Abstract
We sought to determine if childhood wrist circumference predicts insulin resistance in adulthood. Measures were taken in pre-pubertal children and then approximately 30 years later in the same subjects as adults. Our findings suggest that wrist circumference in childhood is not a predictor of insulin resistance in adulthood.
Keywords: Obesity, Children, Adults, Insulin, Insulin resistance, Wrist
The gold standard measurement of insulin resistance (IR), the euglycemic, hyperinsulinemic clamp (Mlbm),1,2 is technically challenging, invasive, and expensive, limiting its clinical usefulness. Surrogate measures of IR including fasting insulin and the homeostasis model assessment of IR (HOMA-IR)3 require a blood sample, show only moderate correlation with direct measures of IR in children,2 and vary greatly among laboratories.4 A non-invasive screening tool easy to perform in the office that provides an acceptable estimate of IR risk is needed.
It has been proposed that wrist circumference (WrC) may be a good surrogate in children as a simple, non-invasive marker of IR.5 A close cross-sectional relationship between pediatric WrC and HOMA-IR has been reported in overweight youth,5 and supported by recent findings that wrist breadth was associated with HOMA-IR in normal-weight children.6
We hypothesized that childhood WrC would positively predict adult IR as measured by euglycemic hyperinsulinemic clamp. We also assessed HOMA-IR to provide a direct comparison to the previous cross-sectional studies.
Methods
The University of Minnesota Institutional Review Board approved the research. All parents and subjects provided informed consent and assent, respectively. A previously-established cohort was used.7 Subjects were excluded if: body mass index (BMI) and WrC measurements in childhood were obtained greater than six months apart (n=75), age data discrepant (n=5), or IR data not available (n=41). The final cohort included 275 individuals.
Height and weight were measured, and BMI (kg/m2) and BMI-percentile were calculated.8 WrC was measured on the right wrist immediately proximal to the ulnar and radial epicondyles to the nearest 0.5 cm by trained technicians.7
Adult testing was conducted at the University of Minnesota Clinical Research Center after a 10-hour fast. Height and weight were measured, and BMI was calculated. Waist circumference was measured to the nearest 0.5 cm. Body fat percent, fat mass, lean mass, and bone mineral density were determined by dual energy X-ray absorptiometry (Lunar Prodigy, General Electric Medical Systems, Madison, WI, USA). All scans were analyzed using General Electric Medical Systems enCore™ software platform version 10.5. IR was measured by euglycemic hyperinsulinemic clamp as previously described.9 IR was expressed as the glucose infusion rate (mg/kg/min of glucose), adjusting for lean mass (Mlbm). A lower Mlbm indicates greater IR. Glucose and insulin were measured using standard procedures. HOMA-IR was calculated as previously described.3
Statistical Analyses
Stata/SE 12.0 (StataCorp, College Station, TX, USA) was used for statistical analyses. Results are expressed as mean±standard error of the mean. An independent t-test was used to compare demographic characteristics. Stepwise multivariate linear regression (backward elimination, P=0.05) was used to identify the best predictor of Mlbm and HOMA-IR from childhood WrC, sex, BMI-percentile, and height. Weight and BMI were not included due to concerns about multicollinearity. HOMA-IR data were logarithmically transformed. Spearman correlation was used to evaluate relationships between WrC and adulthood height, weight, BMI, percent fat mass, fat mass, lean mass, bone mineral density, waist circumference, fasting glucose, fasting insulin, log HOMA-IR, and Mlbm. Statistical significance was determined at the 0.05 level.
Results
Data from childhood and adulthood are shown in the Table. Childhood WrC correlated with childhood age (ρ=0.175, P=0.004), height (ρ=0.557, P<0.001), weight (ρ=0.812, P<0.001), BMI (ρ=0.778, P<0.001), BMI-percentile (ρ=0.752, P<0.001), and BMI category (ρ=0.606, P<0.001).
Table 1. Demographic and Clinical Characteristics.
