Abstract
Objective
Depression affects about 16% of the U.S. population over a lifetime. People with chronic diseases have especially high rates of co-morbid depression; 32% to 48% of people with epilepsy experience depression. This study evaluated the efficacy of a mindfulness-based cognitive therapy (MBCT) intervention for preventing major depressive disorder (MDD) episodes in people with epilepsy.
Method
Participants (n = 128) were adults from Georgia, Michigan, Texas, and Washington with epilepsy and mild/moderate depressive symptoms. The eight-session, weekly Project UPLIFT intervention, based on MBCT, was group-delivered via Web or telephone. Using a randomized, controlled, cross-over design, participants were assigned to Project UPLIFT or a treatment-as-usual (TAU) waitlist and assessed at baseline, and after intervening in the intervention group (~10 weeks) and in the TAU group (~20 weeks). Assessments included valid self-report measures of depression and MDD, knowledge/skills, and satisfaction with life.
Results
The incidence of MDD episodes (new or relapse) from baseline to interim assessment was significantly lower in the intervention condition (0.0%) than in TAU (10.7%). Depressive symptoms decreased significantly more in the intervention condition than in TAU; Web- and telephone did not differ. Change in knowledge/skills mediated the effect, which persisted over the 10 weeks of follow-up. Knowledge/skills and life satisfaction increased significantly more in the intervention condition than in TAU.
Conclusions
Distance delivery of group MBCT can prevent episodes of MDD, reduce symptoms of depression, and increase life satisfaction in people with epilepsy. This intervention is easily modified for persons with other chronic diseases and other disparity populations.
Keywords: major depressive disorder, mindfulness-based cognitive therapy, internet, telephone, epilepsy
Introduction
Depression ranks first for disease burden among all diseases in the U. S., and fourth worldwide (Ustun, Ayuso-Mateos, Chatterji, Mathers, & Murray, 2004). In the U. S., it affects about one in six people (16.2%) over the lifetime (Kessler et al., 2003). People with chronic diseases have a particularly high risk of depression due to their health and life circumstances (Carroll, Cassidy, & Cote, 2003; Evans et al., 2005), and public health agencies strongly support efforts to improve outcomes in adults with multiple chronic conditions (IOM [Institute of Medicine], 2012; Prevention, 2011; U. S. Department of Health and Human Services, 2013). Epilepsy, a neurological disorder characterized by recurrent seizures, exemplifies the risk of co-morbid depression (American Epilepsy Society [AES] & Centers for Disease Control and Prevention [CDC], 2003). Occurring at a rate between 32% and 48% among people with epilepsy (Jones et al., 2003), depression is their most frequent co-morbid psychiatric disorder (Hermann, Seidenberg, & Bell, 2000; Kanner, 2003; Kanner & Balabanov, 2002). Although those with epilepsy and depression report increased levels of perceived seizure severity (Cramer, Blum, Reed, & Fanning, 2003), their depression is often under-treated and even unrecognized, possibly due to concern about additional medications, and lack of access to mental health providers (AES & CDC, 2003).
In response to these concerns, and funded by the CDC, Project UPLIFT was developed as a cognitively-based, distance-delivered program for depression management (Thompson et al., 2010). First used as a home-based depression treatment for people with epilepsy, UPLIFT was recently noted in the IOM report on epilepsy (IOM, 2012). The UPLIFT acronym stands for Using Practice and Learning to Increase Favorable Thoughts, a reference to both Mindfulness (Using Practice) and Cognitive-Behavioral Therapy (Learning to Increase Favorable Thoughts), the bases of the intervention (Segal, Williams, & Teasdale, 2002). The UPLIFT materials were designed for group delivery by either telephone or Web. Offering this intervention in a group setting is not only cost-effective, it also provides modeling and social support among members of the group. Groups are particularly helpful for those who are isolated, but for persons with epilepsy or other disorders, there can be numerous barriers to attending group therapeutic sessions. These include transportation problems or physical barriers to access. When an individual is even mildly depressed, lack of motivation can exacerbate these barriers.
Project UPLIFT was demonstrated effective for individuals with depressive symptoms in a randomized, controlled, cross-over trial (Thompson et al., 2010). A total of 53 participants were recruited for the trial; 26 (13 Web, 13 phone) were randomized into the intervention condition and 27 (13 Web, 14 phone) into treatment-as-usual. Forty-four (83%) participants completed the baseline measures and started the program, 40 of whom completed all measures for inclusion in the analyses. Among those in the analyses, 19 were in the intervention condition (9 Web, 10 phone) and 21 were in treatment-as-usual (10 Web, 11 phone). All participants were from Georgia and scored in the high-mild to severe range of depression (Devins & Orme, 1985). Depressive symptoms and other measures were assessed at baseline, at about 8 weeks (after intervening in the intervention group), and again at about 16 weeks (after intervening in the treatment-as-usual [TAU] waitlist group). At 8 weeks, knowledge and skills had increased and depressive symptoms had decreased significantly more in the intervention group than in the TAU group; the Web and telephone groups did not differ. These findings raised the question of whether delivery of Project UPLIFT could prevent depressive episodes before they occurred in people with epilepsy. We also wanted to determine whether the intervention could be effective in a geographically diverse study sample, since prior research has suggested that depression-related outcomes may occur less frequently in the southeast, the only region in which it was previously tested (Jia et al., 2008; Polednak, 2012).
According to the Commission on Chronic Illness (1957), primary prevention efforts are designed to decrease the number of new cases of an adverse health outcome, while secondary prevention efforts are designed to lower the rate of existing cases of a disorder. Preventing the onset of depressive episodes encompasses both primary prevention and secondary prevention; it reduces new cases, and lowers the prevalence of existing cases. The two objectives of this study were to: (1) assess the effectiveness of Project UPLIFT for reducing depressive symptoms and preventing the incidence of depressive episodes in adults with epilepsy; and (2) expand the use of Project UPLIFT to three additional states.
