Abstract
Objective
We aimed to study whether prenatal vitamin (PNV) use protects against low 25(OH)D levels in all women and particularly in obese and black women who are both at risk of vitamin D deficiency and poor pregnancy outcomes.
Study design
We studied 1019 women enrolled in a prospective study at Brigham and Women’s Hospital in Boston, 2007–2009. We used multivariable logistic regression to analyze associations of PNV use and odds of vitamin D deficiency defined as 25(OH)D levels < 50 nmol/L.
Results
56% of black and 86% of white women reported pre- and/or post-conceptional PNV use. 75% of black and 19% of white women were vitamin D deficient in the first trimester. PNV use among black women was not associated with vitamin D deficiency (adjusted OR 1.0, 95%CI 0.4, 2.3) but was among white women (3.5, 95%CI 2.1, 5.8)(Interaction P<0.01).
Conclusions
Ongoing trials of vitamin D supplementation during pregnancy should consider potential effect modification by race/ethnicity.
Keywords: vitamin D, 25-hydroxyvitamin D, pregnancy, vitamin D deficiency, race, African American, black, obesity, overweight, multivitamin, prenatal vitamins
Introduction
Perinatal health outcomes vary dramatically by race in the United States.1 African American women develop preeclampsia more often than their white counterparts2 and are more likely to develop preterm labor.3 The result is that black infants are 60% more likely be preterm and four times more likely to die due to prematurity than white infants.1 Because of less efficient vitamin D synthesis in the skin of darker pigmented individuals, African Americans are at higher risk than white Americans of vitamin D deficiency.4, 5 Black women are also more likely than white women to be overweight or obese6 which is of concern because obesity is another risk factor for vitamin D deficiency5, 7 and poor perinatal outcomes.8 In observational studies, 25-hydroxyvitamin D (25[OH]D) levels have been shown to be associated with higher risk of several adverse perinatal outcomes including gestational diabetes9, 10, preeclampsia,11 preterm birth12 and small-for-gestational age status.13, 14, 15, 16, 17 Because of the paucity of vitamin D trial data with respect to perinatal outcomes, whether differences in vitamin D status during pregnancy explains or partially explains perinatal disparities is plausible18 but remains unknown. Furthermore, while multivitamin intake has been shown to vary by race,19 it remains unknown whether multivitamin intake improves vitamin D status among the highest risk groups (African Americans and overweight/obese) during pregnancy. The object of this study was to examine whether women who reported taking a prenatal vitamin had lower risk of low 25(OH)D levels. Our hypothesis was that lack of prenatal vitamin (PNV) use would be associated with vitamin D deficiency (defined as <50 nmol/).
Methods
Study Design and Participants
Between 2007 and 2009, 2246 pregnant women enrolled in a three site, observational cohort study of the prevention of preeclampsia in Boston and Philadelphia.20 Women provided written, informed consent to participate and the Institutional Review Board of participating institutions approved the study. This substudy includes women enrolled from Brigham and Women’s Hospital, a high-risk tertiary perinatal center in Boston, MA who had complete exposure (PNV use) and outcome data (vitamin D status at two time points during pregnancy). Details of study participation are shown in Figure 1. Women enrolled at a median (interquartile range) gestational age of 9.6 weeks (8.4–11.4). We collected baseline demographics using a questionnaire including race/ethnicity and education obtained data from the medical record. Body mass index (BMI) was calculated from measurements obtained during the first trimester visit (kg/m2). PNV use was ascertained by questionnaire that asked women, “Prior to pregnancy, did you take a multivitamin?” and “Since getting pregnant have you taken a multivitamin?” We categorized women as PNV users if they reported any PNV use. We performed secondary analyses restricting to women who initiated PNV use before pregnancy only and after pregnancy only and compared each group to women with no reported PNV use.
Figure 1.
