Abstract
Objective
Report the results for an interim analysis of the data collected to date for an ongoing study designed to characterize the age-related changes in Eustachian tube opening efficiency measured using a pressure chamber protocol in children without a history of middle ear disease.
Methods
To date, 41, 3-year old children without past otitis media were enrolled in a longitudinal study of the changes in Eustachian tube function between 3 and 7 years of age. At entry and at scheduled 1-year intervals, Eustachian tube opening efficiency, quantified by the percent of the applied pressure gradient between the middle ear and chamber that was equilibrated by a swallow, was measured using a pressure chamber protocol. For this analysis, the data for 120 tests with representation across all ages were treated as independent observations and analyzed using an ANOVA with variance partitioned for effects of age (3 through 6 years), gradient direction (positive/negative) and ear (left/right).
Results
Eustachian tube opening efficiency was higher for left versus right ears and for positive versus negative driving gradients, but was not different among age groups.
Conclusions
Limitations of the pressure chamber protocol were identified and accounted for in the analysis. The measure of Eustachian tube opening efficiency used in this test protocol behaved similarly to other, more standard measures in response to driving gradient direction. A finer resolution of possible age-related differences in Eustachian tube opening efficiency is expected on application of more sophisticated statistical models to the complete dataset at study end.
Keywords: Eustachian tube function, Children, Age Effects, Pressure-Chamber, Methodology
Introduction
Otitis media (OM) is a common disease of infancy and early childhood characterized by an inflammation of the middle ear (ME) mucosa with or without the presence of an effusion in the usually gas filled ME1. During periods with extant effusion, ME hearing function is compromised and vestibular function can be affected, these being expressed as transient deafness and balance disturbances1,2. OM onset can be symptomatic (acute OM, AOM) usually attributable to a bacterial (or viral?) infection of the ME mucosa, or asymptomatic (OM with effusion, OME) believed to be caused by inefficient ME pressure-regulation3. Subpopulations of affected children are characterized by frequent recurrences of these disease expressions (RAOM, ROME) or by persistent OME (chronic OME, COME) lasting from months to years, or combinations of both1. The incidence of new OM episodes in a given individual and the prevalence of RAOM and COME in the population decrease from infancy through childhood, though OM can present in adolescents and adults, albeit at much lesser frequencies4.
For adequate ME hearing function and preservation of a disease-free ME, the gas pressure in the ME must be maintained at near atmospheric levels5. Because the ME is usually closed to the atmosphere, the ME-atmospheric pressure balance is continuously being disturbed as atmospheric pressure is independently changed by weather fronts and by changes in altitude, and ME gas pressure is independently changed by physiologic processes that promote the exchange of ME gas with adjacent anatomical compartments5. These developing ME-atmospheric pressure gradients are lessened by Eustachian tube (ET) openings which establish an open, gas-phase communication between the nasopharynx (approximately atmospheric pressure) and the ME gas-space, allowing gradient-driven gas flow between those compartments to “reset” ME pressure to near atmospheric, i.e. ME pressure regulation5.
The ET, a usually closed biologic tube connecting the ME to the nasopharynx, can be actively opened by Tensor Veli Palatini muscle (mTVP) contractions during swallowing or other activities and passively opened by increasing the ME or nasopharyngeal pressure to supra-ambient levels6,7. There is a large body of experimental and clinical evidence supporting a role for efficient ET function in the preservation of “normal” hearing and ME health as well as a causal role for inefficient ET function in the pathogenesis of the various OM expressions8,9.
Most evidence supports the concept of a constitutive level of ET functional efficiency constrained by the structure of the ET system (e.g. constituent tissue properties, muscle-ET vector relationships, etc.) that improves with growth and development, but is down-graded during periods with extant nasopharyngeal inflammation (e.g. active allergic rhinitis, viral upper respiratory infection)7. If correct, this model implies that maturation of ET anatomy/structure during growth and development will be reflected in a progressive improvement in ET functional efficiency, and, consequently, a decreasing risk for the various OM expressions over that period. There, the decreased risk for OM with aging in infants and children is well documented1, one cross-sectional study reported age-related changes in the anatomy of the ET system predictive of an improved efficiency of the mTVP to effect ET opening10, and comparative studies showed better ET opening function in adults than in children11,12.
Here, we focus on characterizing the change in one measure of ET opening efficiency, the percent of an applied ME-ambient pressure gradient equilibrated with a swallow7, in children aged 3 through 6 years with no significant OM history. Specifically, negative and a positive ME-ambient pressure gradients were created in the environment of a hyper/hypobaric pressure chamber and the change in those gradients consistent with tubal opening during a swallow was measured by pre- and post-swallow tympanometry12. Our expectations were that, for all ears tested, more efficient ET opening characterizes positive when compared to negative ME-ambient pressure gradients, and, for both types of driving gradients, ET opening efficiency improves with advancing age.