| Mean(±SEM) | |
|---|---|
| Sex (% Male) | 54.9% (151 male) |
| Race: n (%) | |
| 1 – White | 196 (71.3%) |
| 2 – African American | 49 (17.8%) |
| 3 – Other | 30 (10.9%) |
| In Childhood | |
| Age (yrs) | 8.4±0.05 |
| Height (cm) | 129.3±0.4 |
| Weight (kg) | 27.4±0.3 |
| BMI (kg/m2) | 16.2±0.1 |
| BMI Percentile | 48.9±1.7 |
| Underweight (%) | 6.5 |
| Normal (%) | 80 |
| Overweight (%) | 10.2 |
| Obese (%) | 3.3 |
| Wrist Circumference (cm) | 13.3±0.1 |
| In Adulthood | |
| Age (yrs) | 39.0±0.1 |
| Height (cm) | 172.4±0.7 |
| Weight (kg) | 85.4±1.2 |
| BMI (kg/m2) | 25.5±0.4 |
| Underweight (%) | 3.3 |
| Normal (%) | 49.8 |
| Overweight (%) | 25.1 |
| Obese (%) | 21.8 |
| Fat Mass (%) | 34.6±0.6 |
| Fat Mass (kg) | 29.2±0.8 |
| Lean Mass (kg) | 52.5±0.7 |
| Waist Circumference (cm) | 97.5±1.0 |
| Bone Mineral Density (z-score) | 1.3±0.01 |
| Fasting Glucose (mmol/L) | 5.0±0.04 |
| Fasting Insulin (mU/L) | 8.7±0.6 |
| HOMA-IR | 2.0±0.2 |
| Mlbm (mg/kg/minute) | 11.9±0.3 |
BMI, body mass index; BMI percentile determined using the 2000 CDC Growth Charts9; HOMA-IR, Homeostasis Model for Assessment–Insulin Resistance; Mlbm, insulin resistance adjusted for lean body mass.
Childhood weight (ρ=0.125, P=0.039) and BMI-percentile (ρ=0.120, P=0.048) correlated with adult HOMA-IR, whereas other childhood variables did not (race: P=0.093; height: P=0.088; BMI: P=0.078; WrC: P=0.177). No childhood measures correlated with adult Mlbm (race: P=0.513; height: P=0.700; weight: P=0.270; BMI: P=0.257; BMI-percentile: P=0.229; WrC: P=0.051).
Childhood BMI-percentile predicted adult HOMA-IR (β=0.004, P=0.033), but not Mlbm (P=0.653). When analyzed by sex, childhood BMI-percentile no longer predicted HOMA-IR. Childhood WrC correlated with adult height (ρ=0.274, P<0.001), weight (ρ=0.436, P<0.001), BMI (ρ=-0.444, P<0.001), bone mineral density (ρ=0.393, P<0.001), waist circumference (ρ=0.336, P<0.001), fat mass (ρ=0.306, P<0.001), lean mass (ρ=0.414, P<0.001), and fasting glucose (ρ=0.163, P=0.007), but not percent fat mass (P=0.083) or fasting insulin (P=0.259).
Childhood WrC did not predict adult IR as measured by Mlbm (P=0.575) or HOMA-IR (P=0.426). The correlations of childhood WrC with adult log HOMA-IR and Mlbm are shown in the Figure. No sex differences were observed for the relations between WrC and Mlbm or HOMA-IR. WrC did not predict Mlbm or HOMA-IR for any child BMI category; however, the P-value for WrC and Mlbm in the overweight category was marginal but not significant (P=0.068).
Figure 1.
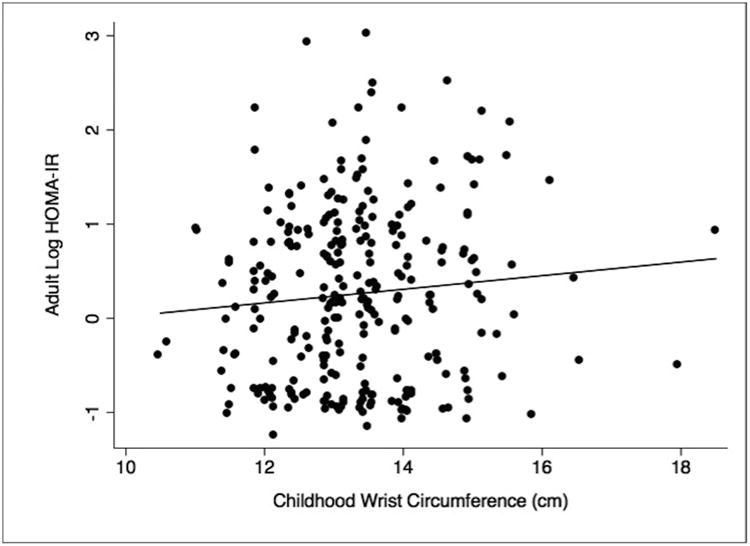
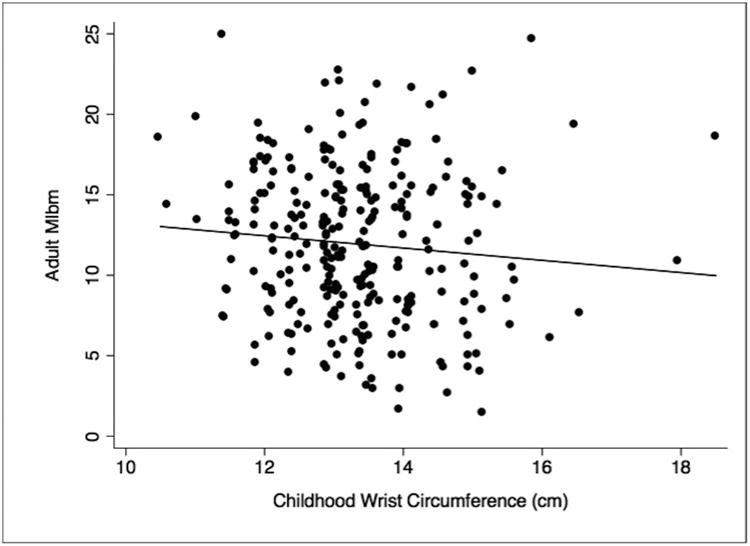
Correlation of child WrC and adult insulin resistance as measured by A, log HOMA-IR (ρ=0.082, P=0.177; higher log HOMA-IR indicates greater insulin resistance), and B, Mlbm (ρ=-0.118, P=0.051; lower Mlbm indicates greater insulin resistance). A jitter of 4 was applied to avoid point overlap.
