Abstract
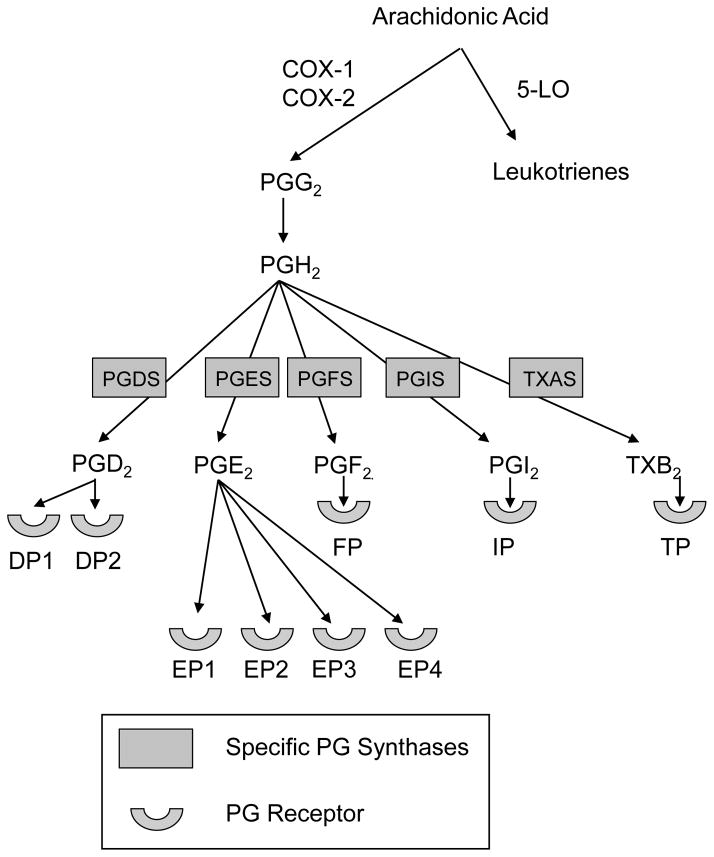
Prostaglandins are products of the cyclooxygenase pathway of arachidonic acid metabolism. There are five primary prostaglandins, PGD2, PGE2, PGF2, PGI2, and thromboxane B2, all of which signal through distinct seven transmembrane, G-protein coupled receptors. Some prostaglandins may counteract the actions of others, or even the same prostaglandin may have opposing physiologic or immunologic effects, depending on the specific receptor through which it signals. In this review, we will examine the effects of cyclooxygenase activity and the various prostaglandins on allergic airway inflammation and physiology that is associated with asthma. We also highlight the potential therapeutic benefit of targeting prostaglandins in allergic lung inflammation and asthma based on basic science, animal model, and human studies.
Prostaglandins are lipids derived from plasma and nuclear membranes that are produced by the actions of cyclooxygenase (COX) enzymes in the arachidonic acid metabolic pathway.1 Prostaglandins were discovered in the mid-1930s in independent laboratories led by von Euler and Goldblatt, and initial studies focused on their effects on blood pressure and smooth muscle constriction.2;3 One of the first publications that suggested prostaglandins had an important role in allergic disease was published by Piper and Vane in 1969.4 These investigators found that prostaglandin (PG) E2 and PGF2α were released during anaphylaxis of guinea pig lungs and their production could be blocked by low doses of aspirin and indomethacin. Subsequent to this discovery, myriad both pro- and anti-allergic effects have been attributed to prostaglandins. Early studies were hampered by the prostaglandin’s short biologic half-lives, on the order of seconds to a few minutes. However, the discoveries of how prostaglandins regulate allergic inflammation have accelerated in the last 15 years. This has largely been a result of the proliferation of transgenic mouse models in which either a prostaglandin receptor gene or synthase has been knocked out or overexpressed. In addition, the development of prostaglandin agonists that have longer biologic activity than a native prostaglandin, in addition to specific receptor antagonists, have greatly advanced both human and animal studies in our knowledge of how these regulate allergic diseases. In this article, we will review the pathways of prostaglandin generation, examine studies that confirm the presence of these products in allergic inflammatory states, and discuss in vivo intervention studies in humans and recent murine studies which elucidate the activity of these mediators in the pathogenesis of allergic disease. Based on this data, we speculate on individual prostaglandins as potential therapeutic targets in the treatment of allergic diseases and asthma.
Generation of prostaglandins by phospholipase A2
Arachidonic acid is the precursor for the synthesis of all prostaglandins and leukotrienes. These products of arachidonic acid metabolism are together known as eicosanoids because the Greek word for twenty is “eikosi”, the number of carbon atoms in arachidonic acid. There are several phospholipases A2 (PLA2) enzymes that hydrolyze fatty acids at the sn-2 position of membrane phospholipids, resulting in the formation of free fatty acids, including arachidonic acid.5 There are six classes of PLA2s, secretory PLA2s (sPLA2), cytosolic PLA2s (cPLA2), Ca2+ independent PLA2 (iPLA2), platelet-activating factor acetylhydrolases (PAF-AH), lysosomal PLA2s, and adipose-specific PLA2.5 The PLA2s are classified based upon the catalytic mechanism of the individual PLA2, in addition to their functional and structural properties. Sixteen groups of PLA2 have now been identified, however, the groups that lead to lipid mediator generation are limited to group IIA, group IVA, group V, group VI and group X.5;6
The sPLA2 are small enzymes (14–18 kDa) secreted from their cellular source.5 After secretion, the sPLA2s participate in either paracrine or autocrine generation of arachidonic acid from the outer leaflet of plasma membranes. Group IIA sPLA2 is critical in the generation of lysophosphatidyl choline for synthesis of LPA.5 Group V sPLA2 has an important role in the development of allergic airway inflammation in mice. For instance, in the house dust mite model, group V sPLA2-deficient mice had markedly decreased pulmonary inflammation and goblet cell metaplasia in comparison to wild type (WT) mice, likely a result of reduced antigen processing and maturation of antigen presenting cells.7 Mice deficient in group X sPLA2 had decreased bronchial inflammation, production of lung Th2 cytokines, airway remodeling, and concentrations of several lipid mediators in a model of ovalbumin (OVA)-induced airway disease. The importance of human group X sPLA2 to the allergic phenotype was verified when human group X sPLA2 was knocked-in to mice deficient in murine group X sPLA2.8 Group X sPLA2 is abundantly produced by the airway epithelium of asthmatic subjects and may have a critical role in asthma provoked by exercise and in the severe asthma phenotype by providing arachidonic acid for the rapid transformation to cysteinyl LTs.9–11
The cPLA2 are present in the cytosol and are larger than the sPLA2 (61–114 kDa).5 There are six subgroups (denoted A–F) of cPLA2 enzymes in group IV. This enzyme may have a role in asthma pathogenesis as group IVA cPLA2 was over-expressed in patients with persistent asthma.12
The group VI PLA2 are Ca2+ independent and termed iPLA2.5 Group VIA and group VIB iPLA2 act to generate arachidonic acid release for eicosanoid production. Group VIA is important in glycerophospholipid remodeling, protein expression, acetylcholine-modulated endothelium-dependent relaxation of vessels, apoptosis, and lymphocyte proliferation. Lastly, there are two groups of platelet-activating factor acetylhydrolases (PAF-AH), classified as groups VII and VIII. While PAF-AH is not known to participate in eicosanoid formation, inactivation of PAF by PAF-AH may have a protective role against anaphylaxis as persons with lower levels of PAH-AF had more severe manifestations of anaphylaxis than those with higher levels of PAF-AH.13
Thus, the PLA2 enzymes are critical for the generation of arachidonic acid from membrane phospholipids.
CYCLOOXYGENASE PATHWAY
Arachidonic acid can be oxidatively metabolized by both the COX and lipoxygenase (LO) pathways, but the COX pathway is the primary focus of this review.14 COX catalyzes two reactions, an initial cyclooxygenase reaction resulting in the insertion of two oxygen molecules into arachidonic acid to produce prostaglandin (PG)G2, with a subsequent endoperoxidase reaction that reduces PGG2 to PGH2 (Figure 1). PGH2 is the precursor for the prostanoids PGD2, PGE2, PGF2α, PGI2, and thromboxane A2 (TXA2). Each of the prostanoids is produced by tissue specific enzymes and isomerases that will be further discussed later. Two COX enzymes, COX-1 and COX-2, are functional in humans. A third cyclooxygenase enzyme, COX-3, is encoded by the COX-1 gene, but has an intron that is not retained in COX-1 and is not believed to be functional in humans. COX-1 and COX-2 are products of separate genes and have different biologic functions based on their divergent temporal and tissue-specific expression.14 The human COX-1 gene is present on chromosome 9 and is constitutively expressed in most tissues. COX-1 can be induced in specific instances and is thought to participate in homeostatic prostanoid synthesis.15 In contrast, COX-2 expression is usually induced and the induction is transient. The human COX-2 gene is located on chromosome 1. COX-2 expression is induced by the cytokines interleukin (IL)-1, IL-2, and TNF, as well as by lipopolysaccharide (LPS) produced by Gram-negative bacteria.15 While COX-2 is primarily considered to be an inducible enzyme, it is also constitutively expressed in cultured human lung epithelial cells, cortical thick ascending limb of the kidney, pancreatic islet cells, and in human gastric carcinoma.16–18 The ability of nonsteroidal anti-inflammatory drugs to inhibit COX-2 activity is likely their major therapeutic effect, while the inhibition of COX-1 may result in some of their undesired side effects.15 However, there are instances where inhibition of COX-2 may be harmful. For instance, there was an increase in cardiovascular disease resulted from medications that specifically inhibited COX-2, likely as a result PGI2, inhibition, while the COX-1 product TXA2 was unaffected.19
Figure 1.
Human studies of the COX pathway in allergic inflammation
Several investigators have examined COX-2 expression in the airway to help discern the role of this enzyme in allergic diseases; however, the results have been contradictory. For instance, one study reported a fourfold amplification in bronchial epithelial COX-2 immunostaining in asthmatic subjects compared to healthy controls;20 in contrast, another reported no difference in the level of immunostaining in asthmatics, chronic bronchitics, or controls who had no lung disease.21 Corticosteroids may decrease COX-2 mRNA expression and immunoreactive protein, as both of these were increased in the airway epithelium of asthmatics that had not been treated with corticosteroids compared with non-asthmatic controls. Possibly supporting this notion, corticosteroid-treated asthmatics had decreased COX-2 expression compared to non-treated asthmatics.22 The relationship between the cytokines implicated in the allergic response and COX-2 expression is complex. IL-4 and IL-13 inhibited PGE2 production in bronchial epithelial cells by reducing both COX-2 and microsomal PGE synthase (mPGES) via JAK1 and STAT6 signaling.23 Therefore, in persons with asthma, increased TNF expression might induce COX-2, while IL-4 and IL-13 might reduce COX-2 expression. Therefore, corticosteroids may modulate COX-2 expression by indirectly reducing IL-4 and IL-13, while in contrast, TNF in the asthmatic airway may induce COX-2. This concept is supported by in vitro data in which COX-2 immunoreactivity in cultured airway epithelial cells was decreased by corticosteroid treatment.24 Corticosteroids reduced basal and bradykinin-induced levels of PGE2 in airway epithelial cells, suggesting that COX-2 is the primary producer of PGE2 in airway epithelium.24 PGE2, as will be discussed later in this review, has potent anti-inflammatory properties when it signals through the EP2 receptor. Downregulation of COX-2 by corticosteroids may decrease PGE2 production, thus perhaps removing the brake PGE2 exerts on inflammation. This is a possible mechanism by which corticosteroids fail to reduce inflammation in certain patient populations and might lead to corticosteroid resistant asthma. There is controversy over the in vivo effect of corticosteroids on COX-1 and COX-2 expression in nasal polyp tissue. For instance, prednisone increased COX-2 mRNA expression in polyp tissue after two weeks of therapy, yet there was no effect on COX-1 mRNA expression.25 However, topical glucocorticoids significantly reduced the number of COX-1 expressing nasal polyp cells, yet had no effect on COX-2 expressing cells in nasal polyps.26
In addition to structural cells in the airway, COX-1 and COX-2 mRNA is present in resting human T lymphocytes.27 T cell activation did not alter COX-1 expression in T cells, yet T cell stimulation increased COX-2 mRNA levels with increased COX-2 protein and cyclooxygenase activity.27 Macrophages, endothelial cells, airway epithelial cells, airway smooth muscle cells, mast cells, eosinophils, and airway fibroblasts have the potential for inducible COX-2 expression.20;28 Therefore, COX expression is present in both resident airway cells and adaptive immune cells.
COX products are increased as a result of allergic inflammation. There is a significant increase in prostanoids in the bronchoalveolar (BAL) fluid of allergic asthmatics compared to healthy nonasthmatic controls. In addition, allergic antigen challenge of the airways further increases prostanoid production. There was a 12- to 22-fold increase in BAL fluid PGD2 and PGF2α levels in asthmatics compared to nonallergic subjects, and a 10-fold increase in these same metabolites in allergic asthmatics compared to nonasthmatic subjects who had allergic rhinitis.29 Segmental allergen challenge, a process where allergen is instilled to a segment of the lung via bronchoscopy, resulted in a 17- to 208-fold increase in the levels of PGD2, thromboxane (Tx) B2, and 6-keto-PGF1α, a PGI2 metabolite in allergic asthmatics.30 When these subjects were treated for three days with prednisone prior to segmental allergen challenge, there was no change in the BAL fluid prostanoid concentrations, suggesting that corticosteroids did not reduce COX pathway activation resulting from an allergic inflammatory stimulus,31 supporting the findings in patients with nasal polyps that were treated with prednisone discussed in the preceding paragraph.
Investigations blocking the COX pathway with medications such as indomethacin, which inhibits both COX-1 and COX-2, have been performed to determine the impact of COX products on allergen-induced airway inflammation and physiologic changes. Indomethacin did not change lung function before allergen challenge in either subjects with allergic asthma or allergic rhinitis that did not have asthma.32 However, indomethacin treatment decreased the forced expiratory volume in one second (FEV1) and specific airway conductance in nonasthmatic subjects with allergic rhinitis in response to inhaled allergen challenge.32 Indomethacin administration prior to allergen challenge caused a small, but significant reduction in specific airway conductance in subjects with allergic asthmatic subjects compared to placebo; however, this non-specific COX inhibitor did not alter allergen-induced alterations in FEV1.32 Indomethacin treatment also neither significantly changed airway responsiveness to histamine nor the immediate or late phase pulmonary response to allergen challenge in allergic asthmatics.33;34 In subjects with exercise-induced asthma, indomethacin did not change bronchoconstriction after exercise, but prevented refractoriness after exercise.35 The apparent complex effect of COX inhibition on lung function reflects the diversity of the individual prostanoids and the receptors with which they signal (see below). It is clear that some prostanoids may counteract the actions of others, or even the same prostanoid may have opposing physiologic or immunologic effects, depending on the specific receptor through which it signals.