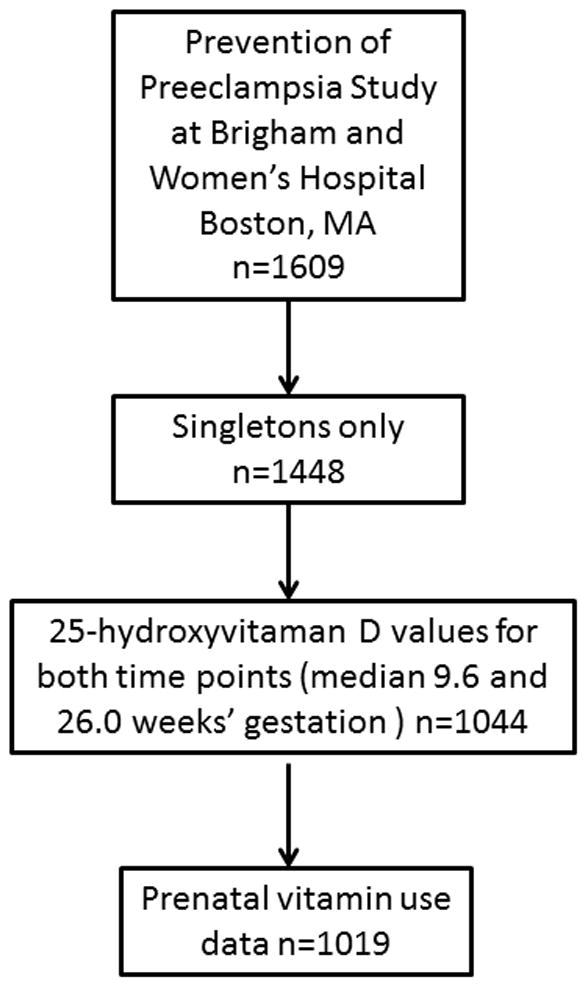
Participant selection.
Laboratory analysis
Maternal blood was obtained at the initial visit (median gestational age 9.6 weeks, IQR 8.4–11.4) and again in the late second/early third trimester (mean 26.0 weeks’ gestation, IQR 25.0–26.9). Approximately 10 mL of blood was drawn in ethylene diamine tetraacetic acid plasma tubes at each study visit; the samples were kept at 4°C until processing for storage within 4 hours of venipuncture. The specimens were centrifuged for 20 minutes and stored at −80°C. The plasma samples were analyzed for 25-hydroxyvitamin D concentration (25(OH)D) using chemiluminescence, an automated radioimmunoassay21 in the Weiss laboratory at the Channing Laboratory, Boston, MA. We defined vitamin D deficiency as <50 nmol/L, a common cut-point in the literature.5, 22, 23
Statistical analyses
First, we analyzed bivariate associations between 25(OH)D category and PNV use as well as covariates including maternal age, race/ethnicity, smoking, education and BMI. We then performed multivariable logistic regression models to estimate adjusted associations of PNV use and vitamin D deficiency. We subsequently stratified by race/ethnicity and obesity status to examine whether PNV was associated with vitamin D deficiency in high risk groups. Women with missing covariates were not included in final multivariable models. All statistical analyses were run using SAS version 9.3, Cary, NC.
Results
Most women reported multivitamin 763/1019 (74.9%) use before and/or early in pregnancy. Of PNV users, 477 (62.5%) reported use before and after pregnancy diagnosis, 238 (31.2%) reported use only after pregnancy was diagnosed, and just 48 (6.3%) of women reported using PNVs prior to pregnancy but discontinuing PNV use after diagnosis of pregnancy. Older, white, lean and better educated women were more likely to report PNV use (Table 1). At the earlier time point, 34.5 % of women had vitamin D levels < 50 nmol/L; at the later time point, 29.1% did. In unadjusted bivariate analyses, black women, overweight/obese women, less educated women, and younger women were more likely to have low 25(OH)D levels (Table 2).
Table 1.
Multivitamin use and characteristics among pregnant women, Brigham and Women’s Hospital, n=1017.
