Abstract
Complex hierarchical organization is a hallmark of tissues and their subsequent integration into organs. A major challenge in tissue engineering is to generate arrays of cells with defined structural organization that display appropriate functional properties. Given what is known about cellular responses to physiochemical cues from the surrounding environment, we can build tissue structures that mimic these microenvironments and validate these platforms using both experimental and computational approaches. Tissue generation encompasses many methods and tissue types, but here we review layering cell sheets to create scaffold-less myocardial patches. We discuss surgical criteria that can drive the design of myocardial cell sheets and the methods used to fabricate, mechanically condition, and functionally test them. We also focus on how computational and experimental approaches could be integrated to optimize tissue mechanical properties by using measurements of biomechanical properties and tissue anisotropy to create predictive computational models. Tissue anisotropy and dynamic mechanical stimuli affect cell phenotype in terms of protein expression and secretion, which in turn, leads to compositional and structural changes that ultimately impact tissue function. Therefore, a combinatorial approach of design, fabrication, testing, and modeling can be carried out iteratively to optimize engineered tissue function.
Keywords: cellular sheets, cardiac regeneration, computational modeling, biomechanical properties
Introduction
Tissues represent specialized collections of cells and cell products that are spatially arranged to carry out precise biological functions. At the cellular level, tissues are regulated by biochemical and mechanical cues present within the surrounding microenvironment; however, it is the tissue structure hierarchical organization that dictates its overall function.9, 33 With normal aging, onset of disease, or direct injury, tissue structure organization may become compromised, impairing organ function. Extensive loss of tissue structure and function or ineffective repair may jeopardize the organism’s ability to recover or even survive. As seen by persistent mortality rates due to cardiovascular disease, the heart is one organ where loss of tissue structure and function is often detrimental to the organism’s survival.17
Currently, the most widely used and readily available surgical solutions for repairing damaged cardiac tissue apply synthetic patch materials, such as Dacron (polyethylene terephthalate or PET) and Gore-Tex (expanded-polytetrafluoroethylene or ePTFE), or naturally occurring materials such as autologous, allogeneic, and xenogeneic pericardium.65 Despite limiting immune responses, these materials do little to promote cardiac regeneration, strengthen damaged tissue, or grow/remodel as the native tissue changes; the mechanical mismatch in compliance may even cause maladaptive remodeling. Ideally, patch implantations would be non-thrombogenic, have long-term durability, resist infections, and directly reinforce the surrounding tissue via rapid incorporation and growth; patches would also be designed to release paracrine signals that activate cardiac progenitor cells that could aid in the repair and vascularization of the injured tissue.38
In recent years, several scaffold and scaffold-less approaches to generate cell-based therapeutic patches for replacing damaged or diseased tissues have been explored. Although recent improvements in biomaterials and cellular science have advanced our understanding and aided design, developing three-dimensional, vascularized tissues for implantation still remains a significant challenge. The ultimate goals of myocardial patch engineering are to mimic tissue natural organization using living cells, and to produce viable structures amenable to mechanical, electrical, and functional integration with the surrounding viable tissue.21, 23, 25 Electrical coupling is essential to cardiac function; however, this review will focus only on mechanical aspects of tissue integration. Although devices such as pacemakers are available to synchronize cardiac tissue, a clinically viable option to regenerate myocardium with the proper mechanical properties to pump blood is still beyond our reach.
To study tissue mechanics, we focus on bottom-up approaches that enable direct control of hierarchical tissue organization in a layer-by-layer fashion such that the end-result consists solely of cells and associated extracellular matrix (ECM) in scaffold-less constructs. While we focus on scaffold-less approaches, synthetic and natural biomaterial scaffolds with a wide variety of biological and chemical properties have been reviewed extensively elsewhere.49 However, patch designs that require scaffolding for cell seeding commonly are not able to adapt to patient growth following surgical implantation, a property important for long-term functionality in most patients. Implanted patches that are similar to healthy tissue at the target site are more likely to incorporate successfully. In addition, because many polymeric scaffolding biomaterials may elicit undesirable inflammation reactions from polymer degradation,19 attention has turned to cell sheet technology to engineer scaffold-less tissues.10, 66 Pioneering this technology, the Okano group enabled the development of a three-dimensional, scaffold-less, completely cellular-based regenerative patch.75 In collaboration with the Okano group, our group was the first to fabricate cell sheets with variable cell alignment patterns,30, 71 different cell types, and different structural and mechanical properties, which can subsequently be layered and stacked together in arrangements that recapitulate native structures without requiring synthetic scaffold implantation. Selecting an appropriate cell type is critical for creating a successful patch. Various cell sources, including commercially available cell lines and freshly isolated primary cell cultures, have been incorporated depending on the intended application. For myocardial tissue replacement, these cell types include endothelial, cardiomyocyte, vascular smooth muscle (VSMCs), and cardiac fibroblasts.74 Several new cardiac progenitor cell sources are currently being investigated for their cardiac regenerative potential as well.12, 44 Recently, human embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) have played a more prominent role in tissue engineering applications as these cells can self-renew and have the potential to differentiate into multiple cell lineages. However an important aspect to consider when envisaging in vivo applications is that undifferentiated cells may circulate away from the targeted tissue and form teratomas.6, 7, 37 Overall, clinical attempts at direct cell injections have had limited success at precisely delivering and retaining cells at the injury site.25 In contrast, a regenerative cardiac patch would confine cell delivery to the repair site.55 Indeed, even without thick and/or vascularized constructs, cardiac cell sheets of 3 stacked cell layers (~100 µm thick), implanted into damaged rat hearts promoted greater functional improvement and cell survival than dissociated cell injections.55
In this review, we focus on the fabrication of engineered tissue patches using cell sheet technology for the repair of myocardium and the surrounding vasculature. We particularly discuss how cell type, cellular organization within individual and stacked cell sheets, and the application of exogenous stressors (particularly mechanical conditioning) to a cell sheet may enhance overall tissue structure and function. We also cover how computational modeling can help prioritize the overwhelming number of design options by elucidating interrelationships between fabrication parameters, growth, and biochemical/mechanical properties. Although a complete, experimentally-validated, and useful computational model for myocardial patches does not currently exist, we have outlined the three tiered model structure our research group would ultimately like to build to aid in the design of our cell sheet tissue constructs. This would give us the ability to predict tissue function based on cellular patch structure; predictions regarding the mechanical properties of a fabricated three-dimensional tissue would be instrumental in designing patches tailored to specific patients in the clinical setting. Therefore, to begin the cell sheet modeling discussion, we start with the surgical priorities that should ultimately be driving patient specific patch design criteria before covering how the patches are actually fabricated and ideally modeled to meet these criteria.
Design Criteria Driven by Surgical Applications
Ideally, myocardial patches under development would be fabricated to meet design criteria set by surgeons and would work synergistically with the adjacent native tissue. Additionally, surgeons are also concerned with the technical process of implantation, which encompasses implant durability during handling, attachment at the site of repair, post-operative monitoring, and any need for additional surgical treatment. Ideally, correlations between resulting cardiac function and patch implantation can be made using both in vitro experimental data and patient specific clinical data such as ejection fraction and cardiac output. Iterating on the fabrication process optimizes patch performance, but we argue that computational modeling of these cellular systems can also provide important insights and predictions for initial fabrication and for post-operative concerns. Three main design criteria relevant to surgeons that should be driving this myocardial patch design, fabrication, and modeling include:
Mechanical Compatibility and Acute Performance: Myocardial “passive stiffness” is a major determinant of overall cardiac function,69 which makes it crucial to match mechanical properties of the patch and native tissue. The burst strength of the patch must be adequate to prevent rupture or bleeding around the patch as the heart beats. Furthermore, passive characteristics of the graft must be similar to the surrounding myocardium to avoid significant discrepancies in regional function. A computational model that predicts resulting patch moduli, tensile strength, and burst pressure based on cell sheet property inputs (e.g., cell type, alignment, number of layers) would allow surgeons to match patch stiffness to a patient’s resident tissue, as well as predict potential failure points post-implantation.3, 67
Technical Implantation: A relatively flexible tissue graft accommodates robust surgical handling and adjusts to irregularly shaped implantation areas. In addition, the graft must be able to hold sutures without tearing. A computational model that determines relative patch elasticity and maximum tensile strength for a sutured cell sheet could predict attachment failure or inform on the number of sutures necessary for successful implantation. In addition, as cell sheets adhere and integrate with neighboring cell layers in culture, cell sheet implants may significantly reduce the number of necessary attachment points.3
Long-Term Function, Durability, and Growth with Resident Tissues: The human heart approximately doubles in size from childhood to adulthood4, 61 and it beats on average 2.5 billion times in a lifetime, exposing an implanted patch to extreme cyclic fatigue.4, 61 As humans age, elasticity decreases and causes heart muscles to thicken and stiffen, which affects organ shape and function.4, 61 Therefore, the implanted patch must be capable of adapting and remodeling as the heart ages. Disproportionately increased growth may lead to aneurysm formation, whereas disproportionately decreased growth may lead to diastolic dysfunction. Cells within the patch must also integrate in synchronous contraction with the surrounding muscle to avoid reentry circuit arrhythmia. To protect graft cells from eventual apoptosis and necrosis, patch designs should also promote contractility-maintenance, perfusion, and appropriate wall tension. Attrition of cells with time from the patch may also lead to abnormal systolic function; thus, developing a patch with similar ECM to normal surrounding muscle may help to control cell behavior so that long-term desirable diastolic properties are achieved. Stacked cellular sheets already offer native-like ECM that is produced and deposited between sheets during in vitro culture.42 In addition, for both monolayer and stacked cell sheets, a computational model would be valuable to predict implant behavior and expectations on how mechanical conditioning will affect tissue growth and cyclic fatigue properties.