Mouse studies of the COX pathway in allergic inflammation
Transgenic mice have been created with targeted deletions of the COX-1 and COX-2 genes and then subjected to models of OVA sensitization and challenge. COX-1 knock out (KO) mice that were OVA-sensitized and challenged had augmented lung eosinophilia, increased serum IgE levels, heightened airway responsiveness, greater numbers of CD4+ and CD8+ T cells, amplified levels of Th2 cytokines, and exaggerated concentrations of eotaxin and thymus- and activation-regulated chemokine (TARC, CCL17) compared to both COX-2 KO and WT control mice.36;37 These results suggest that COX-1-derived prostanoids are critical in maintaining homeostasis during allergen-induced airway inflammation. These studies which show that COX-1 inhibition increases allergic airway inflammation and airway responsiveness would suggest that that COX-1 overexpression might decrease allergen-induced inflammation and inhibit airway responsiveness. However, while airway epithelial cell targeted COX-1 overexpression reduced basal airway responsiveness, there was no effect on allergic inflammation.38 The role of COX-2 in allergic airway inflammation and bronchomotor tone has also been examined in animal models. One report indicated that COX-2 KO mice on a C57BL/6 genetic background had augmented serum IgE levels, vascular cell adhesion molecule-1 (VCAM-1) and intercellular adhesion molecule-1 (ICAM-1) levels compared to WT mice, while there were no differences in airway eosinophils or airway responsiveness.36;37 Supporting this result, other investigators reported that COX-2 KO mice, also on a C57BL/6 background, had increased allergen-induced lung eosinophilia as compared to WT mice.39
Studies employing pharmacologic inhibition complement and, in general, support the transgenic mouse models. WT BALB/c mice treated with indomethacin in the drinking water during both OVA sensitization and challenge had augmented Th2 cytokines in the lungs, greater pulmonary eosinophilia, and heightened airway responsiveness to methacholine compared to mice treated with vehicle.40 While BAL cysteinyl leukotriene levels were increased as a result of indomethacin treatment, 5-LO KO mice on a 129 genetic background, which could therefore not generate leukotrienes, also had augmented allergen-induced inflammation with indomethacin treatment. These results essentially rule out enhanced leukotriene production as a cause for the exaggerated inflammatory response in the indomethacin-treated mice.41 The augmented allergic inflammation with indomethacin treatment was dependent upon CD4+ cells; however, it was independent of IL-4, IL-4 receptor alpha signaling, and STAT6, factors important in the Th2 signaling pathway.42 This augmented allergic phenotype was not specific to indomethacin, as both COX-1 and COX-2 inhibitors independently augmented allergen-induced lung levels of IL-13 and methacholine responsiveness compared to vehicle-treated mice.43 COX-2 inhibition in a mouse model of atopic dermatitis that was induced epicutaneous OVA sensitization resulted in augmented eosinophil skin infiltration, increased total and antigen specific IgE, and a systemic Th2 response to antigen.44 The role of COX-2 in modulating airway tone has also been investigated in guinea pig models. COX-2 was induced during allergic inflammation in guinea pigs and the COX-2 inhibitor celecoxib significantly inhibited allergen-induced bronchoconstriction and release of COX products.45;46 Further, PGE2-induced contraction was abolished by COX-2 inhibition.47 Therefore, a number of studies reveal that COX inhibition during the development of allergic disease increased allergen-induced inflammation and airway responsiveness, implying that a COX product restrains allergic inflammation and possibly could be a therapeutic target for the treatment of allergic diseases such as asthma and atopic dermatitis.
It is important to note that in most of these mouse models of allergen-induced inflammation, COX was inhibited from the initial stage of antigen presentation throughout all allergen challenges. In human studies using indomethacin, COX inhibition transpired only during allergen challenge, long after initial antigen presentation and after the regulatory elements of allergic inflammation in the lung had been set in place. It is also important to note there is divergence between mouse and human studies in regard to airway physiology. For instance, while PGD2 causes bronchoconstriction in humans, this prostanoids fails to constrict mouse airways.48 Therefore, animal models of allergic lung disease, in which COX activity is inhibited either pharmacologically or by targeted gene deletion, may be better suited to identify the immunologic function of prostanoids, rather than the direct effects on end-organ physiology that are more often investigated in human studies.
Individual Prostanoids
Prostaglandin D2
PGD2 is the major mast cell-derived prostanoid and is elaborated in nanogram quantities in these cells in response to IgE-mediated activation.14 Eosinophils also synthesize PGD2.49 There are two different enzymes that produce PGD2, hematopoietic- and lipocalin- PGD2 synthases (H-PGDS and L-PGDS, respectively); H-PGDS produces PGD2 production in mast cells and other hematopoietic cells. In contrast, L-PGDS is present in oligodendrocytes, the choroid plexus, organs of the male genital tract, leptomeninges, and in humans and monkeys hearts. L-PGDS gene expression in the central nervous system can be regulated by glucocorticoid, thyroid, and estrogen hormones, while L-PGDS expression in the heart is regulated by estrogen. H-PGDS is expressed at high levels in human placenta, lung, adipose tissue, and fetal liver, while it is expressed at lower levels in the bone marrow, heart, lymph nodes, and appendix. H-PGDS is expressed not only in mast cells, but also in CD4+ Th2 lymphocytes, CD8+ Tc2 cells, megakaryocytes, dendritic cells (DCs), histiocytes, and Kupffer cells. PGD2 can be metabolized to PGF2α, 9α,11β-PGF2 (the stereoisomer of PGF2α), and the J series of prostanoids which includes PGJ2, Δ12-PGJ2, and 15d-PGJ2.14
All of the prostanoids signal through distinct seven transmembrane, G-protein coupled receptors (GPCRs). The receptors through which PGD2 signals are termed DP1 and DP2 (Figure 1).14 DP1 is expressed on mucus-secreting goblet cells in the nasal and colonic mucosa, nasal serous glands, vascular endothelium, Th2 cells, DCs, basophils, and eosinophils. DP1 stimulation activates adenylate cyclase, leading to an intracellular increase in cAMP levels and protein kinase A activity. DP2 is also known as chemoattractant receptor-like molecule expressed on Th2 cells (CRTH2). In addition to PGD2, other DP2 agonists include Δ12-PGJ2; 15-deoxy-Δ12,14PGJ2 (15d-PGJ2); 13,15-dihydro-15-keto-PGD2; 11-dehydro-TXB2; and the COX inhibitor indomethacin.50;51 DP2 is expressed on immune cells such as eosinophils, basophils, and the T cell subsets CD4+ Th2 and CD8+ Tc2 cells. PGD2 induces chemotaxis in each of the immune cells in a DP2-dependent manner. DP2 is preferentially expressed by IL-4+/IL-13+ T cells compared to IFN-γ+ T cells in the BAL fluid of subjects with asthmatic.52 DP2 signaling in eosinophils increases their release from bone marrow, stimulates their respiratory burst, augments the chemotactic response to other chemokines such as eotaxin, and primes them for degranulation. Further, DP2 signaling increased microvascular permeability, depletion of goblet cells, and constricted coronary arteries. In opposition to DP1 signaling, activation of DP2 decreased intracellular cAMP.14 Therefore, PGD2 signaling through DP2, through suppression of cAMP, would be predicted to facilitate allergic inflammation through its effect on chemotaxis and mediator release by effector cells. PGD2 and its immediate metabolite, 9α, 11β-PGF2 contracts smooth muscle and this is presumed to be predominantly mediated through the thromboxane TP receptor.53;54
Human studies of PGD2 in allergic inflammation
Inhalation challenge of human allergic asthmatic subjects with allergen to which the subjects were sensitized increased PGD2 in BAL fluid.55 PGD2 was also increased in the nasal lavage from subjects with allergic rhinitis,56 in tears from persons experiencing allergic conjunctivitis,57 and in the fluid obtained from experimentally produced skin blisters in patients with late phase reactions of the skin.58 In asthmatic subjects, the stable urinary PGD2 metabolite, 9α,11β-PGF2, was not altered by treatment with the COX-2 specific inhibitor celecoxib for three days, suggesting that PGD2 is predominantly produced by the activity of COX-1.59 In contrast, aspirin challenge of individuals with aspirin-exacerbated respiratory disease did not diminish PGD2 concentration in BAL fluids. PGD2 is a potent bronchoconstrictor and vasodilator, and potentiated airway responsiveness.60 Intranasal administration of PGD2 increased nasal resistance 10-fold more potently than histamine and 100-fold greater than bradykinin.61 PGD2 administration increased vascular leakage in the conjunctiva and skin,62 and resulted in eosinophil influx in the conjunctiva63 and trachea, 64 implicating it as having a pathogenic role in allergic disease. The vascular effects of PGD2 mostly reflect dilation mediated by DP1, whereas recruitment of effector cells is more likely to reflect chemotaxis via DP2.50;65 These data strongly suggest that PGD2 is involved in the pathogenesis of allergic diseases; however, there are no published studies that show that a specific PGD2 antagonist had a beneficial effect in the treatment of these disorders, despite the development of multiple DP1 and DP2 antagonists. Therefore, it is still not clear if PGD2 has a mechanistic role in allergen-induced inflammation. In regard to smooth muscle contraction by PGD2 released upon allergen exposure, TP receptor antagonists such as GR32191 partially antagonized the early bronchoconstrictor response, with other constrictor mediators, such as histamine and LTC4/LTD4, contributing to make up the difference.66
The therapeutic effects of DP2 antagonists have now also been examined in humans with asthma. In a randomized, double-blind, placebo-controlled trial in subjects with moderate-persistent asthma, the DP2 antagonist OC000459 significantly improved both quality of life and night-time symptom score.67 There was also a significant reduction in geometric mean sputum eosinophil count in the DP2 antagonist group compared to pre-treatment baseline, although this decrease was not significant compared to the placebo-treated group. Additional studies will be important to confirm the clinical usefulness DP2 antagonism in asthma.
Mouse studies of PGD2 in allergic inflammation
Studies in mice suggest a complex role for PGD2 in experimental allergic disease.68 Mice that overexpress L-PGDS had greater BAL fluid levels of Th2 cytokines, eotaxin, eosinophils, and lymphocytes after allergen sensitization and challenge compared to nontransgenic littermates.69 Aerosolized PGD2 administered one day prior to inhalational challenge with low-dose antigen increased BAL eosinophils, lymphocytes, and macrophages, in addition to IL-4 and IL-5, in sensitized mice.70 Such findings imply that PGD2 augments pulmonary Th2 responses.
Mouse studies exploring the role of DP1 in allergic inflammation have been contradictory. Allergen sensitized and challenged DP1 KO mice had significantly reduced airway responsiveness and BAL concentrations of IL-4, IL-5, and IL-13 compared to WT mice, while there was no difference in the BAL levels of IFN-γ.68 In addition, DP1 KO mice had decreased BAL eosinophils and lymphocytes compared to WT mice, implying that DP1 signaling was important in the full expression of allergic inflammation.68 However, the DP1 agonist BW245C inhibited lung DC function, including the ability of DCs to stimulate T cell proliferation and DC migration to the lungs.71;72 BW245C-treated mice, or mice receiving adoptively transferred DP1-treated DCs, had an increase in the number of Foxp3+ CD4+ regulatory T cells, which suppressed inflammation in an IL-10–dependent mechanism.72 The reduction in allergic inflammation caused by the DP1 agonist via diminished DC function was regulated via cyclic AMP-dependent protein kinase A.72 In addition, chimeric mice that lacked DP1 expression on hematopoietic cells had increased airway inflammation following allergen challenge, suggesting an important homeostatic role of DP1 and endogenous PGD2.72 Taken together, these results suggest that DP1 signaling facilitates effector responses through structural cells, yet inhibits DC function at the sensitization phase to reduce allergic inflammatory process.
Studies in different species support the concept that signaling through DP2 augments allergic inflammation. A DP2 receptor antagonist, AM211, reduced OVA-induced airway eosinophilia in guinea pigs, while inhibiting the number of sneezes mice experienced following intranasal allergen challenge.73 In addition, a different DP2 antagonist, MK-7246, reduced antigen-induced late phase bronchoconstriction and airway responsiveness in sheep, while inhibiting antigen-induced eosinophilia in both sheep and monkeys.74 Lastly, an oral, potently selective alkynylphenoxyacetic acid DP2 antagonist reduced OVA-induced airway eosinophilia in mice.75 These studies support that PGD2 signaling through DP2 increases allergic inflammation, and inhibiting receptor signaling blunts inflammatory responses in animals.
Prostaglandin E2
PGH2 can be metabolized to PGE2 by three distinct enzymes, microsomal PGE synthase-1 (mPGES-1), mPGES-2, and cytosolic PGE synthase (cPGES).14 mPGES-1 is membrane-associated, localized to the perinuclear area, has a trimeric structure, and is glutathione-dependent. PGE2 production was substantially greater in cells co-transfected with both mPGES-1 and COX-2, suggesting that mPGE-2 preferentially couples with COX-2 to immediately generate PGE2 when COX-2 is active. mPGES-1 metabolizes PGH2 produced from COX-1, but required exogenous administration of arachidonic acid. For instance, arachidonic acid generated by mast cell group IVA cPLA2 led to PGE2 production by mouse fibroblast mPGES-1.76 The expression of cPGES was predominantly constitutive and was not induced by inflammatory stimuli.51;77 Compared to mPGES-1, cPGES coupled more efficiently with COX-1 than with COX-2 for PGE2 generation. These results suggest that cPGE2 may provide PGE2 essential for cellular homeostasis, while mPGES-1 KO mice had significantly decreased basal PGE2 production in most organs. A recent study reported that mPGES-1 activity is inhibited in transformed cell lines by cysteinyl leukotriene receptor-1 antagonists;78 however, this has not been confirmed either in primary cells or in vivo. Studies in KO mice do not support that either cPGES or mPGES-2 are important PGESs enzymes in vivo. cPGES is localized to the cytosol and while there was evidence that it translocated from the cytosol to the nuclear membrane to assemble with COX-1 in PGE2 production, there seems that cPGES has a slight preference to interact with COX-2.79 Dexamethasone decreased cPGES activation.79 mPGES-2 is expressed constitutively in many cells and tissues.79 In transfected cells, mPGES-2 uses PGH2 derived from COX-1 and COX-2 with equal efficiency. Local PGE2 concentrations are regulated by COX-2 driven synthesis and PGE2 degradation by 15-hydroxyprostaglandin dehydrogenase (15-PGDH).80
PGE2 signals through four distinct GPCRs, termed EP receptors 1 through 4 (Figure 1).14 Each EP receptor has a distinct G protein coupling preference and downstream signal activation, and some of these signals counteract with one another. All four receptor subtypes are present in the lung and other organs associated with allergic responses.14 Signaling through the EP1 receptor increased cell Ca2+ and resulted in smooth muscle contraction. Activation of the EP2 and EP4 receptors increased intracellular cAMP concentrations, with resultant smooth muscle relaxation.81 EP2 is expressed most abundantly in the uterus, lung and spleen.82 Stimulation of the EP2 receptor inhibited mast cell mediator release. EP4 receptor expression is greatest in the kidney and peripheral blood leukocytes; however, high level EP4 expression occurs in the thymus, lung and a number of other tissues.83 EP3 receptors caused smooth muscle contraction by decreasing the rate of cAMP synthesis.84 EP3 receptors are unique because of the diversity created by multiple splice variants that produce alternate sequences in the C-terminal tail of this receptor subtype; however, the functional importance of these alternative splice variants is not well understood.82 Usually these splice variants of EP3 decrease cAMP generation, in contrast to signaling through EP2 and EP4 which increase cAMP.82 Therefore, PGE2 signaling may have opposing affects in different tissues dependent upon the relative contributions of the receptors that are stimulated in a given context.