| Prenatal Vitamin Use | Chi Square P value | ||||
|---|---|---|---|---|---|
| Yes (n=763, 74.9%) | No (n=256, 25.1%) | ||||
| n | Column % | n | Column % | ||
| Characteristics (column %)a | |||||
| Maternal Age | |||||
| < 25 (12%) | 45 | 5.9% | 79 | 30.9% | <0.0001 |
| 25 – <30 (58%) | 473 | 62.0% | 122 | 47.7% | |
| >= 30 (29%) | 245 | 32.1% | 55 | 21.5% | |
| Race/Ethnicity | |||||
| Black (13%) | 63 | 8.3% | 71 | 27.7% | <0.0001 |
| Hispanic (14%) | 66 | 8.7% | 72 | 28.1% | |
| White (62%) | 541 | 70.9% | 89 | 34.8% | |
| Other (12%) | 93 | 12.2% | 24 | 9.4% | |
| Prepregnancy BMI Categoryb | <0.0001 | ||||
| Normal weight (< 25kg/m2) (55%) | 451 | 59.3% | 110 | 43.0% | |
| Overweight 25–<30(kg/m2) (25%) | 185 | 24.3% | 70 | 27.3% | |
| Obese >= 30 (kg/m2) (20%) | 124 | 16.3% | 76 | 29.7% | |
| History of smoking | 0.63 | ||||
| Yes (26%) | 194 | 25.4% | 69 | 27.0% | |
| No (74%) | 569 | 74.5% | 187 | 73.0% | |
| Maternal Education | <0.0001 | ||||
| Higher education >12 years (86%) | 709 | 92.9% | 163 | 63.7% | |
| <= 12 years (14%) | 54 | 7.1% | 93 | 36.3% | |
| Vitamin D Category (nmol/L) | |||||
| Time 1 (median 9.6 weeks) | <0.0001 | ||||
| < 50 nmol/L (34%) | 203 | 26.6% | 148 | 57.8% | |
| 50 – < 75 (42%) | 361 | 47.3% | 65 | 25.4% | |
| > = 75 (24%) | 199 | 26.1% | 43 | 16.8% | |
| Vitamin D Category (nmol/L) | |||||
| Time 2 (median 26.0 weeks) | <0.0001 | ||||
| < 50 nmol/L (29%) | 194 | 25.4% | 103 | 40.2% | |
| 50 – < 75 (39%) | 303 | 39.7% | 96 | 37.5% | |
| > = 75 (32%) | 266 | 34.9% | 57 | 22.3% | |
Percentages may not add up to 100% due to rounding.
BMI Missing n=3.
Table 2.
Associations of Maternal Characteristics and Vitamin D concentration <50 nmol/L among pregnant women, Brigham and Women’s Hospital, n=1019.
| All Participants | Time 1 (Median 9.6 weeks’) | Time 2 (Median 26.0 weeks’) | ||
|---|---|---|---|---|
| Row % <50 nmol/L | Row % <50 nmol/L | |||
| 34.4 % | 29.1% | |||
| Characteristics | Chi Square P value | Chi Square P value | ||
| Maternal Age | < 0.0001 | < 0.0001 | ||
| < 25 | 61.3% | 47.6% | ||
| 25 – <30 | 33.8% | 29.4% | ||
| >= 30 | 24.7% | 21.0% | ||
| Race/Ethnicity | <0.0001 | < 0.0001 | ||
| Black | 74.6% | 58.2% | ||
| Hispanic | 52.2% | 39.9% | ||
| White | 18.9% | 17.8% | ||
| Other | 51.3% | 44.4% | ||
| Prepregnancy BMI Category | <0.0001 | < 0.0001 | ||
| Normal weight (< 25kg/m2) | 25.7% | 23.2% | ||
| Overweight 25–<30(kg/m2) | 37.3% | 30.6% | ||
| Obese >= 30 (kg/m2) | 55.5% | 44.0% | ||
| Smoking status | 0.11 | 0.79 | ||
| Yes | 30.4% | 28.5% | ||
| No | 35.8% | 29.4% | ||
| Maternal Education | <0.0001 | <0.0001 | ||
| Higher education >12 years | 29.7% | 26.1% | ||
| <= 12 years | 62.6% | 46.9% | ||
| Season (at time of first blood sample) | < 0.0001 | <0.0001 | ||
| Winter | 40.8% | 40.6% | ||
| Spring | 40.8% | 32.7% | ||
| Summer | 22.2% | 15.2% | ||
| Fall | 30.6% | 29.4% | ||
| Prenatal Vitamin Use | <0.0001 | <0.0001 | ||
| Yes | 26.6% | 25.4% | ||
| No | 57.8% | 40.2% | ||
Abbreviations: BMI, body mass index
Women who reported no PNV use (versus any reported PNV use)had significantly higher odds of 25(OH)D levels <50 nmol/L at the time of the first sample(OR 3.9, 95 % CI 2.9, 5.2) and second sample(OR 2.1, 95% CI 1.6, 2.9) (Table 3) in models adjusting for season. Further adjustment for maternal age, education, smoking status, BMI and race/ethnicity race/ethnicity attenuated these estimates but women reporting no PNV use still had significantly higher odds of 25(OH)D levels<50 (OR 2.1, 95% CI 1.5, 3.0). However, lack of reported PNV use was not associated with increased odds of low 25(OH)D levels later in pregnancy (OR 1.1, 95% CI 0.7, 1.6). In other words, early PNV use was associated with vitamin D sufficiency earlier in pregnancy but not later in pregnancy (Table 4). Because we were concerned that ever-users included a heterogeneous category of PNV users including women who only used before pregnancy or only after pregnancy diagnosis, we compared this estimate to an analogous model comparing women who used both before and after pregnancy diagnosis (always users, n=477) to never users (n=256). In fully adjusted models, women with no PNV use (vs. use before and after pregnancy diagnosis) had higher odds of 25(OH)D levels <50 nmol/L (adjusted OR 2.8, 95% CI: 1.9, 4.3) earlier in pregnancy, and no difference later in pregnancy (adjusted OR 1.3, 95% CI: 0.8, 2.0).