Building a predictive computational model requires integrative knowledge of monolayer and stacked cell sheet fabrication, conditioning, bio-mechanical properties and the graft-induced functional impact on host tissue.
Fabrication: Model Input Parameters
Monolayer Cell Sheets
Cell sheet engineering technologies most commonly utilize the temperature-responsive polymer poly(N-isopropylacrylamide) (P(NIPAAm)), which is a dense, hydrophobic film at 37°C that undergoes a reversible conformation change below 32°C to a swollen, hydrophilic state.46, 66, 75 Surfaces modified with P(NIPAAm) promote cell attachment and growth at cell culture temperatures, while lowering surfaces to room temperature promotes spontaneous, non-damaging cell detachment with preserved cell-cell contact and ECM. In this manner, cell sheets can be cultured and collected non-invasively, with each individual sheet serving as a functional unit that can be stacked to form a 3D tissue.
Other responsive systems, such as electro-, photo-, and pH-responsive, and magnetic systems, have been developed for cell sheet detachment and were recently reviewed extensively by Patel and Zhang.47 Additionally, our lab has also recently developed a method using a sacrificial substrate with tunable stiffness made from cellulose and alginate that allows for the controlled growth of aligned cell monolayers and the enzymatic release of an intact cell sheet (manuscript in preparation and patent submitted). However, the majority of cell sheet technologies incorporate P(NIPAAm), which will be the focus in this review.
The myocardium is a highly aligned network of cardiomyocytes, capillaries and interstitial fibroblasts. This structural alignment is critical for anisotropic contraction, and is under constant dynamic loading in vivo. Methods have been devised to mimic this native composition and structural organization in cell sheets, as well as increase the mechanical integrity of cell sheet monolayers.30, 35, 71, 72 Some approaches have used contact guidance or biochemical cues from adhesion proteins (e.g., fibronectin) to organize cell and tissue growth into monolayers of aligned cells.63, 71, 72 In our lab, we have used microgroove textured substrates to guide cell attachment in an aligned pattern. Mechanical testing of these cell sheets revealed mechanical anisotropy that was significantly larger in the direction of alignment, demonstrating that cellular structural organization can result in functional changes in macroscale material behavior.30 Patterned cell sheets that grow beyond ~20 µm thick become disorganized;48 in contrast, we showed with human mesenchymal stem cells that patterned sheets could increase in cell density over 2 weeks in culture and reach thicknesses of 13–15 µm without loss of patterning cues.72 We and others have since developed methods to use P(NIPAAm) on microtextured elastic substrates for creating harvestable aligned cell sheets.41, 62
Changing the compositional profile can also alter the material and structural behavior of tissues, and mechanical stress is a well-known regulator of protein and ECM gene expression.21, 22 To this end, Lee and von Recum modified a commercially available cell culture platform for mechanical conditioning with P(NIPAAm) copolymers such that cell sheets could be detached with conditioned cell-derived matrix intact.35 They subsequently demonstrated that cell sheets detached from their modified platform following conditioning promoted a significant increase in contractile protein expression in mouse cardiomyocytes.36
Stacked Cell Sheets
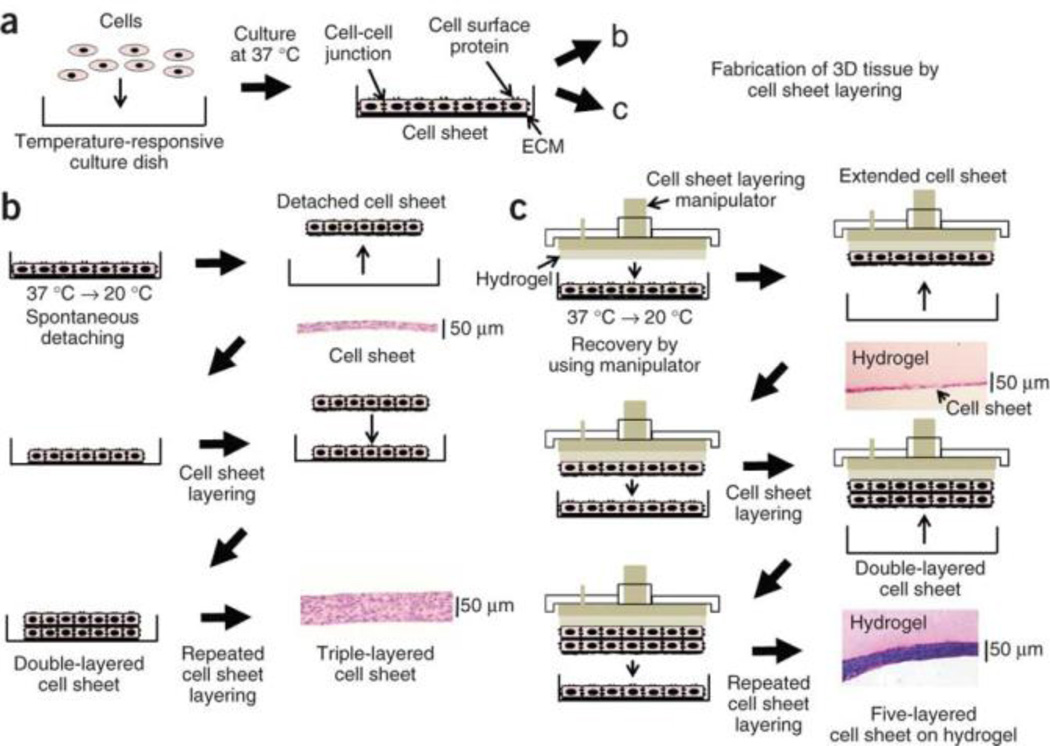
To form three-dimensional tissues out of individually fabricated cell sheets, the Okano group developed two main methods for stacking cellular sheets detached from P(NIPAAm) culture dishes: (1) simple pipetting and (2) using a hydrogel-coated plunger (Figure 1).24 In the pipetting method, cell sheets released from the substrate following temperature reduction are suctioned up into the pipette tip and re-deposited into a new dish; excess media is slowly drained to allow the sheet to open up and re-adsorb to the new surface. A second sheet can be detached, placed on top, and manipulated into position before it spontaneously adheres to the first sheet. With the hydrogel-coated plunger method, a sacrificial fibrin or gelatin gel is molded onto the surface of an acrylic resin plunger manipulator. The hydrogel surface of the manipulator can be placed onto the cell sheet surface where it adheres tightly to the cells, allowing the sheet to be recovered in its monolayer state without shrinkage. The plunger can be used to pick up as many cell sheets as desired before melting the hydrogel, which releases the cell sheet stack as a 3D tissue.24
Figure 1.
Two main methods for stacking cellular sheets after detachment from substrate. (a) After culturing of cells on temperature-responsive culture dish, they can be detached and stacked one of two ways: (b) simple pipette method or (c) hydrogel-coated plunger mechanism.
