Abstract
Dementia in Parkinson’s disease (PD) is a serious health issue and a major concern for many patients. In most cases mild cognitive impairment (MCI) is considered a transitional stage between normal cognitive functioning and dementia which is of potential importance in the early identification of patients at risk for dementia. Recently, the Movement Disorder Society (MDS) proposed diagnostic criteria for MCI in PD (PD-MCI). These criteria comprise two operationalizations: Level I (based on an abbreviated assessment) and Level II (based on comprehensive neuropsychological evaluation permitting MCI subtyping). These criteria need to be validated.
This paper describes a project aiming to validate the MDS PD-MCI criteria by pooling and analyzing cross-sectional and longitudinal neuropsychological databases comprising ≥5,500 PD patients and ≥1,700 controls. After applying the MDS PD-MCI Level I and Level II criteria, rates of conversion to PD-dementia and predictive variables for conversion to PD-dementia will be established. This study will also assist in identifying whether revisions of the PD-MCI criteria are required.
Keywords: Parkinson disease, mild cognitive impairment, neuropsychological tests/standards, dementia, validation studies
INTRODUCTION
Patients with Parkinson’s disease (PD), compared to the healthy population, experience an increased risk of dementia (PDD) [1], which has a substantial negative impact upon patients’ wellbeing and caregiver burden [2]. Mild cognitive impairment in PD (PD-MCI) refers to the stage between normal cognitive functioning and PDD. Establishing the diagnosis of PD-MCI is important for the identification and management of at risk PD patients and future studies concerning the etiology, course, and treatment of PD-MCI and the delay or prevention of PDD.
Prior studies found that cognitive functions in PD deteriorate over time: 24% of the patients have cognitive disturbances at onset [3]; three years later 50% show cognitive decline and 9% develop dementia [4]. Although dementia is present in about 80% of patients in studies of long-term follow-up [1], little is known about the rate of change in the different cognitive abilities or the pattern of change of cognitive deficits. The brevity of follow-up intervals (often one year or less), limited assessment of cognitive functions (often just global dementia screening measures), and lack of control groups hamper the ability to draw firm conclusions about the nature and extent of cognitive decline in PD [5]. With few exceptions [1, 2, 4, 6–12, 20], most longitudinal studies have examined prevalent cases with long-standing disease. Selection bias in those studies probably led to underestimation of the true extent of cognitive decline in established patients [12]. In addition, most studies have evaluated cognitive change at a group level, not accounting for individual variability in the trajectory of decline, which is probably large given the heterogeneity of PD. Furthermore, there are opposing views on PD-MCI being solely part of a continuum from normal cognition to PDD versus the existence of a stable subtype of PD-MCI [13]. Hence, it remains to be established how different cognitive domains change over time after the onset of disease, who will exhibit cognitive decline, and what factors predict cognitive deterioration.
An important requirement for answering these research questions is a set of uniform criteria defining PD-MCI, particularly to aid the comparability of different studies across different PD populations and sites. In the past, the MCI criteria used across PD studies have varied considerably in several factors including the number of required cognitive tests and different cut-off points for cognitive impairment. These factors can affect the proportion of PD-MCI cases identified [14]. To address these issues, PD-MCI criteria based on a literature review and expert consensus [15, 16], were recently proposed by the Movement Disorders Society (MDS) Study group on PD-MCI criteria [16]. Validation of the proposed criteria, and if necessary, refinement, will further facilitate research on the epidemiology, clinical characteristics, and prognostic value of MCI in PD. This paper describes the proposed MDS PD-MCI criteria, recent studies using these criteria and the aims of the intended validation studies by the MDS PD-MCI Validation Study Group.