Discussion
In a previous study5 reporting a positive correlation between WrC and HOMA-IR in childhood, the authors explained this relationship by hypothesizing that bone diameter might increase with increasing IR. A compensatory increase in insulin secretion is typical with IR.10 Insulin overproduction has been linked with increased bone formation,11,12 likely mediated by insulin-like growth factor 1 (IGF-1).13-15 IGF-1 levels have been linked with bone cross-sectional area,17 and WrC provides a view of bone formation18,19 that is minimally affected by fat deposition.20 Adult WrC has been shown to predict diabetes, even after controlling for BMI and waist circumference,21 indicating that a larger WrC may become a predictor of IR later in life. In the current study, childhood WrC was related to childhood age, height, weight, BMI, BMI-percentile, and BMI category, but did not predict adult IR.
Direct comparisons with the prior report in children5 were not possible due to three important differences. The prior study was cross-sectional, a high proportion of children were overweight/obese (in the current study they were normal weight), and used HOMA-IR (the current study used a direct measure of IR [Mlbm]).
In the current study, none of the childhood anthropometric variables (BMI-percentile, height, weight, or WrC) correlated with adult IR measured by Mlbm. Although childhood BMI-percentile was a predictor of HOMA-IR, when analyzed by sex, BMI-percentile was no longer significant.
Limitations of the current study include the single time point for WrC assessment in childhood and for IR in adulthood, precluding analyses of these correlations in the two age groups, as well as of their tracking into adulthood. It is conceivable that WrC might be associated with child lean body mass, however, in the absence of body composition measurements in children, this could not be assessed. Finally, although separating by sex or BMI-percentile did not yield significant results, this may be related to power limitations of each category size.
Acknowledgments
Funded by the National Institutes of Health (NIH)/National Institute of Diabetes and Digestive and Kidney Diseases (R01DK072124 [to J.S.]), the GCRC (M01-RR00400), General Clinical Research Center Program, National Center for Research Resources/NIH, and Clinical and Translational Science Institute NIH/National Center for Advancing Translational Science (UL1TR000114).
Abbreviations
- BMI
body mass index
- HOMA-IR
homeostasis model assessment of insulin resistance
- IGF-1
insulin-like growth factor 1
- IR
insulin resistance
- Mlbm
insulin-stimulated glucose uptake = insulin sensitivity/resistance (clamp method)
- WrC
wrist circumference
Footnotes
Portions of the study were presented as a poster at the North American Society for Pediatric Exercise Medicine conference, xx, August x, 2014.