Methods
The data for these analyses were abstracted from those available for an ongoing longitudinal study designed to characterize the changes in ET anatomy and function between 3 and 8 years of age in children with a history of RAOM or of COME or with no significant OM history (control). There, young children are enrolled at 3 years of age and measures of ET anatomy (by combinations of anthropometry, dental casts, cephalograms and MRI scans) and function (ET function tests) are collected at one-year intervals through age 7 years. Group assignment is made using standard criteria based on history information and a review of personal physician and, when available, hospital records13. For children with patent ventilation tubes (most of the younger children in the RAOM and COME cohorts), ET function is evaluated using the Forced-Response test14 and, for children with intact tympanic membranes and effusion-free MEs, ET function is tested using a standard Pressure Chamber test protocol (see below). Here, we present the first analysis of the ET function test data for the 41 children enrolled in the “control” group. At entry, these children were in good health and had few, if any, OM episodes. The study protocol was approved by the IRB at the University of Pittsburgh, and the parent(s) of enrolled children provided written Informed consent for their child's participation.
On the day of testing, the child with a parent(s) or parent-designated adult presented to the Middle Ear Physiology Laboratory at the University of Pittsburgh. An interim history was taken and the child had a standard ENT examination done by a study physician or nurse practitioner that included pneumatic otoscopy and tympanometry (Titan, Interacoustics USA, Eden Prairie, MN). The child was excluded from ET function testing if he/she had a concurrent cold, signs and/or symptoms indicative of active allergic rhinitis, or evidence of extant ME effusion. If qualified for testing at the visit, the child with or without an accompanying parent or designated adult and a technician entered the chamber and were seated on exam chairs (or, if preferred, the child was seated on the parent's lap). If a parent/other designated adult accompanied the child, they underwent otoscopy and tympanometry before entering and again after exiting the chamber. A member of the study staff located outside of the chamber monitored and controlled chamber-pressures and recorded test data. The pressure chamber is a Hyper-tec, 6-person hyperbaric chamber (Hypertec 9100, Olney, Texas) modified during construction for hyper/hypobaric applications and then secondarily modified for fine control of pressure stability/change rate by the addition of a computer-based servo-sensory system that maintains a desired “through-chamber” air-flow (See Figure 1a, b). The test protocol consisted of a series of paired tympanometric measurements before and after a swallow at different chamber-atmospheric pressure gradients. Briefly, after a short acclimation period at a chamber pressure equal to atmospheric pressure, ME pressure was measured by tympanometry, the child was instructed or induced to swallow and the ME pressure measurement repeated. Then, chamber pressure was increased at a rate of approximately 10 daPa/sec to a pressure of atmospheric+200 daPa. ME pressure was measured by tympanometry, the child was instructed or induced to swallow, and the pressure measurement repeated. Chamber pressure was returned to atmospheric and ME pressure was measured by tympanometry before and after swallowing as above. This sequence was repeated at a chamber pressure of atmospheric-200 daPa and then when returned to atmospheric pressure. Then, microphones (Knowles Electronic BT-21834-000-Itasca, Illinois, USA) were placed in the ear-canals and the external ears covered with a standard ear-protector (EARMUFF 1000-Aero Technologies, Indianapolis, IN) to reduce ambient noise at the ear-canal. A plastic nasal probe (2 cm in length, 8 mm in diameter) fitted to a hand-held plastic housing containing a speaker (Piezo Electric Tweeter SS-990-Herald Electronics, Lincolnwood, IL) was inserted part-way into the nostril on the most patent side of the nasal cavity for sound delivery and the speaker activated to deliver sound via the nose to the nasopharynx (at source, sound pressure=110 dB, white noise=2-20KHz). Microphone signals were ported to the outside of the chamber where they were amplified and conditioned (proprietary hardware and software) and synchronously displayed with chamber pressure on a computer screen. The chamber pressure was decreased from atmospheric at a rate of 10 daPa/sec until a spike in one or both of the microphone signals indicative of passive ET opening was noted or until the chamber pressure reached -500 daPa (i.e. increased transmission of sound to the ME across the open ET) and then the chamber pressure was returned to atmospheric. The microphones and speakers were removed and the sequence of tympanometry-swallowing-tympanometry was repeated. The chamber was unlocked, the doors (inner and outer) opened and the technician, child and parent/other adult exited.
Figure 1.
