Abstract
Introduction
Obesity incurs a substantial economic burden to healthcare systems. Little is known about the combined medical costs attributable to obesity among individuals with physical disabilities (PDs).
Purpose
To estimate the annual healthcare utilization and expenditure associated with overweight and obesity among adults with and without PDs.
Methods
Weighted multivariate generalized linear models were used to estimate healthcare costs and utilization among adults with and without PDs, across standard BMI categories, using the 2002–2011 Medical Expenditure Panel Survey. The analyses, performed in 2013–2014, included a population representative sample of 215,107 individuals, aged ≥18 years. 36,349 adults reported moderate or significant PDs. The primary outcomes were total healthcare costs, physician office visits, and hospitalization.
Results
After adjusting for sociodemographic variables, self-rated mental and physical health, physical activity, and year, adults with PDs incurred more than 1.96 times the adjusted total healthcare costs ($4,298, 95% CI=$3,980, $4,617) than adults without PDs. Obese individuals spent significantly more than those at normal weight ($726, p<0.001). Obese individuals with PDs spent 1.13 times more than normal-weight individuals with PDs ($1,107, p<0.001), and >2.2 times more than normal-weight individuals without PDs ($5,197, p<0.001). PDs plus obesity represents $23.9 billion/year, or roughly 50% of the total costs attributable to obesity in the U.S.
Conclusions
Across BMI categories, there was significantly greater healthcare utilization and cost among adults with PDs, independent of age, race, education, and SES. Health policies need to identify behavioral interventions that address both healthy weight achievement/maintenance and functional independence among all adults.
Introduction
Previous research has examined the effect of overweight and obesity on healthcare utilization in the general population,1–4 and on the whole, demonstrates a considerable economic burden that continues to escalate as the prevalence of overweight and obesity increases. By 2030, obesity prevalence and the medical costs attributable to obesity are projected to reach 50% of the population, and account for 16%–18% of total healthcare expenditure,5 respectively. Though clearly disturbing, these statistics generally fail to account for individuals with chronic or congenital physical disabilities (PDs)—a subpopulation in which overweight and obesity prevalence is significantly higher.6–10 Considering that individuals with disabilities also incur higher state and national healthcare expenditures,11,12 the combined effect of obesity as a secondary condition of disability may represent a significant, multiplicative burden. Recent changes in the structure of national health care were devised to increase coverage for the uninsured and promote greater emphasis on access to preventive care. However, there has been very little surveillance of the healthcare utilization associated with modifiable behaviors such as obesity among individuals with PDs.
Although many individuals with PDs are at increased risk for weight gain due to habitually sedentary lifestyles,13 it is also well-established that obesity itself is a primary driver of mobility disability and functional decline.14–16 Whether obesity is a contributing factor or consequence of PD is certainly a vexing clinical concern; however, there prevails an urgent demand for large-scale epidemiologic studies that can identify the associations between PDs plus obesity and outcomes related to both healthcare utilization and medical comorbidities. Anderson and colleagues17 recently demonstrated that obese individuals with disabilities had almost three times the additional cost of people without disabilities. Although an important addition to the body of literature pertaining to healthcare utilization in a non-specific disabilities subpopulation, what remains to be determined is the extent to which PDs and obesity influence healthcare utilization, as well as the comparative involvement of chronic conditions between people with and without PDs. Indeed, because physical dysfunction and obesity are interrelated factors, it is vital to better understand the healthcare implications stemming from each, and perhaps more importantly, the burden associated with a synchronicity of obesity plus PD. Therefore, the purposes of this study were to determine the healthcare utilization associated with PDs and obesity, using the 2002– 2011 Medical Expenditure Panel Survey (MEPS), and to estimate the differences in chronic, obesity-related comorbidities between adults with and without PDs.
Methods
Data
The Household Component files of the 2002–2011 MEPS were used for this investigation. MEPS is an ongoing, nationally representative survey of the U.S. civilian, non-institutionalized population, conducted annually by the Agency for Healthcare Research and Quality (AHRQ).18 MEPS has been reviewed and approved by the Westat IRB, established under a multi-project assurance granted by the Office for Protection from Research Risks. The project is reviewed and the approval renewed annually. In these analyses, which were performed in 2013–2014, only individuals who were aged ≥18 years and had a BMI of ≥18.5 kg/m2 were eligible for inclusion. Individuals with BMI <18.5 kg/m2 were excluded, given the known association between underweight status and pre-existing illness (i.e., reverse causation).19 The initial sample size included 230,369 individuals. Variable-specific non-response rates ranged from 0% to 4%. After deleting cases with missing data on dependent or independent variables, and cases with non-positive weights,20–22 the final sample consisted of 215,107 individuals. Of those, 36,349 reported moderate or severe PDs. Variables and descriptive statistics are reported in Table 1. Adjustments were made for the clustered and stratified survey design of MEPS, and all estimates were weighted using the AHRQ-supplied weights. Stata, version 13 (StataCorp LP, College Station TX) was used for all statistical analyses.
Table 1.