MDS PD-MCI criteria
In brief, the MDS PD-MCI criteria include: 1) diagnosis of idiopathic PD, 2) gradual cognitive decline reported by the patient, caregiver and/or the clinician, 3) deficits at neuropsychological testing, 4) deficits not significantly interfering with functional independence and 5) absence of dementia or other explanations for cognitive deficits [16]. The criteria contain a two-level operational schema of PD-MCI depending on the comprehensiveness of assessment. Level I is based on an abbreviated assessment (e.g., global cognitive scale validated for PD or limited battery of neuropsychological tests) and Level II is based on comprehensive neuropsychological testing of each of five cognitive domains (i.e., attention and working memory, executive, language, memory, and visuospatial). Impairment on neuropsychological tests is demonstrated through scores approximately 1 to 2 standard deviations (SD) below age, education, gender, and culturally appropriate norms, significant decline as demonstrated on serial neuropsychological assessment, or significant decline from estimated premorbid functioning. Examples of suggested neuropsychological tests are described [16]. Classification of PD-MCI into single and multiple domain subtypes is optional in Level II assessment.
A number of issues with the proposed criteria remain unresolved, including which level of the proposed criteria best captures the PD-MCI construct and how impairment on neuropsychological tests is best defined [14, 17]. Questions such as these provide the basis for this project to validate the MDS PD-MCI criteria.
Studies on MDS PD-MCI criteria
Recently, several studies using the MDS PD-MCI criteria were published [7, 18–20]. These studies reflect the emergence of applying the MDS PD-MCI criteria in cross-sectional and longitudinal cohorts and provide preliminary exploration of the criteria’s validation and operationalization. Pedersen et al. [20] applied Level I criteria (limited battery of neuropsychological tests), using 1.5 SD below appropriate norms as a cut-off, to assess a population cohort of newly diagnosed drug naïve PD patients who had a mean PD duration of 2.3 years. One hundred eighty-two patients were assessed at baseline, 178 at one-year follow-up and 167 at three-year follow-up. At baseline, patients with PD-MCI (20.3%) were significantly older, had less education, longer disease duration, lower Unified Parkinson’s Disease Rating Scale scores, higher Hoehn and Yahr stage, and lower MMSE scores than patients without PD-MCI. Twenty seven percent of these PD-MCI patients converted to dementia at three-year follow-up, versus 0.7% of non-MCI patients. MCI at one-year follow-up was equally predictive of dementia with 27.8% conversion at three-year follow-up. However, the reconversion rate from PD-MCI to normal cognition was high as well (21.6% from PD-MCI at baseline to normal and 19.4% from PD-MCI at one-year follow-up to normal). Of those with PD-MCI both at baseline and at one-year follow-up, 45.5% converted to dementia and only 9.1% reconverted to normal cognition. Only age, attention (Stroop color) and verbal memory (CVLT-II immediate and delayed total free recall) were significantly different between the PD-MCI patients who converted to dementia and those who did not convert. Because not all cognitive domains were tested, however, impairments may have been overlooked and the prevalence of PD-MCI might have been underestimated.
Broeders et al. [7] assessed newly diagnosed PD patients using Level II criteria with 1.5 SD below appropriate norms as cut-off. One hundred twenty-three patients were available at baseline, 97 at three-year follow-up and 73 at five-year follow-up. Of the 123 patients, 35.0% fulfilled the criteria for PD-MCI at baseline. After three years 48.5% had PD-MCI and 9.3% had progressed to PDD. After five years 38.4% had PD-MCI and 23.3% PDD. These numbers might underrepresent the development of PDD and PD-MCI given attrition of the cognitively most compromised cases [7], a problem occurring in many longitudinal studies. Reconversion rates from PD-MCI to normal were 9.3% from baseline to three years and 6.4% from three- to five-years follow-up. Regarding the PD-MCI subtypes the majority were multiple domain PD-MCI (baseline 65.1%; 3 year 63.8%; 5 year 42.9%). This is in contrast to other estimates [15], which might reflect the effect of the new MDS criteria. Additionally, Broeders et al. [7] examined the inter-rater agreement, which was high (95.6%; kappa = 0.91). These studies not only provide information regarding the frequency of PD-MCI with the MDS PD-MCI criteria, but also their use in estimating stability or progression of PD-MCI in longitudinal follow-up.