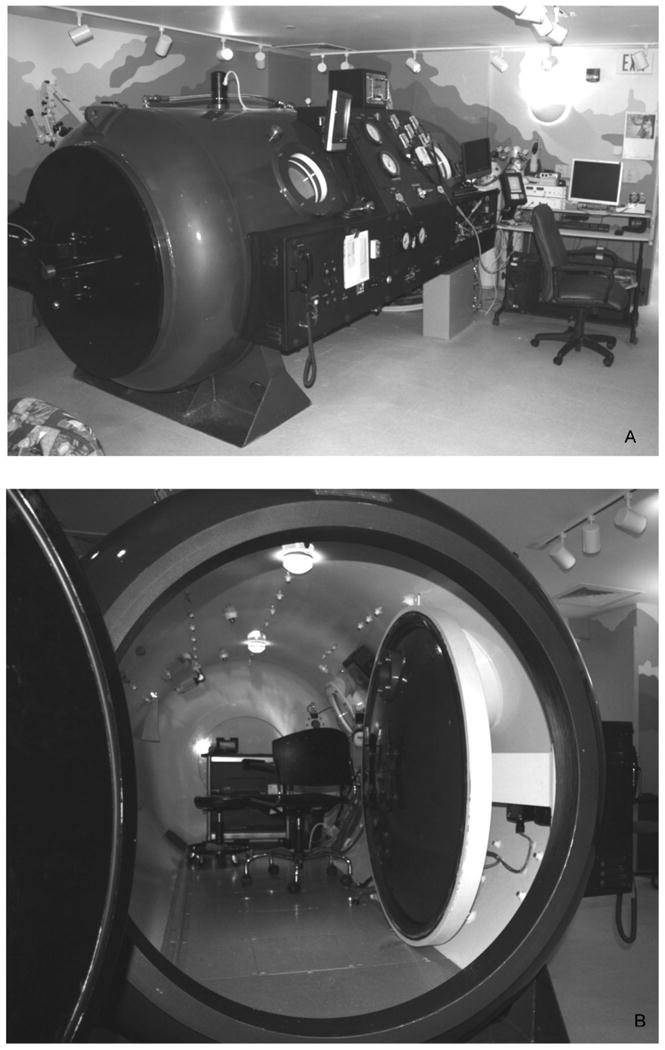
Exterior (A) and interior (B) views of the hypo/hyperbaric pressure chamber used for testing in the present study.
Tympanometry data (pressure and compliance) for both ears at each measurement made during the test were double entered by two persons into a computer file and then reconciled for errors. Because the ME “pressure” measured by tympanometry is a gauge, not an absolute pressure, a more correct description of that “pressure” is the extant pressure gradient between the ME and a reference compartment (chamber, atmospheric, etc.), and we adopt that usage here. In interpreting the tests, we considered three paired ME-chamber pressure gradients (i.e. tympanometric pressures): the pre/post-swallow ME-chamber pressure gradients at atmospheric+200 daPa chamber pressure (Test Sequence 1) and at atmospheric-200 daPa chamber pressure (Test Sequence 2), and the pre/post-swallow ME-chamber pressure gradients at atmospheric chamber pressure after a passive ET opening was detected during the period of decreasing chamber pressure (Test Sequence 3). These sequences were selected because they are expected to establish pre-swallow ME-chamber pressure gradients on the order of -200, +200 and <-200 daPa. Because gradient-driven airflow through the open ET during a swallow reduces (toward 0 daPa) the magnitude of the pre-swallow ME-chamber pressure gradient, we quantified the response as the percent gradient equilibrated with swallowing (PGE), calculated as the difference between the pre- and post-swallow ME-chamber pressure gradients divided by the pre-swallow gradient and multiplied by 100%.
In past studies that measured ET function in children using different pressure chamber protocols, the ME-chamber pressure gradient was estimated as being equal to the chamber-atmospheric pressure gradient11,12,15,16. Thus, for example, raising the chamber pressure to atmospheric+100 daPa was expected to create a ME-chamber pressure gradient of approximately -100 daPa. However, this is only true if the ME pressure at the time of the last ET opening and before increasing/decreasing chamber pressure is approximately equal to atmospheric pressure. There, the true ME-chamber pressure gradient at any applied pressure is equal to the difference between the ME-atmospheric pressure gradient after the most recent ET opening and the chamber-atmospheric pressure gradient at the time of testing (or, algebraically: Pme - Pchamber = Pme - Patm - (Pchamber - Patm) = Pme - Pchamber + Patm - Patm; where Patm - Patm = 0 daPa). In an attempt to “reset” any pre-existing ME-atmospheric gradient to approximately 0 daPa between test sequences, we included periods of swallowing (attempted ET openings) at chamber=atmospheric pressure. However, this attempt was not always successful, and the measured pre-swallow ME-chamber gradient at chamber pressures of atmospheric±200 daPa was variable. Therefore, to preserve comparable test conditions (pre-swallow ME-chamber gradient magnitude and direction) and to ensure an adequate signal indicative of ET opening (measureable gradient decay after a swallow), we excluded the paired data for tests when the measured pre-swallow ME-chamber pressure gradient was greater than -50 daPa for Test Sequences 1 and 3, or less than +50 daPa for Test Sequence 2.