Materials and Methods
Intervention
Content
The original 8-module Project UPLIFT intervention (Thompson et al., 2010; Walker, Obolensky, Dini, & Thompson, 2010), with language modified for use in prevention, provided the intervention content. Project UPLIFT is a manualized intervention that includes a script for use by the telephone facilitators in leading activities and discussions; use of a script is possible because the delivery is not face-to-face. The same script is used on the Web pages of the Internet version.
Activities and discussions are designed to increase knowledge about depression; monitoring, challenging, and changing of thoughts; coping and relaxing; attention and mindfulness; focusing on pleasure; the importance of reinforcement; and preventing relapse. Sessions are designed to last one hour by telephone, and are comprised of a check-in period, teaching on the topic of that week’s session, group discussion, a skill-building exercise, and a homework assignment.
Facilitators
The telephone- and Web-based groups were facilitated from Georgia, each co-facilitated by a graduate student with a Mental Health concentration in Public Health, and a selected adult with epilepsy. The same facilitators led all eight sessions of a particular group. Facilitators received 4 hours of training in delivery of the program, including delivery of a practice session, from the Principal Investigator, a Georgia-licensed clinical psychologist and Associate Professor of Behavioral Sciences, Psychiatry, and Epidemiology. She also supervised the facilitators on an ongoing basis.
Fidelity
All telephone sessions were audio-recorded; Web discussions were available to the Project staff. The clinical psychologist reviewed the audio-recordings, as well as the discussion boards on the Web, to ensure fidelity to the intervention script and to ensure that responses to questions or additional examples provided were consistent with the intention of the program. All Web and telephone sessions were also independently reviewed and transcribed by Project staff.
Treatment-as-usual
Participants in the treatment-as-usual waitlist condition followed the usual protocol that was in place for people with depressive symptoms at their epilepsy clinic. This meant that some of the participants were on antidepressant medication and some were in psychotherapy. The one exception was that these participants were contacted weekly by the Project UPLIFT staff, unless they requested that we discontinue this practice. The regular contact was performed to maintain ongoing contact with all the participants and control for interaction with the project staff.
Design
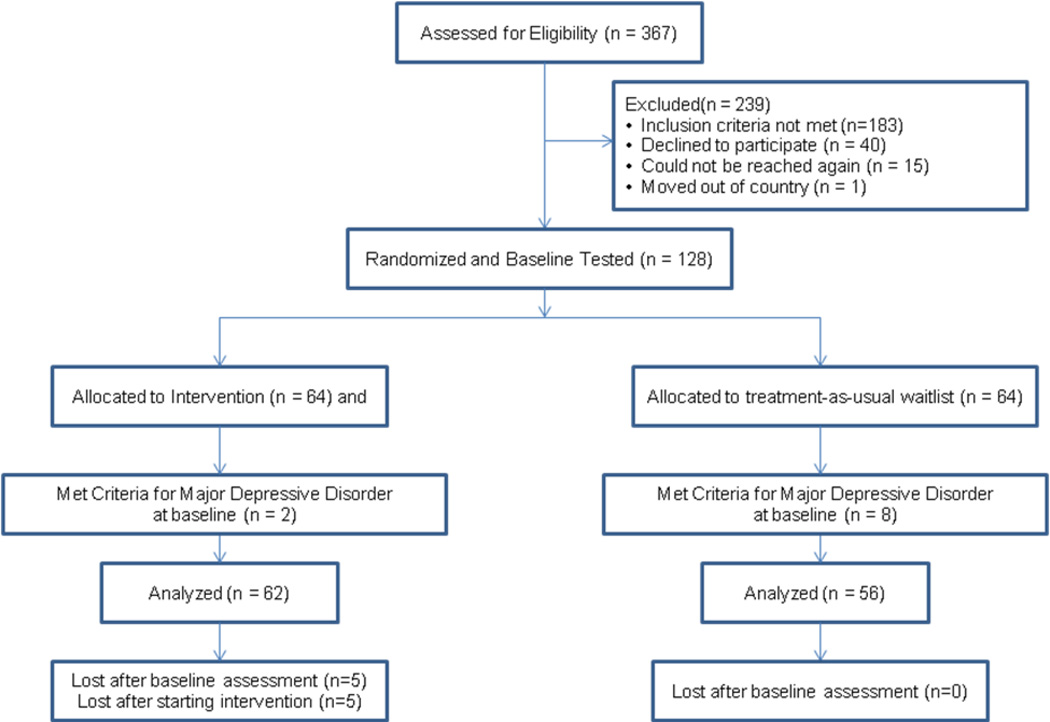
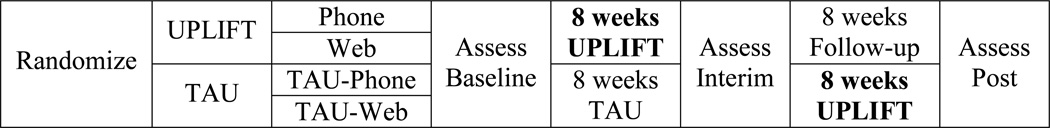
This randomized, controlled trial was conducted between May 2010 and June 2012 and used a cross-over design similar to that used in the original Project UPLIFT study (see Figure 1). Participants were stratified on antidepressant medication use, then randomized to the intervention condition or a treatment-as-usual waitlist condition. Within each condition, participants were assigned to telephone or Web delivery. All groups were assessed at Baseline, Interim (after the intervention groups completed the program; about 9-10 weeks), and Follow-up (after the TAU groups completed the program; about 18-20 weeks).
Figure 1.