Human studies of PGE2 in allergic inflammation
PGE2 is one of the most abundant COX products produced by the airway epithelium and smooth muscle.85;86 Several studies suggest that endogenous PGE2 may be bronchoprotective in human asthma.87 PGE2 produced by epithelial cells reduced vagal cholinergic contraction of airway smooth muscle.88 Bronchial epithelial cell-derived PGE2 also suppressed DC migration and pro-inflammatory cytokine protein expression.89 In this experiment, PGE2 inhibited dendritic cell by migration by signaling through the EP4 receptor, as DCs treated with an EP4 antagonist as well as DCs from EP4 KO mice had reduced inhibition by airway epithelial cells with respect to secretion of proinflammatory cytokines. There was an inverse correlation between the sputum levels of PGE2 from asthmatics and sputum eosinophil counts. This result suggests that higher levels of PGE2 may protect against airway eosinophila.90;91 PGE2 inhalation also decreased the pulmonary early and late phase responses to inhaled allergen.92;93 Inhaled PGE2 reduced the change in methacholine airway reactivity and blunted the number of airway eosinophils after inhaled allergen challenge.92 In addition, PGE2 inhibited both exercise-induced and aspirin-induced bronchoconstriction in patients sensitive to these challenges.94;95 Interestingly, although PGE2 significantly protected against decrements in pulmonary function in challenge models, it did not alter baseline FEV1 or methacholine reactivity.93 The results from these studies suggest that PGE2 has significant immunomodulatory properties than directly regulating airway caliber. This is supported by the observation that PGE2 inhalation prior to segmental allergen challenge significantly decreased BAL levels of PGD2, an important product of mast cell activation, and BAL concentrations of cys-LTs.96 Signaling through the EP4 receptor in human, guinea pig, and rat airways results in smooth muscle relaxation,97 whereas EP3 receptor signaling mediates the cough properties of PGE2.98 PGE2 in combination with the β2-adrenergic receptor agonist albuterol also reduced human airway smooth muscle migration and mitogenesis,99;100 revealing that PGE2 has a plethora of effects on airway function.
PGE2 is rapidly metabolized, leading investigators to use the more stable orally active PGE1 analogue, misoprostol, in studies of allergen-induced airway inflammation and lung function in humans. The effects of misoprostol in these studies have largely been negative. Misoprostol did not change pulmonary function, β2 agonist use, or asthma severity score in aspirin-sensitive asthmatics.101 In mild asthmatics, misoprostol did not later either baseline lung function or histamine reactivity; however, it did lead to significant gastrointestinal side effects in one-third of study participants.102 It is important to note that misoprostol is significantly less potent than PGE2 in stimulating adenylate cyclase.103
Despite its capacity to reduce eosinophilia and allergic early- and late-phase responses, in vitro studies demonstrate that PGE2 has the ability to either stimulate or suppress immune cell function. PGE2 reduced T cell secretion of the Th1 cytokines IL-2 and interferon-γ in vitro, resulting in enhanced T cell differentiation toward a Th2 cytokine profile.104–107 These in vitro results suggesting PGE2 promoted Type 2 cytokine production may be regulated at the antigen presentation. Myeloid DCs matured in the presence of IFN-γ produced Th1 CD4+ T lymphocyte responses, while DCs matured in PGE2 elicited Th2 responses.108 PGE2 induction of Th2 cytokine secretion, mostly through its activity at the time of antigen presentation, does not necessarily contradict in vivo human studies that have suggested PGE2 is anti-inflammatory. More recently, in combination with IL-23, PGE2 induced differentiation and expansion of CD4+ Th17, along with secretion of Th17 signature cytokines.109 Acute antigen challenge models probably more precisely reflect effector cell function, since allergic sensitization occurs much earlier in life.
In addition to PGE2’s activity in the development of CD4+ Th1 and Th2 cells, this prostanoid has important immunomodulatory effects on other inflammatory cells thought to be pathogenic in asthma. In a cell culture system, both PGE2 and cAMP reduced spontaneous eosinophil apoptosis, as did an EP2 agonist.110 Therefore, by prolonging eosinophil survival, PGE2 might increase the inflammatory potential of these cells in asthma. However, PGE2 was also reported to inhibit eosinophil chemotaxis, aggregation, degranulation, and IL-5-mediated survival.111;112 PGE2 inhibition of eosinophil trafficking was modulated through EP2 signaling.113 Therefore, the relevance of these in vitro findings to in vivo disease states is not clear.
PGE2 also regulated the secretion of granulocyte macrophage-colony stimulating factor (GM-CSF) from human airway smooth muscle cells114. The COX inhibitor indomethacin upregulated GM-CSF production by cultured human airway smooth muscle cells; however, exogenous PGE2 decreased this indomethacin-induced GM-CSF production, implying that PGE2 inhibited GM-CSF expression and the inflammation that is associated with this cytokine.114 In contrast, PGE2 augmented IL-6 and GM-CSF production resulting from IgE-mediated mast cell degranulation via signaling through EP1 and EP3 receptors.115 There are conflicting reports as to the effect of PGE2 on mast cell production of differing mediators. PGE2 has been reported to either reduce116–118 or enhance119;120 the release of histamine and other inflammatory mediators. It is possible that these differences may relate to the relative dominance of EP3 (activating) versus EP2 (inhibitory) signaling in a given mast cell population. For instance PGE2 can activate human mast cells through EP3, yet inhibit activation through the EP2-PKA signaling pathway.121
PGE2 is also thought to play a key role in aspirin-exacerbated respiratory disease (AERD) with inhibition of COX-1, but not COX-2, being closely aligned with the ability of NSAIDs such as aspirin to precipitate this form of bronchoconstriction.122 COX-1 inhibition blocks the production of endogenous PGE2, which restrains 5-LO-mediated cysteinyl leukotriene production which is, at least in part, responsible for the bronchoconstriction that occurs with NSAID ingestion. This concept is supported by studies which showed that inhaled PGE2 blunted both the increased urinary leukotriene E4 and bronchoconstriction that are characteristic of aspirin challenge in subjects with AERD.95;123 Ingestion of COX-2 inhibitors did not result in symptoms in subjects with AERD, suggesting that COX-1 mediated PGE2 production is protective in this process.124
One of the leading proposed mechanisms of AERD pathophysiology is that subjects with this condition have differential metabolism of arachidonic acid, resulting in decreased PGE2 production. For instance, unstimulated epithelial cells from polyp tissues from subjects with AERD produced significantly decreased PGE2 compared to nasal epithelial cells from healthy subjects.125 Related to this decrease in PGE2, incubation of these epithelial cells from subjects with AERD resulted in significantly increased 15-hydroyeicostetraenoic acid, a product of 5-LO.125 Similarly, nasal tissue from subjects with nasal polyposis and AERD had decreased COX-2 mRNA expression and PGE2 concentrations, yet increased LTC4 synthase (the enzyme that converts LTA4 to LTC4), 5-LO mRNA, and cysteinyl leukotriene levels, compared to healthy subjects or those with only chronic rhinosinusitis.126 This alteration in PGE2 production in AERD patients is not limited to nasal tissue, as airway fibroblasts from subjects with AERD had decreased PGE2 production compared to health subjects. In this investigation, there was a decreased in COX-1, but not COX-2, protein expression in the AERD subjects’ airway fibroblasts compared to those from healthy subjects.127 Fibroblasts from nasal tissue from subjects with AERD produced significantly less PGE2 following IL-1β stimulation compared to normal subjects or those with nasal polyps who were aspirin tolerant.128
There is not only a decrease in PGE2 production in tissue from subjects with AERD compared to healthy subjects, but also aberrant expression of PGE2 receptors in tissues from AERD subjects. There was a decreased density of EP2 expression, and an increased expression of cysteinyl leukotriene receptors, in nasal polyp tissue from AERD subjects compared to aspirin tolerant subjects.129 There was reduced EP2 expression on airway T cells, macrophages, mast cells, and neutrophils from AERD subjects compared to subject with aspirin tolerant asthma.130 There was also a significantly decreased percentage of neutrophils, mast cells, eosinophils, and T cells expressing EP2, but not EP1, EP3, or EP4 in nasal biopsies from subjects with AERD compared to aspirin tolerant controls.131
Investigations into possible genetic regulation of AERD using a candidate gene approach revealed that polymorphisms in the EP2 gene confer susceptibility to AERD. Evaluation of allelic association of 370 single nucleotide polymorphisms (SNPs) of genes that regulate the arachidonic acid metabolic cascade revealed multiple SNPs in the EP2 gene that were significantly associated with AERD.132 SNPs in the EP2 promoter gene, uS5, uS5b, and uS7 were significantly associated with AERD and analysis of haplotypes constructed to linkage disequilibrium patterns showed a significant association with AERD. The most significantly associated SNP, uS5, located in the regulatory region of the EP2 gene, was in a STATs-binding consensus sequence (AERD 31.1% versus control 22.1% [permutation P=0.0016] or versus aspirin-tolerant asthma 22.2% [permutation P=0.0017]). In an in vitro reporter assay, the site containing the uS5 allele showed reduced transcription activity. These results suggest that uS5 allele serves as a target of a transcription repressor protein.132 A functional SNP of the EP2 gene associated with risk of AIA should decrease the transcription level, resulting in reduction of the PGE2 retraining mechanism of inflammation and involvement in the molecular mechanism underlying AERD. In another study, genetic polymorphisms in EP2, EP3, EP4, the PGI2 receptor (IP), and the thromboxane A receptor (TP) were associated with AERD.133 Therefore, there is abundant data suggesting that decreased PGE2 production and reduced expression of EP2 on a variety of cell types is pathogenic in AERD.
Mouse studies of PGE2 in allergic inflammation
In the OVA-sensitization and challenge model, EP3 KO mice had increased allergic inflammation compared to WT mice, while there were no differences in the pulmonary allergic inflammation between WT, EP1 KO, EP2 KO, and EP4 KO mice.134 Compared to WT mice, EP3 KO mice had increased airway eosinophils, neutrophils, and lymphocytes, as well as increased IL-4, IL-5, and IL-13 in BAL fluid.134 Administration of the EP3 agonist AE-248 to OVA-sensitized and challenged WT mice significantly inhibited allergic airway cellularity and tended to inhibit airway mucus and airway responsiveness to methacholine.134 In ex vivo experiments, lungs from OVA-sensitized and challenged EP3-deficient or WT mice were harvested and then challenged with OVA.134 In these experiments, there was significantly decreased histamine and cys-LT in lungs from WT mice treated with an EP3 agonist, suggesting that PGE2 may signal through EP on mast cells in vivo to reduce mediator release.134 The results of these studies would not have been predicted from in vivo analyses, since EP3 receptor signaling causes mast cell activation in vitro, whereas EP2 receptor signaling is inhibitory.121 Other studies support the notion that PGE2 restrains allergic airway inflammation in mice. Subcutaneous PGE2 inhibited lung eosinophilia and Th2 cytokine protein expression in a house dust mite model of allergic inflammation.135 The effect of PGE2 on mouse mast cell function in vitro seems to contrast that of other cells involved in the allergic inflammatory response. For example, PGE2 stimulated mast cell chemotaxis and cytokine production through mTORC2 activation.136 The chemotactic activity of PGE2 on mouse mast cells occurs via EP3 activation.137
PGE2 expression is reduced in chronic allergen exposure, likely a result of allergic inflammation, and the consequence of this reduction in PGE2 is increased airway remodeling. In this model, there was an inverse relationship between the number of allergen challenges and both COX-2 and mPGES-1 expression in lung fibroblasts, resulting in decreased cytokine-induced PGE2 production.138 mPGES-1 produced PGE2 did not have an effect on allergen sensitization or effector T cell responses in a house dust mite model comparing the phenotype of mPGES-1 KO and WT mice.139 However, mPGES-1 KO mice had significantly increased vascular smooth muscle cells and thickness of intrapulmonary vessels following allergen challenge.139 These findings suggest that PGE2 produced by mPGES-1 protected the pulmonary vasculature from remodeling during allergen-induced lung inflammation. PGE2 also regulates airway tone in mice. Immunolologically naïve mice that lack 15-PGDH, the major catabolic enzyme of PGE2, and resulting elevated levels of PGE2, had reduced bronchoconstrictor response to methacholine.140 Similarly, mice that had increased PGE2 levels as a result of over-expression of PGE2 synthase in the lung had reduced methacholine-induced airway constriction.140 Thus PGE2 protected against lower airway bronchoconstriction, and other reports suggest that this effect is mediated through EP2. Pretreatment with aerosolized PGE2 inhibited methacholine-induced bronchoconstriction in WT, but not EP2 KO mice.141 In addition, methacholine-induced bronchoconstriction was reversed by aerosolized PGE2 in WT, but not EP2 KO mice.141 This concept was solidifed by another group that reported that PGE2-induced bronchodilation was a consequence of direct activation of EP2 receptors on airway smooth muscle, while PGE2 signaling through EP1 and EP3 led to bronchoconstriction.142 Taken together, these studies suggest that PGE2 regulates homeostasis of bronchomotor tone and pulmonary immune responses through different respective receptors. Based on the available animal data cited above, agents that stimulate EP2, or that antagonize EP1 and EP3, may be useful therapeutic targets for the treatment of asthma.
In vivo mouse experiments support the concept that PGE2 is critical in protection against aspirin-exacerbated respiratory disease. mPGES-1 KO mice with dust mite-induced allergic airway inflammation developed increased airways resistance, enhanced mast cell activation, and increased cysteinyl leukotriene production following lysine aspirin challenge.143 A stable PGE2 analog, 16, 16-dimethyl PGE2, significantly reduced lysine aspirin-induced airways resistance, mast cell-induced histamine release, and cysteinyl leukotriene generation. EP2 and EP4 receptor agonists had similar protective effects as 16, 16-dimethyl PGE2 on histamine and cysteinyl leukotriene levels, while the EP2 agonist reduced airways resistance to a greater degree than did the EP4 agonist. In this model, the lysine aspirin-induced airways resistance and histamine release was dependent on cysteinyl leukotrienes, providing evidence that PGE2 negatively regulates lysine aspirin-induced leukotriene-mediated airway constriction and inflammation. Further studies revealed that lysine aspirin-induced cysteinyl leukotriene and mast cell activation were dependent upon platelets adhering to granulocytes and signaling through the thromboxane receptor TP.143 Therefore, COX-1 mediated inhibition of PGE2 synthesis increases mast cell activation and platelet mediated TP-dependent cysteinyl leukotriene production.