The beauty of cell sheet technology is that each monolayer can be uniquely patterned and seeded with a different cell type (as discussed above) to mimic the individual layers of native myocardium before stacking. Cell sheet technology preserves ECM, cell-cell junctions, and cell surface proteins; cell alignment within sheets in a stack can be preserved for two- and three-layered stacks of striated patterns with varying angles.72 Cell sheet structures also have extremely high cell densities, which can further support regeneration of tissue function and stronger therapeutic efficacy in general.24 However, cell sheet detachment and stacking can also be problematic as sheets may be damaged or break upon removal, or even fail to detach from P(NIPAAm)-modified surfaces. Cell sheet stacking is currently limited to thicknesses of approximately 80 µm, as layered tissue cannot survive in vivo without proper vascularization to provide nutrients and eliminate accumulated waste.60 Creating thick tissues (>2 mm) endowed with a capillary network that sustain oxygen and nutrient diffusion remains a significant challenge.20
Overcoming the Limitation: Perfusable Blood Vessels
Different attempts have been made to vascularize implantable systems in vitro prior to delivery. Sekine et. al produced a triple-layer cardiac cell sheet with perfusable blood vessels composed of neonatal rat cardiac cells and endothelial cells.56 The group showed that endothelial cells could connect to capillaries in the vascular bed, composed of resected tissue with a connectable artery and vein, and form tubular lumens. In a follow-up study, a prevascularized construct of human aortic endothelial cells sandwiched between two human dermal fibroblast sheets was implanted into a rat; three days after transplantation, newly-formed microvessels near the host vasculature were observed which was accompanied by secretion of angiogenic proteins.53, 54, 72 In general, layered cardiac cell sheets have been shown to beat spontaneously, synchronize with existing tissue, and have long-term durability.30 Merging functional cell layers (e.g., cardiomyocytes) with layers that induce vascularization (e.g., endothelial cells) may improve cell survival in a thick tissue-engineered construct in future efforts.
Mechanical Conditioning for Cell Differentiation in Cardiac Cell Sheets
Researchers continually strive to produce increasing amounts of the main cells responsible for contraction within contractile tissues: cardiomyocytes in myocardium and VSMCs in tunica media of blood vessels. Because cardiovascular cells experience constant dynamic stress both during development and postnatally, changing current ESC and iPSC differentiation protocols such that they better mimic the native environmental stresses seen by the cells in vivo may enhance the resulting phenotypic distribution of differentiated populations. Although research applying temporal-specific biochemical cues for pluripotent stem cell differentiation has been extensive and reviewed in-depth elsewhere,40, 43 responses resulting from applying other well-timed exogenous cues, particularly mechanical stress, are less understood. Understanding the role mechanical stress plays in determining cell fate decisions can guide future differentiation protocols. The combinatorial effects of bio-mechanical cues in conjunction with biochemical and other physical cues may improve differentiation yields and significantly reduce the time-frame for tailoring patient-specific regenerative therapies.
It is interesting to note that results from studies that have used cyclic strain on monolayers of ESCs contradict each other on whether strain increases or decreases expression of pluripotent markers.27, 52 Some research groups have found that dynamic stress environments can increase proliferation and inhibit differentiation.5, 11, 52, 57 Most notably, Saha et al. showed that cyclic strain inhibits ESC differentiation.52 However, a recent review discussed how applied mechanical stimulation does in fact direct differentiation of ESCs to cardiomyocytes.16 In contradiction to Saha et al.,52 the sum of these investigations on both cell monolayers and embryoid bodies (EBs, cellular aggregates to recapitulate the developing embryo) suggests: (a) short bursts of higher magnitude strain can decrease pluripotency, and (b) timing of applied cyclic stress affects differentiation, where early and prolonged exposure maintains pluripotency, but short durations at slightly later time points may increase cardiomyocyte marker expression.16 Similarly, although groups have studied the effect of fluid shear to derive endothelial cells from pluripotent stem cells,1, 2, 76 few have studied the role of mechanical stimulation to differentiate pluripotent stem cells to VSMCs,59 which control pulsatile flow in the vasculature. VSMCs can spontaneously differentiate from 10- to 15-day old EBs of human ESCs but not from two-dimensional culture.14, 15 On the other hand, Shimizu et al. determined on a cell monolayer of mouse ESCs that cyclic strain can induce VSMC differentiation from ESCs, with VSMC marker expression increasing as strain magnitude increases.59
Additionally, current pluripotent stem cell differentiation protocols produce VSMC and cardiomyocytes typically with fetal phenotypes.70, 77 Mature cells may induce ECM secretion that can affect the subsequent mechanical properties of tissues, which may impede matching mechanical and contractile properties of grafts to native tissue. Lack of mechanical stimulation can cause cardiomyocytes and VSMCs to dedifferentiate toward fetal phenotypes; thus, Zimmermann et al. reasoned that stimulation may accelerate maturation. They showed that neonatal rat cardiomyocytes cast in collagen gels and subjected to uniaxial cyclic stress (10% and 2 Hz) more closely resembled adult cardiomyocytes with longer stress durations.78 Other studies performed with mouse39 and human ESCs64 gave similarly positive results. Likewise, Wanjare et al. has been the only group to direct regulation of VSMC mature phenotype for human ESCs and iPSCs; however, the study only used growth factors to induce maturation.70 Nunes et al. created a platform capable of generating hESC-derived and hiPSC-derived cardiomyocytes using electrical stimulation.45 For both cardiomyocytes and VSMCs, it remains unknown if mechanical conditioning alone can regulate phenotype maturation.
Overall, the importance of mechanotransduction mechanisms on the regulation of cardiomyocyte function and contractile machinery has been demonstrated for heart development and following in vitro mechanical and physical stimuli. Indeed, a variety of models have been created to predict the impact of geometry and cell architecture in cytoskeletal organization of cardiomyocytes – a subject that has been reviewed elsewhere.58
Characterization of Cell Sheets: Model Output Data Collection
Building and refining a computational model requires experimental measurements; in particular, measurements on composition, structure, and function of a tissue-engineered scaffold-less patch and its individual cell sheet layers will be most informative for modifying future models. Myocardial and vascular tissues are comprised mostly of collagen and elastin, of which the ratio of each component in a cell sheet may affect its mechanical properties, such as uniaxial tensile strength and viscoelasticity. In addition, the organization of cells, proteins, and ECM affects cell sheet and tissue functional properties; for example, cells grown randomly will display isotropic behavior, whereas cells arranged in parallel alignment will more likely exhibit anisotropic behavior.