Crossover Design
Participants
After receiving approval from the Institutional Review Boards of the four participating university sites in Georgia, Michigan, Texas, and Washington, participants were recruited through each site from among the clinical populations to which they had access. Persons attending epilepsy clinics were approached about participating in the study. After the procedures were explained to participants and they were allowed to ask questions, informed consent for both screening and study inclusion was obtained from all interested participants. Inclusion criteria were: 1) diagnosis of epilepsy; 2) at least three months post initial diagnosis of epilepsy and either on medication or physician-approved to participate; 3) symptoms of depression, but absence of moderate-to-severe depression on the Center for Epidemiologic Studies-Depression (CES-D) scale (Devins & Orme, 1985) (i.e., 8 < CES-D score < 27) or Major Depressive Disorder according to the Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2001); 4) 21 years of age and older; 5) English speaking; 6) access to a telephone; and 7) mentally stable, as determined by a score of > 23 on the telephone version of the Mini-Mental Status Examination (T-MMSE; Newkirk et al., 2004). Individuals who were taking antidepressant medication were not excluded from this study, since Cognitive-Behavioral Therapy has been demonstrated to have a greater effect on relapse prevention than antidepressant medication (Segal et al., 2002).
Of the 367 adults recruited from the four sites (Figure 2), 183 did not meet inclusion criteria; 88 (24%) screened as too depressed, and 10 (3%) others expressed suicidal ideation. Those who met criteria and consented (n = 128) were randomly assigned to condition and baseline assessed. Ten (7.8%) of these 128 participants met criteria for Major Depressive Disorder at baseline and were removed from the study. Sixty-two intervention participants and 56 TAU participants (total n=118) were included in the analyses. The study was powered to detect a small-to-medium effect (effect-size r = 0.20) upon depressive symptoms using the main outcome measure described below. Five (8.9%) intervention participants dropped out before attending any sessions, and six (10.7%) others dropped out after attending at least one.
Figure 2.
CONSORT Flow Diagram
Measures
The following reliable and validated self-report measures of depressive symptoms, knowledge and skills, self-efficacy, self compassion, satisfaction with life, and quality of life comprised the baseline, interim, and follow-up assessments.
Depressive Symptoms were assessed using four different measures. The main outcome measure was a modified version (mBDI; Dori & Overholser, 2000) of the Beck Depression Inventory (BDI; Beck, Rush, Shaw, & Emery, 1979; Beck, Steer, Ball, & Ranieri, 1996), measuring depression severity during the past 2 weeks. This measure has been demonstrated to have good internal consistency and test-retest reliability (Dori & Overholser, 2000). It is comprised of the 21 BDI items; the only modification is the addition of a positive response category for each item, such that responses are scaled from 0 (positive) to 4 (severe). Because of this added category, the mBDI better detects differences in low depression scores (Dori & Overholser, 2000; Walker, Engelhard, & Thompson, 2012). The mBDI can also be scored as a BDI, by combining the 0 and 1 categories. The BDI has demonstrated validity for assessing depression in people with epilepsy (Jones et al., 2005).
The third depressive symptoms measure used was the 6-item Neurological Disorders Depression Inventory for Epilepsy (NDDI-E; Gilliam et al., 2006), which eliminates items that might overlap with cognitive deficits or side effects of seizure medications. The final measure of depressive symptoms was the PHQ-9 (Kroenke et al., 2001), a 10-item instrument that closely follows diagnostic criteria for Major Depression as cited in the Diagnostic and Statistical Manual of Psychiatric Disorders (American Psychiatric Association, 1994). The PHQ-9 has been validated for diagnosing Major Depressive Disorder in primary care (Spitzer, Kroenke, Williams, & the Patient Health Questionnaire Study Group, 1999) and in obstetric-gynecologic patients (Spitzer, Williams, Kroenke, Hornyak, & McMurray, 2000). The PHQ-9 was used to identify Major Depressive Disorder.
Knowledge and skills were assessed using a measure developed for the original Project UPLIFT study (Thompson et al., 2010). It includes 18 true–false items assessing depression knowledge (e.g., “Depression is the most common mental disorder among people with epilepsy”) and 13 Likert-scaled skills items with responses ranging from 1 (poor) to 5 (above average) that are based upon the content of the intervention modules. These items assess participants’ perceived ability to use skills to reduce depressive symptoms (e.g., “I can practice seeing and hearing meditations.”). When knowledge and skills were summed into one scale, the coefficient alpha was 0.810.
Depression Coping Self-Efficacy was assessed using the 24-item Depression Coping Self-Efficacy Scale (DCSES; Perraud, 2000). This instrument uses a visual response scale to indicate confidence for each item from 0 to 100%.
Self Compassion is comprised of seeing one’s own experiences as part of a greater human existence, being understanding and kind toward oneself during experiences of failure or pain, and holding difficult and painful thoughts in mindful awareness instead of over-identifying with them (Neff & Vonk, 2009). The Self-Compassion Scale (SCS; Neff & Vonk, 2009) is a 26-item scale comprised of six subscales: self-kindness, self-judgment, common humanity, isolation, mindfulness, and over-identification. A series of studies demonstrated the reliability and validity of the instrument, as well as the underlying factor structure (Neff, 2003).
The Satisfaction with Life Scale (SWLS; Denier, Emmons, Larsen, & Griffin, 1985) is a five-item measure of global life satisfaction. The SWLS has high internal consistency, good inter-rater reliability, and highly correlates with several other measures of well-being; it does not correlate with measures of social desirability (Denier et al., 1985).
Quality of Life was assessed using 14 items from the Behavioral Risk Factor Surveillance System. Five items assess healthy symptoms, five items assess activity limitations, and four items assess healthy days. Items address both physically and mentally healthy days and symptoms. Several studies have found these measures to be reliable and valid (Andresen, Catlin, Wyrwich, & Jackson-Thompson, 2003; Nelson, Holtzman, Bolen, Stanwyck, & Mack, 2001; Newschaffer, 1998).
Procedure
Assignment
After being screened with the CES-D (Devins & Orme, 1985) and the T-MMSE (Newkirk et al., 2004) and giving consent, participants were stratified by whether or not they were on antidepressants or in psychotherapy, and randomly assigned to the Project UPLIFT condition or the TAU waitlist condition. In the original study of Project UPLIFT, Web and telephone delivery were equivalent in efficacy (Thompson et al., 2010). Therefore, within each condition, people who required a particular mode of delivery (Web or telephone) were placed in that group and the remainder (the majority of participants) were assigned to equalize the groups.