In the analysis, PGE was treated as a continuous variable and, for the complete database of non-excluded tests, we evaluated the significance of the effects on PGE of Ear (right/left), Test Sequence (1, 2, 3) and Age Group (age at testing bracketed at 3, 4, 5, 6+ years) using a 3-factor Analysis of Variance (ANOVA) with post-hoc, pair-wise comparisons of factor states for significant factors done using the Tukey-Kramer Multiple Comparison Test. All data analyses were done using the NCSS 2007 statistical software package (Kaysville, Utah). In the text, the format average±standard deviation is used consistently.
Results
One-hundred and twenty pressure chamber tests were done on the 41 enrolled “control” children (21 male; self-assigned race: 26 white, 7 black, 8 “other”). The average age at the first test was 3.8±0.5 (range: 3.0 to 5.3) years and 36 children had a second, 28 a third, 12 a fourth and 3 a fifth test at approximately yearly intervals. The average ME-ambient pressure gradient (i.e. tympanometric ME pressure) for the subset of analyzed tests at entry was -70±91 daPa for the left and -66±83 daPa for the right ME.
The numbers of all tests with complete, analyzable data for 0, 1, 2 and 3 of the test sequences were 7, 23, 42 and 48 for the left ears, and 8, 24, 54 and 34 for the right ears, respectively. For Test Sequence 1, the numbers of tests with no, unilateral and bilateral evaluable responses were 13, 24 and 83, respectively. For included tests, the average left and right ME-chamber pressure gradients prior to swallowing were -224±76 (range: -59 to -399) daPa and -239±77 (range -51 to -399) daPa, respectively. For Test Sequence 2, the numbers of tests with no, unilateral and bilateral evaluable responses were 46, 44 and 30, respectively. For included tests, the average left and right ME-chamber pressure gradients prior to swallowing were 115±45 (range: 50 to 200) daPa and 114±39 (range 52 to 196) daPa, respectively. For Test Sequence 3, the numbers of tests with no, unilateral and bilateral evaluable responses were 26, 22 and 72, respectively. For included tests, the average left and right ME-chamber pressure gradients prior to swallowing were -261±105 (range: -56 to -399) daPa and -271±103 (range -50 to -399) daPa, respectively. For neither of the ears and none of the test sequences was PGE significantly correlated with the pre-swallow ME-chamber pressure gradient. Inter-correlations between the paired PGEs for the different test sessions could not be estimated because the data co-distributions were bimodal.
Table I presents the average and standard deviation of PGE for the right and left ears for each age group and each of the 3 test sequences. Table II presents the results of the ANOVA as the F-Ratios and associated significance levels (P-Level) for the effect of Age Group, Ear and Test Session, and their interactions, on the PGE. Age group and the Age-Sequence, Ear-Sequence and Age-Sequence-Ear interactions were not significant contributors to PGE, but Ear, Test Sequence and the Age-Ear interaction were. There, PGE was significantly greater for left when compared to right ears and was significantly greater for Test Sequence 2 (positive ME-chamber pressure gradient) when compared to either Test Sequence 1 or Test Sequence 3 (negative ME-chamber pressure gradients). The significance of the Age Group-Ear interaction indicates that the effect of Ear on PGE was not consistent across Age Groups.
Table I.
Sample Size (N), Average (AVG) and Standard Deviation (STD) of the Percent Gradient Equilibrated (%) for the left and right ears of tests done at different ages (years) and combined (All) and for Test Sequences 1 to 3.
| LEFT | RIGHT | ||||||
|---|---|---|---|---|---|---|---|
| TEST | AGE | N | AVG. | STD. | N | AVG. | STD. |
| Sequence 1 | 3 | 22 | 24 | 24 | 17 | 22 | 23 |
| 4 | 28 | 22 | 27 | 29 | 21 | 26 | |
| 5 | 28 | 20 | 25 | 27 | 16 | 18 | |
| 6+ | 18 | 36 | 35 | 19 | 18 | 26 | |
| All | 97 | 24 | 28 | 93 | 19 | 23 | |
| Sequence 2 | 3 | 11 | 25 | 32 | 14 | 19 | 27 |
| 4 | 18 | 43 | 59 | 10 | 34 | 33 | |
| 5 | 11 | 48 | 55 | 15 | 34 | 34 | |
| 6+ | 14 | 62 | 33 | 11 | 36 | 35 | |
| All | 54 | 45 | 45 | 50 | 34 | 34 | |
| Sequence 3 | 3 | 19 | 39 | 46 | 10 | 4 | 5 |
| 4 | 26 | 16 | 31 | 23 | 13 | 26 | |
| 5 | 23 | 17 | 35 | 25 | 12 | 28 | |
| 6+ | 20 | 33 | 37 | 22 | 20 | 31 | |
| All | 89 | 25 | 37 | 81 | 14 | 26 | |
Table II.