Prostaglandin F2α
PGF2α is produced by PGF synthase (PGFS).144 PGFS has two main activities. First, PGFS catalyzes the formation of PGF2α from PGH2 by PGH2 9,11-endoperoxide reductase in the presence of NADPH. Second, PGFS catalyzes the conversion of PGF2α from PGD2 by PGD2 11-ketoreductase.144 The PGFS binding sites for PGH2 and PGD2 are proposed to be distinct.144 PGFS is expressed in lung and peripheral blood lymphocytes, suggesting a possible role in allergic diseases such as asthma.145 PGFS is inhibited by non-steroidal anti-inflammatory drugs (NSAIDS) such as indomethacin and this may partially explain the protective effect of this class of drugs in some gastrointestinal tumors in which PGFS activity is high.144 PGF2α binds a solitary receptor, termed FP (Figure 1) which is the most promiscuous of the prostanoid GPCRs in binding the principal prostaglandins. Both PGD2 and PGE2 both to FP at nanomolar concentrations.146 Selective FP agonists such as fluprostenol and latanoprost have been produced that are used in clinical settings as a result of these agents’ ocular hypotensive properties.146 PGF2α has critical functions in reproduction, renal physiology, and modulation of intraocular pressure. Tissue distribution of FP receptor mRNA expression is greatest in the ovarian corpus luteum, followed by the kidney, with lower-level expression in the lung, stomach, and heart.147 FP expression has not been detected in the spleen, thymus, or on immune cells. Therefore, in contrast to the other prostaglandins, PGF2α-FP receptor signaling does not seem to have an important role in inflammatory and immunological processes.146
Human studies of PGF2α
PGF2α has not been studied to nearly the same degree as PGD2 or PGE2 in allergic disease and asthma. PGF2α inhalation led to a dose-related decrease in specific airway conductance in both control and asthmatic subjects.148–150 While there has been a relatively small inter-individual variation in healthy control subjects in response to inhaled PGF2α, there has been a wide variation in the pulmonary function response to PGF2α in asthmatics.150 Asthmatics who inhaled PGF2α experienced wheezing, coughing and chest irritation within 3 to 4 minutes, while watery sputum also occurred shortly thereafter.150 Maximal decrease in specific airway conductance after PGF2α occurred 6 minutes after inhalation and recovery took place within 30 minutes.150 Asthmatic subjects experienced an approximate 150-fold greater sensitivity to PGF2α than did healthy controls, yet asthmatics were only 8.5-fold more sensitive to histamine than nonasthmatic subjects.150 There was decreased variation in individual responses to histamine compared to inhaled PGF2α challenge; however, there was a correlation of sensitivity to both mediators with each other.150 In general, women had a reduced bronchoconstrictor response to PGF2α compared to men.150 Both PGE2 and isoprenaline shortened recovery from the reduction in pulmonary function caused by inhalation of PGF2α; however, neither atropine, disodium cromoglycate, nor flufenamic acid prevented PGF2α-induced bronchoconstriction.150 PGF2α, and PGE2 as well, decreased exhaled nitric oxide (NO) concentrations in both healthy controls and asthmatic subjects; however, the meaning of this outcome is unknown.151 Although FP is not expressed on immune cells, there is some evidence that PGF2α may have a role on airway inflammation. In subjects with asthma, the magnitude of sputum eosinophilia correlated with the log sputum PGF2α concentrations, while there was an inverse correlation between sputum eosinophilia and PGE2 levels, and no correlation between the number of sputum eosinophils and sputum levels of cys-LTs, thromboxane, and PGD2.91
Mouse studies of PGF2α in allergic inflammation
To our knowledge, there are no published studies examining the effect of PGF2α administration or signaling through the FP receptor in the mouse allergen challenge model. An FP-deficient mouse has been created and these mice had attenuated bleomycin-induced pulmonary fibrosis independent of TGF-β expression.152 To date, no studies have examined whether FP-deficient mice are protected from collagen deposition and airway wall remodeling in a chronic allergen challenge model.
Prostaglandin I2
PGI2 is converted from PGH2 by PGI synthase (PGIS) and the gene encoding PGIS is located on chromosome 20q13.11-13.153 PGIS is strongly expressed in the heart, lung, smooth muscle, kidney, and ovary and expressed at moderate levels in the brain, pancreas, and prostate.153 There is low level PGIS expression in the placenta, spleen, and leukocytes.153 PGI2 signals through its receptor, IP, a GPCR (Figure 1).82 Binding of PGI2 to its receptor activates adenylate cyclase via Gs in a dose-dependent manner, increasing cAMP production.154 This increase in intracellular cAMP mediates the ability of PGI2 to inhibit platelet aggregation, thus dispersing existing platelet aggregates both in vitro and in human circulation.154 Northern blot analysis reveals that IP mRNA is expressed to the highest degree in the thymus, while high levels of IP mRNA expression are also found in spleen, heart, lung, and neurons in the dorsal root ganglia. IP is also expressed on mouse bone marrow-derived dendritic cells (BMDCs).155 The PGI2 analogs iloprost and cicaprost inhibited BMDC production of proinflammatory cytokines (IL-12, TNF-alpha, IL-1alpha, IL-6) and chemokines (MIP-1alpha, MCP-1), yet these analogs increased the production of the immunoinhibitory cytokine IL-10 by BMDCs.155 The modulatory effect was associated with IP-dependent increase in intracellular cAMP and reduction of NF-κB activity.155 Iloprost and cicaprost also inhibited LPS-induced expression of CD86, CD40, and MHC class II molecules by BMDCs and reduced the ability of BMDCs to stimulate antigen-specific CD4+ T cell proliferation and production of IL-5 and IL-13.155 Iloprost also enhanced human DC production of IL-10 and in co-culture experiments of iloprost-treated DCs and naïve T cells, there was induction of T regulatory cells.156 IP is also expressed in T cells of mice, along with the PGE2 receptor (EP) subtypes and the thromboxane receptor (TP).157 In addition IP is expressed by kidney smooth muscle and epithelial cells.158 Messenger RNA for IP is expressed in both CD4+ Th1 and Th2 cells.159 Thus, IP has been located on several different cell types, including those critical to the adaptive immune response.
Human studies of PGI2 in allergic inflammation
PGI2 and PGD2 were the major COX products produced in antigen-induced anaphylactic reactions of human lung parenchyma, on the order of 3- to 7-fold increased concentrations than that of the other prostanoids.160 The PGI2 metabolite 6-keto-PGF1α was present in concentrations 2-to-3-fold greater than all the other prostanoids in both airway and subpleural lung fragments in an in vitro anaphylaxis assay of passively sensitized human lung.161 Surprisingly, plasma 6-keto-PGF1α was increased subsequent to antigen challenge in which asthmatic subjects were pretreated with indomethacin.162 Thus, PGI2 is produced in abundance in allergic inflammatory responses in the lung, presumably a reflection of activated endothelial cells that express almost all the PGIS in the human airway.
Most of the published intervention studies examining the modulatory effect of PGI2 in human asthma were performed over 20 years ago and an important limitation of these older reports is that PGI2 (half-life 3–5 minutes) was used, rather than recently developed stable analogs. Therefore, these older studies may not accurately reflect the therapeutic capability of the currently available class of PGI2 agents. Pretreatment with PGI2 had no effect on allergen-induced immediate phase bronchoconstriction.163 In another study, PGI2 protected against both exercise and ultrasonic water-induced bronchospasm; however, it again had no effect on allergen-induced airway reactivity.164 Inhaled PGI2 also had no effect on specific airway conductance, but did result in consistent bronchodilation in two asthmatic subjects. In this study, there was a significant effect of PGI2 on the cardiovascular system. Inhaled PGI2 resulted in a fall in both diastolic (20±3 mmHg) and systolic (8±2 mmHg) blood pressure, as well as an increased pulse rate (29±3 beats per minute).165 Intravenous PGI2 administration had no effect on the fall in airflow induced by aspirin in subjects with aspirin-induced asthma.166 Somewhat contradictory results of the effect of inhaled PGI2 in subjects with mild asthma have been reported.167 In these studies PGI2 did not alter specific airway conductance, but resulted in a concentration-dependent decrease in FEV1. In contrast, these same investigators reported that PGI2 protected against bronchoconstriction induced by either PGD2 or methacholine. The authors proposed that these disparate findings might be explained by PGI2’s marked vasodilator effect, resulting in airway narrowing through mucosal blood engorgement, while this same phenomenon possibly reduced the spasmogenic properties of other inhaled mediators by increasing their clearance from the airways. An oral PGI2 analog (OP-41483) did not change FEV1 or airways responsiveness to methacholine in stable asthmatics.168 Since this last report which was published in 1991, to our knowledge, there has been only other published manuscript examining PGI2 in human allergic inflammation in the lung or asthma. In this report, the feasibility of administering inhaled iloprost to subjects with mild atopic asthma was examined.169 Subjects inhaled iloprost four times daily at either 2.5 or 5 μg for 14 days. In this safety study, chronic iloprost inhalation had did not have a negative effect on spirometry or methacholine responsiveness.169 The therapeutic potential of newer, more stable PGI2 analogs in asthma, already approved for use in pulmonary hypertension, remains unexplored.
Mouse studies of PGI2 in allergic inflammation
Four studies using mouse models suggest that endogenous PGI2 signaling through IP restrains allergic airway inflammation. In a model of short-term OVA challenge, IP KO mice had greater lung production of IL-4 and IL-5, serum antigen-specific and total IgE levels, and airway cellularlity compared to WT mice.170 In another study, the period of allergen challenge was extended to mimic chronic allergen exposure. In this report, IP KO mice had increased airway eosinophils and lymphocytes, Th2 cytokine levels, and hydroxyproline concentrations compared to WT mice.171 IP KO mice had increased inflammatory and physiologic changes compared to WT mice in the model of bleomycin-induced fibrosis.172 In another bleomycin model of lung injury, mice that overexpressed PGIS in airway epithelial cells were protected against lung injury and had decreased production of F2-isoprostanes, a marker of oxidant injury. In these experiments, PGI2 stimulated the expression of NAD(P)H:quinone oxidoreductase type I (NQO1), an enzyme that prevents generation of reactive oxidant species.173
Supporting the concept that PGI2 restrains airway inflammation, inhaled iloprost reduced maturation and migration of lung DCs to the mediastinal lymph nodes following intranasal antigen administration, resulting in decreased induction of an allergen-specific Th2 response in these nodes.174 In this in vivo model, iloprost-treated DCs also inhibited Th2 differentiation from naive T cells and did not boost effector cytokine production in primed Th2 cells.174 Not only did PGI2 downregulate mature DC function, but it also inhibited immature DC function. The PGI2 analog cicaprost decreased uptake of FITC-labeled OVA by immature BMDCs.175 In addition, cicaprost increased immature BMDC dissolution of podosomes, focal adhesion structures that are necessary for DC adherence to extracellular matrix in the lung and other tissues.175 When podosomes are dissolved, the DC is no longer tethered to the epithelium and can migrate to the regional lymph node. Podosome dissolution usually only takes place after the DC has taken up antigen; however, PGI2-regulated podosome dissolution allows for the DC to leave the environment-epithelial cell interface prior to antigen uptake. Cicaprost further increased pro-MMP-9 production, which has an essential role in DC egress from mucosal surfaces to draining lymph nodes.175 Further, cicaprost increased cell surface CCR7 expression with resultant chemotactic migration toward CCL19 and CCL21 produced in the T cell zone of the lymph node. These in vitro results suggested that cicaprost promoted migration of immature DCs from mucosal surface to draining lymph nodes and this concept was supported by the finding that migration of immature green fluorescent protein expressing BMDCs to draining lymph nodes was enhanced by pretreatment with cicaprost. Cicaprost-mediated inhibition of antigen uptake by immature DCs, enhanced podosome dissolution, heightened pro-MMP-9 production, and increased CCR7 expression were all dependent upon signaling through the IP receptor.175 These data reveal that PGI2 inhibits DC-mediated immune activation by enhancing immature DC migration and also by decreasing antigen uptake, providing two additional potential mechanisms by which PGI2 may be therapeutically beneficial in hypersensitivity diseases, such as asthma.
While these results in animal models of allergic inflammation are encouraging for the use of PGI2 in the treatment of allergic airway inflammation, cost and difficulty in drug delivery are currently obstacles.176;177 However, the development of less expensive and longer acting agonists may make stable analogs of PGI2 a viable therapeutic option.
Thromboxane A2
Thromboxane A2 (TXA2) is the major product of arachidonic acid metabolism formed by platelets and is a potent platelet aggregating agent.178 Thromboxane synthase (TXAS) is an endoplasmic reticulum membrane protein that catalyzes the conversion of prostaglandin H2 to thromboxane A2.179 TXAS is localized to band q33-q34 of the long arm of chromosome 7 in humans.179 TXAS is expressed abundantly in lung, liver, kidney, and blood cells, including megakaryocytes and monocytes.179 Lower, but still significant, levels of TXAS mRNA are observed in kidney, placenta and thymus.179 TXA2 is principally produced by platelets, monocytes, macrophages, neutrophils and lung parenchyma.180 After it is formed, TXA2 is nonezymatically hydrolyzed to thromboxane B2, which is further metabolized to the principle urinary metabolites 2,3-dinor-thromboxane B2 and 11-dehydro-thromboxane B2.181 The TXA2 receptor is termed TP (Figure 1) and there are two isoforms, TPα and TPβ, which are produced by alternative splicing occurring in the carboxy-terminal region after the seventh transmembrane domain.182 Both of these isoforms couple to a Gq protein resulting in phospholipase C activation, calcium release, and activation of protein kinase C.183 However, these receptor isoforms couple oppositely to adenylate cyclase, as TPα activates adenylate cyclase while TPβ inhibits this enzyme.184 The TP receptors are localized to both plasma membrane and cytosolic compartments and are mainly distributed in tissues rich in vasculature such as lung, heart and kidney.146 These GPCRs are involved in a myriad of physiological and pathological processes, including vasoconstriction that is implicated in vascular diseases such as hypertension, atherosclerosis, stroke, and myocardial infarction.185
Human studies of TXA2 in allergic inflammation
TXA2 has a half-life of approximately 30 seconds,186 and because of this lability there is a paucity of in vivo studies examining the effect of TXA2 in the human airway. TXB2 did not cause bronchoconstriction of human airway in vivo.187 However, TXA2 was a potent stimulant of in vitro smooth muscle constriction.178 TXA2 might have a role in the physiology associated with acute asthma exacerbations. Levels of TXA2 metabolites were increased 4–6 fold in the urine of patients admitted to the hospital with asthma compared to non-smoking controls admitted for other diagnoses.187 Allergic asthmatics subjected to inhaled allergen challenge had a significant increase in urinary excretion of TXA2 products;34;188 however, others have not found similar results.187 Inhibition of platelet COX by low dose aspirin inhibited the increase in urinary 2,3-dimer thromboxane, supporting the concept that allergen inhalation causes platelet activation. Allergic asthmatics pre-treated with indomethacin prior to inhaled allergen challenge resulted in a significant decrease in urinary TXA2 metabolites; however, no change in pulmonary function occurred.34 Subjects that experience ozone-induced airway hyperresponsiveness had significant greater concentrations of TXA2 in BAL in addition to airway neutrophilia.189 Similarly, LTB4 inhalation also resulted in greater levels of TXA2 and neutrophils in BAL fluid.190
TXA2 antagonists have been used in challenge models and in short-term studies in asthma to discern the effect of TXA2 on pulmonary function and airway reactivity. In a non-randomized, uncontrolled study the TP antagonist seratrodast (AA-2414) significantly reduced bronchial reactivity in asthmatic subjects after 4 weeks of once daily therapy compared to a pre-treatment baseline.191 Seratrodast had no effect on either exhaled nitric oxide or on the percentage of eosinophils in sputum.191 In a follow-up double blind, placebo-controlled study of asthmatic treated for four weeks, seratrodast treatment resulted in significant improvements in symptom score, peak expiratory flow (PEF) rates, diurnal variation of PEF, and bronchial responsiveness compared with placebo.192 These improvements were associated with a significant decrease in the number of submucosal eosinophils on bronchial biopsy.192 Seratrodast significantly decreased the number of cells in the epithelium expressing the chemokines RANTES (CCL5) and macrophage inflammatory protein (MIP)-1α (CCL3). Seratrodast also diminished the number of cells in the submucosa expressing monocyte chemotactic protein-3, RANTES, MIP-1α, and eotaxin (CCL11).192 These findings suggest that TXA2 antagonism inhibits allergic inflammation in the lung, although the mechanisms are not well defined.