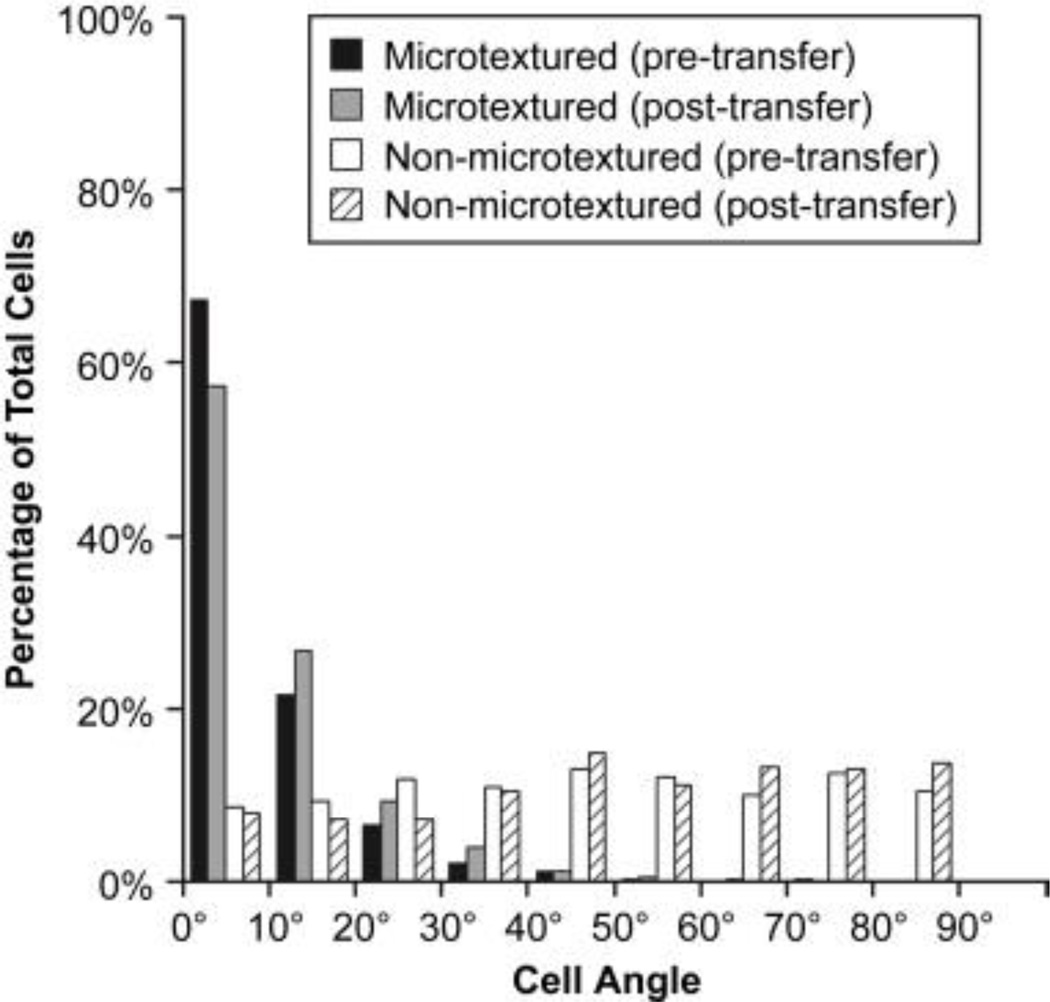
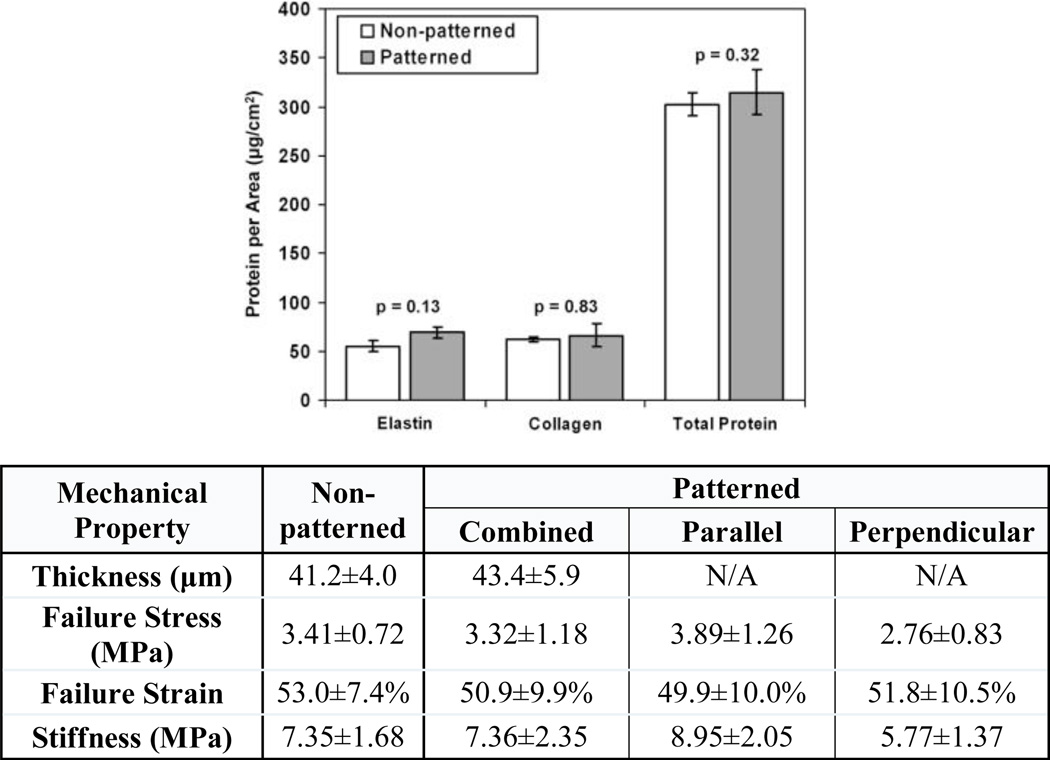
Measurements determined by biochemical (e.g., composition) and physical (e.g., patterning) analyses are unique in that they are outputs of the fabrication inputs, but also can be considered as inputs for models predicting tissue mechanical properties and cell behavior (e.g. growth and remodeling), which can be fed back into the model. Fabrication methods that incorporate biochemical cues (e.g., growth factors) and physical cues (e.g., contact guidance) can thus influence both cell secretion as well as the arrangement of structures in cell sheets and tissues. Experimental evidence suggests the value of incorporating a hierarchical system that ties structure-function relationships into computational models for cell sheet mechanics and growth. For example, our group fabricated polystyrene culture dishes with altered topography (grooves and ridges, 50 µm wide, 5 µm deep) and demonstrated that cell sheets of VSMCs grown and detached from these surfaces retained strong cellular alignment even after transfer from the original substrate (Figure 2 Isenberg).30 We later showed that our cell sheets cultured on micro-textured silicone substrates (same patterning) were ECM-rich and several cell-layers thick; subsequent mechanical testing demonstrated mechanical anisotropy similar to native vessels and resulted in stiffness and strengths that were significantly larger in the direction of alignment (Figure 3 Isenberg).29 Using these parameters (cell alignment angle and sample thickness), we may be able to formulate a simple computational model to predict uniaxial tensile strength; our group is currently collecting more experimental data for establishing similar robust correlations between these types of parameters.
Figure 2.
Orientation of cells on micro-textured and non-micro-textured substrates before and after transfer. VSMC cell sheets maintained strong cellular alignment even after transfer.
Figure 3.
Results showing micro-patterned cell sheets with defined cell and extracellular matrix orientation exhibit anisotropic mechanical properties. Above: Cell sheet matrix composition quantification. Below: Mechanical data for aligned bovine aortic smooth muscle cellular sheets of various thicknesses and alignments.
Current State of the Computational Modeling Space in Relevance to Myocardial Tissue Patch Design
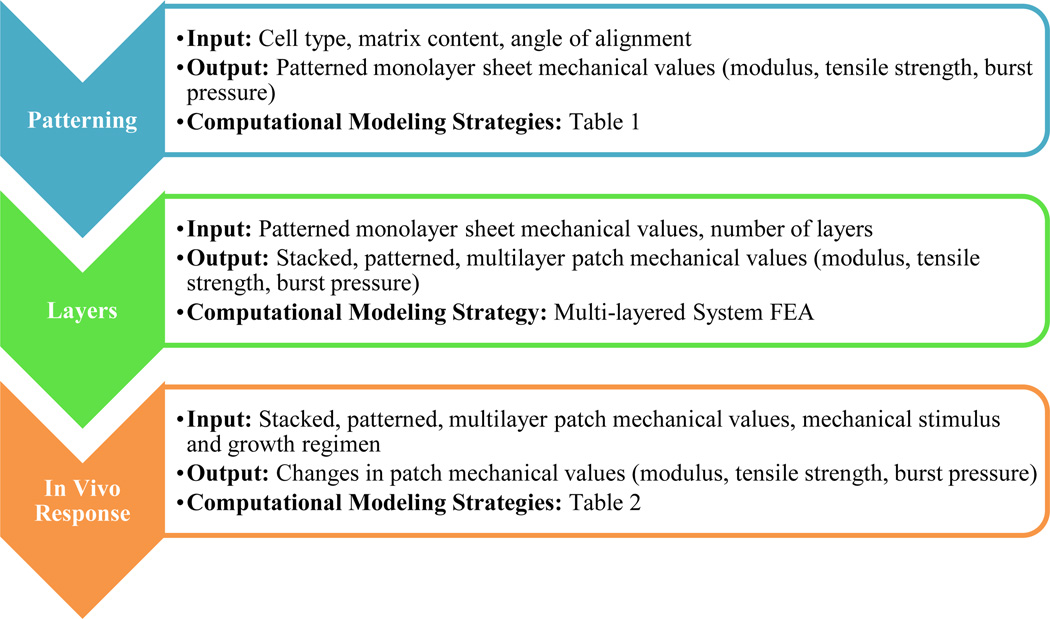
Although using merely experimental methods to optimize tissue design is possible, the large number of input and output variables would make design optimization costly, time-consuming, and inefficient. Computational modeling offers one valuable solution to this problem; this section seeks to explore the current tissue engineering modeling techniques and how they can best be used to build the three tiered model structure we believe is necessary for predictive design of myocardial cell sheet structure and resulting patch mechanical function. As seen in Figure 5, this envisioned computational model would predict resulting patch moduli, tensile strength, and burst pressure based on cell sheet property inputs such as cell type, alignment, and the number of stacked layers. In addition to the inputs and outputs listed for each tier in the diagram, we have also referenced past studies that are most applicable to modeling the specific structure-function relationship within each tier.