In a cross-sectional study, Marras et al. [19] investigated the frequency of PD-MCI and its subtypes in a population cohort of 139 PD patients who had a mean PD duration of 5.2 years. Level II criteria were applied using 1.5 SD below appropriate norms as cut-off. Thirty-three percent of the sample was classified as PD-MCI, of which 93% had multi-domain MCI, which is comparable to Broeders et al. [7]. When requiring two abnormal tests per domain (which is a modification of the proposed MDS PD-MCI criteria), 31% of the patients were classified as having PD-MCI, of which only 19% had multi-domain MCI. The elimination of the necessity to have subjective complaints of cognitive deficits led to a small rise in PD-MCI from 33% to 41%. However, when including cognitive decline from estimated premorbid levels, as is suggested in the MDS PD-MCI criteria, 79% were classified as PD-MCI. Cognitive decline on a neuropsychological test was defined as an age-corrected z-score 1.5 SD below the estimated premorbid intelligence z-score, as estimated by the Wechsler Test of Adult Reading (WTAR). It should be noted that application of the WTAR for this aim is still under discussion [21, 22]. Furthermore, Marras et al. [19] compared three global screening tests (MMSE, MoCA and Scopa-Cog) with the level II neuropsychological assessment. They concluded that none had a good combined sensitivity and specificity, which suggests that these tests are not well suited for Level I PD-MCI determination.
In another study, Goldman et al. [18] examined the issue of defining optimal neuropsychological test cut-off scores for PD-MCI using the MDS PD-MCI criteria in a cohort of 76 PD patients with a mean PD duration of 9.3 years. Level II criteria were applied, and impairment was examined across different SD cut-offs relative to appropriate normative values to determine the influence of the different cut-offs (i.e., 1, 1.5, 2 SD below appropriate norms, as well as an exploratory lower limit of 2.5 SD). Sensitivity, specificity, positive predictive and negative predictive values, receiver operating curves, and concordance of the MDS PD-MCI Level II criteria were calculated for each of the different cut-off scores, compared to the classification of PD-MCI by consensus diagnosis. In this cohort, the best sensitivity (85.4%) and specificity (78.6%) measures for PD-MCI by MDS criteria were achieved using a cut-off of 2 SD below norms. At this cut-off, 61.8% of patients were classified as PD-MCI. Using a 1.5 SD cut-off yielded high sensitivity (93.8%) but lower specificity (60.7%). In addition, with the MDS PD-MCI Level II criteria, multiple domain PD-MCI was more frequent than single domain impairment at all cut-off scores, similar to Marras et al. [19] and Broeders et al. [7]. Executive function deficits predominated in PD-MCI across all definitions used. Further validation of these observations in larger and diverse cohorts, such as in the MDS Study Group, will be important in determining optimal definitions for PD-MCI.
These four studies using the MDS PD-MCI criteria demonstrate several findings: the operational applicability of Level I and Level II diagnostic criteria in community-based populations [18–20] as well as in a newly diagnosed hospital population [7]; high inter-rater agreement [7], a high prevalence of multi-domain PD-MCI compared to earlier studies [15], and differences in frequency of PD-MCI with different operationalizations of the criteria [18, 19]. These studies provide a basis for the MDS PD-MCI Validation Study Group’s efforts to further examine the MDS PD-MCI criteria, thereby building upon the observations and use of the PD-MCI criteria in these studies and further extending it to much larger datasets of PD patients.
MATERIALS AND METHODS
Aims of the validation study
Initial studies reviewed above demonstrate applicability of the MDS PD-MCI criteria but they need further validation and possibly refinement. The aims of the proposed study are: (1) Validation of the MDS PD-MCI criteria (examining the concordance of PD-MCI classification according to Level I and Level II criteria and their ability to predict conversion to dementia); (2) Definition of the best cut-off scores on the suggested global cognitive scales and on neuropsychological tests for the separate cognitive domains (to discriminate patients with and without PD-MCI; to predict conversion to dementia); and (3) Generating epidemiologic data (defining the frequency of PD-MCI, comparing the stability of this frequency across different cohorts and defining the prevalence of different subtypes of PD-MCI). To answer these research questions, a study group was formed in 2012 which has been endorsed by the MDS as the MDS PD-MCI Validation Study Group. More than twenty-five specialized movement disorders centers in twelve countries over the world participate (Fig. 1).
Fig. 1.