Characteristics of individuals with and without physical disabilities, aged 18 and over.
| N = 215,107 | 36,349 | 178,758 | |||||
|---|---|---|---|---|---|---|---|
| With physical disabilities | Without physical disabilities | ||||||
| Definition | Mean | SE | Mean | SE | Difference | % missing | |
| Independent variables: | |||||||
| Normal weight | 1 if 18.4= < BMI = < 25 | 0.27 | 0.00 | 0.38 | 0.00 | −0.11* | 4.23 |
| Overweight | 1 if 25 < BMI = < 30 | 0.31 | 0.00 | 0.37 | 0.00 | −0.06* | 4.23 |
| Obese | 1 if BMI > 30 | 0.42 | 0.00 | 0.25 | 0.00 | 0.16* | 4.23 |
| Age 18-24 | 1 if age between 18-24 | 0.03 | 0.00 | 0.15 | 0.00 | −0.12* | 0.00 |
| Age 25-34 | 1 if age between 25-34 | 0.06 | 0.00 | 0.21 | 0.00 | −0.15* | 0.00 |
| Age 35-44 | 1 if age between 35-44 | 0.11 | 0.00 | 0.21 | 0.00 | −0.10* | 0.00 |
| Age 45-54 | 1 if age between 45-54 | 0.19 | 0.00 | 0.19 | 0.00 | −0.01 | 0.00 |
| Age 55-64 | 1 if age between 55-64 | 0.21 | 0.00 | 0.13 | 0.00 | 0.08* | 0.00 |
| Age 65-74 | 1 if age between 65-74 | 0.18 | 0.00 | 0.07 | 0.00 | 0.11* | 0.00 |
| Age 75+ | 1 if age is 75 or older | 0.23 | 0.00 | 0.04 | 0.00 | 0.19* | 0.00 |
| Female | 1 if individual is female | 0.61 | 0.00 | 0.49 | 0.00 | 0.12* | 0.00 |
| White | 1 if individual is white | 0.75 | 0.01 | 0.68 | 0.01 | 0.07* | 0.00 |
| African-American | 1 if individual is African-American | 0.12 | 0.00 | 0.11 | 0.00 | 0.01* | 0.00 |
| Hispanic | 1 if individual is Hispanic | 0.08 | 0.00 | 0.14 | 0.00 | −0.06* | 0.00 |
| Other race/ethnicities | 1 if individual is other race/ethnicity | 0.05 | 0.00 | 0.07 | 0.00 | −0.02* | 0.00 |
| Married | 1 if individual is married | 0.47 | 0.01 | 0.57 | 0.00 | −0.11* | 0.00 |
| Less than high school | 1 if individual has no high school diploma | 0.23 | 0.00 | 0.14 | 0.00 | 0.09* | 0.00 |
| High school | 1 if individual has high school diploma/GED | 0.54 | 0.00 | 0.49 | 0.00 | 0.04* | 0.83 |
| College degree | 1 if individual has college/graduate degree | 0.16 | 0.00 | 0.29 | 0.00 | −0.12* | 0.83 |
| Other degree | 1 if individual has other degree | 0.07 | 0.00 | 0.08 | 0.00 | −0.01* | 0.83 |
| Poor income level | 1 if household income is <100% FPL | 0.18 | 0.00 | 0.10 | 0.00 | 0.08* | 0.00 |
| Near poor income level | 1 if household income is 100-124% FPL | 0.07 | 0.00 | 0.04 | 0.00 | 0.04* | 0.00 |
| Low income level | 1 if household income is 125-199% FPL | 0.18 | 0.00 | 0.12 | 0.00 | 0.06* | 0.00 |
| N = 215,107 | 178,758 | 36,349 | |||||
|---|---|---|---|---|---|---|---|
| With physical disabilities | Without physical disabilities | ||||||
| Mean | SE | Mean | SE | Difference | %missing | ||
| Middle income level | 1 if household income is 200-399% FPL | 0.29 | 0.00 | 0.31 | 0.00 | −0.02* | 0.00 |
| High income level | 1 if household income >=400% FPL | 0.28 | 0.00 | 0.44 | 0.00 | −0.16* | 0.00 |
| Has private health insurance | 1 if individual has private insurance | 0.50 | 0.01 | 0.70 | 0.00 | −0.19* | 1.07 |
| Has Medicare | 1 if individual has Medicare | 0.52 | 0.01 | 0.12 | 0.00 | 0.39* | 1.07 |
| Has Medicaid | 1 if individual has Medicaid | 0.17 | 0.00 | 0.06 | 0.00 | 0.11* | 1.07 |
| Has no health insurance | 1 if individual has no health insurance | 0.09 | 0.00 | 0.15 | 0.00 | −0.07* | 0.00 |
| Has good health | 1 if individual reported good health | 0.57 | 0.00 | 0.93 | 0.00 | −0.36* | 0.89 |
| Has good mental health | 1 if individual reported good mental health | 0.78 | 0.00 | 0.96 | 0.00 | −0.17* | 0.91 |
| Exercisec | 1 if individual reported exercising weekly | 0.38 | 0.00 | 0.62 | 0.00 | −0.24* | 12.58 |
| Northeast | 1 if individual lives in Northeast | 0.17 | 0.01 | 0.19 | 0.01 | −0.02* | 1.07 |
| Midwest | 1 if individual lives in Midwest | 0.23 | 0.01 | 0.22 | 0.01 | 0.01 | 1.07 |
| West | 1 if individual lives in West | 0.21 | 0.01 | 0.23 | 0.01 | −0.02* | 1.07 |
| South | 1 if individual lives in South | 0.39 | 0.01 | 0.36 | 0.01 | 0.03* | 1.07 |
| Metropolitan area | 1 if individual lives in a metropolitan area | 0.79 | 0.01 | 0.84 | 0.01 | −0.05* | 1.07 |
Source: Data are from the household component files of the 2002-2011 Medical Expenditure Panel Survey.