Assessment
Baseline, interim, and follow-up assessments included the measures previously described. Assessment of participants from all sites was conducted by telephone by Master of Public Health students in Georgia. Participants were contacted in advance to schedule the timing of the assessment. They were paid $25 for each assessment completed, and $15 for each session attended.
Delivery
Telephone sessions were held weekly at a scheduled time. Before each telephone session, participants received reminder phone calls. The telephone groups used the technology services of the university in Georgia. Participants got a conference bridge for each call; this allowed them to call in using their own telephone. Those whose call incurred long-distance charges, were provided a calling card number to cover the cost.
The Web-based intervention used Blackboard Course Management System software, a secure online learning system that houses content and includes communication tools. Blackboard tools can be accessed using standard dial-up or higher Internet access. It can be used in any location, at any hour. Within the Blackboard system, one develops "courses," which include asynchronous discussion boards, areas for posting content, and other resources. The Web intervention was created as a Blackboard course. Only the course in which (s)he was enrolled was accessible to the user once (s)he logged into the system. Users’ communications and personal information within the course could be viewed only by the users and system administrators. A username, which did not include an actual name, and a password created by each participant were the only personal information that was entered into Blackboard. Participants were allowed to choose whether or not they wished to share their names with other members of the group. Web sessions were posted on Mondays, and the previous session was moved to an accessible archive when a new session was posted. If a Web participant had not logged into the session by Wednesday, (s)he received a reminder call or email.
Safety Management
As a part of this study, a mental health professional in each state was identified. This mental health professional and the lead author, a Georgia-licensed clinical psychologist, were notified during screening when anyone expressed suicidal ideation or was excluded from the study because they scored above our upper inclusion criterion score of 26 on the CES-D (Devins & Orme, 1985). The mental health professionals provided these persons with referrals for mental health services and their physicians at the epilepsy centers were notified.
Throughout the intervention, research assistants contacted Internet participants who had not logged in within 3 days of the start of a new session, and telephone participants who missed a session. The purpose of the contact was to inquire about their mood and welfare, as well as to remind them about the next session. The group facilitators were trained to make immediate contact with the clinical psychologist, should anything in a session suggest that a participant was in distress. Furthermore, telephone participants signed a consent form acknowledging that they understood the sessions were being audio-recorded and that recordings would be destroyed after review. The clinical psychologist reviewed these audio-recordings, as well as the discussion boards on the Web, to ensure fidelity to the intervention, as well as to detect suicidal ideation or severe depression. Neither condition developed in any of the participants. As an additional precaution, research assistants obtained emergency contact information from participants assigned to telephone groups, so the contact could be reached by a co-facilitator in the event that the participant experienced a seizure during a telephone session. This, also, did not occur.
Analysis
Data input and management were initially performed using SPSS version 19.0. Mean values were used to replace missing data for any participant who was missing fewer than 10 percent of the items on a scale. All statistical tests were 2-sided and a P value ≤ 0.05 was considered statistically significant. The difference in incidence was assessed using a Fisher’s Exact test.
Analyses of changes in depressive symptoms and other measures were performed according to patients’ original treatment assignment (i.e., an intention-to-treat analysis). Repeated-measures analysis of each outcome used a means model with SAS Proc Mixed (version 9), providing separate estimates of the means by time (pre and interim) for each condition. The model included condition, time, and the statistical interaction between the independent variables. A compound-symmetric variance-covariance form among the repeated measurements was assumed for the outcomes and robust estimates of the standard errors of parameters were used to perform statistical tests and construct 95% confidence intervals (Diggle, Liang, & Zeger, 1994).
Mediation was assessed using the student version of LISREL 8.8. Data were pre-screened for missing data, outliers, and skewness. Then, an asymptotic covariance matrix and the diagonally weighted least squares (DWLS) estimation method were used to estimate the model parameters. The asymptotic covariance matrix and DWLS estimation method account for the mix of dichotomous and continuous variables included in the model. Additionally, DWLS is a robust estimation method for analyses with a smaller sample size. Model fit was determined by examining the Satorra-Bentler χ2, Root Mean Squared Error of Approximation (RMSEA), and the Comparative Fit Index (CFI; Hu & Bentler, 1999).
Results
Sample Description
The Project UPLIFT program was delivered to 22 groups of up to 7 people. The 118 participants ranged in age from 21 to 70, with a mean of 41.2 years. Almost two-thirds (65.3%) were female, and 30.5% were on antidepressant medication. Most (n=70; 59.3%) reported they were Caucasian, with 14 (11.9%) African Americans, 3 (2.5%) of Hispanic origin, and 6 (5.1%) of other races; 25 (21.2%) participants did not provide their race/ethnicity. The only difference between the intervention and TAU waitlist conditions at baseline was in the number of days in the last 30 of activity limitation due to poor physical health (t = 1.96, df = 116, p = 0.05), which was greater in the intervention condition (9.2) than in the TAU condition (5.8). This variable was controlled in all other analyses. The difference in PHQ-9 scores between intervention and TAU waitlist approached significance (t = 1.88, df = 116, p = 0.062), with the mean for depressive symptoms in the intervention group (6.9) greater than that in the TAU group (5.5).
Intervention Attendance
Attendance of the sessions was very good, as might be expected with distance delivery to people with transportation limitations. As a result, the distribution of the number of sessions attended was severely negatively skewed (z = −5.49, p < 0.001). Out of a possible 8 sessions to attend, the first quartile was at 6 sessions, the mean was 6.6, and the median was at 7. Due to this extreme skewness, for the purpose of assessing dose-response, the attendance variable was categorized. Dose response requires at least three categories. We set one category above the median and, because the frequency doubled between 4 and 5 sessions and remained relatively constant between 5 and 6 sessions, we set the second cut-point between 4 and 5 sessions. Thus, the three categories selected were half or fewer of the sessions (0–4), most but not all of the sessions (5–7), and all of the sessions (8).