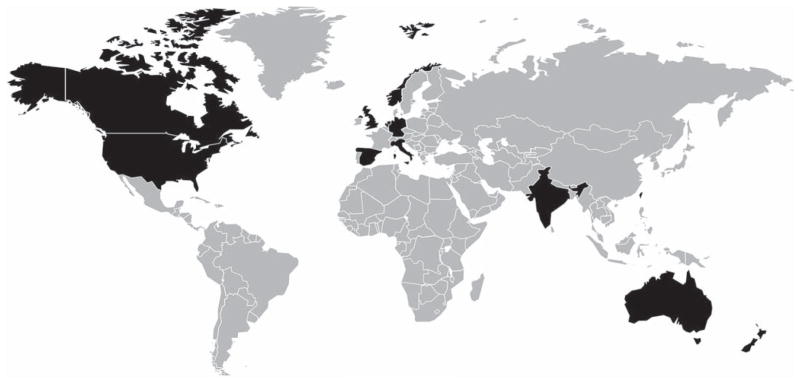
Participating countries in the MDS PD-MCI Validation Study Group are marked black.
The MDS PD-MCI Validation Study Group will pool extant large PD databases including clinical and neuropsychological measures. Both community and clinic samples and both incident and prevalent cohorts will be included. This broad representation is a unique reflection of cognition in PD world wide. The combined databases from the Study Group sites contain more than 5,500 PD patients, of whom 89% are participating in longitudinal studies, and more than 1,700 controls. Level I criteria will be applied to all patients for whom a global cognitive measure or a limited neuropsychological battery was performed. Level II PD-MCI criteria will be applied to approximately 1,600 patients who have had comprehensive neuropsychological assessment. Just over 1,200 (75%) of those Level II patients are followed longitudinally with measurements at one and two years, just over 308 are followed for 5 years and just over 120 for 8 years.
DISCUSSION
The intended study will provide a comprehensive and informative analysis of the applicability and validity of the MDS PD-MCI criteria. This study will help answer several questions regarding how to best operationalize the proposed MDS PD-MCI criteria and will shed light on PD-MCI as a construct and transitional state. The intended study using already collected databases from the Study Group sites is a major step forward in the validation of the MDS PD-MCI criteria.
The MDS PD-MCI Validation Study Group database includes the pooling of datasets from multiple centers across the world to examine PD-MCI. A strong point of the proposed study is the large number of PD patients in the pooled database and the length of follow-up available. This is an important requirement considering the slow and variable progress from normal cognitive functioning to dementia [2], the stable MCI construct [13] and attrition rates of 10–15% per year in longitudinal studies [12]. Therefore, large numbers of patients in longitudinal studies are needed to determine the predictive value of PD-MCI for conversion to dementia. This validation can be done by pooling existing databases. In future prospective studies additional validation issues can be resolved.
In our study design, we will also have the opportunity to examine the potential challenges of defining PD-MCI and its subtypes across various databases, combining studies of heterogeneous populations and using different clinical and neuropsychological tests, and investigating rates of progression of PD-MCI to PDD. This approach was successfully pioneered in an eight-center PD-MCI study by Aarsland et al. [23]. Our study will describe and examine the use of different methods of assessment for the presence of cognitive complaints, functional impairment, and selection of neuropsychological tests. Analyses such as these will help advance our understanding of uniform definitions of PD-MCI and how the criteria can be readily applied across multiple centers. For instance, a difference in methods for assessing the impairments in instrumental activities of daily living (iADL) is expected, although a difference in the number of dementia cases due to assessment method seems unlikely [24]. We will evaluate comparability of the obtained outcomes with different methods before pooling data for combined analysis. When systematic differences appear, the intended analyses will be done separately or where possible correcting for iADL assessment method. In addition, we will examine the various methods used for assessing the gradual decline in cognitive abilities (e.g. through subjective complaints of the patient, their caregiver or by observations of the clinician) as well as for the determination of functional independence. We will assess the influence of these different methods on the measurement of PD-MCI. Furthermore, our study will permit the examination of different rates of progression of PD-MCI.