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ferrannini E, Mari A. How to measure insulin sensitivity. J Hypertens. 1998;16:895–906. doi: 10.1097/00004872-199816070-00001. [DOI] [PubMed] [Google Scholar]
- 2.Schwartz B, Jacobs DR, Moran A, Steinberger J, Hong CP, Sinaiko AR. Measurement of insulin sensitivity in children: comparison between the euglycemic-hyperinsulinemic clamp and surrogate measures. Diabetes Care. 2008;31:783–8. doi: 10.2337/dc07-1376. [DOI] [PubMed] [Google Scholar]
- 3.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 4.Robbins DC, Andersen L, Bowsher R, Chance R, Dinesen B, Frank B, et al. Report of the American Diabetes Association's Task Force on standardization of the insulin assay. Diabetes. 1996;45:242–56. doi: 10.2337/diab.45.2.242. [DOI] [PubMed] [Google Scholar]
- 5.Capizzi M, Leto G, Petrone A, Zampetti S, Papa RE, Osimani M, et al. (2011). Wrist circumference is a clinical marker of insulin resistance in overweight and obese children and adolescents. Circulation. 2011;123:1757–62. doi: 10.1161/CIRCULATIONAHA.110.012898. [DOI] [PubMed] [Google Scholar]
- 6.Mueller NT, Johnson W, Odegaard AO, Lee M, Czerwinski SA, Demerath EW. Wrist breadth and homeostasis model assessment of insulin resistance in youth: the Fels Longitudinal Study. Am J Hum Biol. 2013;25:581–5. doi: 10.1002/ajhb.22416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prineas RJ, Gillum RF, Horibe H, Hannan PJ. The Minneapolis Children's Blood Pressure Study. Part 1: standards of measurement for children's blood pressure. Hypertension. 1980;2:I18. doi: 10.1161/01.hyp.2.4_pt_2.i18. [DOI] [PubMed] [Google Scholar]
- 8.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002:1–190. [PubMed] [Google Scholar]
- 9.Sinaiko AR, Jacobs DR, Jr, Steinberger J, Moran A, Luepker R, Rocchini AP, et al. Insulin resistance syndrome in childhood: associations of the euglycemic insulin clamp and fasting insulin with fatness and other risk factors. J Pediatr. 2001;139:700–7. doi: 10.1067/mpd.2001.118535. [DOI] [PubMed] [Google Scholar]
- 10.Kahn SE, Prigeon RL, McCulloch DK, Boyko EJ, Bergman RN, Schwartz MW, et al. Quantification of the relationship between insulin sensitivity and β-cell function in human subjects: evidence for a hyperbolic function. Diabetes. 1993;42:1663–72. doi: 10.2337/diab.42.11.1663. [DOI] [PubMed] [Google Scholar]
- 11.Stolk RP, Van Daele PLA, Pols HAP, Burger H, Hofman A, Birkenhäger JC, et al. Hyperinsulinemia and bone mineral density in an elderly population: The Rotterdam Study. Bone. 1996;18:545–9. doi: 10.1016/8756-3282(96)00079-8. [DOI] [PubMed] [Google Scholar]
- 12.Kinjo M, Setoguchi S, Solomon DH. Bone mineral density in adults with the metabolic syndrome: analysis in a population-based US sample. J Clin Endocrinol Metab. 2007;92:4161–4. doi: 10.1210/jc.2007-0757. [DOI] [PubMed] [Google Scholar]
- 13.Thomas DM, Udagawa N, Hards DK, Quinn JM, Moseley JM, Findlay DM, et al. Insulin receptor expression in primary and cultured osteoclast-like cells. Bone. 1998;23:181–6. doi: 10.1016/s8756-3282(98)00095-7. [DOI] [PubMed] [Google Scholar]
- 14.Ferron M, Wei J, Yoshizawa T, Del Fattore A, DePinho RA, Teti A, et al. Insulin signaling in osteoblasts integrates bone remodeling and energy metabolism. Cell. 2010;142:296–308. doi: 10.1016/j.cell.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fulzele K, Riddle RC, DiGirolamo DJ, Cao X, Wan C, Chen D, et al. Insulin receptor signaling in osteoblasts regulates postnatal bone acquisition and body composition. Cell. 2010;142:309–19. doi: 10.1016/j.cell.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Polgreen LE, Jacobs DR, Nathan BM, Steinberger J, Moran A, Sinaiko AR. Association of osteocalcin with obesity, insulin resistance, and cardiovascular risk factors in young adults. Obesity. 2012;20:2194–201. doi: 10.1038/oby.2012.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mora S, Pitukcheewanont P, Nelson JC, Gilsanz V. Serum levels of insulin-like growth factor I and the density, volume, and cross-sectional area of cortical bone in children. J Clin Endocrinol Metab. 1999;84:2780–3. doi: 10.1210/jcem.84.8.5874. [DOI] [PubMed] [Google Scholar]
- 18.Grant JP, Custer PB, Thurlow J. Current techniques of nutritional assessment. Surg Clin North Am. 1981;61:437. doi: 10.1016/s0039-6109(16)42430-8. [DOI] [PubMed] [Google Scholar]
- 19.Miller JZ, Slemenda CW, Meaney FJ, Reister TK, Hui S, Johnston CC. The relationship of bone mineral density and anthropometric variables in healthy male and female children. Bone Miner. 1991;14:137–52. doi: 10.1016/0169-6009(91)90091-d. [DOI] [PubMed] [Google Scholar]
- 20.Ferrante E, Pitzalis G, Deganello F, Galastri E, Sciarpelletti R, Imperato C. The evaluation of body composition in children by anthropometry and impedance measurement. Minerva Pediatr. 1993;45:289. [PubMed] [Google Scholar]
- 21.Noudeh YJ, Hadaegh F, Vatankhah N, Momenan AA, Saadat N, Khalili D, et al. Wrist circumference as a novel predictor of diabetes and prediabetes: results of cross-sectional and 8.8-year follow-up studies. J Clin Endocrinol Metab. 2013;98:777–84. doi: 10.1210/jc.2012-2416. [DOI] [PubMed] [Google Scholar]