Table 3.
Odds of 25-hydroxyvitamin D levels <50 nmol/L among Women Reporting No (vs. any) Prenatal Vitamin Use
| Time 1 (Median 9.6 weeks’ gestation) | Time 2 (Median 26.0 weeks’ gestation) | |||
|---|---|---|---|---|
| All Participants: (n=1017, 75% PNV use) | OR | (95% CI) | OR | (95% CI) |
| Model 1: Seasonally-adjusted | 3.9 | (2.9, 5.2) | 2.1 | (1.6, 2.9) |
| Model 2: Model 1 + maternal age, education and smoking | 2.8 | (2.0, 3.8) | 1.5 | (1.1, 2.1) |
| Model 3: Model 2+ BMI | 2.5 | (1.8, 3.5) | 1.3 | (0.9, 1.9) |
| Model 4: Model 3 + maternal race/ethnicity | 2.1 | (1.5, 3.0) | 1.1 | (0.7, 0.9) |
| Overweight/Obese Participants (BMI >= 25kg/m2)(n=461, 67% PNV use) | ||||
| Model 1: Seasonally-adjusted | 4.1 | (2.7, 6.3) | 2.5 | (1.6, 3.7) |
| Model 2: Model 1 + Race | 2.8 | (1.7, 4.4) | 1.6 | (0.99, 2.6) |
| Lean (BMI <25 kg/m2)(n=561, 80% PNV use) | ||||
| Model 1: Seasonally-adjusted | 3.0 | (1.9, 4.8) | 1.4 | (0.9, 2.3) |
| Model 2: Model 1 + Race | 1.8 | (1.0, 3.0 | 0.8 | (0.5, 1.4) |
| Black Participants (n=137, 56 % PNV use) | ||||
| Model 1: Seasonally-adjusted | 1.0 | (0.4, 2.4) | 1.0 | (0.5, 2.1) |
| Model 2: Model 1 + BMI | 1.0 | (0.4, 2.3) | 1.0 | (0.5, 2.2) |
| White Participants (n= 630, 86% PNV use) | ||||
| Model 1: Seasonally-adjusted | 3.5 | (2.1, 5.8) | 1.4 | (0.8, 2.5) |
| Model 2: Model 1 + BMI | 3.3 | (2.0, 5.5) | 1.3 | (0.7, 2.4) |
Abbreviations: BMI, body mass index; PNV, prenatal vitamins.
Table 4.
Vitamin D status at 2 time points in pregnancy and percent prenatal vitamin use.
| Sufficient Time 1 | Deficient at Time 1 | |
|---|---|---|
| Sufficient at Time 2 | n= 581 (84% PNV use) | n = 141 (57% PNV use) |
| Deficient at Time 2 | n = 87 (83% PNV use) | n = 200 (61% PNV use) |
Sufficiency defined as 25(OH)D level ≥ 50 nmol/L, deficiency defined as <50 nmol/L.
Time 1: median 9.6 weeks’, IQR 8.4 – 11.4; Time: median 26.0 weeks’, IQR 25.0 – 26.9; 25(OH)D, 25-hydroxyvitamin D.