Uniform reliable criteria for diagnosing PD-MCI and PD-MCI subtypes are an important step forward in the field, and the proposed study will be the first to apply these uniform criteria for PD-MCI across large, pooled cohorts of PD patients. Validation of the MDS PD-MCI criteria will help future research concerning etiology, disease course, and trials assessing treatments for symptomatic improvement or for delaying or preventing onset of dementia. Furthermore, validation of these criteria will aid clinicians, patients, caregivers, and researchers in their communication by providing a common language.
Acknowledgments
The preparation of this manuscript was not funded. The upcoming studies described in this manuscript will be funded by the Michael J. Fox Foundation and by the Parkinson Vereniging (Dutch Parkinson Foundation).
Members of the MDS Study group on the validation of PD-MCI criteria
North America
J. Vincent Filoteo and Irene Litvan, San Diego Veteran Administration Medical Center and Department of Neurosciences University of California, San Diego, CA, USA
Jennifer G. Goldman, Department of Neurological Sciences, Rush University Medical Center, Chicago, IL, USA
Daniel Weintraub, Howard Hurtig, Alice Chen-Plotkin, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, USA
Charles H. Adler and Sandra A. Jacobson, Parkinson’s Disease and Movement Disorders Center, Mayo Clinic, Scottsdale, AZ, USA
Jim Leverenz and Cyrus Zabetian, Department of Neurology, University of Washington School of Medicine, Seattle, WA, USA
Xuemei Huang and Paul J. Eslinger, Department of Neurology, Hershey Medical Center, PA, USA
Connie Marras and Sarah Duff-Canning, Morton and Gloria Shulman Movement Disorders Centre and the Edmond J. Safra Program in Parkinson’s Research, Division of Neurology, University Health Network, Toronto, Canada
Pacific
John C. Dalrymple-Alford and Tim J. Anderson, New Zealand Brain Research Institute, Christchurch, New Zealand
Sharon L. Naismith and Simon J.G. Lewis, Parkinson’s Disease Research Clinic, Brain & Mind Research Institute, The University of Sydney, Australia
Asia
Ruey-Meei Wu and Rwei-Ling Yu, Department of Neurology and Psychology, National Taiwan University Hospital, College of Medicine, National Taiwan University, Taipei, Taiwan
Kalyan B. Bhattacharyya, Department of Neuromedicine, Bangur Institute of Neurology, Kolkata, India
Europe
Caroline H. Williams-Gray, David P. Breen and Roger A. Barker, John Van Geest Centre for Brain Repair, Department of Clinical Neurosciences, University of Cambridge, UK
Alison J. Yarnall, Institute for Aging and Health, Newcastle University, UK
Rob M.A. de Bie, Department of Neurology, Academic Medical Center Amsterdam and University of Amsterdam, The Netherlands
Ted Koene and Martin Klein, Department of Medical Psychology, VU University Medical Center, Amsterdam, The Netherlands
Ellen Trautmann, Paracelsus-Elena-Klinik and Kassel University, Kassel, Germany
Brit Mollenhauer, Paracelsus-Elena-Klinik, Kassel and University Medical Center, Göttingen, Germany
Richard Dodel, Department of neurology, Philipps University Marburg, Marburg, Germany
Jaime Kulisevsky and Javier Pagonabaragga, Movement Disorders Unit, Neurology Department, Hospital and Institute of Biomedical Research Sant Pau, Barcelona, Spain
Maria C. Rodriguez-Oroz and Carmen Gasca-Salas, Department of Neurology, Hospital Donostia, BioDonostia Research Institute, San Sebatian and Ikerbasque, Basque Foundation for Science, Bilbao, Spain
Carme Junque and Barbara Segura, Department of Psychiatry and Clinical Psychobiology, Faculty of Medicine, University of Barcelona, Spain
Marco Timpano Sportiello and Davide M. Cammisuli, Department of Surgery, Medical, Molecular, and Critical Area Pathology, Pisa University School of Medicine, Italy
Paolo Barone, Neurogenerative disease centre, University of Salerno, Italy
Kenn Freddy Pedersen and Guido Alves, Department of Neurology and the Norwegian Centre for Movement Disorders, Stavanger University Hospital, Norway
Footnotes
CONFLICT OF INTEREST
Gert J. Geurtsen has no conflict of interest to report.