Notes: The variables listed are the explanatory variables in the estimated regression models.
The mean of this variable differs significantly between the individuals with and without physical disabilities at the alpha = 0.01 level.
Because of the high percentage of missing values, this variable is not included in the regression models.
Measures
PDs were defined by questions related to limitations in physical functioning within MEPS. The following question was asked at the family level: Does anyone in the family have difficulties walking, climbing stairs, grasping objects, reaching overhead, lifting, bending, or stooping for long period of time? If yes, then the specific person was identified and coded as “yes.” Thereafter, a subsequent series of questions was administered to identify the severity as: (1) no difficulty; (2) some difficulty; (3) a lot of difficulty; (4) unable to do; or (5) completely unable to do. Individuals were identified as having a PD who answered yes to the above screening question, and that had either a lot of difficulty, were unable, or were completely unable to do the specific physical functioning activities.
Healthcare costs and utilization were examined with five measures: (1) total annual healthcare costs; (2) whether the individual had any office visits during the year; (3) total number of office visits during the year; (4) whether the individual stayed in the hospital during the year; and (5) total number of nights stayed in the hospital during the year, if any. Questions were asked regarding each office and hospital visit during the previous round, and the corresponding total cost of each visit. Numbers of annual office and hospital visits were obtained from the utilization section of MEPS, and total annual healthcare cost was from the expenditures section. Total costs were converted to inflation-adjusted 2013 dollars using the all-items Consumer Price Index.
Andersen's conceptual framework guided the choice of explanatory variables for the models.23,24 Each model included need-related variables such as age, gender, and measures of health and function. Relevant sociodemographic factors were also included, such as race and ethnicity, marital status, education, income, health insurance, and geographic location. Weight status was determined by a series of mutually exclusive indicators to determine whether the individual was normal weight (BMI between 18.5 and 24.9 kg/m2), overweight (BMI between 25 and 29.9 kg/m2), or obese (BMI ≥30 kg/m2). Two indicators for whether self-rated health and mental health, respectively, were fair or poor, as opposed to good or better, were included in the models, as well as an indicator for whether the individual reported any of the PD measures (difficulty in walking, stepping, standing, lifting, bending, reaching, or grasping). To ascertain physical activity participation, adult respondents were asked if they spend half an hour or more in moderate or vigorous physical activity at least three times a week. The MEPS glossary states, “moderate physical activity causes only light sweating or a slight or moderate increase in breathing or heart rate and would include activities such as fast walking, raking leaves, mowing the lawn, or heavy cleaning. Vigorous physical activity causes heavy sweating or large increases in breathing or heart rate and would include activities such as running, race walking, lap swimming, aerobic classes, or fast bicycling.”
Race and ethnicity was determined using the U.S. Census, with white serving as the reference category, and with African American, Hispanic, and other race/ethnicities representing the other categories. Marital status was measured with an indicator for whether the individual was currently married. Education was measured by a series of mutually exclusive indicators for whether education attainment was less than high school, college degree, graduate school degree, or another degree, with high school serving as the reference category. Household income was measured using four mutually exclusive categories: poor (household income <100% of the federal poverty level [FPL]), near poor (household income 100%–125% of FPL), low income (household income 125%–199% of FPL), middle income (household income 200%–399% of FPL), and high income (household income ≥400% of FPL). For health insurance, indicators were included for whether the individual reported (at any time during the previous year) having Medicare, Medicaid, private health insurance, or no insurance. Analyses also controlled for whether the individual resided in an urban area, and the U.S. Census region, with the South as the reference.
Statistical Analysis
For any-office-visits and any-nights-hospitalized categories, logistic regression models were fitted (Appendix Tables 1–2). For the total healthcare costs and positive number of office visits and nights hospitalized, generalized linear models (GLMs) were used.25 On the basis of a modified Park test26 and other standard diagnostics,27,28 GLM was used with a log link and gamma distribution for the cost measure, and GLM with a log link and negative binomial distribution for the total number of positive utilization measures (Appendix Tables 3–5). Values reported in Tables 2–4 are the fully adjusted predicted values based on the previously described regression models.
Table 2.
Estimated differences in healthcare utilization and costs between individuals with and without physical disabilities
| Measures | Individuals with physical disabilities | Individuals without physical disabilities | Difference (95% CI) | |||
|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | |||
| Total healthcare costs ($) | 8,766.38* | 151.09 | 4,468.35* | 43.94 | 4,298.03** | (3,979.55 – 4,616.53) |
| Any office visits | 0.84* | 0.00 | 0.72* | 0.00 | 0.12** | (0.12 – 0.13) |
| Any hospitalization | 0.13* | 0.00 | 0.07* | 0.00 | 0.06** | (0.06 – 0.07) |
| Number of office visits | 11.19* | 0.12 | 6.90* | 0.06 | 4.29** | (4.02 – 4.56) |
| Number of nights hospitalized | 7.18* | 0.21 | 4.94* | 0.11 | 2.24** | (1.73 – 2.73) |
Source: Data are from the household component files of the 2002-2011 Medical Expenditure Panel Survey.
