] [Google Scholar]
- Moyer VA, on behalf of the U.S. Preventive Services Task Force Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:210–8. doi: 10.7326/0003-4819-159-3-201308060-00652. [DOI] [PubMed] [Google Scholar]
- Naimi TS, Blanchette J, Nelson TF, et al. A new scale of the U.S. alcohol policy environment and its relationship to binge drinking. Am J Prev Med. 2014;46:10–6. doi: 10.1016/j.amepre.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Prevention Council . National Prevention Strategy. U.S. Department of Health and Human Services, Office of the Surgeon General; Washington, DC: 2011. [Google Scholar]
- Nelson DE, Naimi TS, Brewer RD, et al. US state alcohol sales compared to survey data, 1993–2006. Addiction. 2010;105:1589–96. doi: 10.1111/j.1360-0443.2010.03007.x. [DOI] [PubMed] [Google Scholar]
- Nelson DE, Jarman DW, Rehm J, et al. Alcohol-attributable cancer deaths and years of potential life lost in the United States. Am J Public Health. 2013;103:641–8. doi: 10.2105/AJPH.2012.301199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkin DM. Cancers attributable to consumption of alcohol in the UK in 2010. Br J Cancer. 2011;105:S14–8. doi: 10.1038/bjc.2011.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelucchi C, Tramacere I, Boffetta P, et al. Alcohol Consumption and Cancer Risk. Nutr Cancer. 2011;63:983–90. doi: 10.1080/01635581.2011.596642. [DOI] [PubMed] [Google Scholar]
- Schoenborn CA, Stommel M, Ward BW. Mortality risks associated with average drinking level and episodic heavy drinking. Subst Use Misuse. 2014 doi: 10.3109/10826084.2014.891620. doi:10.3109/10826084.10822014.10891620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockwell T, Donath S, Cooper-Stanbury M, et al. Under-reporting of alcohol consumption in household surveys: a comparison of quantity–frequency, graduated–frequency and recent recall. Addiction. 2004;99:1024–33. doi: 10.1111/j.1360-0443.2004.00815.x. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture and U.S. Department of Health and Human Services . Dietary Guidelines for Americans, 2010. U.S. Government Printing Office; Washington, DC: 2010. http://health.gov/dietaryguidelines/dga2010/DietaryGuidelines2010.pdf (24 September 2014, date last accessed) [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Cancer Research Fund/American Institute for Cancer Research . Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective. AICR; Washington, DC: 2007. [Google Scholar]
- World Health Organization Global Strategy to Reduce Harmful use of Alcohol. 2010 http://www.who.int/substance_abuse/activities/gsrhua/en/index.html (24 September 2014, date last accessed)