Jeroen Hoogland has no conflict of interest to report.
Jennifer G. Goldman – has no conflict of interest to report. Grant/research support: NIH K23NS060949, Parkinson’s Disease Foundation, Rush University Medical Center, Site-PI for clinical research trial (Teva). Honoraria for educational activities: Movement Disorders Society.
Ben A. Schmand has no conflict of interest to report. Grant/research support: Michael J. Fox Foundation and Prinses Beatrix Fonds.
Alexander I. Troster has no conflicts relevant to this study.
David J. Burn has no conflicts relevant to this study.
Irene Litvan: no conflicts relevant to this study. Grant/research support: National Institutes of Aging 5R01AG024040 and CurePSP; Member of the Pfizer and Abbvie Advisory Boards and consultant for Novartis.
References
- 1.Reid WG, Hely MA, Morris JG, Loy C, Halliday GM. Dementia in Parkinson’s disease: A 20-year neuropsychological study (Sydney Multicentre Study) J Neurol Neurosurg Psychiatry. 2011;82:1033–1037. doi: 10.1136/jnnp.2010.232678. [DOI] [PubMed] [Google Scholar]
- 2.Hely MA, Reid WG, Adena MA, Halliday GM, Morris JG. The Sydney multicenter study of Parkinson’s disease: The inevitability of dementia at 20 years. Mov Disord. 2008;23:837–844. doi: 10.1002/mds.21956. [DOI] [PubMed] [Google Scholar]
- 3.Muslimovic D, Post B, Speelman JD, Schmand B. Cognitive profile of patients with newly diagnosed Parkinson disease. Neurology. 2005;65:1239–1245. doi: 10.1212/01.wnl.0000180516.69442.95. [DOI] [PubMed] [Google Scholar]
- 4.Muslimovic D, Post B, Speelman JD, de Haan RJ, Schmand B. Cognitive decline in Parkinson’s disease: A prospective longitudinal study. J Int Neuropsychol Soc. 2009;15:426–437. doi: 10.1017/S1355617709090614. [DOI] [PubMed] [Google Scholar]
- 5.Muslimovic D, Schmand B, Speelman JD, de Haan RJ. Course of cognitive decline in Parkinson’s disease: A meta-analysis. J Int Neuropsychol Soc. 2007;13:920–932. doi: 10.1017/S1355617707071160. [DOI] [PubMed] [Google Scholar]
- 6.Aarsland D, Bronnick K, Larsen JP, Tysnes OB, Alves G. Cognitive impairment in incident, untreated Parkinson disease: The Norwegian ParkWest study. Neurology. 2009;72:1121–1126. doi: 10.1212/01.wnl.0000338632.00552.cb. [DOI] [PubMed] [Google Scholar]
- 7.Broeders M, de Bie RM, Velseboer DC, Speelman JD, Muslimovic D, Schmand B. Evolution of mild cognitive impairment in Parkinson disease. Neurology. 2013;81:346–352. doi: 10.1212/WNL.0b013e31829c5c86. [DOI] [PubMed] [Google Scholar]
- 8.Elgh E, Domellof M, Linder J, Edstrom M, Stenlund H, Forsgren L. Cognitive function in early Parkinson’s disease: A population-based study. Eur J Neurol. 2009;16:1278–1284. doi: 10.1111/j.1468-1331.2009.02707.x. [DOI] [PubMed] [Google Scholar]
- 9.Williams-Gray CH, Foltynie T, Brayne CE, Robbins TW, Barker RA. Evolution of cognitive dysfunction in an incident Parkinson’s disease cohort. Brain. 2007;130:1787–1798. doi: 10.1093/brain/awm111. [DOI] [PubMed] [Google Scholar]
- 10.Williams-Gray CH, Evans JR, Goris A, Foltynie T, Ban M, Robbins TW, et al. The distinct cognitive syndromes of Parkinson’s disease: 5 year follow-up of the CamPaIGN cohort. Brain. 2009;132:2958–2969. doi: 10.1093/brain/awp245. [DOI] [PubMed] [Google Scholar]
- 11.Williams-Gray CH, Mason SL, Evans JR, Foltynie T, Brayne C, Robbins TW, et al. The CamPaIGN study of Parkinson’s disease: 10-year outlook in an incident population-based cohort. J Neurol Neurosurg Psychiatry. 2013 doi: 10.1136/jnnp-2013-305277. [DOI] [PubMed] [Google Scholar]