Mouse studies of TXA2 in allergic inflammation
Both the TXA2 synthase inhibitor OKY-046 and the TP receptor antagonist S-1452 significantly reduced BAL total cells and eosinophils in a dose response relationship in OVA-sensitized and challenged mice.193 Treatment with either the TXA2 synthase inhibitor or the TP receptor antagonist significantly reduced antigen-specific activation of splenic mononuclear cells from sensitized mice in ex vivo experiments as defined by pro-inflammatory cytokine production.193 A recent study revealed that genetic deletion of TP receptors from mice lacking mPGES-1 prevented the development of dust mite-induced pulmonary eosinophilia, airway hyperresponsiveness, Th2 cytokine generation, and vascular remodeling.194 Thus, the pathogenic contributions from TXA2 may be amplified when local concentrations of PGE2 are low. The available mouse data suggests that inhibiting TP signaling, either through a receptor antagonist or through neutralizing TXA2, may be a therapeutic target in the treatment of asthma.
FIVE-YEAR VIEW
Future research will continue to expand understanding of PG signaling pathways and further identify therapeutic options in allergic lung disease and asthma. Specifically, research in the next five years will broaden our understanding of the molecular signaling pathways of PGs with further emphasis on modification of downstream gene expression. Further knowledge of these signaling pathways will provide additional therapeutic targets outside of traditional PG analogue therapy. The short half-life of PGs limits their potential use in vivo; however, discoveries in extending the bioactivity of PG analogs may increase their therapeutic applicability. One strategy for expanding the role of PG analogue therapy in asthma will be through the development of new delivery mechanisms in humans. Currently, several delivery options are being investigated in animal studies but have yet to be transitioned to human studies. PG receptor agonists and antagonists currently represent a promising option for therapy in asthma. However, further human studies will be needed to establish their role in the treatment of asthma. Together, these strategies represent the likely options for expanding the role of PGs in asthma therapy in the next five years.
KEY ISSUES.
COX inhibition, either by gene deletion or pharmacologic approach, augmented allergic inflammation in several animal models.
PGD2 is the major mast cell-derived prostanoid and is elaborated in nanogram quantities in these cells in response to IgE-mediated activation.
Mouse studies suggest that signaling through DP augments allergic inflammation and a DP2 antagonist significantly improved both quality of life and night-time symptom score in a randomized, double-blind, placebo-controlled trial in humans with moderate-persistent asthma.
PGE2 inhibits the cysteinyl leukotriene synthesis pathway and inhibition of PGE2 synthesis is a major pathogenic mechanism of aspirin exacerbated respiratory disease.
PGI2 restrains allergic airway inflammation in mice by inhibiting dendritic cell activation of CD4+ Th2 cells, Th2 cell differentiation, and eosinophil migration.
TXA2 is an inflammatory and bronchoconstrictive mediator in asthma.
PGF2α is a pro-fibrotic mediator in pulmonary fibrosis.
Future research will continue to expand understanding of the molecular signaling pathways of prostaglandins and further identify therapeutic options in pulmonary disease.
Acknowledgments
This work was supported by NIH Grants R01 AI 111820, U19 AI 095227-02, R01 HL 090664-04, and Veteran Affairs Grant 2I01BX000624.
Reference List
- 1.Ricciotti E, Fitzgerald GA. Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol. 2011;31(5):986–1000. doi: 10.1161/ATVBAHA.110.207449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldblatt MW. A depressor substance in seminal fluid. J Soc Chem Ind (Lond) 1933;52:1056–1057. [Google Scholar]
- 3.von Euler US. A depressor substance in the vesicular gland. J Physiol. 2014;84:21P. [Google Scholar]
- 4.Piper PJ, Vane JR. Release of additional factors in anaphylaxis and its antagonism by anti-inflammatory drugs. Nature. 1969;223(5201):29–35. doi: 10.1038/223029a0. [DOI] [PubMed] [Google Scholar]
- 5.Dennis EA, Cao J, Hsu YH, et al. Phospholipase A2 enzymes: physical structure, biological function, disease implication, chemical inhibition, and therapeutic intervention. Chem Rev. 2011;111(10):6130–6185. doi: 10.1021/cr200085w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balestrieri B, Hsu VW, Gilbert H, et al. Group V secretory phospholipase A2 translocates to the phagosome after zymosan stimulation of mouse peritoneal macrophages and regulates phagocytosis. J Biol Chem. 2006;281(10):6691–6698. doi: 10.1074/jbc.M508314200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giannattasio G, Fujioka D, Xing W, et al. Group V secretory phospholipase A2 reveals its role in house dust mite-induced allergic pulmonary inflammation by regulation of dendritic cell function. J Immunol. 2010;185(7):4430–4438. doi: 10.4049/jimmunol.1001384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henderson WR, Jr, Oslund RC, Bollinger JG, et al. Blockade of human group X secreted phospholipase A2 (GX-sPLA2)-induced airway inflammation and hyperresponsiveness in a mouse asthma model by a selective GX-sPLA2 inhibitor. J Biol Chem. 2011;286(32):28049–28055. doi: 10.1074/jbc.M111.235812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hallstrand TS, Chi EY, Singer AG, et al. Secreted phospholipase A2 group X overexpression in asthma and bronchial hyperresponsiveness. Am J Respir Crit Care Med. 2007;176(11):1072–1078. doi: 10.1164/rccm.200707-1088OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hallstrand TS, Lai Y, Ni Z, et al. Relationship between levels of secreted phospholipase A(2) groups IIA and X in the airways and asthma severity. Clin Exp Allergy. 2011;41(6):801–810. doi: 10.1111/j.1365-2222.2010.03676.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai Y, Oslund RC, Bollinger JG, et al. Eosinophil cysteinyl leukotriene synthesis mediated by exogenous secreted phospholipase A2 group X. J Biol Chem. 2010;285(53):41491–41500. doi: 10.1074/jbc.M110.153338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sokolowska M, Stefanska J, Wodz-Naskiewicz K, et al. Cytosolic phospholipase A2 group IVA is overexpressed in patients with persistent asthma and regulated by the promoter microsatellites. J Allergy Clin Immunol. 2010;125(6):1393–1395. doi: 10.1016/j.jaci.2010.02.016. [DOI] [PubMed] [Google Scholar]
- 13.Vadas P, Gold M, Perelman B, et al. Platelet-activating factor, PAF acetylhydrolase, and severe anaphylaxis. N Engl J Med. 2008;358(1):28–35. doi: 10.1056/NEJMoa070030. [DOI] [PubMed] [Google Scholar]
- 14.Smith WL, Urade Y, Jakobsson PJ. Enzymes of the cyclooxygenase pathways of prostanoid biosynthesis. Chem Rev. 2011;111(10):5821–5865. doi: 10.1021/cr2002992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kang YJ, Mbonye UR, Delong CJ, et al. Regulation of intracellular cyclooxygenase levels by gene transcription and protein degradation. Prog Lipid Res. 2007;46(2):108–125. doi: 10.1016/j.plipres.2007.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferguson S, Hebert RL, Laneuville O. NS-398 upregulates constitutive cyclooxygenase-2 expression in the M-1 cortical collecting duct cell line. J Am Soc Nephrol. 1999;10(11):2261–2271. doi: 10.1681/ASN.V10112261. [DOI] [PubMed] [Google Scholar]
- 17.Sorli CH, Zhang HJ, Armstrong MB, et al. Basal expression of cyclooxygenase-2 and nuclear factor-interleukin 6 are dominant and coordinately regulated by interleukin 1 in the pancreatic islet. Proc Natl Acad Sci U S A. 1998;95(4):1788–1793. doi: 10.1073/pnas.95.4.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soslow RA, Dannenberg AJ, Rush D, et al. COX-2 is expressed in human pulmonary, colonic, and mammary tumors. Cancer. 2000;89(12):2637–2645. doi: 10.1002/1097-0142(20001215)89:12<2637::aid-cncr17>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 19.Fitzgerald GA. Coxibs and cardiovascular disease. N Engl J Med. 2004;351(17):1709–1711. doi: 10.1056/NEJMp048288. [DOI] [PubMed] [Google Scholar]
- 20.Sousa A, Pfister R, Christie PE, et al. Enhanced expression of cyclo-oxygenase isoenzyme 2 (COX-2) in asthmatic airways and its cellular distribution in aspirin-sensitive asthma. Thorax. 1997;52(11):940–945. doi: 10.1136/thx.52.11.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Demoly P, Jaffuel D, Lequeux N, et al. Prostaglandin H synthase 1 and 2 immunoreactivities in the bronchial mucosa of asthmatics. Am J Respir Crit Care Med. 1997;155(2):670–675. doi: 10.1164/ajrccm.155.2.9032211. [DOI] [PubMed] [Google Scholar]
- 22.Redington AE, Meng QH, Springall DR, et al. Increased expression of inducible nitric oxide synthase and cyclo-oxygenase-2 in the airway epithelium of asthmatic subjects and regulation by corticosteroid treatment. Thorax. 2001;56(5):351–357. doi: 10.1136/thorax.56.5.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cho W, Kim Y, Jeoung DI, et al. IL-4 and IL-13 suppress prostaglandins production in human follicular dendritic cells by repressing COX-2 and mPGES-1 expression through JAK1 and STAT6. Mol Immunol. 2011;48(6–7):966–972. doi: 10.1016/j.molimm.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 24.Aksoy MO, Li X, Borenstein M, et al. Effects of topical corticosteroids on inflammatory mediator-induced eicosanoid release by human airway epithelial cells. J Allergy Clin Immunol. 1999;103(6):1081–1091. doi: 10.1016/s0091-6749(99)70183-1. [DOI] [PubMed] [Google Scholar]
- 25.Pujols L, Benitez P, Alobid I, et al. Glucocorticoid therapy increases COX-2 gene expression in nasal polyps in vivo. Eur Respir J. 2009;33(3):502–508. doi: 10.1183/09031936.00017408. [DOI] [PubMed] [Google Scholar]
- 26.Ebbens FA, Maldonado M, de Groot EJ, et al. Topical glucocorticoids downregulate COX-1 positive cells in nasal polyps. Allergy. 2009;64(1):96–103. doi: 10.1111/j.1398-9995.2008.01815.x. [DOI] [PubMed] [Google Scholar]
- 27.Iniguez MA, Punzon C, Fresno M. Induction of cyclooxygenase-2 on activated T lymphocytes: regulation of T cell activation by cyclooxygenase-2 inhibitors. J Immunol. 1999;163(1):111–119. [PubMed] [Google Scholar]
- 28.Kang YJ, Mbonye UR, Delong CJ, et al. Regulation of intracellular cyclooxygenase levels by gene transcription and protein degradation. Prog Lipid Res. 2007 doi: 10.1016/j.plipres.2007.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu MC, Bleecker ER, Lichtenstein LM, et al. Evidence for elevated levels of histamine, prostaglandin D2, and other bronchoconstricting prostaglandins in the airways of subjects with mild asthma. Am Rev Respir Dis. 1990;142(1):126–132. doi: 10.1164/ajrccm/142.1.126. [DOI] [PubMed] [Google Scholar]
- 30.Liu MC, Hubbard WC, Proud D, et al. Immediate and late inflammatory responses to ragweed antigen challenge of the peripheral airways in allergic asthmatics. Cellular, mediator, and permeability changes. Am Rev Respir Dis. 1991;144(1):51–58. doi: 10.1164/ajrccm/144.1.51. [DOI] [PubMed] [Google Scholar]
- 31.Liu MC, Proud D, Lichtenstein LM, et al. Effects of prednisone on the cellular responses and release of cytokines and mediators after segmental allergen challenge of asthmatic subjects. J Allergy Clin Immunol. 2001;108(1):29–38. doi: 10.1067/mai.2001.116004. [DOI] [PubMed] [Google Scholar]
- 32.Fish JE, Ankin MG, Adkinson NF, Jr, et al. Indomethacin modification of immediate-type immunologic airway responses in allergic asthmatic and non-asthmatic subjects: evidence for altered arachidonic acid metabolism in asthma. Am Rev Respir Dis. 1981;123(6):609–614. doi: 10.1164/arrd.1981.123.6.609. [DOI] [PubMed] [Google Scholar]
- 33.Kirby JG, Hargreave FE, Cockcroft DW, et al. Effect of indomethacin on allergen-induced asthmatic responses. J Appl Physiol. 1989;66(2):578–583. doi: 10.1152/jappl.1989.66.2.578. [DOI] [PubMed] [Google Scholar]
- 34.Sladek K, Dworski R, Fitzgerald GA, et al. Allergen-stimulated release of thromboxane A2 and leukotriene E4 in humans. Effect of indomethacin. Am Rev Respir Dis. 1990;141(6):1441–1445. doi: 10.1164/ajrccm/141.6.1441. [DOI] [PubMed] [Google Scholar]
- 35.O’Byrne PM, Jones GL. The effect of indomethacin on exercise-induced bronchoconstriction and refractoriness after exercise. Am Rev Respir Dis. 1986;134(1):69–72. doi: 10.1164/arrd.1986.134.1.69. [DOI] [PubMed] [Google Scholar]
- 36.Carey MA, Germolec DR, Bradbury JA, et al. Accentuated T helper type 2 airway response after allergen challenge in cyclooxygenase-1−/− but not cyclooxygenase-2−/− mice. Am J Respir Crit Care Med. 2003;167(11):1509–1515. doi: 10.1164/rccm.200211-1383OC. [DOI] [PubMed] [Google Scholar]
- 37.Zeldin DC, Wohlford-Lenane C, Chulada P, et al. Airway inflammation and responsiveness in prostaglandin H synthase-deficient mice exposed to bacterial lipopolysaccharide. Am J Respir Cell Mol Biol. 2001;25(4):457–465. doi: 10.1165/ajrcmb.25.4.4505. [DOI] [PubMed] [Google Scholar]