Figure 5.
Ideal three-tiered model structure for predicting the mechanical properties of monolayer and stacked cell sheets.
TIER 1: Patterning
Current computational techniques relevant to single sheet mechanics model the constitutive stress-strain behaviors of soft tissue structures by using cellular and matrix properties as inputs. Many of the initial tissue engineering modeling efforts were focused on developing constitutive models that accurately predicted the mechanical properties of native tissues. However, more recent work has been devoted to applying similar mechanical models to tissue-engineered constructs. Two fundamental types of constitutive models exist: phenomenological models and microstructurally-based models. Phenomenological models adequately describe the stress-strain response of a material, but have limited predictive capability because they do not factor in how the microstructure is affecting ultimate function. We, therefore, believe microstructural models such as those outlined in Table 1 are the best way to model our monolayer cell sheets. The table includes examples of modeling both native tissues and tissue engineered constructs and embodies the techniques that we seek to employ in our own monolayer sheet engineering model.
Table 1.
Examples of previous computational tissue engineering work that could be leveraged when creating Tier 1 of the model.
| Author | Year | Hallmark of Model |
|---|---|---|
| Lanir34 | 1983 | Prediction of growth and remodeling of tissue with aligned fibers (specific attention to tissue microstructure, dimensions, and mechanical properties) when an external load is applied to the tissue. |
| Wuyts73 | 1995 | Incorporation of wavy collagen, elastin, and smooth muscle cells. |
| Elson68 | 2000 | Tissue model that uses both extracellular matrix and cellular components to predict mechanical properties of a fibroblast-populated matrix, a type of connective tissue model. |
| Holzapfel26 | 2002 | Framework to describe arterial mechanics by treating the tissue as a two-layered structure with fibers oriented in different directions between layers. |
| Sacks51 | 2003 | Structural constitutive model based on fiber orientation information obtained by using small angle light scattering. Model accurately predicted measure biaxial mechanical response of native bovine pericardium. |
| Zulliger13 | 2004 | Incorporation of unfolding collagen fibers during loading and unloading. |
| Gasser79 | 2006 | Strain energy formulation that incorporated aligned fibers with dispersion. |
| Barocas32 | 2013 | Models the passive mechanical contribution of cells in tissues by representing them as dilute spherical inclusions, allowing for the computational study of ECM-cell interactions. |
| Chesler18 | 2014 | Review of cardiac tissue structure and properties from a materials science perspective. |
TIER 2: Layers
Using the constitutive relationships within tier 1, the mechanical property values of individual cell sheets can be defined. These individual sheet model outputs then become the inputs for a finite element analysis of a multi-layered construct. Standard modeling of stacked materials requires knowledge of each individual layer’s mechanical properties as well as the types of connections at the boundaries between layers. Further experimentation is necessary to understand how individual sheets attach to each other and therefore, what types of connections are forming between layers. Once this is known, these connections along with the mechanical profile of each individual sheet establish a unique set of boundary conditions for solving the constitutive equations associated with the layered construct. Therefore, the optimal design could be determined in silico by iterating over the orientation and stiffness of individual layers until the number and types of layers necessary to form a patch with the desired properties are determined.
TIER 3: In Vivo Response
The ability to predict engineered tissue constructs’ mechanical properties may not be useful for implantable patch design if the effects of in vivo conditions are unknown. Developing computational models to predict how a cell sheet-based tissue responds and reorients to external stimuli such as stretch as discussed in the above section on mechanical conditioning can help to (1) determine optimal culture conditions for obtaining desired patch property values and (2) to establish realistic expectations for how the patch will respond upon implantation. Table 2 documents examples of stimuli-response type models. A model similar to these could be employed to predict tissue response to external stimuli such as surrounding tissue growth and or other mechanical conditioning stimuli.
Table 2.
Examples of previous computational tissue engineering work that could be leveraged when creating Tier 3 of the model.
| Author | Year | Hallmark of Model |
|---|---|---|
| Humphrey28 | 2003 | Theoretically constrained mixture growth model to predict development of residual stresses and changes in material properties by considering that each component of the artery can evolve separately with its own turnover rate. |
| Driessen8 | 2008 | Simulates the structure remodeling in cardiovascular tissues associated with the angular collagen fiber distribution within the arterial wall and aortic valve. |
| Raykin50 | 2009 | Framework for gel-based tissue-engineered blood vessels that predicts tissue geometry and material properties for gels under both static and dynamic loading conditions. |
| Kroon31 | 2010 | Incorporation of remodeling and reorientation of collagen fibers by assuming collagen fibers reorient toward the direction of maximum Cauchy stress; model successfully predicts both collagen alignment and stress-strain curves of the tissues. |
| Kroon31 | 2010 | Computational model for myocardial tissue that assumes fibers reorient to minimize shear; model successfully predicts myofibril reorientation of native tissue under hemodynamic loads. |
Summary and Future Directions
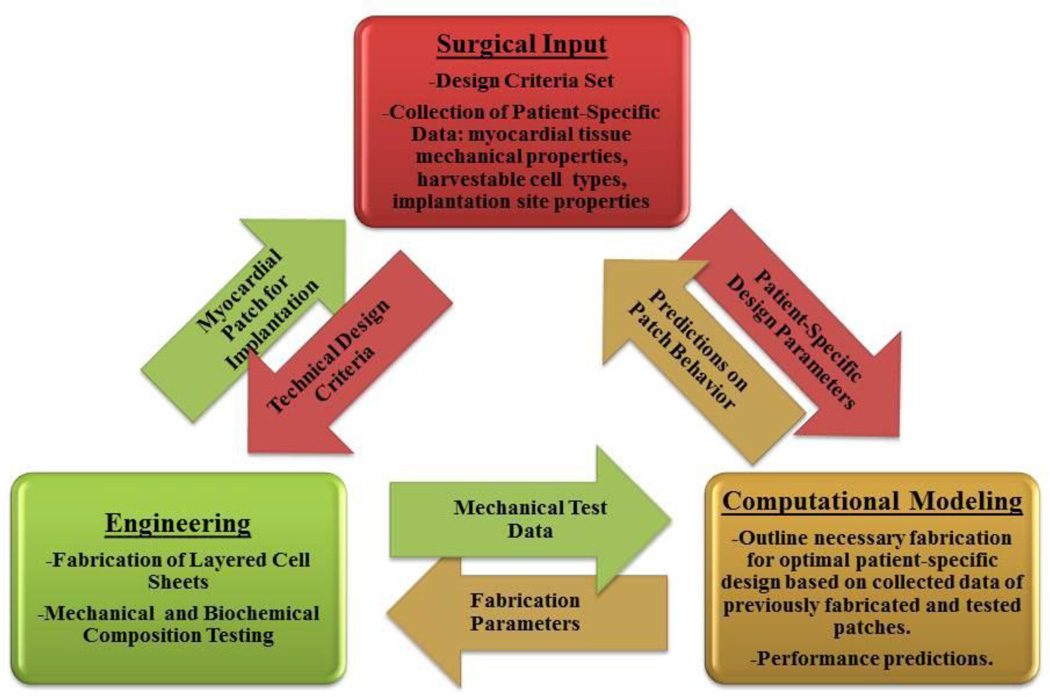
The use of computational modeling to predict mechanical properties and drive experimental fabrication of patient-specific myocardial and vascular patches would be an excellent use of this toolset. As more research groups continue to explore and optimize the use of different cell types with cardiac strengthening and regenerative properties, the library of relevant data will continue to grow. Surgeons can provide patient-specific design criteria to the computational model that can be used to fabricate a myocardial patch with the most promising surgical outcome. Ultimately, the process is iterative, continually building and improving on itself (Figure 4).