- 12.Broeders M, Velseboer DC, de BR, Speelman JD, Muslimovic D, Post B, et al. Cognitive change in newly-diagnosed patients with Parkinson’s disease: A 5-year follow-up study. J Int Neuropsychol Soc. 2013;19:695–708. doi: 10.1017/S1355617713000295. [DOI] [PubMed] [Google Scholar]
- 13.Yarnall AJ, Rochester L, Burn DJ. Mild cognitive impairment in Parkinson’s disease. Age Ageing. 2013;42:567–576. doi: 10.1093/ageing/aft085. [DOI] [PubMed] [Google Scholar]
- 14.Dalrymple-Alford JC, Livingston L, MacAskill MR, Graham C, Melzer TR, Porter RJ, et al. Characterizing mild cognitive impairment in Parkinson’s disease. Mov Disord. 2011;26:629–636. doi: 10.1002/mds.23592. [DOI] [PubMed] [Google Scholar]
- 15.Litvan I, Aarsland D, Adler CH, Goldman JG, Kulisevsky J, Mollenhauer B, et al. MDS Task Force on mild cognitive impairment in Parkinson’s disease: Critical review of PD-MCI. Mov Disord. 2011;26:1814–1824. doi: 10.1002/mds.23823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Litvan I, Goldman JG, Troster AI, Schmand BA, Weintraub D, Petersen RC, et al. Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: Movement Disorder Society Task Force guidelines. Mov Disord. 2012;27:349–356. doi: 10.1002/mds.24893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gisslen M, Price RW, Nilsson S. The definition of HIV-associated neurocognitive disorders: Are we overestimating the real prevalence? BMC Infect Dis. 2011;11:356. doi: 10.1186/1471-2334-11-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldman JG, Holden S, Bernard B, Ouyang B, Goetz CG, Stebbins GT. Defining optimal cutoff scores for cognitive impairment using MDS Task Force PD-MCI-criteria. Mov Disord. 2013 doi: 10.1002/mds.25655. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marras C, Armstrong MJ, Meaney CA, Fox S, Rothberg B, Reginold W, et al. Measuring mild cognitive impairment in patients with Parkinson’s disease. Mov Disord. 2013;28:626–633. doi: 10.1002/mds.25426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pedersen KF, Larsen JP, Tysnes OB, Alves G. Prognosis of mild cognitive impairment in early Parkinson disease: The Norwegian ParkWest study. JAMA Neurol. 2013;70:580–586. doi: 10.1001/jamaneurol.2013.2110. [DOI] [PubMed] [Google Scholar]
- 21.Koerts J, Tucha L, Lange KW, Tucha O. The influence of cognitive reserve on cognition in Parkinson’s disease. J Neural Transm. 2013;120:593–596. doi: 10.1007/s00702-012-0916-6. [DOI] [PubMed] [Google Scholar]
- 22.Testa SM, Winicki JM, Pearlson GD, Gordon B, Schretlen DJ. Accounting for estimated IQ in neuropsychological test performance with regression-based techniques. J Int Neuropsychol Soc. 2009;15:1012–1022. doi: 10.1017/S1355617709990713. [DOI] [PubMed] [Google Scholar]
- 23.Aarsland D, Bronnick K, Williams-Gray C, Weintraub D, Marder K, Kulisevsky J, et al. Mild cognitive impairment in Parkinson disease: A multicenter pooled analysis. Neurology. 2010;75:1062–1069. doi: 10.1212/WNL.0b013e3181f39d0e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Christ JB, Fruhmann BM, Riedl E, Prakash D, Csoti I, Molt W, et al. How precise are activities of daily living scales for the diagnosis of Parkinson’s disease dementia? A pilot study. Parkinsonism Relat Disord. 2013;19:371–374. doi: 10.1016/j.parkreldis.2012.11.004. [DOI] [PubMed] [Google Scholar]