When then we stratified by overweight/obesity status, we found that among women with BMI >25 kg/m2 lack of PNV use was associated with higher odds of 25(OH)D levels <50 nmol/L during the first trimester(seasonally-adjusted OR 4.1, 95% CI 2.7, 6.3)and later in pregnancy (OR 2.5, 95% CI: 1.6, 3.7). Further adjustment for race did not substantially change these estimates (Table 3). Among women with BMI < 25 kg/m2, lack of PNV use was associated with higher odds of 25(OH)D levels <50 nmol/L during the first trimester (seasonally adjusted OR 3.0, 95% CI: 1.9, 4.8), but not at the later time point (OR 1.4, 95% CI 0.9, 2.3). Further adjustment for race in lean women attenuated the odds ratio in the first trimester (OR 1.8, 95% CI 1.0, 3.0).
When we stratified by race/ethnicity status, we found that for black women, lack of PNV use was not associated with significantly higher seasonally-adjusted odds of 25(OH)D levels <50 nmol/L early in pregnancy (OR 1.0 (0.4, 2.3) (Table 3). In contrast for white women, lack of PNV use was associated with significantly higher seasonally-adjusted odds of 25(OH)D levels <50 nmol/L early (OR 3.5, 95% CI 2.1, 5.8) (Interaction P value 0.01). Further adjustment for BMI did not change this estimate. The interaction of race with the association between PNV use and low 25(OH)D levels was not significant later in pregnancy (interaction P value= 0.3).
Discussion
Our data suggest that while prenatal PNV use is associated with lower odds of vitamin D deficiency, the association is not uniform. Both overweight/obesity as well as darker skin pigmentation are both well-established risk factors for vitamin D deficiency. While lack of PNV use among overweight/obese pregnant women was associated with higher odds of low 25(OH)D levels, this was not the case for black women, who were less likely to take PNV’s compared to white women.
Our data are consistent with other similar cohort data. In another study of Massachusetts women, black women reported taking periconceptional multivitamins half as often as white women.19 Additionally, our prevalence of vitamin D deficiency is similar to that reported in NHANES24 and in another Boston cohort, Project Viva.13, 25 Others have analyzed the association between PNV use and vitamin D status. Shea et al studied 2500 elderly adults and found that lack of PNV use was associated with higher odds of vitamin D insufficiency (<75 nmol/L) in both black (5.2 (95% CI: 3.5, 7.7)) and white participants (OR 2.6, 95% CI: 2.0, 3.2), however these subjects were much older and not pregnant.26 A small Turkish study of 79 pregnant women showed significantly higher 25(OH)D levels among women reporting PNV use in the third trimester,27 but this study did not include women of African descent and did not have the power to address potential interaction by BMI. Similarly Holmes et al reported higher 25(OH)D levels among pregnant women taking PNV in a longitudinal study, but only included Caucasian women.23
Our study has several strengths including 25(OH)D concentrations at two separate time points, self-reported race/ethnicity, and measured height and weight during the first trimester and weight at subsequent visits. Our study has limitations associated with self-report of PNV use which could differ from actual use. Additionally we lacked data on sun exposure, actual skin pigmentation or food intake which contribute to 25(OH)D concentration. However, our data remain relevant because PNV use is likely to be more modifiable than latitude of residence, skin pigmentation, sun exposure which should be limited due to skin cancer risk, or even dietary patterns which can be difficult to change. Our study is also limited by lack of detailed data about PNV use. We had no information as to the duration of use or the vitamin D dose in the PNV which typically is 400–600 IU per tablet, but can vary. We did not have data on whether women were taking separate calcium or vitamin D supplements beyond what is contained in PNVs. We also had no information on frequency of use which could have varied from daily to sparse use. Our findings could be affected by unmeasured or inadequately measured confounding variables such as socioeconomic status which could vary by weight and race and could possibly affect self-report of PNV use. We also lacked data on vitamin D binding protein which may differ by race/ethnicity and could affect the association between PNV use and 25(OH)D measured in the plasma. The optimal method of vitamin D measurement remains controversial, but our laboratory uses U.S. National Institute of Standards and Technology level 1 and this method is commonly used clinically and in the literature. Lastly, we are not suggesting the futility of PNV use in black women. In contrast, our data support investigation into higher doses of vitamin D in subgroups at high risk if benefits are demonstrated by ongoing trials in pregnancy of achieving higher 25(OH)D levels. Future analyses of health effects of vitamin D status in this population are planned but beyond the scope of this analysis.