Depression
Incidence of Episodes of Major Depressive Disorder from baseline to interim in the UPLIFT condition was 0/52 (0%; 95% c.l.: 0.0%–6.9%) versus 6/56 (10.7%; 95% c.l.: 2.6%–18.8%) in the TAU condition. This difference was statistically significant (Fisher’s Exact 2-tailed probability = 0.028), and more notable given the fact that participants in the UPLIFT condition approached having higher scores on the PHQ-9 at baseline (see sample description above). In the treatment-as-usual waitlist condition, among those on antidepressant medications there were 3 (21%) incident episodes of Major Depressive Disorder and among those who were not on antidepressant medication there were also 3 (7%) incident episodes of Major Depressive Disorder.
Decrease in Depressive Symptoms from pretest to interim was greater for the UPLIFT condition than for the TAU condition for all measures of depression (see Table 1). The difference was statistically significant for the mBDI and the BDI, and approached significance for the PHQ-9. When this analysis was limited only to those who provided both baseline and interim data (i.e., “completers”), the results for the PHQ-9 were significant (F1,104 = 3.895, p = 0.050). The decrease in the NDDI-E score was greater in the intervention condition, as for the other depression measures, but the difference did not achieve significance. The NDDI-E is the least sensitive measure, with only 6 items. The change in score on the mBDI from pretest to interim did not differ between those receiving Web delivery and those receiving telephone delivery (F1,50=0.02, p = 0.88). There was a dose-response association between number of sessions attended and change in depressive symptoms (see Table 2).
Table 1.
Mean Scores and Time by Condition Interaction for Study Measures
| Measure | Condition | n | Least Squares Means Estimate |
Interaction F |
df | p- value |
||
|---|---|---|---|---|---|---|---|---|
| Baseline | Interim | Num | Den | |||||
| mBDI | UPLIFT | 62 | 20.3 | 16.7 | 4.67 | 1 | 106 | 0.033* |
| TAU | 56 | 20.2 | 19.5 | |||||
| BDI | UPLIFT | 62 | 7.3 | 5.4 | 4.50 | 1 | 106 | 0.036* |
| TAU | 56 | 7.2 | 7.1 | |||||
| NDDI-E | UPLIFT | 62 | 13.1 | 12.3 | 0.35 | 1 | 106 | 0.555 |
| TAU | 56 | 13.0 | 12.6 | |||||
| PHQ−9 | UPLIFT | 62 | 6.7 | 6.4 | 2.75 | 1 | 106 | 0.100+ |
| TAU | 56 | 5.8 | 6.7 | |||||
| Knowledge/Skills | UPLIFT | 62 | 152.4 | 164.0 | 6.01 | 1 | 106 | 0.016* |
| TAU | 56 | 151.9 | 155.6 | |||||
| Depression Coping Self-efficacy | UPLIFT | 62 | 70.5 | 72.6 | 0.67 | 1 | 106 | 0.416 |
| TAU | 56 | 72.6 | 72.5 | |||||
| Self Compassion | UPLIFT | 62 | 19.6 | 20.5 | 1.56 | 1 | 106 | 0.185 |
| TAU | 56 | 20.2 | 20.3 | |||||
| Satisfaction with Life | UPLIFT | 62 | 22.8 | 25.2 | 8.02 | 1 | 106 | 0.006** |
| TAU | 56 | 23.5 | 22.4 | |||||
| Physical Health Quality of Life | UPLIFT | 62 | 75.5 | 73.9 | 0.74 | 1 | 105 | 0.392 |
| TAU | 55 | 78.1 | 79.3 | |||||
| Mental Health Quality of Life | UPLIFT | 62 | 80.5 | 81.4 | 0.28 | 1 | 105 | 0.600 |
| TAU | 55 | 80.3 | 78.4 | |||||
p ≤ 0.01
p ≤ 0.05
p ≤ 0.10
Table 2.
Mean Change in Measure Scores by Number of Sessions Attended
| Measures | 0–4 Sessions Attended |
5–7 Sessions Attended |
All 8 Sessions Attended |
|---|---|---|---|
| Depressive Symptoms (mBDI) | −2.4 | −3.3 | −3.8 |
| Depressive Symptoms (BDI) | −0.7 | −1.8 | −2.3 |
| Depressive Symptoms (PHQ−9) | −0.3 | −0.7 | −0.7 |
| Knowledge/Skills | 3.4 | 8.4 | 12.1 |
| Satisfaction with Life | 1.0 | 1.7 | 2.7 |
When state was added to the model, the decrease in depressive symptoms from pretest to interim continued to differ by condition (F1,99=5.67, p = 0.019). It did not differ by state (F3,110=1.99, p = 0.120), or by the interaction between state and condition (F6,99=0.99, p = 0.435). The mean change in the UPLIFT condition demonstrated a greater decrease than that in the TAU condition in all states (see Table 3).
Table 3.
Change in mBDI Scores by State and Condition
| State | UPLIFT | TAU | ||||
|---|---|---|---|---|---|---|
| Baseline | Interim | Change | Baseline | Interim | Change | |
| A (n=21) | 20.4 | 16.9 | −3.5 | 29.3 | 27.5 | −1.8 |
| B (n=20) | 21.6 | 16.3 | −5.3 | 18.3 | 17.5 | −0.8 |
| C (n=32) | 19.3 | 18.5 | −0.8 | 20.5 | 20.9 | +0.4 |
| D (n=35) | 19.5 | 12.8 | −6.7 | 15.4 | 15.8 | +0.4 |
The mean follow-up in the UPLIFT intervention group was 10.5 weeks (range 7.3–15.1). As shown in Table 4, the groups were almost identical at baseline and follow-up (p ≥ 0.99), but approached a significant difference at interim (p = 0.079). When the analysis was limited to “completers”, the difference at interim became significant (F1,94 = 4.826, p = 0.030). These findings are consistent with the expectation for a cross-over design. While the least squares mean mBDI score increased somewhat in the UPLIFT group from interim (end of intervention) to follow-up, it remained below the baseline least squares mean, although the difference now only approached significance (F1,190= 1.71, p = 0.088). When restricted to “completers” the difference achieved significance (F1,94= 4.031, p = 0.048). At follow-up, when both groups had completed the intervention, the least squares mean mBDI score for all participants (18.07) was significantly lower than at baseline (20.22; t = 2.64, df = 1,190, p = 0.009).