Notes: All estimates are based on regression models presented in Appendix Tables 1-5.
Coefficient significant at the 95% CI (alpha = 0.05)
The mean of this estimate differs significantly between the individuals with and without physical disabilities at the 95% CI (alpha =0.05).
Table 4.
Healthcare utilization and costs associated with physical disability status, and for normal weight, overweight, and obesity
| Individuals with physical disabilities: | ||||||||
|---|---|---|---|---|---|---|---|---|
| Normal weight | Overweight | Differences | Obese | Differences | ||||
| Measures | Mean | SE | Mean | SE | Mean | SE | ||
| Total healthcare costs ($) | 8,341.19*,*** | 175.23 | 8,571.34*,*** | 169.47 | −230.15 | 9,448.21*,*** | 171.26 | −1,107.02** |
| Any office visits | 0.83*,*** | 0.00 | 0.85*,*** | 0.00 | −0.02** | 0.87*,*** | 0.00 | −0.04** |
| Any hospitalization | 0.12*,*** | 0.00 | 0.12*,*** | 0.00 | 0.00 | 0.13*,*** | 0.00 | −0.01** |
| Number of office visits | 10.77*,*** | 0.15 | 11.13*,*** | 0.14 | −0.36** | 11.75*,*** | 0.15 | −0.98** |
| Number of nights hospitalized | 7.47*,*** | 0.26 | 7.16*,*** | 0.26 | 0.31 | 6.88*,*** | 0.22 | 0.59 |
| Individuals without physical disabilities: | ||||||||
| Total healthcare costs ($) | 4,251.62* | 61.83 | 4,368.93* | 57.22 | −117.31 | 4,815.88* | 63.03 | −564.26** |
| Any office visits | 0.70* | 0.00 | 0.72* | 0.00 | −0.02** | 0.75* | 0.00 | −0.05** |
| Any hospitalization | 0.07* | 0.00 | 0.07* | 0.00 | 0.00 | 0.08* | 0.00 | −0.01** |
| Number of office visits | 6.64* | 0.09 | 6.86* | 0.08 | −0.22** | 7.25* | 0.11 | −0.61** |
| Number of nights hospitalized | 5.14* | 0.14 | 4.93* | 0.14 | 0.21 | 4.73* | 0.14 | 0.41 |
Source: Data are from the household component files of the 2002-2011 Medical Expenditure Panel Survey.
Notes: All estimates are based on regression models presented in Appendix Tables 1-5.
Coefficient significant at the 95% CI (alpha = 0.05)
The mean of this estimate differs significantly between individuals with normal weight and individuals who are overweight or obese at the 95% CI (alpha =0.05).
The mean of this estimate differs significantly between the individuals with and without physical disabilities, within each weight level, at the 95% CI (alpha =0.05).
Results
Table 1 provides unadjusted healthcare utilization and sociodemographic information for adults with and without PDs. Obesity prevalence was higher among adults with PDs (42% vs 25% among adults without PDs, p<0.001). Adults with PDs had less formal education (i.e., 23% of the adults with PDs vs 14% without had less than a high school diploma, and 16% compared to 29% without PDs had a college degree). Adults with PDs also had lower income: 18% of individuals with PDs (vs 10% without) were considered to be poor, and 28% with PDs (vs 44% without) were considered to have high income. Compared to individuals without PDs, most individuals with PDs had health insurance: 91% vs 75%, respectively. However, the majority of adults with PDs relied on public health insurance such as Medicare (52% vs 12%) or Medicaid (17% vs 6%). Finally, compared to the 93% and 62% of adults without PDs, only 57% and 38% of adults with PDs reported having good health and regular exercise participation, respectively.
All five measures of costs and utilization indicated significantly higher costs and utilization of services among adults with PDs (Table 2). Based on the full adjusted models (Appendix Tables 1–5), on average adults with PDs spent $4,298 more on total health care, had 12% greater probability of visiting the office at least once, had 6% greater probability of being hospitalized at least once, had four more office visits during the year, and spent two more nights in hospital (i.e., if hospitalized) throughout a given year.
Table 3 shows the predicted differences in healthcare costs and utilization between individuals within the normal weight range as compared to individuals that were overweight and obese (Appendix Tables 1–5). The estimated differences between individuals with normal BMIs and individuals who were overweight were small and not significant. However, the total annual healthcare costs were $727 greater for individuals who were obese, compared to normal weight adults. Moreover, obese adults had 5% greater probability of visiting the office at least once, 1% greater probability of getting hospitalized, and had less than one additional office visit (8.43 vs 7.73) during the year.
Table 3.