In conclusion, we found that lack of PNV use during pregnancy was associated with vitamin D deficiency early in pregnancy, but not among black women. In light of two recent meta-analyses/systematic reviews concluding that low 25(OH)D levels during pregnancy are associated with several morbidities in pregnancy 15, 16, optimizing vitamin D status during pregnancy may be important. Ongoing trials of vitamin D supplementation during pregnancy should consider effect modification by race/ethnicity.
Acknowledgments
Dr. Burris received support from NIH/NIEHS K23ES022242 and Klarman Scholars Program at Beth Israel Deaconess Medical Center. Dr. McElrath received funds from an unrestricted grant from Abbott Diagnostics. This work was also supported though the generosity of the Zugg family.
Abbreviations
- 25(OH)D
25-hydroxyvitamin D
- BMI
body mass index (kg/m2)
- PNV
prenatal vitamins
Footnotes
Conflict of interest
The authors declare no conflict of interest.
References
- 1.MacDorman MF. Race and ethnic disparities in fetal mortality, preterm birth, and infant mortality in the United States: an overview. Seminars in perinatology. 2011;35(4):200–208. doi: 10.1053/j.semperi.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 2.Eskenazi B, Fenster L, Sidney S. A multivariate analysis of risk factors for preeclampsia. JAMA. 1991;266(2):237–241. [PubMed] [Google Scholar]
- 3.Timofeev J, Feghali M, Boyle A, Istwan N, Rhea D, Driggers RW. Rates of recurrent preterm birth by maternal body habitus in women receiving 17 alpha-hydroxyprogesterone caproate. J Matern Fetal Neonatal Med. 2013;26(9):881–884. doi: 10.3109/14767058.2013.765847. [DOI] [PubMed] [Google Scholar]
- 4.Holick MF. Photosynthesis of vitamin D in the skin: effect of environmental and life-style variables. Fed Proc. 1987;46(5):1876–1882. [PubMed] [Google Scholar]
- 5.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 6.Kim SY, Saraiva C, Curtis M, Wilson HG, Troyan J, England L, et al. Fraction of Gestational Diabetes Mellitus Attributable to Overweight and Obesity by Race/Ethnicity, California, 2007–2009. American journal of public health. 2013 doi: 10.2105/AJPH.2013.301469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bodnar LM, Catov JM, Roberts JM, Simhan HN. Prepregnancy obesity predicts poor vitamin D status in mothers and their neonates. J Nutr. 2007;137(11):2437–2442. doi: 10.1093/jn/137.11.2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Honein MA, Devine O, Sharma AJ, Rasmussen SA, Park S, Kucik JE, et al. Modeling the potential public health impact of prepregnancy obesity on adverse fetal and infant outcomes. Obesity. 2013;21(6):1276–1283. doi: 10.1002/oby.20156. [DOI] [PubMed] [Google Scholar]
- 9.Burris HH, Rifas-Shiman SL, Kleinman K, Litonjua AA, Huh SY, Rich-Edwards JW, et al. Vitamin D deficiency in pregnancy and gestational diabetes mellitus. Am J Obstet Gynecol. 2012 doi: 10.1016/j.ajog.2012.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang C, Qiu C, Hu FB, David RM, van Dam RM, Bralley A, et al. Maternal plasma 25-hydroxyvitamin D concentrations and the risk for gestational diabetes mellitus. PLoS One. 2008;3(11):e3753. doi: 10.1371/journal.pone.0003753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bodnar LM, Catov JM, Simhan HN, Holick MF, Powers RW, Roberts JM. Maternal vitamin D deficiency increases the risk of preeclampsia. J Clin Endocrinol Metab. 2007;92(9):3517–3522. doi: 10.1210/jc.2007-0718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bodnar LM, Klebanoff MA, Gernand AD, Platt RW, Parks WT, Catov JM, et al. Maternal Vitamin D Status and Spontaneous Preterm Birth by Placental Histology in the US Collaborative Perinatal Project. Am J Epidemiol. 2014;179(2):168–176. doi: 10.1093/aje/kwt237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burris HH, Rifas-Shiman SL, Camargo CA, Jr, Litonjua AA, Huh SY, Rich-Edwards JW, et al. Plasma 25-hydroxyvitamin D during pregnancy and small-for-gestational age in black and white infants. Ann Epidemiol. 