Table 4.
Maintenance of depression outcomes from pretest to posttest.
| Measure | Time | UPLIFT | TAU | t | df | p-value |
|---|---|---|---|---|---|---|
| mBDI | Pretest | 20.2 | 20.2 | 0.00 | 1,190 | 0.999 |
| Interim | 16.6 | 19.5 | −1.77 | 1,190 | 0.079+ | |
| Follow-up | 18.1 | 18.1 | −0.02 | 1,190 | 0.988 |
p < 0.10
Change in Knowledge and Skills
Because there was a ceiling effect in the distribution of knowledge at baseline, the baseline measure was controlled in assessing knowledge and skills. The knowledge and skills score increased by about 3 points from pretest to interim in the TAU condition, compared to an increase of more than 11 points in the UPLIFT condition (see Table 1). This difference was statistically significant (F1,106=6.01, p = 0.016) and demonstrated a dose relationship with sessions attended (see Table 2).
Change in knowledge and skills mediated the association between condition and change in depressive symptoms. In bivariate analyses, condition was significantly associated with knowledge/skills change (r=−0.22, p = 0.025) and condition (r=0.25; p = 0.009) and knowledge/skills change (r=−0.30; p = 0.002) were both associated with change in mBDI score. When change in isolation was controlled, change in knowledge/skills remained significantly associated with change in mBDI score (Beta = −0.30, t = −3.34, p = 0.001)
To assess whether change in knowledge/skills mediated the relationship between condition and change in mBDI score using structural equation modeling, an asymptotic covariance matrix and the diagonally weighted least squares (DWLS) estimation method were used to fit the data to the specified path model from condition, to change in knowledge/skills, to change in mBDI. The model was over-identified (u > t). The effects from condition to change in knowledge/skills (−0.250; 95% confidence interval: −0.421 to −0.079) and from change in knowledge/skills to change in mBDI (−0.980; 95% confidence interval: −1.686 to −0.274) were both significant. The indirect effect of condition on change in mBDI through change in knowledge/skills was 0.245, with a confidence interval from 0.002 to 0.488, indicating a significant mediation effect. The model chi square = 0.0023 (p = 0.96), the RMSEA = 0.00, and the CFI = 1.00 all indicated a good fit of the model.
Change in Other Variables Studied
As seen in Table 1, there was a significant difference between the UPLIFT and TAU conditions in the change in Satisfaction with Life scale (Denier et al., 1985) scores (F1,106=8.02, p = 0.006), and the change varied with number of session attended (see Table 2). Changes in Depression Coping Self Efficacy (Perraud, 2000), Self Compassion (Neff & Vonk, 2009), and Physical and Mental Health Quality of Life (Andresen et al., 2003; Nelson et al., 2001; Newschaffer, 1998) were in the desired direction but not significant.
Discussion
Summary of Findings
Among people with epilepsy with mild-to-moderate symptoms of depression, participation in Project UPLIFT significantly reduced the incidence of Major Depressive Disorder episodes. Moreover, their symptoms of depression were significantly decreased and remained below baseline for 2–3 months. This is particularly notable because the participants for this prevention study were selected from among those on the low end of the depressive symptoms scale; in spite of that fact, Project UPLIFT further decreased their depressive symptoms. As in the original study of Project UPLIFT, there was no difference between the Web- and telephone-delivery groups. This study also found no significant differences by state, although the power was low for doing so. In all four states, the decrease in the intervention condition was greater than that in the treatment-as-usual condition, although the effect sizes may differ from state to state.
The dose-relationship between the number of sessions attended and decline in depression provides support that the decrease in depression was due to participation in Project UPLIFT. The finding that the significant change in knowledge and skills mediated the relationship between condition (UPLIFT versus TAU) and change in depression further supports this conclusion. Furthermore, change in knowledge and skills remained a significant predictor of decline in depression when change in isolation was controlled. Thus, the acquisition of knowledge and skills through Project UPLIFT effected the change in depression, independent of participating in a group with other people with epilepsy.
Participation in Project UPLIFT also increased satisfaction with life, although physical and mental health qualities of life were not significantly changed. The absence of effect upon quality of life may result from studying people with epilepsy. With or without depression, epilepsy is associated with unhealthy days and activity limitation, which constitute more than one-third of the items comprising the quality-of-life measures used (Nelson et al., 2001). Yet, in spite of the absence of impact on participants’ limitations and poor life quality, their satisfaction with life improved. As noted in our previous study (Thompson et al., 2010), this finding accords with the effect of mindfulness (Segal et al., 2002). By attending to suffering, rather than turning away, we recognize the ways in which we link thoughts to the suffering that prolong and even exacerbate it. Once we notice the thoughts, we can use mindfulness skills to let them go and, thus, reduce the suffering.
Clinical Importance
Project UPLIFT was not developed as a replacement for face-to-face treatment. When developed, the program’s purpose was to reach people who otherwise frequently do not have access to treatment for depression. In this study, the target was people with epilepsy. With an eye toward the high level of comorbidity of depression with chronic diseases in general (Egede, 2007), however, the program was designed to be easily adapted for other hard-to-reach populations.