Figure 4.
Iterative process involving fabrication and experimental testing, surgical implantation design criteria, and computational modeling.
This theoretically ideal system relies on extensive data collection in several areas of the experimental fabrication process: cell selection, cell differentiation, tissue patterning, mechanical conditioning, and layering different combinations of tissues. The combinations are endless, and while modeling can be used to predict many of the outcomes, an initial investment in experimental data collection will be necessary to establish a reliable, effective modeling system. In addition, the existing models have much room for development of more reliable and effective prediction methods that will ultimately accelerate our efforts in creating a three-dimensional, vascularized scaffold-less myocardial patch. Challenges within the field that have not yet been sufficiently addressed include but are not limited to: the simulation-based estimation of patch failure as it relates to individual and layered cell sheets apparent strength, the collection of a standard database of cell and cell sheet properties that can be used as inputs to models across the field, and a method for establishing properties of crosslinking between layers. Also, important to consider are the differences between healthy and diseased heart tissue as they relate to patch fabrication and successful incorporation into the patient heart, more specifically understanding interactions between both layers within the patch and the patch-tissue interfaces. It is also important to note that each component of the modeling process have a sound method of experimental validation to demonstrate agreement between the model and experimentally collected data as well as other groups’ models. Most mechanical validation involves using both the uniaxial and biaxial tissue testing functionalities on a mechanical testing system to measure mechanical properties during elastic deformation, cyclic motion, and or ultimate failure; experimental values should match those predicted by the model. Once established and validated, a robust model supported by substantial clinical and experimental data will certainly have an impact on the quality of therapeutic design and overall patient surgical care is expected to improve immensely.
Acknowledgments
This work was supported in part by The Hartwell Foundation to J.Y. Wong. E. L. Lee is supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number F32HL115999.
References
- 1.Adamo L, García-Cardeña G. Directed stem cell differentiation by fluid mechanical forces. Antioxidants & redox signaling. 2011;15:1463–1473. doi: 10.1089/ars.2011.3907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adamo L, Naveiras O, Wenzel PL, McKinney-Freeman S, Mack PJ, Gracia-Sancho J, Suchy-Dicey A, Yoshimoto M, Lensch MW, Yoder MC. Biomechanical forces promote embryonic haematopoiesis. Nature. 2009;459:1131–1135. doi: 10.1038/nature08073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen Q, Bismarck A, Hansen U, Junaid S, Tran MQ, Harding SE, Ali NN, Boccaccini AR. Characterisation of a soft elastomer poly (glycerol sebacate) designed to match the mechanical properties of myocardial tissue. Biomaterials. 2008;29:47–57. doi: 10.1016/j.biomaterials.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Cleveland Clinic Heart Book. Disney Press; 2000. Cleveland Clinic Staff. [Google Scholar]
- 5.Cormier JT, Nieden NIZ, Rancourt DE, Kallos MS. Expansion of undifferentiated murine embryonic stem cells as aggregates in suspension culture bioreactors. Tissue Eng. 2006;12:3233–3245. doi: 10.1089/ten.2006.12.3233. [DOI] [PubMed] [Google Scholar]
- 6.Damjanov I. From stem cells to germ cell tumors and back. Verh. Dtsch. Ges. Pathol. 2004;88:39–44. [PubMed] [Google Scholar]
- 7.Denker HW. Potentiality of embryonic stem cells: an ethical problem even with alternative stem cell sources. J. Med. Ethics. 2006;32:665–671. doi: 10.1136/jme.2005.014738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Driessen NJ, Cox MA, Bouten CV, Baaijens FP. Remodelling of the angular collagen fiber distribution in cardiovascular tissues. Biomechanics and Modeling in Mechanobiology. 2008;7:93–103. doi: 10.1007/s10237-007-0078-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ebrahimkhani MR, Young CL, Lauffenburger DA, Griffith LG, Borenstein JT. Approaches to< i>in vitro tissue regeneration with application for human disease modeling and drug development. Drug Discov. Today. 2014 doi: 10.1016/j.drudis.2014.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elloumi-Hannachi I, Yamato M, Okano T. Cell sheet engineering: a unique nanotechnology for scaffold-free tissue reconstruction with clinical applications in regenerative medicine. J. Intern. Med. 2010;267:54–70. doi: 10.1111/j.1365-2796.2009.02185.x. [DOI] [PubMed] [Google Scholar]
- 11.Fok EY, Zandstra PW. Shear-Controlled Single-Step Mouse Embryonic Stem Cell Expansion and Embryoid Body–Based Differentiation. Stem Cells. 2005;23:1333–1342. doi: 10.1634/stemcells.2005-0112. [DOI] [PubMed] [Google Scholar]
- 12.Freire AG, Nascimento DS, Forte G, Valente M, Resende TP, Pagliari S, Abreu C, Carvalho I, Nardo PD, Pinto-do-Ó P. Stable Phenotype and Function of Immortalized Lin− Sca-1 Cardiac Progenitor Cells in Long-Term Culture: A Step Closer to Standardization. Stem cells and development. 2013;23:1012–1026. doi: 10.1089/scd.2013.0305. [DOI] [PubMed] [Google Scholar]
- 13.Gasser TC, Ogden RW, Holzapfel GA. Hyperelastic modelling of arterial layers with distributed collagen fibre orientations. J. R. Soc. Interface. 2006;3:15–35. doi: 10.1098/rsif.2005.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gerecht-Nir S, Ziskind A, Cohen S, Itskovitz-Eldor J. Human embryonic stem cells as an in vitro model for human vascular development and the induction of vascular differentiation. Laboratory investigation. 2003;83:1811–1820. doi: 10.1097/01.lab.0000106502.41391.f0. [DOI] [PubMed] [Google Scholar]
- 15.Gerecht-Nir S, Osenberg S, Nevo O, Ziskind A, Coleman R, Itskovitz-Eldor J. Vascular development in early human embryos and in teratomas derived from human embryonic stem cells. Biol. Reprod. 2004;71:2029–2036. doi: 10.1095/biolreprod.104.031930. [DOI] [PubMed] [Google Scholar]
- 16.Geuss LR, Suggs LJ. Making cardiomyocytes: How mechanical stimulation can influence differentiation of pluripotent stem cells. Biotechnol. Prog. 2013;29:1089–1096. doi: 10.1002/btpr.1794. [DOI] [PubMed] [Google Scholar]
- 17.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Golob M, Moss RL, Chesler NC. Cardiac Tissue Structure, Properties, and Performance: A Materials Science Perspective. Ann. Biomed. Eng. 2014;42:2003–2013. doi: 10.1007/s10439-014-1071-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greisler HP. Interactions at the blood/material interface. Ann. Vasc. Surg. 1990;4:98–103. doi: 10.1007/BF02042699. [DOI] [PubMed] [Google Scholar]
- 20.Griffith CK, Miller C, Sainson RC, Calvert JW, Jeon NL, Hughes CC, George SC. Diffusion limits of an in vitro thick prevascularized tissue. Tissue Eng. 2005;11:257–266. doi: 10.1089/ten.2005.11.257. [DOI] [PubMed] [Google Scholar]