- 38.Card JW, Carey MA, Bradbury JA, et al. Cyclooxygenase–1 overexpression decreases Basal airway responsiveness but not allergic inflammation. J Immunol. 2006;177(7):4785–4793. doi: 10.4049/jimmunol.177.7.4785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakata J, Kondo M, Tamaoki J, et al. Augmentation of allergic inflammation in the airways of cyclooxygenase-2-deficient mice. Respirology. 2005;10(2):149–156. doi: 10.1111/j.1440-1843.2005.00687.x. [DOI] [PubMed] [Google Scholar]
- 40.Peebles RS, Jr, Dworski R, Collins RD, et al. Cyclooxygenase inhibition increases interleukin 5 and interleukin 13 production and airway hyperresponsiveness in allergic mice. Am J Respir Crit Care Med. 2000;162:676–681. doi: 10.1164/ajrccm.162.2.9911063. [DOI] [PubMed] [Google Scholar]
- 41.Peebles RS, Jr, Hashimoto K, Sheller JR, et al. Allergen-induced airway hyperresponsiveness mediated by cyclooxygenase inhibition is not dependent on 5-lipoxygenase or IL-5, but is IL-13 dependent. J Immunol. 2005;175(12):8253–8259. doi: 10.4049/jimmunol.175.12.8253. [DOI] [PubMed] [Google Scholar]
- 42.Hashimoto K, Sheller JR, Morrow JD, et al. Cyclooxygenase inhibition augments allergic inflammation through CD4-dependent, STAT6-independent mechanisms. J Immunol. 2005;174(1):525–532. doi: 10.4049/jimmunol.174.1.525. [DOI] [PubMed] [Google Scholar]
- 43.Peebles RS, Jr, Hashimoto K, Morrow JD, et al. Selective cyclooxygenase-1 and -2 inhibitors each increase allergic inflammation and airway hyperresponsiveness in mice. Am J Respir Crit Care Med. 2002;165(8):1154–1160. doi: 10.1164/ajrccm.165.8.2106025. [DOI] [PubMed] [Google Scholar]
- 44.Laouini D, Elkhal A, Yalcindag A, et al. COX-2 inhibition enhances the TH2 immune response to epicutaneous sensitization. J Allergy Clin Immunol. 2005;116(2):390–396. doi: 10.1016/j.jaci.2005.03.042. [DOI] [PubMed] [Google Scholar]
- 45.Oguma T, Asano K, Shiomi T, et al. Cyclooxygenase-2 expression during allergic inflammation in guinea-pig lungs. Am J Respir Crit Care Med. 2002;165(3):382–386. doi: 10.1164/ajrccm.165.3.2103093. [DOI] [PubMed] [Google Scholar]
- 46.Selg E, Lastbom L, Ryrfeldt A, et al. Effects of selective and non-selective COX inhibitors on antigen-induced release of prostanoid mediators and bronchoconstriction in the isolated perfused and ventilated guinea pig lung. Prostaglandins Leukot Essent Fatty Acids. 2008;78(2):89–97. doi: 10.1016/j.plefa.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 47.Safholm J, Dahlen SE, Delin I, et al. PGE2 maintains the tone of the guinea pig trachea through a balance between activation of contractile EP1 receptors and relaxant EP2 receptors. Br J Pharmacol. 2013;168(4):794–806. doi: 10.1111/j.1476-5381.2012.02189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martin TR, Gerard NP, Galli SJ, et al. Pulmonary responses to bronchoconstrictor agonists in the mouse. Journal of Applied Physiology. 1988;64(6):2318–2323. doi: 10.1152/jappl.1988.64.6.2318. [DOI] [PubMed] [Google Scholar]
- 49.Luna-Gomes T, Magalhaes KG, Mesquita-Santos FP, et al. Eosinophils as a novel cell source of prostaglandin D2: autocrine role in allergic inflammation. J Immunol. 2011;187(12):6518–6526. doi: 10.4049/jimmunol.1101806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hirai H, Tanaka K, Yoshie O, et al. Prostaglandin D2 Selectively Induces Chemotaxis in T Helper Type 2 Cells, Eosinophils, and Basophils via Seven-Transmembrane Receptor CRTH2. J Exp Med. 2001;193(2):255–262. doi: 10.1084/jem.193.2.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sugimoto H, Shichijo M, Okano M, et al. CRTH2-specific binding characteristics of [3H]ramatroban and its effects on PGD2-, 15-deoxy-Delta12, 14- Eur J Pharmacol. 2005;524(1–3):30–37. doi: 10.1016/j.ejphar.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 52.Mutalithas K, Guillen C, Day C, et al. CRTH2 expression on T cells in asthma. Clin Exp Immunol. 2010;161(1):34–40. doi: 10.1111/j.1365-2249.2010.04161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johnston SL, Freezer NJ, Ritter W, et al. Prostaglandin D2-induced bronchoconstriction is mediated only in part by the thromboxane prostanoid receptor. Eur Respir J. 1995;8(3):411–415. doi: 10.1183/09031936.95.08030411. [DOI] [PubMed] [Google Scholar]
- 54.Larsson AK, Hagfjard A, Dahlen SE, et al. Prostaglandin D(2) induces contractions through activation of TP receptors in peripheral lung tissue from the guinea pig. Eur J Pharmacol. 2011;669(1–3):136–142. doi: 10.1016/j.ejphar.2011.07.046. [DOI] [PubMed] [Google Scholar]
- 55.Murray M, Webb MS, O’Callaghan C, et al. Respiratory status and allergy after bronchiolitis. Archives of Disease in Childhood. 1992;67(4):482–487. doi: 10.1136/adc.67.4.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Naclerio RM, Meier HL, Kagey-Sobotka A, et al. Mediator release after nasal airway challenge with allergen. Am Rev Respir Dis. 1983;128(4):597–602. doi: 10.1164/arrd.1983.128.4.597. [DOI] [PubMed] [Google Scholar]
- 57.Proud D, Sweet J, Stein P, et al. Inflammatory mediator release on conjunctival provocation of allergic subjects with allergen. J Allergy Clin Immunol. 1990;85(5):896–905. doi: 10.1016/0091-6749(90)90075-f. [DOI] [PubMed] [Google Scholar]
- 58.Charlesworth EN, Kagey-Sobotka A, Schleimer RP, et al. Prednisone inhibits the appearance of inflammatory mediators and the influx of eosinophils and basophils associated with the cutaneous late- phase response to allergen. J Immunol. 1991;146(2):671–676. [PubMed] [Google Scholar]
- 59.Daham K, Song WL, Lawson JA, et al. Effects of celecoxib on major prostaglandins in asthma. Clin Exp Allergy. 2011;41(1):36–45. doi: 10.1111/j.1365-2222.2010.03617.x. [DOI] [PubMed] [Google Scholar]
- 60.Johnston SL, Freezer NJ, Ritter W, et al. Prostaglandin D2-induced bronchoconstriction is mediated only in part by the thromboxane prostanoid receptor. Eur Respir J. 1995;8(3):411–415. doi: 10.1183/09031936.95.08030411. [DOI] [PubMed] [Google Scholar]
- 61.Doyle WJ, Boehm S, Skoner DP. Physiologic responses to intranasal dose-response challenges with histamine, methacholine, bradykinin, and prostaglandin in adult volunteers with and without nasal allergy. J Allergy Clin Immunol. 1990;86(6 Pt 1):924–935. doi: 10.1016/s0091-6749(05)80156-3. [DOI] [PubMed] [Google Scholar]
- 62.Flower RJ, Harvey EA, Kingston WP. Inflammatory effects of prostaglandin D2 in rat and human skin. Br J Pharmacol. 1976;56(2):229–233. doi: 10.1111/j.1476-5381.1976.tb07446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Woodward DF, Hawley SB, Williams LS, et al. Studies on the ocular pharmacology of prostaglandin D2. Invest Ophthalmol Vis Sci. 1990;31(1):138–146. [PubMed] [Google Scholar]
- 64.Emery DL, Djokic TD, Graf PD, et al. Prostaglandin D2 causes accumulation of eosinophils in the lumen of the dog trachea. J Appl Physiol. 1989;67(3):959–962. doi: 10.1152/jappl.1989.67.3.959. [DOI] [PubMed] [Google Scholar]
- 65.Monneret G, Gravel S, Diamond M, et al. Prostaglandin D2 is a potent chemoattractant for human eosinophils that acts via a novel DP receptor. Blood. 2001;98(6):1942–1948. doi: 10.1182/blood.v98.6.1942. [DOI] [PubMed] [Google Scholar]
- 66.Beasley RC, Featherstone RL, Church MK, et al. Effect of a thromboxane receptor antagonist on PGD2- and allergen-induced bronchoconstriction. J Appl Physiol. 1989;66(4):1685–1693. doi: 10.1152/jappl.1989.66.4.1685. [DOI] [PubMed] [Google Scholar]
- 67.Barnes N, Pavord I, Chuchalin A, et al. A randomized, double-blind, placebo-controlled study of the CRTH2 antagonist OC000459 in moderate persistent asthma. Clin Exp Allergy. 2012;42(1):38–48. doi: 10.1111/j.1365-2222.2011.03813.x. [DOI] [PubMed] [Google Scholar]
- 68.Matsuoka T, Hirata M, Tanaka H, et al. Prostaglandin D2 as a mediator of allergic asthma. Science. 2000;287(5460):2013–2017. doi: 10.1126/science.287.5460.2013. [DOI] [PubMed] [Google Scholar]
- 69.Fujitani Y, Kanaoka Y, Aritake K, et al. Pronounced eosinophilic lung inflammation and Th2 cytokine release in human lipocalin-type prostaglandin D synthase transgenic mice. J Immunol. 2002;168(1):443–449. doi: 10.4049/jimmunol.168.1.443. [DOI] [PubMed] [Google Scholar]
- 70.Honda K, Arima M, Cheng G, et al. Prostaglandin D2 reinforces Th2 type inflammatory responses of airways to low-dose antigen through bronchial expression of macrophage-derived chemokine. J Exp Med. 2003;198(4):533–543. doi: 10.1084/jem.20022218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hammad H, de Heer HJ, Soullie T, et al. Prostaglandin D2 inhibits airway dendritic cell migration and function in steady state conditions by selective activation of the D prostanoid receptor 1. J Immunol. 2003;171(8):3936–3940. doi: 10.4049/jimmunol.171.8.3936. [DOI] [PubMed] [Google Scholar]
- 72.Hammad H, Kool M, Soullie T, et al. Activation of the D prostanoid 1 receptor suppresses asthma by modulation of lung dendritic cell function and induction of regulatory T cells. J Exp Med. 2007;204(2):357–367. doi: 10.1084/jem.20061196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bain G, Lorrain DS, Stebbins KJ, et al. Pharmacology of AM211, a potent and selective prostaglandin D2 receptor type 2 antagonist that is active in animal models of allergic inflammation. J Pharmacol Exp Ther. 2011;338(1):290–301. doi: 10.1124/jpet.111.180430. [DOI] [PubMed] [Google Scholar]
- 74.Gervais FG, Sawyer N, Stocco R, et al. Pharmacological characterization of MK-7246, a potent and selective CRTH2 (chemoattractant receptor-homologous molecule expressed on T-helper type 2 cells) antagonist. Mol Pharmacol. 2011;79(1):69–76. doi: 10.1124/mol.110.068585. [DOI] [PubMed] [Google Scholar]
- 75.Crosignani S, Pretre A, Jorand-Lebrun C, et al. Discovery of potent, selective, and orally bioavailable alkynylphenoxyacetic acid CRTH2 (DP2) receptor antagonists for the treatment of allergic inflammatory diseases. J Med Chem. 2011;54(20):7299–7317. doi: 10.1021/jm200866y. [DOI] [PubMed] [Google Scholar]
- 76.Ueno N, Taketomi Y, Yamamoto K, et al. Analysis of two major intracellular phospholipases A(2) (PLA(2)) in mast cells reveals crucial contribution of cytosolic PLA(2)alpha, not Ca(2+)-independent PLA(2)beta, to lipid mobilization in proximal mast cells and distal fibroblasts. J Biol Chem. 2011;286(43):37249–37263. doi: 10.1074/jbc.M111.290312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tanioka T, Nakatani Y, Semmyo N, et al. Molecular identification of cytosolic prostaglandin E2 synthase that is functionally coupled with cyclooxygenase-1 in immediate prostaglandin E2 biosynthesis. J Biol Chem. 2000;275(42):32775–32782. doi: 10.1074/jbc.M003504200. [DOI] [PubMed] [Google Scholar]
- 78.Kahnt AS, Rorsch F, Diehl O, et al. Cysteinyl leukotriene-receptor-1 antagonists interfere with PGE2 synthesis by inhibiting mPGES-1 activity. Biochem Pharmacol. 2013;86(2):286–296. doi: 10.1016/j.bcp.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 79.Park JY, Pillinger MH, Abramson SB. Prostaglandin E2 synthesis and secretion: the role of PGE2 synthases. Clin Immunol. 2006;119(3):229–240. doi: 10.1016/j.clim.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 80.Kalinski P. Regulation of immune responses by prostaglandin E2. J Immunol. 2012;188(1):21–28. doi: 10.4049/jimmunol.1101029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Coleman RA, Smith WL, Narumiya S. International Union of Pharmacology classification of prostanoid receptors: properties, distribution, and structure of the receptors and their subtypes [Review] [242 refs] Pharmacological Reviews. 1994;46(2):205–229. [PubMed] [Google Scholar]
- 82.Breyer RM, Bagdassarian CK, Myers SA, et al. Prostanoid receptors: subtypes and signaling. Annu Rev Pharmacol Toxicol. 2001;41:661–690. doi: 10.1146/annurev.pharmtox.41.1.661. [DOI] [PubMed] [Google Scholar]
- 83.An S, Yang J, Xia M, et al. Cloning and expression of the EP2 subtype of human receptors for prostaglandin E2. Biochemical & Biophysical Research Communications. 1993;197(1):263–270. doi: 10.1006/bbrc.1993.2470. [DOI] [PubMed] [Google Scholar]
- 84.Adam M, Boie Y, Rushmore TH, et al. Cloning and expression of three isoforms of the human EP3 prostanoid receptor. FEBS Letters. 1994;338(2):170–174. doi: 10.1016/0014-5793(94)80358-7. [DOI] [PubMed] [Google Scholar]
- 85.Churchill L, Chilton FH, Resau JH, et al. Cyclooxygenase metabolism of endogenous arachidonic acid by cultured human tracheal epithelial cells. Am Rev Respir Dis. 1989;140(2):449–459. doi: 10.1164/ajrccm/140.2.449. [DOI] [PubMed] [Google Scholar]
- 86.Delamere F, Holland E, Patel S, et al. Production of PGE2 by bovine cultured airway smooth muscle cells and its inhibition by cyclo-oxygenase inhibitors. Br J Pharmacol. 1994;111(4):983–988. doi: 10.1111/j.1476-5381.1994.tb14840.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pavord ID, Tattersfield AE. Bronchoprotective role for endogenous prostaglandin E2. Lancet. 1995;345(8947):436–438. doi: 10.1016/s0140-6736(95)90409-3. [DOI] [PubMed] [Google Scholar]
- 88.Barnett K, Jacoby DB, Nadel JA, et al. The effects of epithelial cell supernatant on contractions of isolated canine tracheal smooth muscle. Am Rev Respir Dis. 1988;138(4):780–783. doi: 10.1164/ajrccm/138.4.780. [DOI] [PubMed] [Google Scholar]