When it was first developed, Project UPLIFT constituted an important step forward in the delivery of depression treatment (Thompson et al., 2010) in several regards: (1) people whose mobility is impaired by disability, or even the fatigue and loss of energy associated with depressive symptoms, can be reached; (2) people who are in rural or otherwise hard-to-reach areas can participate; (3) persons with specific conditions who live far apart can be brought together in a group to connect and share their experiences; and (4) this intervention builds capacity for future intervening within populations with chronic disease by training peers with the disease to co-deliver the intervention. Furthermore, there is a significant savings in terms of cost and time associated with travel to treatment by the participants, and cost of professional time, as the intervention is delivered by peers and trainees who are supervised by the professional. This study, which demonstrates that Project UPLIFT is also effective for preventing episodes of Major Depressive Disorder, adds to these benefits. The added benefits include: (1) avoiding the disability and lost productivity associated with depression (Gillham, Shatté, & Freres, 2000); (2) eliminating the tangible and intangible costs associated with treating an episode of Major Depressive Disorder after it has already occurred; and (3) providing people with the skills to manage future encounters with stress and difficult life circumstances.
Limitations and Strengths
The current study was powered to detect differences in depressive symptoms and, as a result, it had limited power for detecting the smaller differences seen in self-efficacy and self compassion, or changes seen at follow-up. In addition, because of the cross-over design, only the analyses before the crossover could employ a control condition and the follow-up period was restricted to a period of about 10 weeks. With such a limited follow-up period, it is possible that these results reflect a temporary delay in onset of depressive episodes. The duration of the effects should be the subject of future studies. Another limitation was that only four states participated, with one-to-two referring clinics in each. While, distance delivery allows access to persons beyond state lines, mental health professionals are licensed at the state-level. Until there is better coordination from state to state to ensure the safety of participants at a distance, and greater clarity about how licenses apply in distance-delivery situations, delivery locations must be restricted. Lastly, the intervention was compared with a TAU condition rather than another active intervention, resulting in several limitations. Notable among these is the fact that, due to session attendance, intervention participants had the potential for greater compensation from baseline to interim than those in the TAU condition.
There are also some important strengths of the study. First, the study contributes to literature on the prevention of depression. It also contributes to the literature on the effectiveness of cognitive-behavioral therapy and mindfulness-based treatment of depression by employing distance delivery of these techniques and reaching groups of people who might otherwise have no access to treatment. Furthermore, this is one of the first studies demonstrating the effectiveness of a preventive intervention for depression that is distance delivered. Finally, we employed a randomized, controlled design and the intervention was compared to a TAU control. In some cases, TAU included medication and psychotherapy. Thus, our intervention provided benefit over and above these.
Conclusions
Project UPLIFT was effective in preventing episodes of Major Depressive Disorder and further reducing depressive symptoms among people with epilepsy and mild-to-moderate depressive symptoms. It also increased their knowledge and skills related to mindfulness and cognitive methods, as well as their satisfaction with life. Although initially developed for people with epilepsy, the intervention is easily be adapted to other chronic disease populations, and has already been adapted for people with cystic fibrosis and people with multiple sclerosis in two pilot studies. Many people with chronic illness and other disparity populations suffer increased rates of depression (Carroll, Cassidy, & Cote, 2003; Evans et al., 2005); as a result, preventing their depression has the potential to significantly decrease the prevalence of depression in the entire population. Project UPLIFT provides one mechanism for doing so.
Public Health Significance.
Using distance delivery, Project UPLIFT prevented episodes of Major Depressive Disorder and further reduced depressive symptoms among people with epilepsy and mild-to-moderate depressive symptoms. Easily adapted for people with other chronic diseases, many of whom suffer increased rates of depression, interventions like Project UPLIFT have the potential to significantly decrease the prevalence of depression in the population.
Acknowledgments
This research was supported by NIH Grant #5RC1 MD004563 from the National Center for Minority Health and Health Disparities
References
- Agresti A, Coull BA. Approximate is better than “exact” for interval estimation of binomial proportions. The American Statistician. 1998;52(2):119–126. [Google Scholar]
- American Epilepsy Society, & The Centers for Disease Control and Prevention (CDC) Living Well with Epilepsy II. Baltimore, Maryland: 2003. Report of the 2003 National Conference on Public Health and Epilepsy: Priorities for a public health agenda on epilepsy. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. J Epidemiol Community Health. 2003;57(5):339–343. doi: 10.1136/jech.57.5.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Carroll LJ, Cassidy JD, Cote P. Factors associated with the onset of an episode of depressive symptoms in the general population. Journal of Clinical Epidemiology. 2003;56:651–658. doi: 10.1016/s0895-4356(03)00118-5. [DOI] [PubMed] [Google Scholar]
- Cramer JA, Blum D, Reed M, Fanning K. The influence of comorbid depression on seizure severity. Epilepsia. 2003;44(12):1578–1584. doi: 10.1111/j.0013-9580.2003.28403.x. [DOI] [PubMed] [Google Scholar]
- Commission on Chronic Illness. Chronic Illness in the United States. Volume I: Prevention of Chronic Illness. Cambridge, MA: Harvard University Press; 1957. [Google Scholar]