- 21.Guilak F, Butler DL, Goldstein SA, Baaijens F. Biomechanics and mechanobiology in functional tissue engineering. J. Biomech. 2014 doi: 10.1016/j.jbiomech.2014.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gupta V, Grande-Allen KJ. Effects of static and cyclic loading in regulating extracellular matrix synthesis by cardiovascular cells. Cardiovasc. Res. 2006;72:375–383. doi: 10.1016/j.cardiores.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 23.Guvendiren M, Burdick JA. Engineering synthetic hydrogel microenvironments to instruct stem cells. Curr. Opin. Biotechnol. 2013;24:841–846. doi: 10.1016/j.copbio.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haraguchi Y, Shimizu T, Sasagawa T, Sekine H, Sakaguchi K, Kikuchi T, Sekine W, Sekiya S, Yamato M, Umezu M. Fabrication of functional three-dimensional tissues by stacking cell sheets in vitro. Nature protocols. 2012;7:850–858. doi: 10.1038/nprot.2012.027. [DOI] [PubMed] [Google Scholar]
- 25.Haraguchi Y, Shimizu T, Yamato M, Okano T. Concise review: cell therapy and tissue engineering for cardiovascular disease. Stem Cells Transl. Med. 2012;1:136–141. doi: 10.5966/sctm.2012-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holzapfel GA, Gasser TC, Stadler M. A structural model for the viscoelastic behavior of arterial walls: continuum formulation and finite element analysis. European Journal of Mechanics-A/Solids. 2002;21:441–463. [Google Scholar]
- 27.Horiuchi R, Akimoto T, Hong Z, Ushida T. Cyclic mechanical strain maintains Nanog expression through PI3K/Akt signaling in mouse embryonic stem cells. Exp. Cell Res. 2012;318:1726–1732. doi: 10.1016/j.yexcr.2012.05.021. [DOI] [PubMed] [Google Scholar]
- 28.Humphrey J, Rajagopal K. A constrained mixture model for arterial adaptations to a sustained step change in blood flow. Biomechanics and modeling in mechanobiology. 2003;2:109–126. doi: 10.1007/s10237-003-0033-4. [DOI] [PubMed] [Google Scholar]
- 29.Isenberg BC, Backman DE, Kinahan ME, Jesudason R, Suki B, Stone PJ, Davis EC, Wong JY. Micropatterned cell sheets with defined cell and extracellular matrix orientation exhibit anisotropic mechanical properties. J. Biomech. 2012;45:756–761. doi: 10.1016/j.jbiomech.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 30.Isenberg BC, Tsuda Y, Williams C, Shimizu T, Yamato M, Okano T, Wong JY. A thermoresponsive, microtextured substrate for cell sheet engineering with defined structural organization. Biomaterials. 2008;29:2565–2572. doi: 10.1016/j.biomaterials.2008.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kroon M. A continuum mechanics framework and a constitutive model for remodelling of collagen gels and collagenous tissues. J. Mech. Phys. Solids. 2010;58:918–933. [Google Scholar]
- 32.Lai VK, Hadi MF, Tranquillo RT, Barocas VH. A Multiscale Approach to Modeling the Passive Mechanical Contribution of Cells in Tissues. J. Biomech. Eng. 2013;135:071007. doi: 10.1115/1.4024350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Langer R, Vacanti JP. Tissue Engineering. Science. 1993;260:920–926. doi: 10.1126/science.8493529. [DOI] [PubMed] [Google Scholar]
- 34.Lanir Y. Constitutive equations for fibrous connective tissues. J. Biomech. 1983;16:1–12. doi: 10.1016/0021-9290(83)90041-6. [DOI] [PubMed] [Google Scholar]
- 35.Lee EL, Von Recum HA. Cell culture platform with mechanical conditioning and nondamaging cellular detachment. Journal of Biomedical Materials Research Part A. 2010;93:411–418. doi: 10.1002/jbm.a.32754. [DOI] [PubMed] [Google Scholar]
- 36.Lee EL, Watson KC, von Recum HA. Contractile Protein and Extracellular Matrix Secretion of Cell Monolayer Sheets Following Cyclic Stretch. Cardiovascular Engineering and Technology. 2012;3:302–310. [Google Scholar]
- 37.Lees JG, Lim SA, Croll T, Williams G, Lui S, Cooper-White J, McQuade LR, Mathiyalagan B, Tuch BE. Transplantation of 3D scaffolds seeded with human embryonic stem cells: biological features of surrogate tissue and teratoma-forming potential. 2007 doi: 10.2217/17460751.2.3.289. [DOI] [PubMed] [Google Scholar]
- 38.Leor J, Cohen S. Myocardial tissue engineering: creating a muscle patch for a wounded heart. Ann. N. Y. Acad. Sci. 2004;1015:312–319. doi: 10.1196/annals.1302.026. [DOI] [PubMed] [Google Scholar]
- 39.Liau B, Christoforou N, Leong KW, Bursac N. Pluripotent stem cell-derived cardiac tissue patch with advanced structure and function. Biomaterials. 2011;32:9180–9187. doi: 10.1016/j.biomaterials.2011.08.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lin C, Yu C, Ding S. Toward directed reprogramming through exogenous factors. Curr. Opin. Genet. Dev. 2013;23:519–525. doi: 10.1016/j.gde.2013.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lin JB, Isenberg BC, Shen Y, Schorsch K, Sazonova OV, Wong JY. Thermo-responsive poly (< i>N-isopropylacrylamide) grafted onto microtextured poly (dimethylsiloxane) for aligned cell sheet engineering. Colloids and Surfaces B: Biointerfaces. 2012;99:108–115. doi: 10.1016/j.colsurfb.2011.10.040. [DOI] [PubMed] [Google Scholar]
- 42.Masuda S, Shimizu T, Yamato M, Okano T. Cell sheet engineering for heart tissue repair. Adv. Drug Deliv. Rev. 2008;60:277–285. doi: 10.1016/j.addr.2007.08.031. [DOI] [PubMed] [Google Scholar]
- 43.Mummery CL, Zhang J, Ng ES, Elliott DA, Elefanty AG, Kamp TJ. Differentiation of human embryonic stem cells and induced pluripotent stem cells to cardiomyocytes: a methods overview. Circ. Res. 2012;111:344–358. doi: 10.1161/CIRCRESAHA.110.227512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nascimento DS, Mosqueira D, Sousa LM, Teixeira M, Filipe M, Resende TP, Araujo AF, Valente M, Almeida J, Martins JP, Santos JM, Barcia RN, Cruz P, Cruz H, Pinto-do-O P. Human umbilical cord tissue-derived mesenchymal stromal cells attenuate remodeling following myocardial infarction by pro-angiogenic, anti-apoptotic and endogenous cell activation mechanisms. Stem Cell. Res. Ther. 2014;5:5. doi: 10.1186/scrt394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nunes SS, Miklas JW, Liu J, Aschar-Sobbi R, Xiao Y, Zhang B, Jiang J, Massé S, Gagliardi M, Hsieh A. Biowire: a platform for maturation of human pluripotent stem cell-derived cardiomyocytes. Nature methods. 2013;10:781–787. doi: 10.1038/nmeth.2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Okano T, Yamada N, Sakai H, Sakurai Y. A novel recovery system for cultured cells using plasma-treated polystyrene dishes grafted with poly (N-isopropylacrylamide) J. Biomed. Mater. Res. 1993;27:1243–1251. doi: 10.1002/jbm.820271005. [DOI] [PubMed] [Google Scholar]
- 47.Patel NG, Zhang G. Responsive systems for cell sheet detachment. Organogenesis. 2013;9:93–100. doi: 10.4161/org.25149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pietak A, McGregor A, Gauthier S, Oleschuk R, Waldman S. Are micropatterned substrates for directed cell organization an effective method to create ordered 3D tissue constructs? Journal of tissue engineering and regenerative medicine. 2008;2:450–453. doi: 10.1002/term.114. [DOI] [PubMed] [Google Scholar]
- 49.Prabhakaran MP, Venugopal J, Kai D, Ramakrishna S. Biomimetic material strategies for cardiac tissue engineering. Materials Science and Engineering: C. 2011;31:503–513. [Google Scholar]
- 50.Raykin J, Rachev AI, Gleason RL. A phenomenological model for mechanically mediated growth, remodeling, damage, and plasticity of gel-derived tissue engineered blood vessels. J. Biomech. Eng. 2009;131:101016. doi: 10.1115/1.4000124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sacks MS. Incorporation of experimentally-derived fiber orientation into a structural constitutive model for planar collagenous tissues. J. Biomech. Eng. 2003;125:280–287. doi: 10.1115/1.1544508. [DOI] [PubMed] [Google Scholar]
- 52.Saha S, Ji L, de Pablo JJ, Palecek SP. Inhibition of human embryonic stem cell differentiation by mechanical strain. J. Cell. Physiol. 2006;206:126–137. doi: 10.1002/jcp.20441. [DOI] [PubMed] [Google Scholar]