- ANOVA table listing the source, degrees of freedom (DF), sum of squares (SOS), mean square (MS), F-ratio and P-level for the effect of the three factors, age, ear and test sequence and their interactions (AB, AC, BC, ABC) on Percent Gradient Equilibrated (PGE).
| SOURCE | DF | SOS | MS | F-Ratio | P-Level |
|---|---|---|---|---|---|
| A: AGE | 3 | 0.40 | 0.13 | 1.50 | 0.21 |
| B: EAR | 1 | 0.44 | 0.44 | 5.01 | 0.02* |
| AB | 3 | 0.92 | 0.31 | 3.48 | 0.02* |
| C: SEQUENCE | 2 | 4.45 | 2.22 | 25.18 | ≪0.01* |
| AC | 6 | 1.04 | 0.17 | 1.96 | 0.07 |
| BC | 2 | 0.31 | 0.16 | 1.76 | 0.17 |
| ABC | 6 | 0.75 | 0.13 | 1.42 | 0.20 |
| S | 440 | 38.86 | 0.09 | ||
| Total (Adjusted) | 463 | 47.38 | |||
| Total | 464 |
Results for Post-hoc Tukey-Kramer Multiple Comparison Test for Pairwise Comparisons showed:
Left Ear PGE > Right Ear PGE, P<0.05
Test Sequence 2 PGE > Test Sequence 1 PGE = Test Sequence 3 PGE, P<0.05
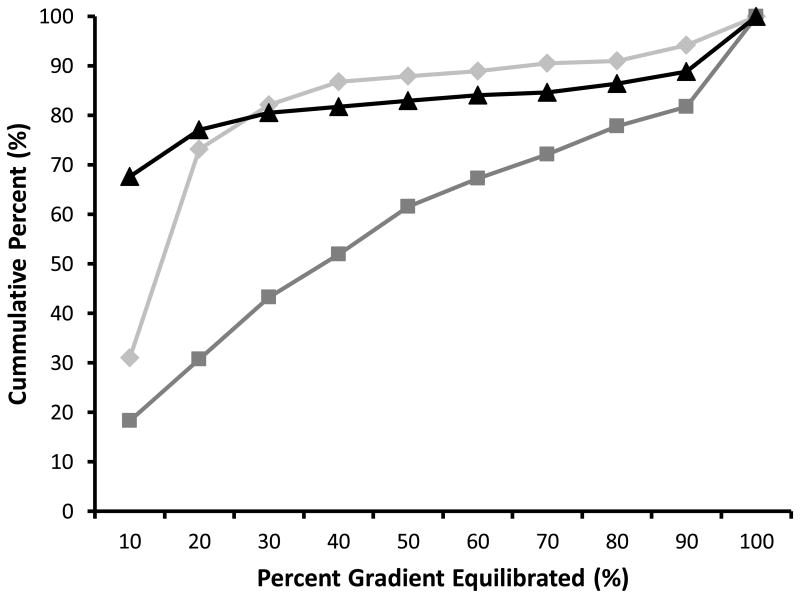
Figure 2 shows the cumulative percent distribution of sequences as a function of increasing PGE values for each of the three test sequences. For Test Sequences 1 and 3, the distributions were highly skewed to lower values while, for Test Sequence 2, the distribution was bimodal with peak frequencies at low and high PGE values. Notably, the median PGE value was approximately 40% for Test Sequence 2, while the median PGE values for Test Sequences 1 and 3 were approximately 15% and 5%, respectively. When presented in this format, the data for each Test Sequence can be easily dichotomized into test pass (above)/fail (below) categories using any chosen cut-off PGE value. For example, a PGE cutoff value of >10% for pass would assign test failure (i.e. the corresponding cumulative percent at that value of PGE) to approximately 31%, 18% and 68% of the observations recorded at Test Sequences 1, 2 and 3, respectively.
Figure 2.
Cumulative percent frequency distributions of the Percent Gradient Equilibrated (PGE) with swallowing recorded for Test Sequences 1 (diamonds), 2 (squares) and 3 (triangles).
Discussion
Consistent with expectation, the analysis of the study data documented a significant directional effect of the ME-chamber pressure gradient on our measure of active ET-opening efficiency, PGE. Specifically, that measure was significantly greater for established positive (Test Sequence 2) versus negative (Test Sequences 1, 3) ME-ambient pressure gradients. This “gradient effect” was demonstrated consistently in past studies that used other response measures and different types of tests to evaluate active ET function in children and adults with and without ME disease16-18, though the mechanism previously proposed to explain the phenomenon, “locking of the valve region”19,20, is unsatisfactory, and without anatomical (identification of an “ET valve”) or physiological (“locking”) foundation. A complete explanation for this phenomenon is beyond the scope of this presentation and requires a detailed analysis of the extant forces acting on the ET lumen under the various conditions21. Nonetheless, the similarity of this “gradient effect” on the response measure used in this study and on those used in earlier studies confirms that PGE captures similar information to other measures of ET opening efficiency.