Healthcare utilization and costs between normal weight and overweight or obese
| Normal Weight | Overweight | Differences | Obese | Differences | ||||
|---|---|---|---|---|---|---|---|---|
| Measures | Mean | SE | Mean | SE | Mean | Mean | SE | Mean |
| Total healthcare costs ($) | 5,474.94* | 80.82 | 5,626.01* | 73.69 | −151.07 | 6,201.55* | 73.43 | −726.61** |
| Any office visits | 0.71* | 0.00 | 0.73* | 0.00 | −0.02** | 0.76* | 0-.00 | −0.05** |
| Any hospitalization | 0.08* | 0.00 | 0.08* | 0.00 | 0.00 | 0.09* | 0.00 | −0.01** |
| Number of office visits | 7.73* | 0.07 | 7.98* | 0.07 | −0.25** | 8.43* | 0.09 | −0.70** |
| Number of nights hospitalized | 6.18* | 0.15 | 5.92* | 0.15 | 0.26 | 5.69* | 0.14 | 0.49 |
Source: Data are from the household component files of the 2002-2011 Medical Expenditure Panel Survey.
Notes: All estimates are based on regression models presented in Appendix Tables 1-5.
Coefficient significant at the 95% CI (alpha = 0.05)
The mean of this estimate differs significantly between individuals with normal weight and individuals who are overweight or obese at the 95% CI (alpha =0.05).
Table 4 shows adjusted predicted healthcare utilization and cost measures, stratified by PD and weight category. Except for at least one office visit (by 1%, p<0.001) and number of office visits (by 0.36, p<0.001), there were no significant differences in estimated cost and utilization between individuals who were normal weight and overweight. However, individuals with PDs who were obese had $1,107 greater total healthcare costs, 4% greater chance of having office visits, approximately one additional office visit, 1% greater chance of having any hospitalization, and yet fewer nights of hospitalization (all p<0.001), as compared to those who were normal weight.
Moreover, for adults without PDs, individuals who were obese had $564 greater total healthcare costs, 5% greater chance of having any office visits, less than one additional office visit, 1% greater chance of having any hospitalization, and fewer nights of hospitalization (all p<0.001), as compared to normal-weight status. Within each BMI category, adults with PDs had significantly greater healthcare costs and utilization than adults without PDs for each outcome (all p<0.001). In summary, Table 4 indicates that having PDs confers significantly increased utilization and cost of health care, regardless of weight status.
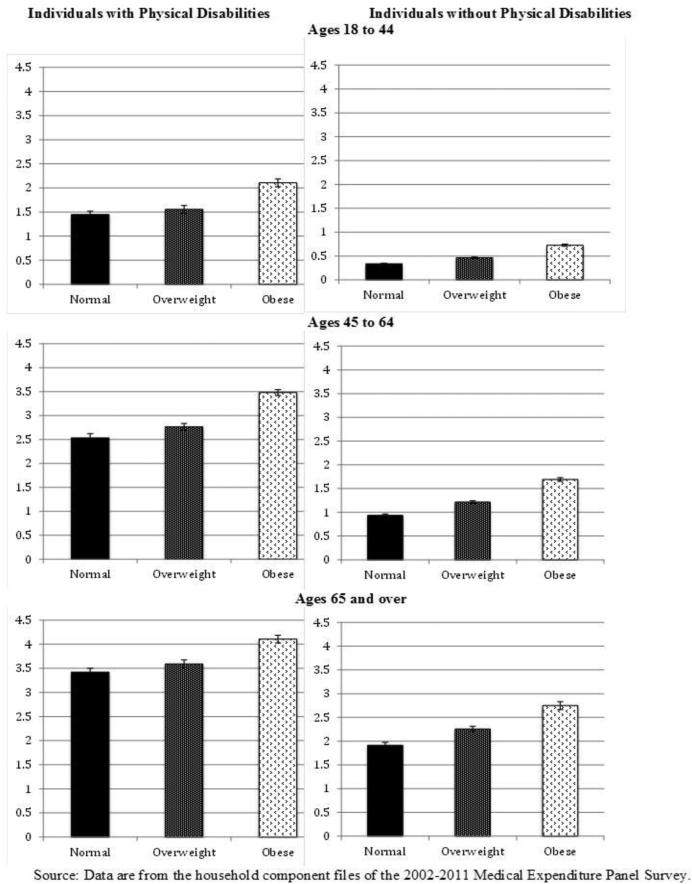
Figure 1 shows the average number of certain chronic conditions, stratified by age, PD status, and weight categories, including type 2 diabetes, asthma, arthritis, joint pain, emphysema, cardiovascular disease, heart attack, angina, and other cardiovascular conditions such as stroke and hypertension. Adults with PDs had a significantly greater age-stratified prevalence of all chronic conditions compared to adults without PDs. Moreover, the average number of all chronic conditions was higher among obese versus normal-weight adults, regardless of disability status.
Figure 1.
Average number of various comorbidities, stratified by age, physical disability status, and BMI category.
Discussion
Among >215,000 adults, 17% reported a significant PD. As compared to adults without PDs, adults with PDs also had significantly higher prevalence of obesity, less education, and lower household income. Although each of these factors individually represents a substantial burden to national health care, these data provide new evidence to confirm the exaggerated burden of PDs plus obesity. The primary finding of this study was that in comparison to adults without PDs, adults with PDs had significantly higher healthcare costs and overall utilization across all weight categories. Moreover, this study confirmed previous work that healthcare utilization and costs were greater among obese individuals compared with normal-weight individuals. However, obese individuals with PDs experienced the largest healthcare costs and utilization compared with all other investigated categories.