2012;22(8):581–586. doi: 10.1016/j.annepidem.2012.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bodnar LM, Catov JM, Zmuda JM, Cooper ME, Parrott MS, Roberts JM, et al. Maternal Serum 25-Hydroxyvitamin D Concentrations Are Associated with Small-for-Gestational Age Births in White Women. J Nutr. 2010 doi: 10.3945/jn.109.119636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wei SQ, Qi HP, Luo ZC, Fraser WD. Maternal vitamin D status and adverse pregnancy outcomes: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2013 doi: 10.3109/14767058.2013.765849. [DOI] [PubMed] [Google Scholar]
- 16.Aghajafari F, Nagulesapillai T, Ronksley PE, Tough SC, O’Beirne M, Rabi DM. Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: systematic review and meta-analysis of observational studies. BMJ. 2013;346:f1169. doi: 10.1136/bmj.f1169. [DOI] [PubMed] [Google Scholar]
- 17.Gernand AD, Simhan HN, Caritis S, Bodnar LM. Maternal Vitamin D Status and Small-for-Gestational-Age Offspring in Women at High Risk for Preeclampsia. Obstetrics & Gynecology. 2014;123(1):40–48. doi: 10.1097/AOG.0000000000000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bodnar LM, Simhan HN. Vitamin D may be a link to black-white disparities in adverse birth outcomes. Obstet Gynecol Surv. 2010;65(4):273–284. doi: 10.1097/OGX.0b013e3181dbc55b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burris HH, Mitchell AA, Werler MM. Periconceptional multivitamin use and infant birth weight disparities. Ann Epidemiol. 2010;20(3):233–240. doi: 10.1016/j.annepidem.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 20.McElrath TF, Lim KH, Pare E, Rich-Edwards J, Pucci D, Troisi R, et al. Longitudinal evaluation of predictive value for preeclampsia of circulating angiogenic factors through pregnancy. American journal of obstetrics and gynecology. 2012;207(5):407e401–407. doi: 10.1016/j.ajog.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 21.Ersfeld DL, Rao DS, Body JJ, Sackrison JL, Jr, Miller AB, Parikh N, et al. Analytical and clinical validation of the 25 OH vitamin D assay for the LIAISON automated analyzer. Clin Biochem. 2004;37(10):867–874. doi: 10.1016/j.clinbiochem.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 22.Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84(1):18–28. doi: 10.1093/ajcn/84.1.18. [DOI] [PubMed] [Google Scholar]
- 23.Holmes VA, Barnes MS, Alexander HD, McFaul P, Wallace JM. Vitamin D deficiency and insufficiency in pregnant women: a longitudinal study. Br J Nutr. 2009;102(6):876–881. doi: 10.1017/S0007114509297236. [DOI] [PubMed] [Google Scholar]
- 24.Ginde AA, Sullivan AF, Mansbach JM, Camargo CA., Jr Vitamin D insufficiency in pregnant and nonpregnant women of childbearing age in the United States. Am J Obstet Gynecol. 2010;202(5):436e431–438. doi: 10.1016/j.ajog.2009.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burris HH, Rifas-Shiman SL, Kleinman K, Litonjua AA, Huh SY, Rich-Edwards JW, et al. Vitamin D deficiency in pregnancy and gestational diabetes mellitus. Am J Obstet Gynecol. 2012;207(3):182e181–188. doi: 10.1016/j.ajog.2012.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shea MK, Houston DK, Tooze JA, Davis CC, Johnson MA, Hausman DB, et al. Correlates and prevalence of insufficient 25-hydroxyvitamin D status in black and white older adults: the health, aging and body composition study. Journal of the American Geriatrics Society. 2011;59(7):1165–1174. doi: 10.1111/j.1532-5415.2011.03476.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ustuner I, Keskin HL, Tas EE, Neselioglu S, Sengul O, Avsar AF. Maternal serum 25(OH)D levels in the third trimester of pregnancy during the winter season. J Matern Fetal Neonatal Med. 2011;24(12):1421–1426. doi: 10.3109/14767058.2011.566768. [DOI] [PubMed] [Google Scholar]