We also expected that PGE would be conditioned on the child's age at the time of testing and, specifically, that PGE would show a tendency to progressively increase with increasing age. For this interim analysis, the available data were treated as a cross-sectional set of independent observations and the complete test (all three sequences) was treated as the response unit. Under those specifications, no significant difference in PGE was documented among age-groups ranging from 3 through 6 years. An examination of the average PGE data reported in Table I for the 3 test sequences across the different age groups does not reveal a patterned relationship between PGE and age for Test Sequences 1 and 3, negative ME-chamber driving gradients, but does show a tendency for the average PGE calculated for Sequence 2, positive ME-chamber driving gradient, to increase with age. A retrospective reanalysis of the data available for Test Sequence 2 alone yielded a p-value by ANOVA of 0.07 with a post-hoc directional hypothesis test significance level of .04 for the effect of age on PGE. While the results for this secondary analysis suggest an age effect on PGE, when restricted to our planned analysis, the null hypothesis of no effect of age on ET opening efficiency as measured by PGE cannot be rejected. However, the full power of the longitudinal design for our study was not realized in the cross-sectional data analysis used for this report, and given the rather narrow range of observed PGE values for each test sequence, small differences in PGE across ages would be difficult to detect. At the study's end (projected for 2017), the application of more powerful analytic methods that take advantage of the complete set of repeated measures available from the longitudinal test protocol is expected to be more sensitive to detect more subtle effects of age on our measure of ET opening efficiency.
There is a strong theoretical foundation for improving ET opening efficiency through infancy and early childhood in concert with the maturation of the anatomical structure of the ET system6. One previous study compared ET function measured unilaterally, using a pressure chamber protocol, between a group of 85 children (average age 7.4 years) and a group of 92 adults, both groups with “normal” MEs and a negative history for OM. While no significant between-group differences in measures of the passive ET opening function (ME-ambient gradient at which the ET passively opens and closes) were observed, a significant between-group difference in active ET opening efficiency, favoring the adults, was reported16. In contrast, few studies have described the pattern of change in ET functional efficiency during early childhood at relatively fine temporal resolutions (e.g. change/year) as was done in the present study. There, protocols to assess ET opening efficiency need to include a reliable method to establish defined ME-ambient pressure gradients and one to capture and quantify the change in those gradients after maneuvers that effect ET opening.
For ears with a non-intact tympanic membrane, as for example those with patent ventilation tubes, standardized ME-ambient pressure gradients can be applied by an external pump coupled to the ear-canal and changes in the applied gradient after maneuvers usually associated with active ET openings can be directly measured by online pressure sensors (manometric ET function testing)7,22. While a non-intact tympanic membrane is an unusual condition for healthy ears, ventilation tubes are commonly inserted to treat COME or to prevent RAOM. Two earlier studies followed young children with ventilation tubes inserted for COME by repeated (6-week to 3 month intervals) manometric ET function tests over the period of ventilation tube functionality (from 12 to 30 months). The longitudinal patterns for the different test measures were examined for evidence of functional improvement with advancing time (i.e. age)17,23. Neither study documented a directional change over time in standard test measures of the passive or active opening functions of the ET. This type of study format is not applicable to children with healthy MEs and is not adaptable to long follow-up periods in children with a history of OM because of the relatively short half-life for ventilation tube functionality (6-12 months). Moreover, the interpretation of the results of such studies in terms of age-related changes in ET function is constrained by the relatively short study period of “aging” represented in the captured data and confounded by the possible erroneous attribution of a documented effect to “aging/maturation” when, in fact, caused by resolution of inflammatory changes within the ET lumen.
For otherwise healthy MEs with no OM history and intact tympanic membranes, the requirements for assessing ET opening efficiency can be satisfied by testing within the environment of a hypo-hyperbaric pressure chamber24. There, positive and negative ME-ambient pressure gradients can be created by changing the chamber pressure (relative to atmospheric) and ET opening can be semi-quantified using repeated tympanometric measurement of the gradient before and after the test subject performs a maneuver, or series of maneuvers, typically associated with ET opening (See Methods). Only one previous study used this methodology to explore the possible age-related changes in the ET function of children with healthy MEs and no history of OM (or in children with a history of OM)12. Specifically, Bylander and colleagues tested unilateral ET function in 44 children aged 3 to 12 years (24 in the 3 through 6 year age-range studied here) with repeat testing 1.5 years after enrollment and, in a subset of 21 subjects, repeat testing at 3 years (only 3 in the age-range for our study) after enrollment. For each test, ME-chamber pressure gradients were established by decreasing and increasing chamber pressure to atmospheric-/+200 daPa. At the established chamber-pressure, the child was asked to swallow repeatedly and the ME-chamber pressure gradient was measured by tympanometry and, if not 0 daPa, the child was permitted to attempt to open their ET using any chosen method (“free-choice”), and the ME-chamber pressure gradient again measured. To assign an ET opening efficiency to each test, they used a categorical rating system originally described by Elner24 that cross-tabulates partial/none, positive/negative ME-chamber pressure gradient equilibration after swallowing and after the “free choice” maneuvers. To address the issue of an age-related change in ET opening efficiency, they compared the frequency of category shifts (along a scale from excellent, category 1, to poor, category 4) between paired tests at the different ages. Between paired tests performed at the younger and older ages, they reported a significantly higher frequency of shifts to the “better function” categories when compared to the frequency of shifts to the “poorer function” categories. Notably, “free choice” maneuvers were often associated with ET openings after no further openings were documented on repeated swallowing. When broadly interpreted, these results provide support for an age-related improvement in the ability to actively open the ET, but the uncritical acceptance of that result is tempered by deficiencies in the published methodological details supplied with respect to validating and quantifying the pre-maneuver ME-chamber pressure gradient. A second concern is the represented distribution of child ages at entry which was centered at approximately 7.5 years with a consequence that the sample period for assessing any change in ET opening efficiency does not overlap the younger age range during which anatomical maturation of the ET system is most rapid and during which infants and young children tend to “outgrow” OM risk1,6.