Among adults with PDs, the unadjusted healthcare costs were four times greater than those without PDs, and this was coincident with significantly greater frequency of medical provider office visits and hospitalization. However, because age, race, education, and SES were each associated with obesity status, disability status, and overall healthcare utilization, they were all adjusted in the final models. Interestingly, it was the PD status that accounted for the greatest proportion of increased healthcare utilization, as costs associated with PDs were >95% higher than non-physically disabled adults, regardless of BMI; whereas, costs associated with obesity were only 13% greater than normal weight status, regardless of disability status (Table 4). Likewise, both hospitalization and number of nights in the hospital were similar across weight categories, whereas there was substantially greater hospitalization among persons with PDs regardless of BMI. Based on these adjusted predictions, the healthcare utilization from adults with PDs that are obese represents nearly 50% of the total annual medical costs attributed to obesity in the U.S. (Appendix Table 6)—a staggering finding considering that this small subset of individuals corresponds to approximately 7% of the total population. As with all cross-sectional investigations, a limitation of this study is the inability to unravel the cause–effect relationship between predictors and outcomes. Indeed, whether the presence of PDs “causes” an increased risk for obesity and healthcare utilization, or if obesity itself is a contributing factor leading to progressive physical dysfunction and greater reliance on health care (i.e., reverse causality), is an interesting and complex topic. Findings do, however, support the independent contributions of PDs, and especially PDs plus obesity, to exponentiation of healthcare utilization. Nevertheless, future studies are certainly needed to examine the longitudinal changes in weight status and healthcare utilization among populations with disabilities. Research is also needed to better describe the trajectory of changes in physical function among adults without a specific congenital, acquired, or chronic disability who become obese.
The differences in costs may have been driven by the greater frequency of office visits among the adults with PDs, which may likely have been a direct consequence of increased chronic conditions in this population. In many cases, the adults with PDs that were normal weight had a greater number of chronic conditions than even the obese adults without PDs. There are several potential explanations for this. First, BMI lacks sensitivity to identify non-obese individuals with excess body fat.29 Many individuals with chronic PDs have altered growth and distribution of adiposity, as well as premature musculoskeletal frailty. As a result, such individuals may have a lower BMI, and yet still have excessive body fat or high risk for chronic diseases.30 The authors31 have recently shown that among adults with mobility impairments, standard BMI cutoffs had excellent specificity to screen for low body fat in both men and women, but sensitivity to detect excessive adiposity was poor. Therefore, because BMI was used in the current study to categorize weight status, it is plausible that many of the individuals with PDs that were classified as “normal weight” or even “overweight” had higher adiposity than adults without PDs.
It is also possible that lack of regular physical activity may have mediated these differences, as sedentary behavior is a well-known predictor of and consequence stemming from both obesity and physical comorbidities.32 Among adults with PDs, nearly 25% fewer reported regular exercise participation than adults without PDs. Although self-reported physical activity is prone to recall bias, it is commonly used as a covariate in large epidemiologic studies and clinical trials, as it is a robust underlying behavioral predictor of health, disease, and all-cause mortality.33,34 The authors31 have also recently demonstrated that mobility-impaired individuals do spend a significantly greater proportion of time in sedentary behavior, and less time participating in physical activity. It is thus possible that chronic physical inactivity and musculoskeletal deterioration may be primary drivers of increased healthcare utilization among adults with PDs, rather than the disproportionately higher prevalence of obesity in this population. However, another limitation that must be considered pertains to the method by which individuals were classified as having a physical disability. By using a self-reported physical function questionnaire, individuals did not report any specific diagnostic disability category per se, but rather the presence/absence of mobility restrictions or physical function. This and similar surveys have been used in the literature35,36 and are clinically relevant for identifying predictors of PDs and frailty. As inclusion was not limited to older adults, it is plausible that many individuals categorized as having a PD were for reasons directly attributable to high body mass (i.e., lending to general movement difficulties). Similarly, it is also possible that arthritis and stroke may have been a primary cause for PD status in some subjects, and thus partially explains the higher prevalence of these two chronic conditions in the subjects with PDs.
Understanding the longitudinal influences of excess adiposity on healthcare utilization, in specific diagnostic disability categories, would provide much-needed information for identifying cost-effective preventive/treatment options. Moreover, a better grasp of the etiology and temporal sequence of general age-related functional decline, obesity, and cardiometabolic outcomes would dramatically improve early risk screening and stratification. Regardless, there is a dire need for more patient-specific clinical studies to identify optimal interventions that may concurrently target preserving physical function and achieving or maintaining healthy weight. Because regular exercise and drug interventions are similar in terms of their mortality benefits in the secondary prevention of heart disease, rehabilitation after stroke, treatment of heart failure, and prevention of diabetes,34 a simplistic clinical directive that could dramatically reduce total healthcare utilization is to continue encouraging healthy lifestyles that lead to increases in physical activity and healthy weight achievement/maintenance.
Recent evidence has demonstrated that insurance coverage plays a significant role in explaining the receipt of preventive services, which is largely mediated by low education and SES.37 The current findings revealed that adults with PDs had less formal education and significantly lower income. Thus, by expanding health insurance coverage and reducing cost sharing for preventive care, the Affordable Care Act may have a direct influence on increasing rates of preventive services among this population.