- 53.Sasagawa T, Shimizu T, Sekiya S, Haraguchi Y, Yamato M, Sawa Y, Okano T. Design of prevascularized three-dimensional cell-dense tissues using a cell sheet stacking manipulation technology. Biomaterials. 2010;31:1646–1654. doi: 10.1016/j.biomaterials.2009.11.036. [DOI] [PubMed] [Google Scholar]
- 54.Sasagawa T, Shimizu T, Yamato M, Okano T. Expression profiles of angiogenesis-related proteins in prevascular three-dimensional tissues using cell-sheet engineering. Biomaterials. 2014;35:206–213. doi: 10.1016/j.biomaterials.2013.09.104. [DOI] [PubMed] [Google Scholar]
- 55.Sekine H, Shimizu T, Dobashi I, Matsuura K, Hagiwara N, Takahashi M, Kobayashi E, Yamato M, Okano T. Cardiac cell sheet transplantation improves damaged heart function via superior cell survival in comparison with dissociated cell injection. Tissue Engineering Part A. 2011;17:2973–2980. doi: 10.1089/ten.tea.2010.0659. [DOI] [PubMed] [Google Scholar]
- 56.Sekine H, Shimizu T, Sakaguchi K, Dobashi I, Wada M, Yamato M, Kobayashi E, Umezu M, Okano T. In vitro fabrication of functional three-dimensional tissues with perfusable blood vessels. Nature communications. 2013;4:1399. doi: 10.1038/ncomms2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shafa M, Sjonnesen K, Yamashita A, Liu S, Michalak M, Kallos MS, Rancourt DE. Expansion and long-term maintenance of induced pluripotent stem cells in stirred suspension bioreactors. Journal of tissue engineering and regenerative medicine. 2012;6:462–472. doi: 10.1002/term.450. [DOI] [PubMed] [Google Scholar]
- 58.Sheehy SP, Grosberg A, Parker KK. The contribution of cellular mechanotransduction to cardiomyocyte form and function. Biomechanics and modeling in mechanobiology. 2012;11:1227–1239. doi: 10.1007/s10237-012-0419-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shimizu N, Yamamoto K, Obi S, Kumagaya S, Masumura T, Shimano Y, Naruse K, Yamashita JK, Igarashi T, Ando J. Cyclic strain induces mouse embryonic stem cell differentiation into vascular smooth muscle cells by activating PDGF receptor beta. J. Appl. Physiol. 2008;104:766–772. doi: 10.1152/japplphysiol.00870.2007. (1985) [DOI] [PubMed] [Google Scholar]
- 60.Shimizu T, Sekine H, Yang J, Isoi Y, Yamato M, Kikuchi A, Kobayashi E, Okano T. Polysurgery of cell sheet grafts overcomes diffusion limits to produce thick, vascularized myocardial tissues. FASEB J. 2006;20:708–710. doi: 10.1096/fj.05-4715fje. [DOI] [PubMed] [Google Scholar]
- 61.Strait JB, Lakatta EG. Aging-associated cardiovascular changes and their relationship to heart failure. Heart failure clinics. 2012;8:143–164. doi: 10.1016/j.hfc.2011.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tekin H, Ozaydin-Ince G, Tsinman T, Gleason KK, Langer R, Khademhosseini A, Demirel MC. Responsive microgrooves for the formation of harvestable tissue constructs. Langmuir. 2011;27:5671–5679. doi: 10.1021/la200183x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tsuda Y, Shimizu T, Yamato M, Kikuchi A, Sasagawa T, Sekiya S, Kobayashi J, Chen G, Okano T. Cellular control of tissue architectures using a three-dimensional tissue fabrication technique. Biomaterials. 2007;28:4939–4946. doi: 10.1016/j.biomaterials.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 64.Tulloch NL, Muskheli V, Razumova MV, Korte FS, Regnier M, Hauch KD, Pabon L, Reinecke H, Murry CE. Growth of engineered human myocardium with mechanical loading and vascular coculture. Circ. Res. 2011;109:47–59. doi: 10.1161/CIRCRESAHA.110.237206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Venugopal JR, Prabhakaran MP, Mukherjee S, Ravichandran R, Dan K, Ramakrishna S. Biomaterial strategies for alleviation of myocardial infarction. J. R. Soc. Interface. 2012;9:1–19. doi: 10.1098/rsif.2011.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.von Recum HA, Kim SW, Kikuchi A, Okuhara M, Sakurai Y, Okano T. Novel thermally reversible hydrogel as detachable cell culture substrate. J. Biomed. Mater. Res. 1998;40:631–639. doi: 10.1002/(sici)1097-4636(19980615)40:4<631::aid-jbm15>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 67.Vunjak-Novakovic G, Tandon N, Godier A, Maidhof R, Marsano A, Martens TP, Radisic M. Challenges in cardiac tissue engineering. Tissue Engineering Part B: Reviews. 2009;16:169–187. doi: 10.1089/ten.teb.2009.0352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wakatsuki T, Kolodney MS, Zahalak GI, Elson EL. Cell mechanics studied by a reconstituted model tissue. Biophys. J. 2000;79:2353–2368. doi: 10.1016/S0006-3495(00)76481-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang B, Borazjani A, Tahai M, de Jongh Curry, Amy L, Simionescu DT, Guan J, To F, Elder SH, Liao J. Fabrication of cardiac patch with decellularized porcine myocardial scaffold and bone marrow mononuclear cells. Journal of Biomedical Materials Research Part A. 2010;94:1100–1110. doi: 10.1002/jbm.a.32781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wanjare M, Kuo F, Gerecht S. Derivation and maturation of synthetic and contractile vascular smooth muscle cells from human pluripotent stem cells. Cardiovasc. Res. 2013;97:321–330. doi: 10.1093/cvr/cvs315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Williams C, Tsuda Y, Isenberg BC, Yamato M, Shimizu T, Okano T, Wong JY. Aligned Cell Sheets Grown on Thermo-Responsive Substrates with Microcontact Printed Protein Patterns. Adv Mater. 2009;21:2161–2164. [Google Scholar]
- 72.Williams C, Xie AW, Yamato M, Okano T, Wong JY. Stacking of aligned cell sheets for layer-by-layer control of complex tissue structure. Biomaterials. 2011;32:5625–5632. doi: 10.1016/j.biomaterials.2011.04.050. [DOI] [PubMed] [Google Scholar]
- 73.Wuyts F, Vanhuyse V, Langewouters G, Decraemer W, Raman E, Buyle S. Elastic properties of human aortas in relation to age and atherosclerosis: a structural model. Phys. Med. Biol. 1995;40:1577. doi: 10.1088/0031-9155/40/10/002. [DOI] [PubMed] [Google Scholar]
- 74.Xin M, Olson EN, Bassel-Duby R. Mending broken hearts: cardiac development as a basis for adult heart regeneration and repair. Nature Reviews Molecular Cell Biology. 2013;14:529–541. doi: 10.1038/nrm3619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yamada N, Okano T, Sakai H, Karikusa F, Sawasaki Y, Sakurai Y. Thermo-responsive polymeric surfaces; control of attachment and detachment of cultured cells. Die Makromolekulare Chemie, Rapid Communications. 1990;11:571–576. [Google Scholar]
- 76.Yamamoto K, Sokabe T, Watabe T, Miyazono K, Yamashita JK, Obi S, Ohura N, Matsushita A, Kamiya A, Ando J. Fluid shear stress induces differentiation of Flk-1-positive embryonic stem cells into vascular endothelial cells in vitro. Am. J. Physiol. Heart Circ. Physiol. 2005;288:H1915–H1924. doi: 10.1152/ajpheart.00956.2004. [DOI] [PubMed] [Google Scholar]
- 77.Yang X, Pabon L, Murry CE. Engineering adolescence: maturation of human pluripotent stem cell-derived cardiomyocytes. Circ. Res. 2014;114:511–523. doi: 10.1161/CIRCRESAHA.114.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zimmermann WH, Schneiderbanger K, Schubert P, Didie M, Munzel F, Heubach JF, Kostin S, Neuhuber WL, Eschenhagen T. Tissue engineering of a differentiated cardiac muscle construct. Circ. Res. 2002;90:223–230. doi: 10.1161/hh0202.103644. [DOI] [PubMed] [Google Scholar]
- 79.Zulliger MA, Rachev A, Stergiopulos N. A constitutive formulation of arterial mechanics including vascular smooth muscle tone. Am. J. Physiol. Heart Circ. Physiol. 2004;287:H1335–H1343. doi: 10.1152/ajpheart.00094.2004. [DOI] [PubMed] [Google Scholar]