At present, there are no established protocols for assessing the efficiency of ET opening by swallowing or other maneuvers applicable to tests done in the environment of a pressure chamber. From our experience, we raise two issues that need be considered in formulating any protocol design. First, as outlined in the Methods section, simple assumptions relating the ME-chamber to chamber-atmospheric pressure gradients are not valid for all tests, and provisions should be made to directly measure the “true” driving gradients for trans-ET airflow extant at the time of an ET opening by any maneuver. The chamber pressure could then be adjusted to establish the desired gradient which may be difficult in practice or, as was done by us, only tests within a desired range of gradients included in the analysis. Second, categorical response variables should be discontinued in favor of quantitative measures of the “degree” of ET opening during a maneuver or over a series of maneuvers. For example, for ears with similar volumes, our measure, PGE, can be directly related to a physical measure, i.e. the volume flow of gas through a given ET during a swallow-induced opening at a specified gradient, or, more simply, the trans-ET conductance when the ET lumen is opened by a swallow.
In conclusion, we present a method for assessing the efficiency of active, muscle-assisted ET opening during a swallow in ears without extant ME disease and with intact TMs. Potential sources of error in “real-life” protocol applications and the measurements required to avoid misinterpretation of test results are presented. Data available to date from our ongoing longitudinal study of the age-related changes in active ET opening efficiency in children with no history of OM as measured using the protocol were analyzed using a standard statistical model for cross-sectional data. That analysis failed to reject the null hypothesis of no difference among age groups in our measure of ET opening efficiency. It is expected that a finer resolution of the differences among age-groups in ET opening efficiency will be afforded by the use of more sophisticated statistical techniques applicable to the repeated-measures structure of the longitudinal dataset at study completion.
Acknowledgments
This study was supported in part by a grant from the National Institutes of Health (P50 DC007667), and by the Hamburg and Eberly Endowments to the Division of Pediatric Otolaryngology, University of Pittsburgh. These sources provided funding for the study, but did not have input into the study design or the analyses and interpretation of the data.
Footnotes
Conflict Of Interest Statement: None of the authors has a real or potential conflict of interest to declare regarding the materials presented in this manuscript.
References
- 1.Bluestone CD, Klein JO. Otitis Media in Infant and children. 5th. Ontario: B. C. Decker, Inc.; 2007. [Google Scholar]
- 2.Casselbrant ML, Villardo RJ, Mandel EM. Balance and otitis media with effusion. International journal of audiology. 2008 Sep;47(9):584–589. doi: 10.1080/14992020802331230. [DOI] [PubMed] [Google Scholar]
- 3.Mandel EM, Doyle WJ, Winther B, Alper CM. The incidence, prevalence and burden of OM in unselected children aged 1-8 years followed by weekly otoscopy through the “common cold” season. Int J Pediatr Otorhinolaryngol. 2008 Apr;72(4):491–499. doi: 10.1016/j.ijporl.2007.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swarts JD, Bluestone CD. Eustachian tube function in older children and adults with persistent otitis media. Int J Pediatr Otorhinolaryngol. 2003 Aug;67(8):853–859. doi: 10.1016/s0165-5876(03)00127-7. [DOI] [PubMed] [Google Scholar]
- 5.Doyle W. Middle ear pressure regulation. In: Rosowski J, Merchant S, editors. The Function and Mechanics of Normal, Diseased and Reconstructed Middle Ears. The Hague, The Netherlands: Kugler Publications; 2000. [Google Scholar]
- 6.Bluestone CD. Eustachian Tube Structure, Function, Role in Otitis Media. Hamilton, Ontario: BC Decker Inc; 2005. [Google Scholar]