Conclusions
Obesity is associated with increased healthcare utilization, independent of age, race, education, and SES; however, there is a significantly greater burden among adults with PDs who are obese. This is likely due to the disproportionately higher prevalence of chronic conditions in this subpopulation and a greater need for routine office visits. PDs plus obesity represents $23.9 billion/year, or roughly 50% of the total annual costs attributable to obesity in the U.S. Future attempts to identify and support behavioral interventions that can address both healthy weight achievement/maintenance and functional independence among all adults are vital.
Supplementary Material
Acknowledgments
EM was supported by Advanced Rehabilitation Research Training award H133P090008, from the National Institute on Disability and Rehabilitation Research, U.S. Department of Education Office of Special Education and Rehabilitative Services. MDP is funded by the NIH (1KO1-HD074706).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Arterburn DE, Maciejewski ML, Tsevat J. Impact of morbid obesity on medical expenditures in adults. Int J Obes. 2005;29(3):334–339. doi: 10.1038/sj.ijo.0802896. http://dx.doi.org/10.1038/sj.ijo.0802896. [DOI] [PubMed] [Google Scholar]
- 2.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. http://dx.doi.org/10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 3.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–825. doi: 10.1016/S0140-6736(11)60814-3. http://dx.doi.org/10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 4.Grieve E, Fenwick E, Yang HC, Lean M. The disproportionate economic burden associated with severe and complicated obesity: a systematic review. Obesity reviews. 2013;14(11):883–894. doi: 10.1111/obr.12059. http://dx.doi.org/10.1111/obr.12059. [DOI] [PubMed] [Google Scholar]
- 5.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity. 2008;16(10):2323–2330. doi: 10.1038/oby.2008.351. http://dx.doi.org/10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]
- 6.Weil E, Wachterman M, McCarthy EP, et al. Obesity among adults with disabling conditions. JAMA. 2002;288(10):1265–1268. doi: 10.1001/jama.288.10.1265. http://dx.doi.org/10.1001/jama.288.10.1265. [DOI] [PubMed] [Google Scholar]
- 7.Rimmer JH, Wang E. Obesity prevalence among a group of Chicago residents with disabilities. Arch Phys Med Rehab. 2005;86(7):1461–1464. doi: 10.1016/j.apmr.2004.10.038. http://dx.doi.org/10.1016/j.apmr.2004.10.038. [DOI] [PubMed] [Google Scholar]
- 8.Bandini LG, Curtin C, Hamad C, Tybor DJ, Must A. Prevalence of overweight in children with developmental disorders in the continuous national health and nutrition examination survey (NHANES) 1999-2002. J Pediatr. 2005;146(6):738–743. doi: 10.1016/j.jpeds.2005.01.049. http://dx.doi.org/10.1016/j.jpeds.2005.01.049. [DOI] [PubMed] [Google Scholar]
- 9.Neter JE, Schokker DF, de Jong E, Renders CM, Seidell JC, Visscher TLS. The Prevalence of Overweight and Obesity and Its Determinants in Children with and without Disabilities. J Pediatr. 2011;158(5):735–739. doi: 10.1016/j.jpeds.2010.10.039. http://dx.doi.org/10.1016/j.jpeds.2010.10.039. [DOI] [PubMed] [Google Scholar]
- 10.IOM . The Future of Disability in America. Institute of Medicine; Washington: 2007. [Google Scholar]
- 11.Anderson WL, Wiener JM, Finkelstein EA, Armour BS. Estimates of National Health Care Expenditures Associated With Disability. J Disabil Policy Stu. 2011;21(4):230–240. http://dx.doi.org/10.1177/1044207310391407. [Google Scholar]
- 12.Anderson WL, Armour BS, Finkelstein EA, Wiener JM. Estimates of state-level health-care expenditures associated with disability. Public health rep. 2010;125(1):44–51. doi: 10.1177/003335491012500107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rimmer JH, Schiller W, Chen MD. Effects of disability-associated low energy expenditure deconditioning syndrome. Exerc sport sci rev. 2012;40(1):22–29. doi: 10.1097/JES.0b013e31823b8b82. http://dx.doi.org/10.1097/JES.0b013e31823b8b82. [DOI] [PubMed] [Google Scholar]
- 14.Walter S, Kunst A, Mackenbach J, Hofman A, Tiemeier H. Mortality and disability: the effect of overweight and obesity. Int J Obes. 2009;33(12):1410–1418. doi: 10.1038/ijo.2009.176. http://dx.doi.org/10.1038/ijo.2009.176. [DOI] [PubMed] [Google Scholar]
- 15.Alley DE, Chang VW. The changing relationship of obesity and disability, 1988-2004. JAMA. 2007;298(17):2020–2027. doi: 10.1001/jama.298.17.2020. http://dx.doi.org/10.1001/jama.298.17.2020. [DOI] [PubMed] [Google Scholar]
- 16.Rillamas-Sun E, Lacroix A, Waring M, et al. Obesity and Late-Age Survival Without Major Disease or Disability in Older Women. JAMA Intern Med. 2014;174(1):98–106. doi: 10.1001/jamainternmed.2013.12051. http://dx.doi.org/10.1001/jamainternmed.2013.12051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson WL, Wiener JM, Khatutsky G, Armour BS. Obesity and people with disabilities: The implications for health care expenditures. Obesity. 2013;21(12):E798–E804. doi: 10.1002/oby.20531. http://dx.doi.org/10.1002/oby.20531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen JW, Monheit AC, Beauregard KM, et al. The Medical Expenditure Panel Survey: a national health information resource. Inquiry. 1997;33(4):373–389. [PubMed] [Google Scholar]
- 19.Flegal KM, Graubard BI, Williamson DF, Cooper RS. Reverse causation and illness-related weight loss in observational studies of body weight and mortality. Am J Epidemiol. 2011;173(1):1–9. doi: 10.1093/aje/kwq341. http://dx.doi.org/10.1093/aje/kwq341. [DOI] [PubMed] [Google Scholar]
- 20.AHRQ MEPS HC-050: Full Year Consolidated Data File. 2000 www.meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h50/h50doc.pdf.