- 89.Schmidt LM, Belvisi MG, Bode KA, et al. Bronchial epithelial cell-derived prostaglandin E2 dampens the reactivity of dendritic cells. J Immunol. 2011;186(4):2095–2105. doi: 10.4049/jimmunol.1002414. [DOI] [PubMed] [Google Scholar]
- 90.Aggarwal S, Moodley YP, Thompson PJ, et al. Prostaglandin E2 and cysteinyl leukotriene concentrations in sputum: association with asthma severity and eosinophilic inflammation. Clin Exp Allergy. 2010;40(1):85–93. doi: 10.1111/j.1365-2222.2009.03386.x. [DOI] [PubMed] [Google Scholar]
- 91.Pavord ID, Ward R, Woltmann G, et al. Induced sputum eicosanoid concentrations in asthma. Am J Respir Crit Care Med. 1999;160(6):1905–1909. doi: 10.1164/ajrccm.160.6.9903114. [DOI] [PubMed] [Google Scholar]
- 92.Gauvreau GM, Watson RM, O’Byrne PM. Protective effects of inhaled PGE2 on allergen-induced airway responses and airway inflammation. American Journal of Respiratory & Critical Care Medicine. 1999;159(1):31–36. doi: 10.1164/ajrccm.159.1.9804030. [DOI] [PubMed] [Google Scholar]
- 93.Pavord ID, Wong CS, Williams J, et al. Effect of inhaled prostaglandin E2 on allergen-induced asthma. Am Rev Respir Dis. 1993;148(1):87–90. doi: 10.1164/ajrccm/148.1.87. [DOI] [PubMed] [Google Scholar]
- 94.Melillo E, Woolley KL, Manning PJ, et al. Effect of inhaled PGE2 on exercise-induced bronchoconstriction in asthmatic subjects. Am J Respir Crit Care Med. 1994;149(5):1138–1141. doi: 10.1164/ajrccm.149.5.8173753. [DOI] [PubMed] [Google Scholar]
- 95.Sestini P, Armetti L, Gambaro G, et al. Inhaled PGE2 prevents aspirin-induced bronchoconstriction and urinary LTE4 excretion in aspirin-sensitive asthma. Am J Respir Crit Care Med. 1996;153(2):572–575. doi: 10.1164/ajrccm.153.2.8564100. [DOI] [PubMed] [Google Scholar]
- 96.Hartert TV, Dworski RT, Mellen BG, et al. Prostaglandin E(2) decreases allergen-stimulated release of prostaglandin D(2) in airways of subjects with asthma. Am J Respir Crit Care Med. 2000;162(2 Pt 1):637–640. doi: 10.1164/ajrccm.162.2.9904038. [DOI] [PubMed] [Google Scholar]
- 97.Buckley J, Birrell MA, Maher SA, et al. EP4 receptor as a new target for bronchodilator therapy. Thorax. 2011;66(12):1029–1035. doi: 10.1136/thx.2010.158568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Maher SA, Birrell MA, Belvisi MG. Prostaglandin E2 mediates cough via the EP3 receptor: implications for future disease therapy. Am J Respir Crit Care Med. 2009;180(10):923–928. doi: 10.1164/rccm.200903-0388OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Goncharova EA, Goncharov DA, Zhao H, et al. beta2-adrenergic receptor agonists modulate human airway smooth muscle cell migration via vasodilator-stimulated phosphoprotein. Am J Respir Cell Mol Biol. 2012;46(1):48–54. doi: 10.1165/rcmb.2011-0217OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yan H, Deshpande DA, Misior AM, et al. Anti-mitogenic effects of beta-agonists and PGE2 on airway smooth muscle are PKA dependent. FASEB J. 2011;25(1):389–397. doi: 10.1096/fj.10-164798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wasiak W, Szmidt M. A six week double blind, placebo controlled, crossover study of the effect of misoprostol in the treatment of aspirin sensitive asthma. Thorax. 1999;54(10):900–904. doi: 10.1136/thx.54.10.900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Harmanci E, Ozakyol A, Ozdemir N, et al. Misoprostol has no favorable effect on bronchial hyperresponsiveness in mild asthmatics. Allerg Immunol (Paris) 1998;30(9):298–300. [PubMed] [Google Scholar]
- 103.Pawlotsky JM, Ruszniewski P, Reyl-Desmars F, et al. Effects of PGE2, misoprostol, and enprostil on guinea pig enterocyte adenylate cyclase. Clinical implications Dig Dis Sci. 1993;38(2):316–320. doi: 10.1007/BF01307550. [DOI] [PubMed] [Google Scholar]
- 104.Betz M, Fox BS. Prostaglandin E2 inhibits production of Th1 lymphokines but not of Th2 lymphokines. Journal of Immunology. 1991;146(1):108–113. [PubMed] [Google Scholar]
- 105.Snijdewint FG, Kalinski P, Wierenga EA, et al. Prostaglandin E2 differentially modulates cytokine secretion profiles of human T helper lymphocytes. Journal of Immunology. 1993;150(12):5321–5329. [PubMed] [Google Scholar]
- 106.Katamura K, Shintaku N, Yamauchi Y, et al. Prostaglandin E2 at priming of naive CD4+ T cells inhibits acquisition of ability to produce IFN-gamma and IL-2, but not IL- 4 and IL-5. Journal of Immunology. 1995;155(10):4604–4612. [PubMed] [Google Scholar]
- 107.Hilkens CM, Vermeulen H, van Neerven RJ, et al. Differential modulation of T helper type 1 (Th1) and T helper type 2 (Th2) cytokine secretion by prostaglandin E2 critically depends on interleukin-2. European Journal of Immunology. 1995;25(1):59–63. doi: 10.1002/eji.1830250112. [DOI] [PubMed] [Google Scholar]
- 108.Vieira PL, de Jong EC, Wierenga EA, et al. Development of Th1-inducing capacity in myeloid dendritic cells requires environmental instruction. Journal of Immunology. 2000;164(9):4507–4512. doi: 10.4049/jimmunol.164.9.4507. [DOI] [PubMed] [Google Scholar]
- 109.Chizzolini C, Chicheportiche R, Alvarez M, et al. Prostaglandin E2 synergistically with interleukin-23 favors human Th17 expansion. Blood. 2008;112(9):3696–3703. doi: 10.1182/blood-2008-05-155408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Peacock CD, Misso NL, Watkins DN, et al. PGE 2 and dibutyryl cyclic adenosine monophosphate prolong eosinophil survival in vitro. J Allergy Clin Immunol. 1999;104(1):153–162. doi: 10.1016/s0091-6749(99)70127-2. [DOI] [PubMed] [Google Scholar]
- 111.Kita H, Abu-Ghazaleh RI, Gleich GJ, et al. Regulation of Ig-induced eosinophil degranulation by adenosine 3′,5′-cyclic monophosphate. J Immunol. 1991;146(8):2712–2718. [PubMed] [Google Scholar]
- 112.Teixeira MM, al Rashed S, Rossi AG, et al. Characterization of the prostanoid receptors mediating inhibition of PAF-induced aggregation of guinea-pig eosinophils. Br J Pharmacol. 1997;121(1):77–82. doi: 10.1038/sj.bjp.0701107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sturm EM, Schratl P, Schuligoi R, et al. Prostaglandin E2 inhibits eosinophil trafficking through E-prostanoid 2 receptors. J Immunol. 2008;181(10):7273–7283. doi: 10.4049/jimmunol.181.10.7273. [DOI] [PubMed] [Google Scholar]
- 114.Lazzeri N, Belvisi MG, Patel HJ, et al. Effects of prostaglandin E2 and cAMP elevating drugs on GM-CSF release by cultured human airway smooth muscle cells. Relevance to asthma therapy. Am J Respir Cell Mol Biol. 2001;24(1):44–48. doi: 10.1165/ajrcmb.24.1.4027. [DOI] [PubMed] [Google Scholar]
- 115.Gomi K, Zhu FG, Marshall JS. Prostaglandin E2 selectively enhances the IgE-mediated production of IL- 6 and granulocyte-macrophage colony-stimulating factor by mast cells through an EP1/EP3-dependent mechanism. J Immunol. 2000;165(11):6545–6552. doi: 10.4049/jimmunol.165.11.6545. [DOI] [PubMed] [Google Scholar]
- 116.Hogaboam CM, Bissonnette EY, Chin BC, et al. Prostaglandins inhibit inflammatory mediator release from rat mast cells. Gastroenterology. 1993;104(1):122–129. doi: 10.1016/0016-5085(93)90843-2. [DOI] [PubMed] [Google Scholar]
- 117.Kaliner M, Austen KF. Cyclic AMP, ATP, and reversed anaphylactic histamine release from rat mast cells. J Immunol. 1974;112(2):664–674. [PubMed] [Google Scholar]
- 118.Peachell PT, MacGlashan DW, Jr, Lichtenstein LM, et al. Regulation of human basophil and lung mast cell function by cyclic adenosine monophosphate. J Immunol. 1988;140(2):571–579. [PubMed] [Google Scholar]
- 119.Leal-Berumen I, O’Byrne P, Gupta A, et al. Prostanoid enhancement of interleukin-6 production by rat peritoneal mast cells. J Immunol. 1995;154(9):4759–4767. [PubMed] [Google Scholar]
- 120.Nishigaki N, Negishi M, Honda A, et al. Identification of prostaglandin E receptor ‘EP2’ cloned from mastocytoma cells EP4 subtype. FEBS Lett. 1995;364(3):339–341. doi: 10.1016/0014-5793(95)00421-5. [DOI] [PubMed] [Google Scholar]
- 121.Feng C, Beller EM, Bagga S, et al. Human mast cells express multiple EP receptors for prostaglandin E2 that differentially modulate activation responses. Blood. 2006;107(8):3243–3250. doi: 10.1182/blood-2005-07-2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Mastalerz L, Sanak M, Gawlewicz-Mroczka A, et al. Prostaglandin E2 systemic production in patients with asthma with and without aspirin hypersensitivity. Thorax. 2008;63(1):27–34. doi: 10.1136/thx.2007.080903. [DOI] [PubMed] [Google Scholar]
- 123.Szczeklik A, Mastalerz L, Nizankowska E, et al. Protective and bronchodilator effects of prostaglandin E and salbutamol in aspirin-induced asthma. Am J Respir Crit Care Med. 1996;153(2):567–571. doi: 10.1164/ajrccm.153.2.8564099. [DOI] [PubMed] [Google Scholar]
- 124.Gyllfors P, Bochenek G, Overholt J, et al. Biochemical and clinical evidence that aspirin-intolerant asthmatic subjects tolerate the cyclooxygenase 2-selective analgetic drug celecoxib. J Allergy Clin Immunol. 2003;111(5):1116–1121. doi: 10.1067/mai.2003.1450. [DOI] [PubMed] [Google Scholar]
- 125.Kowalski ML, Pawliczak R, Wozniak J, et al. Differential metabolism of arachidonic acid in nasal polyp epithelial cells cultured from aspirin-sensitive and aspirin-tolerant patients. Am J Respir Crit Care Med. 2000;161(2 Pt 1):391–398. doi: 10.1164/ajrccm.161.2.9902034. [DOI] [PubMed] [Google Scholar]
- 126.Perez-Novo CA, Watelet JB, Claeys C, et al. Prostaglandin, leukotriene, and lipoxin balance in chronic rhinosinusitis with and without nasal polyposis. J Allergy Clin Immunol. 2005;115(6):1189–1196. doi: 10.1016/j.jaci.2005.02.029. [DOI] [PubMed] [Google Scholar]
- 127.Pierzchalska M, Szabo Z, Sanak M, et al. Deficient prostaglandin E2 production by bronchial fibroblasts of asthmatic patients, with special reference to aspirin-induced asthma. J Allergy Clin Immunol. 2003;111(5):1041–1048. doi: 10.1067/mai.2003.1491. [DOI] [PubMed] [Google Scholar]
- 128.Roca-Ferrer J, Garcia-Garcia FJ, Pereda J, et al. Reduced expression of COXs and production of prostaglandin E(2) in patients with nasal polyps with or without aspirin-intolerant asthma. J Allergy Clin Immunol. 2011;128(1):66–72. doi: 10.1016/j.jaci.2011.01.065. [DOI] [PubMed] [Google Scholar]
- 129.Adamusiak AM, Stasikowska-Kanicka O, Lewandowska-Polak A, et al. Expression of arachidonate metabolism enzymes and receptors in nasal polyps of aspirin-hypersensitive asthmatics. Int Arch Allergy Immunol. 2012;157(4):354–362. doi: 10.1159/000329744. [DOI] [PubMed] [Google Scholar]
- 130.Corrigan CJ, Napoli RL, Meng Q, et al. Reduced expression of the prostaglandin E2 receptor E-prostanoid 2 on bronchial mucosal leukocytes in patients with aspirin-sensitive asthma. J Allergy Clin Immunol. 2012;129(6):1636–1646. doi: 10.1016/j.jaci.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 131.Ying S, Meng Q, Scadding G, et al. Aspirin-sensitive rhinosinusitis is associated with reduced E-prostanoid 2 receptor expression on nasal mucosal inflammatory cells. J Allergy Clin Immunol. 2006;117(2):312–318. doi: 10.1016/j.jaci.2005.10.037. [DOI] [PubMed] [Google Scholar]
- 132.Jinnai N, Sakagami T, Sekigawa T, et al. Polymorphisms in the prostaglandin E2 receptor subtype 2 gene confer susceptibility to aspirin-intolerant asthma: a candidate gene approach. Hum Mol Genet. 2004;13(24):3203–3217. doi: 10.1093/hmg/ddh332. [DOI] [PubMed] [Google Scholar]
- 133.Kim SH, Kim YK, Park HW, et al. Association between polymorphisms in prostanoid receptor genes and aspirin-intolerant asthma. Pharmacogenet Genomics. 2007;17(4):295–304. doi: 10.1097/01.fpc.0000239977.61841.fe. [DOI] [PubMed] [Google Scholar]
- 134.Kunikata T, Yamane H, Segi E, et al. Suppression of allergic inflammation by the prostaglandin E receptor subtype EP3. Nat Immunol. 2005;6(5):524–531. doi: 10.1038/ni1188. [DOI] [PubMed] [Google Scholar]
- 135.Herrerias A, Torres R, Serra M, et al. Subcutaneous prostaglandin E(2) restrains airway mast cell activity in vivo and reduces lung eosinophilia and Th(2) cytokine overproduction in house dust mite-sensitive mice. Int Arch Allergy Immunol. 2009;149(4):323–332. doi: 10.1159/000205578. [DOI] [PubMed] [Google Scholar]
- 136.Kuehn HS, Jung MY, Beaven MA, et al. Prostaglandin E2 activates and utilizes mTORC2 as a central signaling locus for the regulation of mast cell chemotaxis and mediator release. J Biol Chem. 2011;286(1):391–402. doi: 10.1074/jbc.M110.164772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Weller CL, Collington SJ, Hartnell A, et al. Chemotactic action of prostaglandin E2 on mouse mast cells acting via the PGE2 receptor 3. Proc Natl Acad Sci U S A. 2007;104(28):11712–11717. doi: 10.1073/pnas.0701700104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Stumm CL, Wettlaufer SH, Jancar S, et al. Airway remodeling in murine asthma correlates with a defect in PGE2 synthesis by lung fibroblasts. Am J Physiol Lung Cell Mol Physiol. 2011;301(5):L636–L644. doi: 10.1152/ajplung.00158.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Lundequist A, Nallamshetty SN, Xing W, et al. Prostaglandin E(2) exerts homeostatic regulation of pulmonary vascular remodeling in allergic airway inflammation. J Immunol. 2010;184(1):433–441. doi: 10.4049/jimmunol.0902835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hartney JM, Coggins KG, Tilley SL, et al. Prostaglandin E2 protects lower airways against bronchoconstriction. Am J Physiol Lung Cell Mol Physiol. 2006;290(1):L105–L113. doi: 10.1152/ajplung.00221.2005. [DOI] [PubMed] [Google Scholar]