- 7.Doyle WJ, Swarts JD, Banks J, Casselbrant ML, Mandel EM, Alper CM. Sensitivity and specificity of eustachian tube function tests in adults. JAMA Otolaryngol Head Neck Surg. 2013 Jul 1;139(7):719–727. doi: 10.1001/jamaoto.2013.3559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bluestone CD. Pathogenesis of otitis media: role of eustachian tube. Pediatr Infect Dis J. 1996 Apr;15(4):281–291. doi: 10.1097/00006454-199604000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Bluestone CD, Doyle WJ. Anatomy and physiology of eustachian tube and middle ear related to otitis media. J Allergy Clin Immunol. 1988 May;81(5 Pt 2):997–1003. doi: 10.1016/0091-6749(88)90168-6. [DOI] [PubMed] [Google Scholar]
- 10.Doyle WJ, Swarts JD. Eustachian tube-tensor veli palatini muscle-cranial base relationships in children and adults: an osteological study. International journal of pediatric otorhinolaryngology. 2010 Sep;74(9):986–990. doi: 10.1016/j.ijporl.2010.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bylander A. Comparison of eustachian tube function in children and adults with normal ears. Ann Otol Rhinol Laryngol Suppl. 1980 May-Jun;89(3 Pt 2):20–24. doi: 10.1177/00034894800890s308. [DOI] [PubMed] [Google Scholar]
- 12.Bylander A, Tjernstrom O. Changes in Eustachian tube function with age in children with normal ears. A longitudinal study. Acta Otolaryngol. 1983 Nov-Dec;96(5-6):467–477. doi: 10.3109/00016488309132733. [DOI] [PubMed] [Google Scholar]
- 13.Casselbrant ML, Swarts JD, Mandel EM, Doyle WJ. The Cephalic Index is not different among groups of children aged 36-48 months with chronic otitis media with effusion, recurrent acute otitis media and controls. Int J Pediatr Otorhinolaryngol. 2013 Mar;77(3):334–337. doi: 10.1016/j.ijporl.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cantekin EI, Saez CA, Bluestone CD, Bern SA. Airflow through the eustachian tube. The Annals of otology, rhinology, and laryngology. 1979 Sep-Oct;88(5 Pt 1):603–612. doi: 10.1177/000348947908800504. [DOI] [PubMed] [Google Scholar]
- 15.Bylander A. Function and dysfunction of the eustachian tube in children. Acta Otorhinolaryngol Belg. 1984;38(3):238–245. [PubMed] [Google Scholar]
- 16.Bylander A, Tjernstrom O, Ivarsson A. Pressure opening and closing functions of the eustachian tube in children and adults with normal ears. Acta Otolaryngol. 1983 Jan-Feb;95(1-2):55–62. doi: 10.3109/00016488309130915. [DOI] [PubMed] [Google Scholar]
- 17.Beery QC, Doyle WJ, Cantekin EI, Bluestone CD. Longitudinal assessment of Eustachian tube function in children. Laryngoscope. 1979 Sep;89(9 Pt 1):1446–1456. doi: 10.1002/lary.5540890910. [DOI] [PubMed] [Google Scholar]
- 18.Briggs DR, Applebaum EL, Noffsinger D. Eustachian tube function in children. J Otolaryngol. 1976 Feb;5(1):12–18. [PubMed] [Google Scholar]
- 19.Flisberg K, Ingelstedt S, Ortegren U. The valve and “locking” mechanisms of the eustachian tube. Acta Otolaryngol Suppl. 1963;182:57–68. doi: 10.3109/00016486309139993. [DOI] [PubMed] [Google Scholar]
- 20.Bluestone CD, Beery QC. Concepts on the pathogenesis of middle ear effusions. Ann Otol Rhinol Laryngol. 1976 Mar-Apr;85(2 Suppl 25 Pt 2):182–186. doi: 10.1177/00034894760850S235. [DOI] [PubMed] [Google Scholar]
- 21.Kanick SC, Doyle WJ. Barotrauma during air travel: predictions of a mathematical model. J Appl Physiol. 2005 May;98(5):1592–1602. doi: 10.1152/japplphysiol.00974.2004. [DOI] [PubMed] [Google Scholar]
- 22.Flisberg K. Ventilatory studies on the eustachian tube. A clinical investigation of cases with perforated ear drums. Acta Otolaryngol. 1966;(Suppl 219):211–282. doi: 10.3109/00016486609129562. [DOI] [PubMed] [Google Scholar]
- 23.Doyle WJ, Mandel EM, Seroky JT, Swarts JD, Casselbrant ML. Reproducibility of the forced response test in children with chronic otitis media with effusion. Otol Neurotol. 2013 Jan;34(1):16–21. doi: 10.1097/MAO.0b013e31827853f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elner A, Ingelstedt S, Ivarsson A. The normal function of the eustachian tube. A study of 102 cases. Acta Otolaryngol. 1971 Nov;72(5):320–328. doi: 10.3109/00016487109122489. [DOI] [PubMed] [Google Scholar]