- 21.AHRQ MEPS HC-113: Full Year Consolidated Data File. 2007 www.meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h113/h113doc.pdf.
- 22.Cohen SB. Design strategies and innovations in the Medical Expenditure Panel Survey. Med Care. 2003;41(7 Suppl):III5–III12. doi: 10.1097/01.MLR.0000076048.11549.71. [DOI] [PubMed] [Google Scholar]
- 23.Andersen R. A behavioral model of families' use of health services. Center for Health Administration Studies, University of Chicago; Chicago: 1968. [Google Scholar]
- 24.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. http://dx.doi.org/10.2307/2137284. [PubMed] [Google Scholar]
- 25.McCullagh P, Nelder JA. Generalized linear models. Chapman & Hall/CRC; 1989. http://dx.doi.org/10.1007/978-1-4899-3242-6. [Google Scholar]
- 26.Park RE. Estimation with heteroscedastic error terms. Econometrica. 1966;34(4):888. http://dx.doi.org/10.2307/1910108. [Google Scholar]
- 27.Deb P, Manning W, Norton E. Preconference Course: Modeling Health Care Costs and Counts. 2010 http://www.ispor.org/OpenSourceIndex/cached/Modeling_Health_Care_Costs_and_Use_Files/ASHE2010_Minicourse_Cost_Use_slides.pdf.
- 28.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J health econ. 2001;20(4):461–494. doi: 10.1016/s0167-6296(01)00086-8. http://dx.doi.org/10.1016/S0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 29.Okorodudu DO, Jumean MF, Montori VM, et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. Int J Obes. 2012;34(5):791–799. doi: 10.1038/ijo.2010.5. http://dx.doi.org/10.1038/ijo.2010.5. [DOI] [PubMed] [Google Scholar]
- 30.Romero-Corral A, Somers VK, Sierra-Johnson J, et al. Normal weight obesity: a risk factor for cardiometabolic dysregulation and cardiovascular mortality. Eur Heart J. 2010;31(6):737–746. doi: 10.1093/eurheartj/ehp487. http://dx.doi.org/10.1093/eurheartj/ehp487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peterson M, Al Snih S, Stoddard J, Shekar A, Hurvitz E. Obesity Misclassification and the Metabolic Syndrome in Adults with Functional Mobility Impairments: NHANES 2003-2006. Prev Med. 2014;60:71–76. doi: 10.1016/j.ypmed.2013.12.014. http://dx.doi.org/10.1016/j.ypmed.2013.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amati F, Dube JJ, Coen PM, Stefanovic-Racic M, Toledo FG, Goodpaster BH. Physical inactivity and obesity underlie the insulin resistance of aging. Diabetes Care. 2009;32(8):1547–1549. doi: 10.2337/dc09-0267. http://dx.doi.org/10.2337/dc09-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A. Sitting time and all-cause mortality risk in 222 497 Australian adults. JAMA Intern Med. 2012;172(6):494–500. doi: 10.1001/archinternmed.2011.2174. http://dx.doi.org/10.1001/archinternmed.2011.2174. [DOI] [PubMed] [Google Scholar]
- 34.Naci H, Ioannidis JPA. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ. 2013;347:f5577. doi: 10.1136/bmj.f5577. http://dx.doi.org/10.1136/bmj.f5577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alley DE, Chang VW. The changing relationship of obesity and disability, 1988-2004. JAMA. 2007;298(17):2020–2027. doi: 10.1001/jama.298.17.2020. http://dx.doi.org/10.1001/jama.298.17.2020. [DOI] [PubMed] [Google Scholar]
- 36.Davison KK, Ford ES, Cogswell ME, Dietz WH. Percentage of body fat and body mass index are associated with mobility limitations in people aged 70 and older from NHANES III. J Am Geriatr Soc. 2002;50(11):1802–1809. doi: 10.1046/j.1532-5415.2002.50508.x. http://dx.doi.org/10.1046/j.1532-5415.2002.50508.x. [DOI] [PubMed] [Google Scholar]
- 37.McMorrow S, Kenney GM, Goin D. Determinants of Receipt of Recommended Preventive Services: Implications for the Affordable Care Act. Am J Public Health. 2014 doi: 10.2105/AJPH.2013.301569. [epub] http://dx.doi.org/10.2105/AJPH.2013.301569. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.