- Denier E, Emmons R, Larsen R, Griffin M. The satisfaction with life scale. Journal of Personality Assessment. 1985;(49):71–76. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Devins G, Orme C. Center for Epidemiologic Studies Depression Scale. In: Keyser D, Sweetland R, editors. Test Critiques. II. Kansas City, MO: Test Corporation of America; 1985. pp. 144–160. [Google Scholar]
- Dori GA, Overholser JC. Evaluating depression severity and remission with a modified Beck Depression Inventory. Personality and Individual Differences. 2000;28(6):1045–1061. [Google Scholar]
- Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. General Hospital Psychiatry. 2007;29:409–416. doi: 10.1016/j.genhosppsych.2007.06.002. [DOI] [PubMed] [Google Scholar]
- Evans DL, Charney DS, Lewis L, Golden RN, Gorman JM, Krishnan KR, Valvo WJ. Mood disorders in the medically ill: scientific review and recommendations. Biological Psychiatry. 2005;58(3):175–189. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Shatté AJ, Freres DR. Preventing depression: A review of cognitive-behavioral and family interventions. Appl & Prev Psychol. 2000;9(2):63–88. [Google Scholar]
- Gilliam FG, Barry JJ, Hermann BP, Meador KJ, Vahle V, Kanner AM. Rapid detection of major depression in epilepsy: a multicentre study. Lancet Neurol. 2006;5(5):399–405. doi: 10.1016/S1474-4422(06)70415-X. [DOI] [PubMed] [Google Scholar]
- Hermann B, Seidenberg M, Bell B. Psychiatric comorbidity in chronic epilepsy: identification, consequences, and treatment of major depression. Epilepsia. 2000;41(Suppl. 2):S31–S41. doi: 10.1111/j.1528-1157.2000.tb01522.x. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- IOM (Institute of Medicine) Epilepsy across the spectrum : Promoting health and understanding. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- Jia H, Ried LD, Wang X, Damush TM, Young LJ, Cameon RH, Williams LS. Geographic variation in poststroke depression among veterans with acute stroke. Journal of Rehabilitation Research & Development. 2008;45(7):1027–1035. doi: 10.1682/jrrd.2007.06.0090. [DOI] [PubMed] [Google Scholar]
- Jones JE, Herman BP, Woodard JL, Barry JJ, Gilliam F, Kanner AM, Meador KJ. Screening for major depression in epilepsy with common self-report depression inventories. Epilepsia. 2005;46:731–735. doi: 10.1111/j.1528-1167.2005.49704.x. [DOI] [PubMed] [Google Scholar]
- Jones JE, Hermann BP, Barry JJ, Gilliam FG, Kanner AM, Meador KJ. Rates and risk factors for suicide, suicidal ideation, and suicide attempts in chronic epilepsy. Epilepsy & Behavior. 2003;4(Suppl 3):S31–S38. doi: 10.1016/j.yebeh.2003.08.019. [DOI] [PubMed] [Google Scholar]
- Kanner AM. Depression in epilepsy: Prevalence, clinical semiology, pathogenic mechanisms, and treatment. Biological Psychiatry. 2003;54:388–398. doi: 10.1016/s0006-3223(03)00469-4. [DOI] [PubMed] [Google Scholar]
- Kanner AM, Balabanov A. Depression and epilepsy: How closely related are they? Neurology. 2002;58(Suppl 5):S27–S39. doi: 10.1212/wnl.58.8_suppl_5.s27. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff K. The development and vaidation of a scale to measure self-compassion. Self and Identity. 2003;2:S3–S42. [Google Scholar]
- Neff KD, Vonk R. Self-compassion versus global self-esteem: two different ways of relating to oneself. J Pers. 2009;77(1):23–50. doi: 10.1111/j.1467-6494.2008.00537.x. [DOI] [PubMed] [Google Scholar]
- Nelson DE, Holtzman D, Bolen J, Stanwyck CA, Mack KA. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS) Soz Praventivmed. 2001;46(Suppl 1):S3–S42. [PubMed] [Google Scholar]
- Newkirk LA, Kim JM, Thompson JM, Tinklenberg JR, Yesavage JA, Taylor JL. Validation of a 26-point telephone version of the Mini-Mental State Examination. J Geriatr Psychiatry Neurol. 2004;17(2):81–87. doi: 10.1177/0891988704264534. [DOI] [PubMed] [Google Scholar]
- Newschaffer C. National Center for Chronic Disease Prevention and Health Promotion. Atlanta, GA: 1998. Validation of Behavioral Risk Factor Surveillance System (BRFSS) HRQOL measures in a statewide sample. [Google Scholar]
- Perraud S. Development of the Depression Coping Self-Efficacy Scale (DCSES) Archives of Psychiatric Nursing. 2000;14(6):276–284. doi: 10.1053/apnu.2000.19090. [DOI] [PubMed] [Google Scholar]
- Polednak A. US regional differences in death rates from depression. Social Psychiatry and Psychiatric Epidemiology. 2012;47(12):1977–1983. doi: 10.1007/s00127-012-0503-z. [DOI] [PubMed] [Google Scholar]
- Prevention, C. f. D. C. a. Public health action plan to integrate mental health promotion and mental illness prevention with chronic disease prevention, 2011–2015. Atlanta: U. S. Department of Health and Human Services; 2011. [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York: Guilford; 2002. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW the Patient Health Questionnaire Study Group. Validity and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Kroenke K, Hornyak R, McMurray J. Validity and utility of the Patient Health Questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. American Journal of Obstetrics & Gynecology. 2000;183:759–769. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- Thompson NJ, Walker ER, Obolensky N, Winning A, Barmon C, Diiorio C, Compton MT. Distance delivery of mindfulness-based cognitive therapy for depression: project UPLIFT. Epilepsy & Behavior. 2010;19(3):247–254. doi: 10.1016/j.yebeh.2010.07.031. [DOI] [PubMed] [Google Scholar]
- U. S. Department of Health and Human Services. How is HHS addressing Multiple Chronic Conditions? [Retrieved June 5, 2013];2013 from http://www.hhs.gov/ash/initiatives/mcc/address-mcc.html.
- Ustun TB, Ayuso-Mateos JL, Chatterji S, Mathers C, Murray CJ. Global burden of depressive disorders in the year 2000. British Journal of Psychiatry. 2004;184:386–392. doi: 10.1192/bjp.184.5.386. [DOI] [PubMed] [Google Scholar]
- Walker ER, Engelhard G, Thompson NJ. Using Rasch measurement theory to assess three depression scales among adults with epilepsy. Seizure: European Journal of Epilepsy. 2012;21(6):437–443. doi: 10.1016/j.seizure.2012.04.009. [DOI] [PubMed] [Google Scholar]
- Walker ER, Obolensky N, Dini S, Thompson NJ. Formative and process evaluations of a cognitive-behavioral therapy and mindfulness intervention for people with epilepsy and depression. Epilepsy & Behavior. 2010;19(3):239–246. doi: 10.1016/j.yebeh.2010.07.032. [DOI] [PubMed] [Google Scholar]