- 141.Sheller JR, Mitchell D, Meyrick B, et al. EP(2) receptor mediates bronchodilation by PGE(2) in mice. J Appl Physiol. 2000;88(6):2214–2218. doi: 10.1152/jappl.2000.88.6.2214. [DOI] [PubMed] [Google Scholar]
- 142.Tilley SL, Hartney JM, Erikson CJ, et al. Receptors and pathways mediating the effects of prostaglandin E2 on airway tone. Am J Physiol Lung Cell Mol Physiol. 2003;284(4):L599–L606. doi: 10.1152/ajplung.00324.2002. [DOI] [PubMed] [Google Scholar]
- 143.Liu T, Laidlaw TM, Katz HR, et al. Prostaglandin E2 deficiency causes a phenotype of aspirin sensitivity that depends on platelets and cysteinyl leukotrienes. Proc Natl Acad Sci U S A. 2013;110(42):16987–16992. doi: 10.1073/pnas.1313185110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Komoto J, Yamada T, Watanabe K, et al. Prostaglandin F2alpha formation from prostaglandin H2 by prostaglandin F synthase (PGFS): crystal structure of PGFS containing bimatoprost. Biochemistry. 2006;45(7):1987–1996. doi: 10.1021/bi051861t. [DOI] [PubMed] [Google Scholar]
- 145.Suzuki-Yamamoto T, Nishizawa M, Fukui M, et al. cDNA cloning, expression and characterization of human prostaglandin F synthase. FEBS Lett. 1999;462(3):335–340. doi: 10.1016/s0014-5793(99)01551-3. [DOI] [PubMed] [Google Scholar]
- 146.Hata AN, Breyer RM. Pharmacology and signaling of prostaglandin receptors: multiple roles in inflammation and immune modulation. Pharmacol Ther. 2004;103(2):147–166. doi: 10.1016/j.pharmthera.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 147.Breyer MD, Breyer RM. G protein-coupled prostanoid receptors and the kidney. Annu Rev Physiol. 2001;63:579–605. doi: 10.1146/annurev.physiol.63.1.579. [DOI] [PubMed] [Google Scholar]
- 148.Mathe AA, Hedqvist P, Holmgren A, et al. Bronchial hyperreactivity to prostaglandin F 2 and histamine in patients with asthma. Br Med J. 1973;1(5847):193–196. doi: 10.1136/bmj.1.5847.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Smith AP, Cuthbert MF. Prostaglandins and resistance to beta adrenoceptor stimulants. Br Med J. 1972;2(806):166. doi: 10.1136/bmj.2.5806.166-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Smith AP, Cuthbert MF, Dunlop LS. Effects of inhaled prostaglandins E1, E2, and F2alpha on the airway resistance of healthy and asthmatic man. Clin Sci Mol Med. 1975;48(5):421–430. doi: 10.1042/cs0480421. [DOI] [PubMed] [Google Scholar]
- 151.Kharitonov SA, Sapienza MA, Barnes PJ, et al. Prostaglandins E2 and F2alpha reduce exhaled nitric oxide in normal and asthmatic subjects irrespective of airway caliber changes. Am J Respir Crit Care Med. 1998;158(5 Pt 1):1374–1378. doi: 10.1164/ajrccm.158.5.9707076. [DOI] [PubMed] [Google Scholar]
- 152.Oga T, Matsuoka T, Yao C, et al. Prostaglandin F(2alpha) receptor signaling facilitates bleomycin-induced pulmonary fibrosis independently of transforming growth factor-beta. Nat Med. 2009;15(12):1426–1430. doi: 10.1038/nm.2066. [DOI] [PubMed] [Google Scholar]
- 153.Nakayama T. Prostacyclin analogues: prevention of cardiovascular diseases. Cardiovasc Hematol Agents Med Chem. 2006;4(4):351–359. doi: 10.2174/187152506784111463. [DOI] [PubMed] [Google Scholar]
- 154.Breyer RM, Kennedy CR, Zhang Y, et al. Structure-function analyses of eicosanoid receptors. Physiologic and therapeutic implications. Ann N Y Acad Sci. 2000;905:221–231. doi: 10.1111/j.1749-6632.2000.tb06552.x. [DOI] [PubMed] [Google Scholar]
- 155.Zhou W, Hashimoto K, Goleniewska K, et al. Prostaglandin I2 analogs inhibit proinflammatory cytokine production and T cell stimulatory function of dendritic cells. J Immunol. 2007;178(2):702–710. doi: 10.4049/jimmunol.178.2.702. [DOI] [PubMed] [Google Scholar]
- 156.Muller T, Durk T, Blumenthal B, et al. Iloprost has potent anti-inflammatory properties on human monocyte-derived dendritic cells. Clin Exp Allergy. 2010;40(8):1214–1221. doi: 10.1111/j.1365-2222.2010.03558.x. [DOI] [PubMed] [Google Scholar]
- 157.Narumiya S, Sugimoto Y, Ushikubi F. Prostanoid receptors: structures, properties, and functions. Physiol Rev. 1999;79(4):1193–1226. doi: 10.1152/physrev.1999.79.4.1193. [DOI] [PubMed] [Google Scholar]
- 158.Komhoff M, Lesener B, Nakao K, et al. Localization of the prostacyclin receptor in human kidney. Kidney Int. 1998;54(6):1899–1908. doi: 10.1046/j.1523-1755.1998.00213.x. [DOI] [PubMed] [Google Scholar]
- 159.Zhou W, Blackwell TS, Goleniewska K, et al. Prostaglandin I2 analogs inhibit Th1 and Th2 effector cytokine production by CD4 T cells. J Leukoc Biol. 2007;81(3):809–817. doi: 10.1189/jlb.0606375. [DOI] [PubMed] [Google Scholar]
- 160.Schulman ES, Newball HH, Demers LM, et al. Anaphylactic release of thromboxane A2, prostaglandin D2, and prostacyclin from human lung parenchyma. Am Rev Respir Dis. 1981;124(4):402–406. doi: 10.1164/arrd.1981.124.4.402. [DOI] [PubMed] [Google Scholar]
- 161.Schulman ES, Adkinson NF, Jr, Newball HH. Cyclooxygenase metabolites in human lung anaphylaxis: airway vs. parenchyma. J Appl Physiol. 1982;53(3):589–595. doi: 10.1152/jappl.1982.53.3.589. [DOI] [PubMed] [Google Scholar]
- 162.Shephard EG, Malan L, Macfarlane CM, et al. Lung function and plasma levels of thromboxane B2, 6-ketoprostaglandin F1 alpha and beta-thromboglobulin in antigen-induced asthma before and after indomethacin pretreatment. Br J Clin Pharmacol. 1985;19(4):459–470. doi: 10.1111/j.1365-2125.1985.tb02671.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Bianco S, Robuschi M, Grugni A, et al. Effect of prostacyclin on antigen induced immediate bronchoconstriction in asthmatic patients. Prostaglandins Med. 1979;3(1):39–45. doi: 10.1016/0161-4630(79)90014-4. [DOI] [PubMed] [Google Scholar]
- 164.Bianco S, Robuschi M, Ceserani R, et al. Effects of prostacyclin on aspecifically and specifically induced bronchoconstriction in asthmatic patients. Eur J Respir Dis Suppl. 1980;106:81–87. [PubMed] [Google Scholar]
- 165.Hardy C, Robinson C, Lewis RA, et al. Airway and cardiovascular responses to inhaled prostacyclin in normal and asthmatic subjects. American Review of Respiratory Disease. 1985;131(1):18–21. doi: 10.1164/arrd.1985.131.1.18. [DOI] [PubMed] [Google Scholar]
- 166.Nizankowska E, Czerniawska-Mysik G, Szczeklik A. Lack of effect of i.v. prostacyclin on aspirin-induced asthma. Eur J Respir Dis. 1986;69(5):363–368. [PubMed] [Google Scholar]
- 167.Hardy CC, Bradding P, Robinson C, et al. Bronchoconstrictor and antibronchoconstrictor properties of inhaled prostacyclin in asthma. J Appl Physiol. 1988;64(4):1567–1574. doi: 10.1152/jappl.1988.64.4.1567. [DOI] [PubMed] [Google Scholar]
- 168.Fujimura M, Ozawa S, Matsuda T. Effect of oral administration of a prostacyclin analog (OP-41483) on pulmonary function and bronchial responsiveness in stable asthmatic subjects. J Asthma. 1991;28(6):419–424. doi: 10.3109/02770909109110624. [DOI] [PubMed] [Google Scholar]
- 169.Majeski E, Hoskins A, Dworski R, et al. Iloprost inhalation in mild asthma. J Asthma. 2012;49(9):961–965. doi: 10.3109/02770903.2012.724130. [DOI] [PubMed] [Google Scholar]
- 170.Takahashi Y, Tokuoka S, Masuda T, et al. Augmentation of allergic inflammation in prostanoid IP receptor deficient mice. Br J Pharmacol. 2002;137(3):315–322. doi: 10.1038/sj.bjp.0704872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Nagao K, Tanaka H, Komai M, et al. Role of prostaglandin I2 in airway remodeling induced by repeated allergen challenge in mice. Am J Respir Cell Mol Biol. 2003 doi: 10.1165/rcmb.2003-0035OC. [DOI] [PubMed] [Google Scholar]
- 172.Lovgren AK, Jania LA, Hartney JM, et al. COX-2-derived prostacyclin protects against bleomycin-induced pulmonary fibrosis. Am J Physiol Lung Cell Mol Physiol. 2006;291(2):L144–L156. doi: 10.1152/ajplung.00492.2005. [DOI] [PubMed] [Google Scholar]
- 173.Zhou W, Dowell DR, Geraci MW, et al. PGI synthase overexpression protects against bleomycin-induced mortality and is associated with increased Nqo 1 expression. Am J Physiol Lung Cell Mol Physiol. 2011;301(4):L615–L622. doi: 10.1152/ajplung.00224.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Idzko M, Hammad H, van Nimwegen M, et al. Inhaled iloprost suppresses the cardinal features of asthma via inhibition of airway dendritic cell function. J Clin Invest. 2007;117(2):464–472. doi: 10.1172/JCI28949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Toki S, Goleniewska K, Huckabee MM, et al. PGI2 signaling inhibits antigen uptake and increases migration of immature dendritic cells. J Leukoc Biol. 2013 doi: 10.1189/jlb.1112559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Boswell MG, Zhou W, Newcomb DC, et al. PGI2 as a regulator of CD4+ subset differentiation and function. Prostaglandins Other Lipid Mediat. 2011;96(1–4):21–26. doi: 10.1016/j.prostaglandins.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Dorris SL, Peebles RS., Jr PGI(2) as a Regulator of Inflammatory Diseases. Mediators Inflamm. 2012;2012:926968. doi: 10.1155/2012/926968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Whittle BJ, Moncada S. Pharmacological interactions between prostacyclin and thromboxanes. Br Med Bull. 1983;39(3):232–238. doi: 10.1093/oxfordjournals.bmb.a071825. [DOI] [PubMed] [Google Scholar]
- 179.Miyata A, Yokoyama C, Ihara H, et al. Characterization of the human gene (TBXAS1) encoding thromboxane synthase. Eur J Biochem. 1994;224(2):273–279. doi: 10.1111/j.1432-1033.1994.00273.x. [DOI] [PubMed] [Google Scholar]
- 180.Ruan KH. Advance in understanding the biosynthesis of prostacyclin and thromboxane A2 in the endoplasmic reticulum membrane via the cyclooxygenase pathway. Mini Rev Med Chem. 2004;4(6):639–647. doi: 10.2174/1389557043403710. [DOI] [PubMed] [Google Scholar]
- 181.Roberts LJ, Sweetman BJ, Oates JA. Metabolism of thromboxane B2 in man. J Biol Chem. 1981;256(16):8384–8393. [PubMed] [Google Scholar]
- 182.Raychowdhury MK, Yukawa M, Collins LJ, et al. Alternative splicing produces a divergent cytoplasmic tail in the human endothelial thromboxane A2 receptor. J Biol Chem. 1994;269(30):19256–19261. [PubMed] [Google Scholar]
- 183.Huang JS, Ramamurthy SK, Lin X, et al. Cell signalling through thromboxane A2 receptors. Cell Signal. 2004;16(5):521–533. doi: 10.1016/j.cellsig.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 184.Hirata T, Ushikubi F, Kakizuka A, et al. Two thromboxane A2 receptor isoforms in human platelets. Opposite coupling to adenylyl cyclase with different sensitivity to Arg60 to Leu mutation. J Clin Invest. 1996;97(4):949–956. doi: 10.1172/JCI118518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Grosser T, Fries S, Fitzgerald GA. Biological basis for the cardiovascular consequences of COX-2 inhibition: therapeutic challenges and opportunities. J Clin Invest. 2006;116(1):4–15. doi: 10.1172/JCI27291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Roberts LJ, Sweetman BJ, Lewis RA, et al. Increased production of prostaglandin D2 in patients with systemic mastocytosis. N Engl J Med. 1980;303(24):1400–1404. doi: 10.1056/NEJM198012113032405. [DOI] [PubMed] [Google Scholar]
- 187.Taylor IK, Ward PS, O’Shaughnessy KM, et al. Thromboxane A2 biosynthesis in acute asthma and after antigen challenge. Am Rev Respir Dis. 1991;143(1):119–125. doi: 10.1164/ajrccm/143.1.119. [DOI] [PubMed] [Google Scholar]
- 188.Lupinetti MD, Sheller JR, Catella F, et al. Thromboxane biosynthesis in allergen-induced bronchospasm. Evidence for platelet activation. Am Rev Respir Dis. 1989;140(4):932–935. doi: 10.1164/ajrccm/140.4.932. [DOI] [PubMed] [Google Scholar]
- 189.Seltzer J, Bigby BG, Stulbarg M, et al. O3-induced change in bronchial reactivity to methacholine and airway inflammation in humans. J Appl Physiol. 1986;60(4):1321–1326. doi: 10.1152/jappl.1986.60.4.1321. [DOI] [PubMed] [Google Scholar]
- 190.O’Byrne PM, Leikauf GD, Aizawa H, et al. Leukotriene B4 induces airway hyperresponsiveness in dogs. J Appl Physiol. 1985;59(6):1941–1946. doi: 10.1152/jappl.1985.59.6.1941. [DOI] [PubMed] [Google Scholar]
- 191.Aizawa H, Inoue H, Nakano H, et al. Effects of thromboxane A2 antagonist on airway hyperresponsiveness, exhaled nitric oxide, and induced sputum eosinophils in asthmatics. Prostaglandins Leukot. Essent Fatty Acids. 1998;59(3):185–190. doi: 10.1016/s0952-3278(98)90061-8. [DOI] [PubMed] [Google Scholar]
- 192.Hoshino M, Sim J, Shimizu K, et al. Effect of AA-2414, a thromboxane A2 receptor antagonist, on airway inflammation in subjects with asthma. J Allergy Clin Immunol. 1999;103(6):1054–1061. doi: 10.1016/s0091-6749(99)70179-x. [DOI] [PubMed] [Google Scholar]
- 193.Shi H, Yokoyama A, Kohno N, et al. Effect of thromboxane A2 inhibitors on allergic pulmonary inflammation in mice. European Respiratory Journal. 1998;11(3):624–629. [PubMed] [Google Scholar]
- 194.Liu T, Laidlaw TM, Feng C, et al. Prostaglandin E2 deficiency uncovers a dominant role for thromboxane A2 in house dust mite-induced allergic pulmonary inflammation. Proc Natl Acad Sci U S A. 2012;109(31):12692–12697. doi: 10.1073/pnas.1207816109. [DOI] [PMC free article] [PubMed] [Google Scholar]